Abstract
Objective:
This systematic review focused on randomized controlled trials (RCTs) with physicians and nurses that tested interventions designed to improve their mental health, well-being, physical health, and lifestyle behaviors.
Data Source:
A systematic search of electronic databases from 2008 to May 2018 included PubMed, CINAHL, PsycINFO, SPORTDiscus, and the Cochrane Library.
Study Inclusion and Exclusion Criteria:
Inclusion criteria included an RCT design, samples of physicians and/or nurses, and publication year 2008 or later with outcomes targeting mental health, well-being/resiliency, healthy lifestyle behaviors, and/or physical health. Exclusion criteria included studies with a focus on burnout without measures of mood, resiliency, mindfulness, or stress; primary focus on an area other than health promotion; and non-English papers.
Data Extraction:
Quantitative and qualitative data were extracted from each study by 2 independent researchers using a standardized template created in Covidence.
Data Synthesis:
Although meta-analytic pooling across all studies was desired, a wide array of outcome measures made quantitative pooling unsuitable. Therefore, effect sizes were calculated and a mini meta-analysis was completed.
Results:
Twenty-nine studies (N = 2708 participants) met the inclusion criteria. Results indicated that mindfulness and cognitive-behavioral therapy-based interventions are effective in reducing stress, anxiety, and depression. Brief interventions that incorporate deep breathing and gratitude may be beneficial. Visual triggers, pedometers, and health coaching with texting increased physical activity.
Conclusion:
Healthcare systems must promote the health and well-being of physicians and nurses with evidence-based interventions to improve population health and enhance the quality and safety of the care that is delivered.
Keywords: physicians, nurses, systematic review, mental health, physical health, lifestyle behaviors
Objectives
In 2017, the National Academy of Medicine (NAM) launched the Action Collaborative on Clinician Well-being and Resilience because of epidemic levels of burnout, depression, and suicide in physicians, nurses, and other healthcare providers.1 Burnout is a syndrome characterized by a high degree of emotional exhaustion and depersonalization along with a low sense of personal accomplishment at work, which has a high association with depression.2 The Action Collaborative’s primary goal is to decrease rates of clinician burnout in the United States in order to ultimately improve population health of clinicians and ensure health-care quality and safety.2
Findings from a recent systematic review indicate that over 50% of physicians and nurses are experiencing burnout. Another recent study with nearly 1800 nurses from 19 healthcare systems across the country found that over 50% of respondents reported suboptimal physical and mental health.3 Depression affected 25% of this sample and was the leading cause of medical errors, which are now the third leading cause of death in America.4 Nurses with poor mental and physical health were 26% to 71% more likely to report making medical errors compared to those in better health.
Although physicians and nurses do their best to provide outstanding care to their patients, they often do not prioritize their own self-care. As a result, participation in healthy lifestyle behaviors are often given a low priority.4 Besides personal factors, there are multiple healthcare system challenges that contribute to clinician burnout and depression, including poor staffing patterns, ongoing challenges with electronic medical records that result in less time with patients, and pressure to increase caseloads.5 Leaders must address these healthcare system challenges in order to optimize clinician well-being outcomes to ensure patient safety.
The fourth aim in healthcare quadruple is to improve the work-life and well-being of clinicians.6 If clinicians are not well, healthcare quality and safety may suffer. It is imperative for healthcare systems to invest in an infrastructure that includes providing evidence-based interventions that are known to cultivate a culture that supports clinician health and well-being in order to reach the quadruple aim in health care. A model identifying factors affecting clinician well-being and resilience has been created by NAM.7 In this model, external and individual factors have been identified. External factors include sociocultural factors, regulatory, business, and payer environment, organizational factors, and learning/practice environment. Individual factors include healthcare role, personal factors, skills, and abilities. A wide array of interventions have been designed to promote well-being in clinicians primarily within the personal factors identified on the model. Individual level interventions include a focus on physical health, mental health, mindfulness, stress reduction, resilience, and others. A website that contains a knowledge hub has been created by the NAM to support clinician well-being and resilience that includes many resources.8
There have been a number of systematic reviews completed that have focused on a singular aspect of wellness for physicians and/or nurses. However, this review is different than others in that a wide array of experimental studies were included that implemented a variety of interventions that sought to improve mental health, well-being, lifestyle behaviors, and/or physical health in order to identify evidence-based interventions to improve population health in physicians and nurses. The objective of this study was to conduct a systematic review of interventions targeted to improve all of these outcomes.
Methods
Data Source
The Institute of Medicine guidelines for completing systematic reviews were used and reporting of findings followed PRISMA guidelines.9,10 Prior to beginning the review, a protocol was developed and registered with PROSPERO (#CRD42018098869). A research librarian conducted the literature search. Electronic databases searched for studies published between 2008 through May of 2018 included PubMed, CINAHL, PsycINFO, SPORTDiscus, and Cochrane Library (see Online Appendix A). All aspects of the review process were completed by 2 researchers. Titles and abstracts of all articles were screened for applicability. If the article appeared to meet the review’s inclusion criteria, the full article was reviewed and assessed to ensure that it met the criteria for inclusion. All discrepancies were reviewed by the same 2 researchers and consensus was met regarding the eligibility of the study. For each article included in this review, all references were reviewed for inclusion criteria. Additionally, citations for all included studies were identified through Google Scholar and reviewed for inclusion criteria.11
Inclusion and Exclusion Criteria
Inclusion criteria for this review included a randomized controlled trial (RCT) design, samples of physicians and/or nurses, and publication year 2008 or later with outcomes targeting mental health (ie, stress, anxiety, depression, and negative mood), well-being/resiliency, healthy lifestyle behaviors, and/or physical health. Exclusion criteria included studies with a focus on burnout without measures of mood (ie, depression/anxiety), resiliency, mindfulness, or stress; primary focus on an area other than health promotion (eg injury prevention and weight loss); and non-English papers.
Data Extraction
Quantitative and qualitative data were extracted from each study by 2 independent researchers using a standardized template created in Covidence™.11 Data extracted included study author, location, population demographics, sample size, intervention details, quality details, and outcomes. Critical appraisal of studies was performed using Cochrane Collaboration’s tool for assessing the risk of bias.12
Data Synthesis
Although meta-analytic pooling across all the studies was desired, a wide variety of outcome measures was used to make quantitative pooling unsuitable. However, Cohen’s deffect sizes were calculated on studies reporting means and standard deviations. For studies measuring similar concepts, effect sizes were assessed with a mini meta-analysis using a fixed-effect approach.13 A Z-score was calculated based on the mean effect size and its standard error with the corresponding P-value identified. Additionally, studies were summarized descriptively and assessed qualitatively.
