Abstract
Previous neuroimaging studies have demonstrated that sleep is associated with brain functional changes in some specific brain regions. However, few studies have examined the relationship between all possible functional connectivities (FCs) within the sensory/somatomotor network (SSN) and the sleep quality of young male samples. The SSN consists of two motor cortices and is known to play a critical role in sleep. Poor sleep quality may be associated with increased sensory/somatomotor functional connectivity during rest. Hence, 202 young male participants underwent a resting-state functional magnetic resonance imaging (fMRI) scan and completed the Pittsburgh Sleep Quality Index (PSQI). Results indicated that increased functional connectivity within the SSN was associated with poor sleep quality. Specifically, the total PSQI score was positively correlated with the increased functional connectivity of the left paracentral lobule (PCL), bilateral precentral gyrus (PreCG), supplementary motor area (SMA) and bilateral postcentral gyrus (PoCG). Additionally, our findings also exhibited that (a) the subjective sleep quality factor of PSQI was positively correlated with FC between the bilateral PoCG and the bilateral PCL as well as between the left PreCG and the right SMA; (b) the sleep latency factor of PSQI was positively correlated with FC between the left PoCG and the right precuneus (PCUN); (c) the sleep disturbances factor of PSQI was positively correlated with FC between the left PCL and the right PoCG, and (d) the daytime dysfunction factor of PSQI was positively correlated with FC between the bilateral PoCG and the left PCL as well as between the bilateral PreCG and the SMA. In short, our findings can be comprehensively understood as neural mechanisms of intrinsic SSN connectivity are associated with sleep quality of man. Meanwhile, it may expand our knowledge and provide new insight into a deeper understanding of the neurobiological mechanisms of sleep or sleep problems.
Keywords: Sleep quality, Functional connectivity, Sensory/somatomotor network, Male
Introduction
Insufficient sleep was associated with negative affect, poor academic performance, suicidal behavior (Becker et al., 2018; Lee et al., 2015), and cognitive decline (Mah et al., 2018). Recently, one study demonstrated that 46% of participants rated their sleep quality as quite bad or very bad (Norbury & Evans, 2019). Several studies also indicated that 25.7% of college students had sleep problems (Cao et al., 2017; Huang et al., 2020; Jiang et al., 2015; Li et al., 2018). It could be seen that poor sleep quality was widespreadly problematic among college students.
Particularly, gender differences in sleep quality were the focus of relevant studies. Some studies found that gender differences caused males and females to sleep differently, which might underlie the differential risk for sleep disorders (Krishnan and Collop, 2006; Mallampalli and Carter, 2014). There were also several studies reporting that sleep quality in males was worse than in their females counterparts (Berkout et al. 2011; Bixler et al., 2009; Mallampalli and Carter, 2014; Okano et al., 2019). More importantly, insufficient sleep was significantly associated with an increased risk of suicide (Ferentinos et al., 2016; Gelaye et al., 2016). Studies also found that males were 4 to 7 times more likely to commit suicide than females (Courtenay, 2000). Furthermore, relative to females, male students might face more financial and social pressures in Chinese society (Zhai et al., 2018). However, to our best knowledge, there were few studies to address this issue in male samples until now. Therefore, it was essential to pay more attention to the sleep quality of man.
Of note, sleep was thought to play a critical and specific role in brain development and function (Bootzin & Epstein, 2011; Colrain, 2011; Riemann et al., 2010). Many previous studies examining the neural substrates of sleep have used neuroimaging techniques to identify regions associated with sleep quality. For instance, Killgore et al. (2013) showed that difficulty in falling asleep was associated with increased FC between the primary visual cortex and the SMA. Cheng et al. (2018) also observed that poor sleep quality was significantly positively associated with functional connectivity in specific regions. These specific regions included PreCG, PCL, PCUN, SMA, and PoCG. The PreCG might be associated with high sensitivity during the falling asleep period. Liu et al. (2015) also revealed that the left cerebellum posterior lobe showed FC with the left PreCG and left PCUN after sleep deprivation. Moreover, the PoCG was a main receptive region for external stimuli, which was located in the somatosensory network (Sung et al., 2020). Previous studies found that primary insomnia patients showed a significant reduction in left PreCG, and bilateral PoCG compared to normal controls (DelRosso & Hoque, 2014). Kong et al. (2018) suggested that sleep deprivation had significantly increased functional connectivity density in the right PCL, bilateral PreCG, and PoCG. The above relevant studies suggested that the brain regions (i.e., the PCL, PreCG, PoCG, and SMA) were related to sleep quality.
