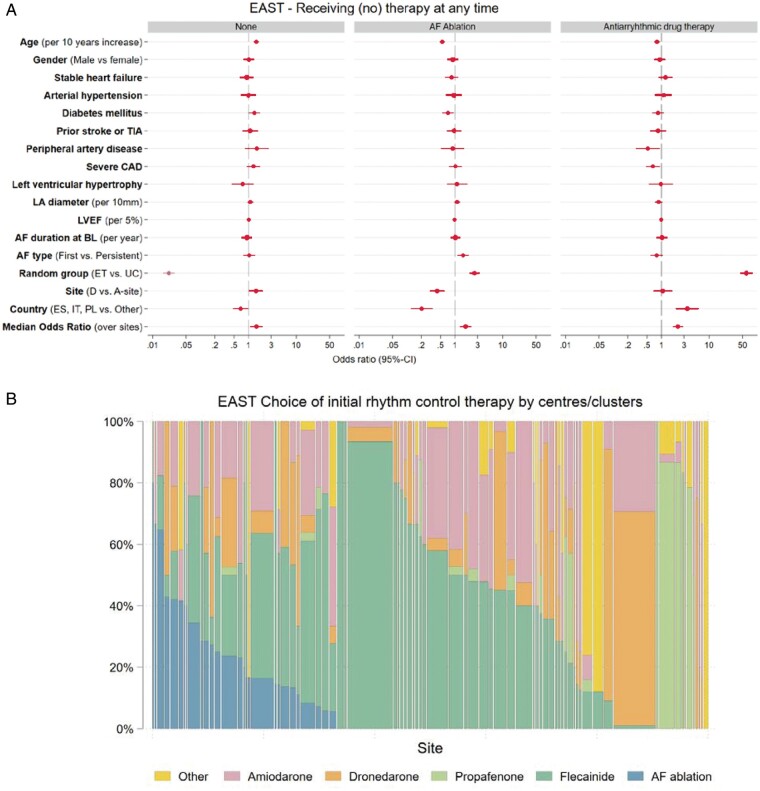
Figure 6.
(A) Multivariate analysis of potential factors influencing the decision to manage patients without rhythm control therapy (None, left panel), to perform AF ablation (middle panel), and to initiate antiarrhythmic drug therapy (AAD, right panel) at any time. The decision to manage without rhythm control therapy was almost entirely driven by randomized group. The decision to perform AF ablation was also influenced by younger age, randomization in an ablation site, diabetes, AF pattern, and country. AF type first, first episode or paroxysmal, persistent, persistent or long-standing persistent; ET, early treatment; Left ventricular hypertrophy on echocardiography was defined based on the inclusion criterium (>15 mm wall thickness); Severe CAD, severe coronary artery disease (previous myocardial infarction, CABG, or PCI); Stable heart failure was defined as either NYHA stage II or LVEF < 50%; TIA, transient ischaemic attack; UC, usual care. (B) Choice of initial rhythm control therapy displayed by centre. Displayed is the proportion of patients receiving each rhythm control therapy option in each centre, limited to centres that initiated rhythm control therapy in at least five patients. There are clear centre-based preferences in the choice of initial antiarrhythmic drug therapy, with individual sites using AF ablation, flecainide, propafenone, dronedarone, or other antiarrhythmic drugs in most patients initially. Therapy choices were guideline-conform in almost all patients.