Results
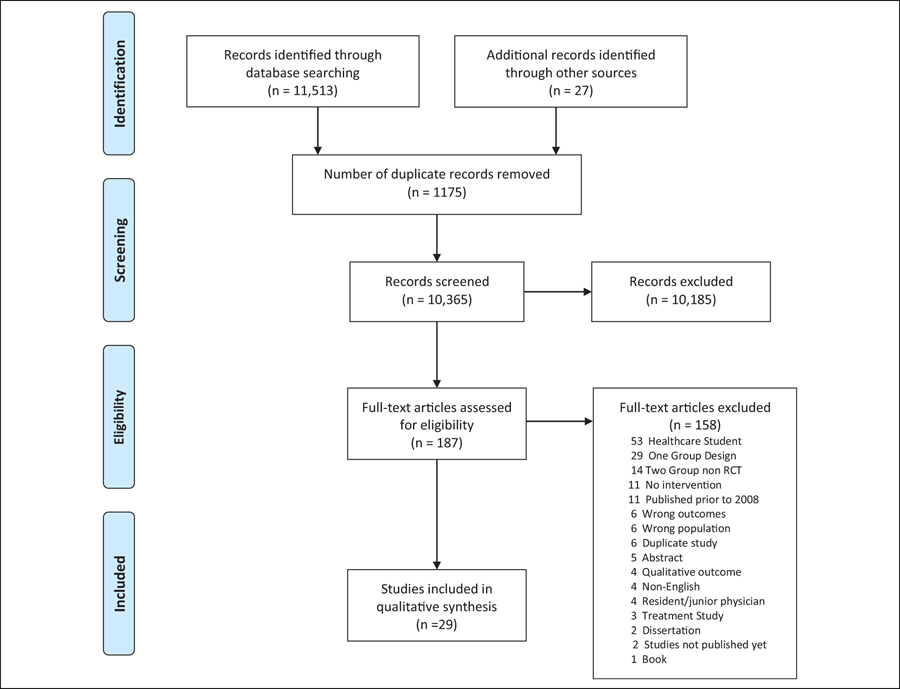
Due to a broad search that was conducted, a wide array of studies were identified with most not meeting inclusion criteria. Eleven thousand five hundred forty references were identified for screening. Duplicates were removed (n = 1175). One hundred eighty-seven studies appeared to meet inclusion criteria and were assessed for full-text eligibility. One hundred fifty-eight studies were excluded for various reasons, including no intervention, the study involved students, and non-RCT design. This process resulted in 29 studies being included in this review (see Figure 1).14–42 These 29 studies had sample sizes of 22 to 557. Six studies included physicians; 6 included nurses; and 17 included physicians, nurses, and/or other allied health-care professionals. Ten studies had attention-control groups, 11 studies used wait-list control groups, 6 studies had no-attention control groups, and 2 studies had cross-over designs.
Figure 1.
PRISMA flow diagram. From: Moher D, Liberati A, Tetzlaff J, Altman DG; The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009;6(7): e1000097. doi:10.1371/journal.pmed1000097
Instrumentation
Multiple instruments were used to measure a variety of mental health outcomes in the included studies. Seven studies measured anxiety, which was captured with the Generalized Anxiety Disorder-7 Scale, the Smith anxiety scale, the Symptoms Checklist-90-Revised, and the Depression, Anxiety, and Stress Scale (DASS-21).18,25,31,32,34,37,38 Tools to measure mood in 8 studies included the Profile of Mood States, symptoms of distress, the Brief Symptom Index, the DASS, and mental health questions from the Short Form 36.15,19,20,23,24,26,29,30 Stress was most commonly measured with the Perceived Stress Scale and the DASS 12-item stress subscale. Other stress tools included the Coping with Stress Scale, the Nursing Stress Scale, and the Post-traumatic Diagnostic Scale.17,18,22,23,25,27–29,31–33,36–38,42 The most common instruments used to assess mindfulness were the Five Facets of Mindfulness Questionnaire and the Mindful Attention Awareness Scale.14,15,18,35,36,38,41
Nine studies measured depression, which was assessed with the Center for Epidemiologic Studies Depression Scale, the DASS-21, the Beck Depression Inventory-II, the Symptom Checklist 90 Revised-Depression, the 2-item Primary Care Evaluation of Mental Health, and a 2-question screen.17,25,29–34,42 Well-being measures included the Work Ability Index Score, the Self Compassion Scale; the World Health OrganisationFive (WHO-5) Well-Being Index, Work Engagement, Empowerment at Work, and the Quality of Life: Linear Analog Self-Assessment Scale.20,21,24,25,29,32,37–39
Three studies measured physical activity with a pedometer or reported physical activity.19,28,40 Six studies included either body mass index (BMI) or weight.16,19,26,28,30,40 Three studies included a measure of percent body fat.16,30,40 Two studies measured blood pressure16,19and 2 studies measured oxygen uptake during peak exercise () peak.16,30
Type and Length of Interventions Delivered
Twelve studies provided a mindfulness-based stress reduction (MBSR) type intervention (see Table 1).14,15,20,31–36,39,41,42 The duration of studies was between 4 weeks to 9 months with total time in intervention sessions ranging from 10 to 53 hours plus home practice. The typical number of sessions in these MBSR interventions were 8 weekly sessions plus home practice. Eight studies provided stress reduction programs that included a variety of interventions, such as journaling, web-based stressed management, breathing exercises, and yoga.17,18,22,23,27,29,37,38 Duration of interventions in these studies were between 4 weeks and 12 to 18 months with time ranging between 1 and 12 hours. Seven studies targeted improvement of lifestyle behaviors, including physical activity and/or healthy eating.16,18,24,26,28,30,40 The duration of these studies was between 4 and 40 weeks with time ranging between 12 and 92 hours. Two studies targeted overall well-being with interventions that included an eMental Health program utilizing cognitive behavior therapy (CBT) components and an online 10-week intervention that included asking physicians to complete microtasks designed to cultivate professional satisfaction and well-being.21,25
Table 1.
Study Details.
| Author, Year, Country, Name and Focus | Design and Control Group; Sample, Setting, N | Intervention Details |
|---|---|---|
| Mindfulness Focused Interventions | ||
| Amutio, 2015, Spain, MBSR | RCT; wait-list CG; physicians; public or private practice; N = 42 | 18 sessions + retreat; FU 12 mo.; TT: 53 hours + home practice |
| Asuero, 2014, Spain, MBSR | RCT; wait-list CG; physicians, nurses, social workers, & clinical psychologist; primary health care; N = 68 | 8 wkly sessions + retreat; mindfulness based coping strategies & yoga; TT 28 hours + home practice |
| Duchemin, 2015, USA, MBSR | RCT; wait-list CG; Nurses & other; Surgical ICU; N = 32 | 8 wkly sessions; Mindfulnes, yoga, mindful eating & music; TT: *26 hours |
| Mealer, 2014, USA, MBSR; PA; counselling; journally | RCT; no attention CG; ICU nurses; hospital; N = 29 | multimodal intervention; duration 12 wks;TT: 27 hours MBSR, exercise, + 2 day training & counselling (CBT) |
| Mistretta, 2018, USA, MBRT | 3 group RCT; attention CG; health-care workers at Mayo Clinic; N = 60 | 6 wkly sessions; duration 6 wks; FU at 3 mo. Resilience trainngMBRTorSmartphone;TT: MBRT I2hours + home practice; smartphone not specified |
| Moody, 2013, Israel & USA, MBSR | RCT; no attention CG; nurses, social workers, physicians, nurse practitioners, psychologists, & child-life specialists; hospital; N = 47 | 8 wkly sessions; FU at postintervention: mindfulness concepts; TT: 15 hours + 9 to 18 hours of practice |
| Pipe, 2009, USA, MBSR | RCT with attention CG; nursing leaders from a health-care system; N = 32 | 5 sessions; duration 4 wks; MBSR &/or educational classes; TT: 10 hours + 15 hours daily practice |
| Querstret, 2017, United Kingdom, MBSR; MBCT | RCT; wait-list CG; Dietitians, physiotherapists, nurses, & physicians; health-care workers across the United Kingdom; N = 127 | 10 online sessions; duration * 7 wks; FU at 6 mo.; formal meditation skills & informal mindfulness techniques; TT: varied |
| Schroeder, 2016, USA, MBSR Steinberg, 2016, USA, MBSR | RCT; wait-list CG; Primary care physicians; N = 33 RCT; wait-list CG; Nurses, patient care assistant, family support coordinator, chaplain, janitor, pharmacist, & unit clerk; hospital; N = 32 |
weekend training + 2 FU sessisions: duration 4 wks; FU at 3 mo.; TT: I7 hours 9 sessions; duration 8 wks; mindfulness; yoga, & music; TT: 10 hours + 13.3 hours home practice |
| Valley, 2017, USA, MBSR | RCT; wait-list CG; Nurses, nurse practitioner, & paramedics, hospital health-care system; N = 22 | 8 wkly session + one full day; duration 8 wks; FU at 6 mo.; MBSR & yoga; TT 27 hours+ home practice |
| West, 2014, USA, MBSR | RCT; attention CG; Internal medicine physician; outpt clinic; N = 74 | biwkly sessions; duration 9 mo.; FU at 12 mo.; mindfulness, reflection, & shared experience or I hour of protected time; TT I9 hours |
| Well-being focused interventions | ||
| Dyrbye, 2016, USA, Promote satisfaction & well-being | RCT; attention CG; Physicians at Mayo Clinic; N = 290 | 10 e-mails; duration 10 wks; FU at 3 mo.; wkly microtasks to promote professional satisfaction & well-being; TT: not specified |
| Ketelaar, 2014, Netherlands, Mental Vitality @ Work eMental Health vs OP | 3 group Cluster RCT; wait-list CG; nurses & allied health professionals (physiotherapists & radiotherapists) in one academic hospital; N = 557 | variable sessions; duration not specified; FU at 6 mo.; eMental health interventions or in-person occupational physician consultation; TT: not specified |
| Stress Reduction & Resilence Interventions | ||
| Cheng, 2015, Hong Kong, Gratitude journally | 3-group RCT; No attention CG; Physicians, nurses, physiotherapists, & occupational therapists in 5 public hospitals; N = 102 | 8 sessions; duration 4 wks; FU at 3 mo; write about gratitude experiences or feeling annoyed/angry; TT: not reported, journals done in evening |
| Chesak, 2015, USA, SMART Stress reduction & enhance resiliency | RCT; attention CG; new nurses; academic medical center; N = 55 | 2 sessions; duration 4 wks; FU at I2 wks; enhance resiliency; brief Stress Management & Resiliency Training (SMART) program; Control: lecture r/t stress, reality shock & work-life connectedness; TT: 2.5 hours |
| Fang, 2015, China, Yoga | RCT; no attention CG; Nurses; hospital, N = 120 | > 2X/week for 50–60 minutes after work hours; |
| Hersch, 2016, USA, Stress Management | RCT; wait-list CG; Nurses, advance practice nurses, clinical nurse managers; hospital; N = 104 | Duration 6 mo.; yoga. TT: varied 7 modules (nurses) + 1 nurse managers. Access for 3 mo.; stress management; TT: ave. logged on I-3X for ave. of 43 minutes |
| Linzer, 2015, USA, Healthy Work Place Study Improve work environment | Cluster RCT; no attention CG; Primary care clinicians (physicians, nurse practitioners, & physician assistant); health-care clinics; N = 166 | 1 facilitated session by research staff to help customize a list of ways to address work conditions; duration 12–18 mo.; FU at postintervention. TT: not specified |
| Luthar, 2017, USA, Authentic Connections Groups; benefit of relational group program | RCT; attention CG; physicians, PhD’s in clinical pratice, nurse practitioners & physician assistant who are also mothers; outpatient clinic; N = 40 | 12 wkly session; duration 12 wks; wkly sessions regarding respect, empathy & empowerment or I hour of wkly protected time; TT: I2 hours |
| Sood, 2011, USA, SMART stress reduction & enhance resiliency | RCT; wait-list CG; General internal medicine physicians; N = 40 | 2 sessions (1 optional); FU at 8 wks; enhance resiliency; brief Stress Management & Resiliency Training (SMART) program; TT: 1.5 hours + optional .5 to 1 hour |
| Sood, 2014, USA, SMART stress reduction & enhance resiliency | RCT; wait-list CG; Physicians or scientists in radiology; Department of Radiology; N = 26 | 2 sessions (1 optional) + 2 phone calls; FU at 12 wks; enhance resiliency; brief Stress Management & Resiliency Training (SMART) program; TT: 1.5 hours + optional .5 to 1 hour & 2 calls |
| Lifestyle Behavior | ||
| Barene, 2014, Norway, PA Soccer or Zumba | 3 group RCT; no attention CG; Nurses, nurse assistants, & other professions; hospital; N = 118 | 2–3/wk in first 12 wks, 2/wk in wks 12 to 40; duration 40 wks; soccer or zumba; TT 80–92 hours |
| Doran, 2018, USA, WHHIP CV risk reduction | Cluster RCT; attention CG; Long-term care staff; N = 98 | I: Multimodal intervention; C: 30 min educational session; duration 9 mo.; FU at 18 mo.; CV health; TT: not specified |
| Jakobsen, 2017, Denmark, PA | Cluster RCT; attention CG; Female health-care workers hospital; N = 200 | 5×/week; duration 10 wks; exercise at work or at home; TT: 12–15 hours |
| Leedo, 2017, Denmark, Meals at work | RCT; Cross-over design; Physicians, nurses, nursing assistants; hospital; N = 60 | 4 wks of cold meal, water, & snack on all workday shifts. Duration 4 wks; TT: not specified |
| Low, 2015, USA, CV risk reduction | RCT; attention CG; Female employees at hospital; N = 62 | I: wkly contact (phone or e-mail); C: variable & optional; duration 6 mo.; FU at 1 year; I: goal setting & overcoming obatacles; all received CV risk reduction type classes; TT: not specified |
| Matsugaki, 2017, Japan, Work vs home PA | RCT; attention CG; nurses; recruited nurses organization; N = 30 | 24 sessions; duration 12 wks; FU at postintervention; Home versus supervised by PT exercise; TT: 16 hours |
| Tucker, 2016, USA, NEAT PA | RCT; cross-over design; Nurses & medical assistants; ambulatory nursing clinic; N = 42 | ↑activity by 1 hour each day. Duration 6 mo.; All received environmental NEAT+ intervention; I: text messages daily mo 1–3; C: text messages daily mo. 4 to 6; TT: not specified |
Abbreviations: CBT, cognitive behavioral therapy; CG, control group; CV, cardiovascular; FU, follow-up; MBCT, mindfulness-based cognitive therapy; ICU, intensive care unit; MBSR, mindfulness-based stress reduction; mo, months; MBRT, mindfulness-based resilience training; OP, occupational physician; PA, physical activity; SMART, Stress Management & Resiliency Training; RCT, randomized controlled trial; TT, total time of intervention; WHHIP, Worksite Heart Health Improvement Project; NEAT, non-exercise activity thermogenesis.
Studies varied widely in the variables evaluated and findings of significance reached postintervention (see Table 2). Authors reported either within group significance, between-group significance, or both. Significant findings were identified for many variables, but not consistently across all studies.
Table 2.
Reported Significance at Postintervention.a
| Author | Stress | Mindfulness | Mood | Anxiety | Depression | Resilience | Self-Compassion | Empowerment at Work Scale | WHO 5 | Work Ability | Distress | Work Engagement Scale | Quality of Life: Linear Analog Scale | Measure of Sleep | Measure of Fatigue | Measure of Fat | Measure of PA | Measure of Mass | DBP | peak (mL/kg/min) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Amutio | ↑↑ | |||||||||||||||||||
| Asuero | ↑↑ | ↑↑ | ||||||||||||||||||
| Barene | – | ↑↑ | – | – | ||||||||||||||||
| Cheng | ↑↑ | ↑↑ | ||||||||||||||||||
| Chesak | – | – | – | – | ||||||||||||||||
| Doran | ↑↑ | – | ↓↓ | – | –b | |||||||||||||||
| Duchemin | – | ↑ | ||||||||||||||||||
| Dyrbye | – | – | – | – | ||||||||||||||||
| Fang | ↑↑ | ↑↑ | ||||||||||||||||||
| Hersch | ↑↑,--c | – | – | |||||||||||||||||
| Jakobsen | – | ↑↑ | ||||||||||||||||||
| Ketelaar | –d | – | – | – | – | – | ↑↑ | – | ||||||||||||
| Leedo | – | – | ||||||||||||||||||
| Linzer | – | |||||||||||||||||||
| Low | – | – | – | |||||||||||||||||
| Luthar | ↑↑ | ↑↑ | ↑↑ | ↑↑ | – | |||||||||||||||
| Matsugaki | – | – | – | – | ↑↑ | |||||||||||||||
| Mealer | ↑d | – | ↑↑ | ↑ | ||||||||||||||||
| Mistretta | ↑ | – | – | – | ↑ | – | ||||||||||||||
| Moody | – | – | ||||||||||||||||||
| Pipe | ↑↑ | ↑↑ | ||||||||||||||||||
| Querstret | ↑↑ | ↑↑ | ↑↑ | |||||||||||||||||
| Schroeder | ↑↑ | ↑↑ | – | |||||||||||||||||
| Sood 2011 | ↑↑ | ↑↑ | ↑↑ | ↑↑ | – | |||||||||||||||
| Sood 2014 | ↑↑ | ↑↑ | ↑↑ | – | ↑↑b | |||||||||||||||
| Steinberg | ↑ | |||||||||||||||||||
| Tucker | –b | ↑ | ↑b | |||||||||||||||||
| Valley | ↑↑ | |||||||||||||||||||
| West | – | – |
Abbreviations: PA, physical activity; DBP, diastolic blood pressure.
Symbol of significance: ↑↑ Intervention group significant between groups P < .05, ↑ Intervention group significant within groups P < .05, – no sig difference), ↓↓ Control group significant between group.
Significantly different at baseline.
Two different measures of concept.
Measured post-traumatic stress.
Interventions That Improved Mental Health Outcomes
Seven studies assessed a mindfulness outcome (see Table 2). Six (86%) studies reported significant differences between groups, with sample sizes ranging from 22 to 127 and duration between 1.5 and 53 hours.14,15,18,35,36,38,41 One study reported only a correlation of mindfulness with subscales of the DASS and the Maslach’s Burnout Inventory.20
Sixteen studies assessed a measure of stress, 2 of which assessed post-traumatic stress.17,18,20,22,23,25,27–29,31–33,36–41 Seven (44%) studies identified a between-group difference with sample sizes ranging from 26 to 120 and duration between 1.5 and 17 hours. The focus of the interventions included MBSR (n = 1, 14%),36 stress and resiliency (n = 3, 43%),23,37,38 and other (n = 3, 43%).22,17,29
Eight studies assessed a general mood measure.15,19,20,23,24,26,29,30 Three (37.5%) studies identified a significant between-group with sample sizes ranging between 40 and 98 and length of intervention was between 12 and 28 hours. The emphasis of the interventions varied and included MBSR,15 cardiovascular risk reduction,19 and benefits of relational groups.29
Seven studies assessed a measure of anxiety.18,25,31,32,34,37,38 Three (43%) studies identified a significant between-group difference with sample sizes ranging between 26 and 40, and duration was between 1.5 and 25 hours. One study focused on MBSR,34 while the other 2 studies37–38 used the same intervention focusing on decreasing stress and enhancing resiliency.
Nine studies assessed a measure of depression.17,25,29–34,42 Four (44%) studies identified a significant between-group difference. Sample sizes ranged from 29 to 102 and duration between 11.5 and 27 hours of MBSR plus exercise, counseling, and journaling. Emphasis of the interventions included mindfulness (n = 2, 50%),31,34 gratitude (n = 1, 25%),17and benefits of a relational group (n = 1, 25%).29
Interventions That Improved Well-Being/Resilience and Sleep
Five studies assessed a measure of resilience;18,31,36–38 however, only 1 study identified a significant between-group difference.37 This study had a sample size of 40 and included a brief stress management and resiliency training intervention (1.5 hours).
Nine studies assessed a measure of well-being.20,21,24,25,29,32,37,39 Five (56%) studies identified a significant between-group difference. Sample sizes ranged between 26 and 557 and the intervention duration was between 1.5 and 12 hours. Emphasis of the interventions included eMental Health (n = 1, 20%),25 decreasing stress and enhancing resiliency (n = 2, 40%),37,38 exercise (n = 1, 10%),24 benefits of a relational group (n = 1, 20%).29
Eight studies assessed a measure of sleep or fatigue.19,21,22,25,29,32,35,37 Two (25%) studies identified a significant between-group difference. Sample sizes ranged between 120 and 127 and duration of the intervention was between 7 weeks and 6 months (length of time not reported). Emphasis of the interventions included MBSR22 and mindfulness-based CBT.35
Interventions That Improved Lifestyle Behaviors/Physical Health
Six studies assessed a measure of body mass, including BMI or weight.16,19,26,28,30,40 One (17%) study identified a significant between-group difference with sample size 118 and intervention duration 40 weeks ( ~ 80 hours).16 The emphasis of the intervention was soccer or Zumba for exercise with the Zumba group having the significant effect. Three studies assessed a measure of fat.16,30,40 None identified a significant between-group difference. Three studies assessed a measure of physical activity of which none had a significant between-group difference.19,28,40 Blood pressure was measured in 2 studies with none identifying a significant between-group difference.16,19
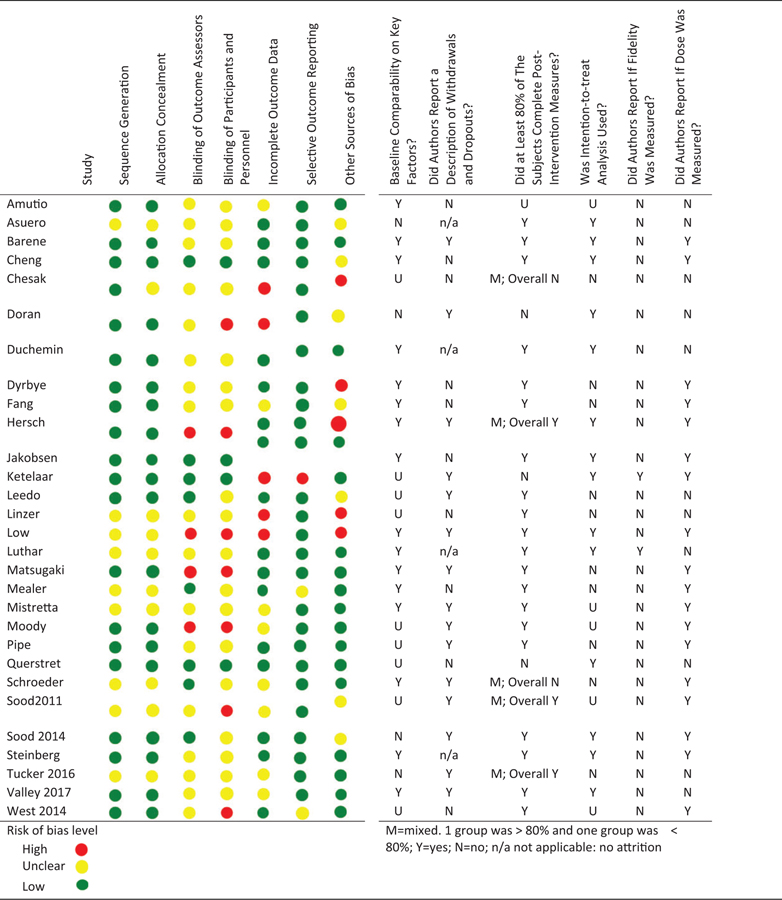
Risk of Bias
All 29 studies were assessed using the Cochrane Bias Tool (see Table 3). Two studies scored low risk of bias for all 7 domains.24,35 The 2 binding domains were predominantly unclear or high risk of bias. The domain primarily judged as low risk was selective outcome reporting. Two domains had 5 studies judged as high risk for bias and included incomplete outcomes data and other sources of bias. Reporting of the randomization method was fairly high with 20 studies being judged as low risk. Six additional items of interest were extracted. Sixteen (55%) studies reported baseline comparability on key factors. Fifteen (52%) studies described drop-outs or withdrawals. Twenty-three (79%) studies had more than 80% of participants with measures at postintervention. Fourteen (48%) studies reported using intention to treat analysis. Only 2 (7%) studies reported fidelity assessment of the interventions. Eighteen (62%) studies indicated dose received by participants.
Table 3.
Quality Measures: Cochrane Risk of Bias for RCT’s and Other Pertinent Information.a
|
Effect Sizes and Mini Meta-Analysis
Effect sizes were calculated for 16 outcome variables (see Table 4). Effect sizes for stress were small, medium, and large almost equally divided. Mindfulness effect sizes were medium to large. Two effect sizes for mood were large with one being less than small. Effect sizes for anxiety ranged between less than small to large. Effect sizes for depression were less than small to small. Resilience effect sizes were medium to large with one being small in favor of the control group. The WHO 5 Well-Being Index and the Work Ability scales had an effect size of less than small to small. Distress and the work engagement scales had small effects. Quality of life effect sizes was less than small and medium. Measures of sleep and fatigue had effect size of less than small, small, and large. The effect size for a measure of fat was large. The effect size for physical activity was medium and large. The effect size for a measure of mass was less than small for 2 studies and large for 1 study. The mean effect size for variables ranged from −0.87 to 0.85. Significant Z-scores for the mini-meta analysis were found for stress, mindfulness, mood, anxiety, resilience, Who-5 Well-Being Index, sleep, and fatigue.
Table 4.
Post Intervention Between Group Effect Sizes and Mini-Meta Analysis.a
| Authorb | Stress | Mindfulness | Mood | Anxiety | Depression | Resilience | WHO 5 | Work Ability | Distress | Work Engagement Scale | Quality of Life | Measure of Sleep | Measure of Fatigue | Measure of Fat | Measure of PA | Measure of Mass |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Amutio | 0.9 | |||||||||||||||
| Asuero | −0.8 | |||||||||||||||
| Chengc | −0.7 | −0.5 | ||||||||||||||
| Chesak | −0.8 | 1.1 | −0.8 | 0.7 | ||||||||||||
| Doran | −1.0 | –0.9d | 0.0d | |||||||||||||
| Fang | −1.4 | |||||||||||||||
| Hersch | −0.6 | 0.2 | ||||||||||||||
| Jakobsenc | 0.2 | |||||||||||||||
| Ketelaar | −0.1 | −0.1 | 0.2 | 0.0 | 0.2 | −0.2 | ||||||||||
| Leedo | −0.1 | 0.0 | ||||||||||||||
| Mistrettae | −0.3 | 0.0c | −0.2 | 0.1 | ||||||||||||
| Querstret | 0.60f | −0.4 | −0.8 | |||||||||||||
| Schroeder | −0.4 | 0.7 | 0.6 | |||||||||||||
| Sood 2011 | −0.9 | −0.6 | 1.1 | 0.6 | −0.4 | |||||||||||
| Sood 2014 | −0.5 | 0.9 | −0.6 | −0.2d | 0.0 | |||||||||||
| Steinberg | 0.2 | |||||||||||||||
| Tucker | −0.9 | 0.6 | −1.1 | |||||||||||||
| Mean ES | −0.60 | 0.85 | −0.63 | −0.20 | −0.13 | 0.58 | −0.18 | 0.13 | n/a | n/a | 0.28 | −0.87 | −0.73 | n/a | −0.29 | −0.21 |
| Mini Meta Z-score | −4.76 | 7.06 | −4.01 | −2.17 | −1.44 | 3.12 | 1.83 | 1.22 | n/a | n/a | 1.29 | −5.90 | −4.06 | n/a | −1.25 | −1.24 |
| P value | <.00001 | <.00001 | .00 | .03 | .15 | .00 | .07 | .11 | n/a | n/a | .20 | <.00001 | .00 | n/a | .21 | .21 |
Abbreviations: ES, effect size; n/a, not applicable: no attrition; PA, physical activity; SD, standard deviation.
Effect size (ES): small 0.20, medium 0.50, large 0.80.
Calculated ES except as noted. Mean (SD) reported in the article.
Effect size reported in manuscript. Mean (SD) not available.
ln favor of control group.
Mean ES of both active intervention groups.
Mean ES of 4 subscales.
Conclusions
There have been several published systematic reviews that focus on 1 specific dimension of wellness for physicians and/or nurses. This review is different and extends the science in that it focused on a wide array of interventions so that findings could reveal which types of interventions are the most effective in improving mental health, well-being, lifestyle behaviors, and/or physical health of physicians and nurses.
Studies in this review evaluated a variety of different types of interventions for decreasing stress, increasing mindfulness and resilience, and improving mood, anxiety, sleep, and fatigue. Many of the studies that incorporated mindfulness techniques had significant positive effects on stress, anxiety, and/or depression and were typically comprised of interventions that included 8 weekly 1- to 2.5-hour sessions led by a mindfulness-trained instructor followed by at least 9 hours of practice at home. Although effective, mindfulness-based interventions are usually time-intensive and require clinicians to attend lengthy sessions followed by several hours of practice that may be difficult to arrange with their schedules. Many hospitals also do not have qualified mindfulness trainers to deliver these interventions.
Three studies included CBT principles or therapy and had positive effects on mindfulness, sleep, fatigue, depression, and work engagement.25,31,35 A recent RCT of an 8-session manualized CBT-based intervention entitled MINDSTRONG© delivered by a nurse to new nurse residents also demonstrated decreases in depression, anxiety, and stress as well as improvements in job satisfaction up to 6 months following the intervention.43,44
Three studies that used a program called Stress Management and Resiliency Training, comprised of a brief 90-minute session that focused on attention and interpretation therapy that aimed to decrease stress and increase resiliency along with the use of deep breathing techniques, was found to lessen physician anxiety.37,38 A focus on helping clinicians to use gratitude practice also was effective on stress and depression.17 Only 1 study measuring physical parameters, such as BMI, fat, or blood pressure, found a significant difference highlighting the difficulty in changing healthy lifestyle behaviors to a significant degree.16
Strengths and Limitations
Strengths of this body of studies include RCT designs and several studies had 6- to 12-month follow-up. However, several weaknesses in methodological design were apparent. Most of the studies did not measure intervention fidelity, which is critical in determining the impact of the interventions on outcomes. Many studies did not have attention-control groups that controlled for time spent with the experimental groups, which threatens their internal validity. Many studies did not report if participants or research staff were blinded. Some studies combined a variety of interventions, which make it difficult to determine what specifically impacted the outcomes. Additionally, the studies assessed outcomes using a variety of different measures, which inhibited pooling of the data across studies. Many studies used self-report measures rather than objective measures. The sample size in many studies also was small and attrition was higher than desirable.
Findings from RCTs are considered high-quality evidence. However, our rating was downgraded due to methodological weaknesses of several studies due to inadequate attention-control groups, lack of blinding or reporting of blinding of participants or research staff, or lack of information regarding handling of missing data. Therefore, the overall quality of this body of evidence appears to be moderate when considering the methodological weaknesses identified.45,46
There are limitations in the conduct of this review. Only English manuscripts have been included with 4 non-English studies identified through the literature search. Studies reported outcomes measured with a variety of tools limiting our ability to pool findings. Effect sizes were only calculated based on data reported in the published manuscripts for each study. Finally, as we wanted to include a large breadth of studies, we limited the study publication dates to the prior 10 years.
Individual and group evidence-based interventions that focus directly on clinicians are important to positively impact their health and well-being outcomes. However, without building a culture of well-being in healthcare systems that makes healthy choices, the norm or the easy choices for clinicians to make, those behaviors are not likely to sustain.47 It is also important to target system-based interventions that are known to adversely affect clinician well-being (eg, short staffing, long work hours, and alarm fatigue). Healthcare systems must invest in the well-being of their clinicians to enhance their outcomes and ultimately improve the quality and safety of care. Prior studies have shown that, for every dollar invested in employee wellness, the return on investment is $3 to $4.48 Value of investment also increases as clinicians who perceive they practice in a healthcare system that is supportive of their well-being tend to be in better physical and mental health, more engaged, and have higher levels of job satisfaction.3
Findings from this systematic review indicate an urgent need for more rigorously designed RCTs with attention-control groups that evaluate the efficacy of interventions to improve the health and well-being outcomes of physicians and nurses. Studies should implement interventions that can be easily reproduced and scaled across the United States. It is critical that fidelity and dose response of interventions be assessed, and similar outcomes be measured so that data can be pooled to conduct meta-analyses. Sample size should be sufficient and long-term follow-up is important. Reliable objective measures provide greater confidence in study results.
Supplementary Material
So What?
What is already known on this topic?
A broad range of interventions have been tested to address physician and nurse mental health, well-being, and physical health with modest improvements.
What does this article add?
Our findings indicated that mindfulness and cognitive-behavioral therapy-based interventions are effective in reducing stress, anxiety, and depression. Brief interventions that incorporate deep breathing and gratitude may be beneficial. Visual triggers, pedometers, and health coaching with texting increased physical activity.
What are the implications for health promotion practice or research?
Healthcare systems need to provide wellness cultures and rapidly translate evidence-based interventions into clinical settings to improve the mental health, healthy lifestyle behaviors, and physical health outcomes of their clinicians, which should lead to improvements in the quality and safety of care. There is a need for more RCTs with rigorous methods and use of similar outcome measures.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Footnotes
Declaration of Conflicting Interests
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Bernadette Mazurek Melnyk is the creator of the MINDBODYSTRONG program referenced in this paper.
Supplemental Material
Supplemental material for this article is available online.
References
- 1.Dzau VJ, Kirch DG, Nasca TJ. To care is human—collectively confronting the clinician-burnout crisis. N Engl J Med. 2018;378(4):312–314. doi: 10.1056/NEJMp1715127. [DOI] [PubMed] [Google Scholar]
- 2.Rotenstein LS, Torre M, Ramos MA, Rosales RC, Guille C, Mata DA. Prevalence of burnout among physicians: a systematic review. JAMA. 2018;320(11):1131–1150. doi: 10.1001/jama.2018.12777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Melnyk BM, Orsolini L, Tan A, et al. A national study links nurses’ physical and mental health to medical errors and perceived worksite wellness. J Occup Environ Med. 2018;60(2):126–131. doi: 10.1097/JOM.0000000000001198. [DOI] [PubMed] [Google Scholar]
- 4.Makary MA, Daniel M. Medical error—the third leading cause of death in the US. BMJ. 2016;353. doi: 10.1136/bmj.i2139. [DOI] [PubMed] [Google Scholar]
- 5.Kavalieratos D, Siconolfi DE, Steinhauser KE, et al. “It is like heart failure. It is chronic ... and it will kill you”: a qualitative analysis of burnout among hospice and palliative care clinicians. J Pain Symptom Manage. 2017;53(5):901–910.e1. doi: 10.1016/j.jpainsymman.2016.12.337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bodenheimer T, Sinsky C. From the triple aim to quadruple aim: care of the patient requires care of the provider. Ann Fam Med. 2014;12:573–576. doi: 10.1370/afm.1713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brigham TC, Barden AL, Dopp A, et al. A journey to construct an all-encompassing conceptual model of factors affecting clinician well-being and resilience. NAM Perspectives, Discussion Paper. National Academy of Medicine, Washington, DC: 2018. doi: 10.31478/201801b. [DOI] [Google Scholar]
- 8.National Academy of Medicine Action Collaborative on Clinician Well-Being and Resilience. 2017. https://nam.edu/initiatives/clinician-resilience-and-well-being/. Accessed February 12, 2020.
- 9.IOM (Institute of Medicine). Finding What Works in Health Care: Standards for Systematic Reviews. Washington, DC: The National Academies Press; 2011. [PubMed] [Google Scholar]
- 10.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–269 doi: 10.7326/0003-4819-151-4-2000908180-00135. [DOI] [PubMed] [Google Scholar]
- 11.Covidence systematic review software, Veritas Health Innovation, Melbourne, Australia. www.covidence.org. [Google Scholar]
- 12.Higgins JP, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration’s Tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Goh JX, Hall JA, Rosenthal R. Mini meta-analysis of your own studies: some arguments on why and a primer on how. Soc Personal Psychol Compass. 2016;10(10):535–549. doi:10.1111.spc3.12267. [Google Scholar]
- 14.Amutio A, Martinez-Taboada C, Hermosilla D, Delgado LC. Enhancing relaxation states and positive emotions in physicians through a mindfulness training program: a one-year study. Psychol Health Med. 2015;20(6):720–731. doi: 10.1080/13548506.2014.986143. [DOI] [PubMed] [Google Scholar]
- 15.Asuero AM, Queralto JM, Pujol-Ribera E, Berenguera A, Rodriguez-Blanco T, Epstein RM. Effectiveness of a mindfulness education program in primary health care professionals: a pragmatic controlled trial. J Contin Educ Health Prof. 2014;34(1):4–12. doi: 10.1002/chp.21211. [DOI] [PubMed] [Google Scholar]
- 16.Barene S, Krustrup P, Brekke OL, Holtermann A. Soccer and Zumba as health-promoting activities among female hospital employees: a 40-weeks cluster randomised intervention study. J Sports Sci. 2014;32(16):1539–1549. doi: 10.1080/02640414.2014.906043. [DOI] [PubMed] [Google Scholar]
- 17.Cheng ST, Tsui PK, Lam JH. Improving mental health in health care practitioners: randomized controlled trial of a gratitude intervention. J Consult Clin Psychol. 2015;83(1):177–186. doi: 10.1037/a0037895. [DOI] [PubMed] [Google Scholar]
- 18.Chesak SS, Bhagra A, Schroeder DR, Foy DA, Cutshall SM, Sood A. Enhancing resilience among new nurses: feasibility and efficacy of a pilot intervention. Ochsner J. 2015;15(1):38–44. http://search.ebscohost.com/login.aspx?direct=true&db=cmedm&AN=25829879&site=ehost-live. Accessed August 28, 2019. [PMC free article] [PubMed] [Google Scholar]
- 19.Doran K, Resnick B, Zhu S, Alghzawi H. Testing the impact of the worksite heart health improvement project on cardiovascular disease risk factors over time. J Occup Environ Med. 2018;60(8):717–723. doi: 10.1097/JOM.0000000000001304. [DOI] [PubMed] [Google Scholar]
- 20.Duchemin AM, Steinberg BA, Marks DR, Vanover K, Klatt M. A small randomized pilot study of a workplace mindfulness-based intervention for surgical intensive care unit personnel: effects on salivary alpha-amylase levels. J Occup Environ Med. 2015;57(4):393–399. doi: 10.1097/JOM.0000000000000371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dyrbye LN, West CP, Richards ML, Ross HJ, Satele D, Shanafelt TD. A randomized, controlled study of an online intervention to promote job satisfaction and well-being among physicians. Burn Res. 2016;3(3):69–75. doi: 10.1016/j.burn.2016.06.002. [DOI] [Google Scholar]
- 22.Fang R, Li X. A regular yoga intervention for staff nurse sleep quality and work stress: a randomised controlled trial. J Clin Nurs. 2015;24(23–24):3374–3379. doi: 10.1111/jocn.12983. [DOI] [PubMed] [Google Scholar]
- 23.Hersch RK, Cook RF, Deitz DK, et al. Reducing nurses’ stress: a randomized controlled trial of a web-based stress management program for nurses. Appl Nurs Res. 2016;32:18–25. doi: 10.1016/j.apnr.2016.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jakobsen MD, Sundstrup E, Brandt M, Jay K, Aagaard P, Andersen LL. Physical exercise at the workplace reduces perceived physical exertion during healthcare work: cluster randomized controlled trial. Scand J Public Health. 2015;43(7):713–720. doi: 10.1177/1403494815590936. [DOI] [PubMed] [Google Scholar]
- 25.Ketelaar SM, Gartner FR, Bolier L, Smeets O, Nieuwenhuijsen K, Sluiter JK. Mental vitality @ work—a workers’ health surveillance mental module for nurses and allied health care professionals: process evaluation of a randomized controlled trial. J Occup Environ Med. 2013;55(5):563–571. doi: 10.1097/JOM.0b013e318289ee3e. [DOI] [PubMed] [Google Scholar]
- 26.Leedo E, Beck AM, Astrup A, Lassen AD. The effectiveness of healthy meals at work on reaction time, mood and dietary intake: a randomised cross-over study in daytime and shift workers at an university hospital. Br J Nutr. 2017;118(2):121–129. doi: 10.1017/S000711451700191X. [DOI] [PubMed] [Google Scholar]
- 27.Linzer M, Poplau S, Grossman E, et al. A cluster randomized trial of interventions to improve work conditions and clinician burnout in primary care: results from the healthy work place (HWP) study. J Gen Intern Med. 2015;30(8):1105–1111. doi: 10.1007/s11606-015-3235-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Low V, Gebhart B, Reich C. Effects of a worksite program to improve the cardiovascular health of female health care workers. J Cardiopulm Rehabil Prev. 2015;35(5):342–347. doi:0.1097/HCR.0000000000000116. [DOI] [PubMed] [Google Scholar]
- 29.Luthar SS, Curlee A, Tye SJ, Engelman JC, Stonnington CM. Fostering resilience in healthcare professionals who are also moms. AACN Bold Voices. 2017;9(8):20–20. http://search.ebscohost.com/login.aspx?direct=true&db=rzh&AN=124182680&site=ehost-live. Accessed August 28, 2019. [Google Scholar]
- 30.Matsugaki R, Kuhara S, Saeki S, et al. Effectiveness of workplace exercise supervised by a physical therapist among nurses conducting shift work: a randomized controlled trial. J Occup Health. 2017;59(4):327–335. doi: 10.1539/joh.16-0125-OA. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mealer M, Conrad D, Evans J, et al. Feasibility and acceptability of a resilience training program for intensive care unit nurses. Am J Crit Care. 2014;23(6):e97–105. doi: 10.4037/ajcc2014747. [DOI] [PubMed] [Google Scholar]
- 32.Mistretta EG, Davis MC, Temkit M, Lorenz C, Darby B, Stonnington CM. Resilience training for work-related stress among health care workers: results of a randomized clinical trial comparing in-person and smartphone-delivered interventions. J Occup Environ Med. 2018;60(6):559–568. doi: 10.1097/JOM.0000000000001285. [DOI] [PubMed] [Google Scholar]
- 33.Moody K, Kramer D, Santizo RO, et al. Helping the helpers: mindfulness training for burnout in pediatric oncology—a pilot program. J Pediatr Oncol Nurs. 2013;30(5):275–284. doi: 10.1177/1043454213504497. [DOI] [PubMed] [Google Scholar]
- 34.Pipe TB, Bortz JJ, Dueck A, Pendergast D, Buchda V, Summers J. Nurse leader mindfulness meditation program for stress management: a randomized controlled trial. J Nurs Adm. 2009;39(3):130–137. doi: 10.1097/NNA.0b013e31819894a0. [DOI] [PubMed] [Google Scholar]
- 35.Querstret D, Cropley M, Fife-Schaw C. Internet-based instructorled mindfulness for work-related rumination, fatigue, and sleep: assessing facets of mindfulness as mechanisms of change. A randomized waitlist control trial. J Occup Health Psychol. 2017;22(2):153–169. doi: 10.1037/ocp0000028. [DOI] [PubMed] [Google Scholar]
- 36.Schroeder DA, Stephens E, Colgan D, Hunsinger M, Rubin D, Christopher MS. A brief mindfulness-based intervention for primary care physicians: a pilot randomized controlled trial. Am J Lifestyle Med. 2016;12(1):83–91. doi: 10.1177/1559827616629121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sood A, Prasad K, Schroeder D, Varkey P. Stress management and resilience training among department of medicine faculty: a pilot randomized clinical trial. J Gen Intern Med. 2011;26(8):858–861. doi: 10.1007/s11606-011-1640-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sood A, Sharma V, Schroeder DR, Gorman B. Stress management and resiliency training (SMART) program among department of radiology faculty: a pilot randomized clinical trial. Explore (NY). 2014;10(6):358–363. doi: 10.1016/j.explore.2014.08.002. [DOI] [PubMed] [Google Scholar]
- 39.Steinberg BA, Klatt M, Duchemin AM. Feasibility of a mindfulness-based intervention for surgical intensive care unit personnel. Am J Crit Care. 2016;26(1):10–18. http://search.ebscohost.com/login.aspx?direct=true&db=cmedm&AN=27965223&site=ehost-live. Accessed August 28, 2019. [DOI] [PubMed] [Google Scholar]
- 40.Tucker S, Farrington M, Lanningham-Foster LM, et al. Worksite physical activity intervention for ambulatory clinic nursing staff. Workplace Health Saf. 2016;64(7):313–325. doi: 10.1177/2165079916633225. [DOI] [PubMed] [Google Scholar]
- 41.Valley MA, Stallones L. Effect of mindfulness-based stress reduction training on health care worker safety: a randomized waitlist controlled trial. J Occup Environ Med. 2017;59(10):935–941. doi: 10.1097/JOM.0000000000001090. [DOI] [PubMed] [Google Scholar]
- 42.West CP, Dyrbye LN, Rabatin JT, et al. Intervention to promote physician well-being, job satisfaction, and professionalism: a randomized clinical trial. JAMA Intern Med. 2014;174(4):527–533. doi: 10.1001/jamainternmed.2013.14387. [DOI] [PubMed] [Google Scholar]
- 43.Sampson M, Melnyk BM, Hoying J. The MINDBODYSTRONG intervention for new nurse residents: 6 month effects on mental health outcomes, healthy lifestyle behaviors and job satisfaction. Worldviews Evid Based Nurs. 2020;17(1):16–23. doi: 10.1111/wvn.12411 [DOI] [PubMed] [Google Scholar]
- 44.Sampson M, Melnyk BM, Hoying J. Intervention Effects of the MINDBODYSTRONG© Cognitive Behavioral Skills Building Program on newly licensed registered nurses’ mental health, healthy lifestyle beliefs and job satisfaction. J Nurs Adm. 2019;49(10):487–495 doi: 10.1097/NNA.0000000000000792 [DOI] [PubMed] [Google Scholar]
- 45.Schünemann H, Brozek J, Guyatt G, Oxman A. GRADE Handbook. https://gdt.gradepro.org/app/handbook/handbook.html#h.hnedbo8gqjqk. Updated October 13, 2013. Accessed April 12, 2019.
- 46.Guyatt GH, Oxman AD, Kunz R, Vist GE, Falch Ytter Y, Schünemann HJ. GRADE: what is ‘quality of evidence’ and why is it important to clinicians. Br Med J. 2008;336:924–926.18436948 [Google Scholar]
- 47.Melnyk BM, Szalacha LA, Amaya M. Psychometric properties of the perceived wellness culture and environment support scale. Am H Health Promot. 2018;32(4):1021–1027. [DOI] [PubMed] [Google Scholar]
- 48.Melnyk BM, Gascon GM, Amaya M, Mehta LS. A comprehensive approach to university wellness emphasizing Million Hearts demonstrates improvement in population cardiovascular risk. Build Healthy Acad Communit J. In Press. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.