Noteworthy, these brain subregions were known as the constitutes of the SSN. The SSN consisted of two motor cortices and was known to play a critical role in sleep. According to the hyperarousal theory of insomnia, it was pointed out that difficulty in falling asleep or maintaining sleep occurred as a result of increased cognitive and physiological arousal caused by acute stressors and associated cognitive rumination (Perlis et al., 1997). The central feature of this theory involved increased sensory processing that interfered with the initiation and maintenance of sleep (Riemann et al., 2010). Thus, we speculated that poor sleep quality might be associated with possible changes within the SSN. Although accumulated neuroimaging studies have explored neural markers related to sleep problems (e.g., sleep deprivation) (Cheng et al., 2018; Kong et al., 2018; Li et al., 2015; Liu et al., 2015; Londei et al., 2010; Wang et al., 2021; Zhang et al., 2020a, b), little is known about the relationship between the intrinsic functional connectivity of the brain regions within SSN and sleep quality of man. Therefore, the current study intended to continue to investigate the relationship between the rsFC of the brain regions within SSN and males sleep quality.
Resting-state functional connectivity (rsFC), emerged as an important approach to study the neural mechanisms underlying sleep-related, analyzed that the temporal correlations of spontaneous low-frequency blood oxygen level-dependent signal fluctuations that were not attributable to specific inputs and outputs in different brain regions (Fox & Raichle, 2007; Fransson, 2005; Horwitz et al., 2005; Jiang et al., 2011; Liu et al., 2015). Previous studies demonstrated that the rsFC for the region of interest (ROI) had a high degree of test-retest reliability (Curtis et al., 2016; Shehzad et al., 2009; Zuo et al., 2010). Thus, the present study utilized the rsFC approach and set the regions of the SSN as the seed regions to examine whether the strength in rsFC between the seed regions and other SSN regions related to sleep quality in males. Moreover, to evaluate the sleep quality of college students, the PSQI had been widely recognized as a reliable research instrument in this field (Buysse et al., 1989; Mollayeva et al., 2016; Neumann et al., 2020). Meanwhile, in our study, sleep quality was assessed by the PSQI, which had seven subcomponents (i.e., subjective sleep quality, sleep latency, sleep duration, sleep efficiency, sleep disturbance, daytime dysfunctions, and use of sleep medication) (Buysse et al., 1989).
In summary, first, several studies demonstrated the sleep quality was associated with changes in some specific brain regions involved the SSN (Cheng et al., 2018; Kong et al., 2018; Liu et al., 2015; Wang et al., 2021; Zhang et al., 2020a, b). To date, few studies had comprehensively explored the relationship between all possible FCs within the SSN and the sleep quality among young male samples. Second, numerous studies had only examined total sleep or specific sleep components (Li et al., 2015; Zhang et al., 2020a, b). It could be possible that significant sleep quality-FC associations in these studies were driven by one of these sub-components (e.g., sleep disturbance). Finally, little was known about the neural mechanisms of male sleep quality. Therefore, the purpose of the current study was to investigate the relationship between the intrinsic rsFC of the brain regions within SSN and the sleep quality of man. We hypothesized that the sleep quality of man might be associated with the rsFC of regions within the SSN. Exploring associations between sleep quality and intrinsic FC of the brain regions within SSN might expand our knowledge and provide new insight into a deeper understanding of underlying neural mechanisms related to male sleep or sleep disorders.
Methods
Participants
A cohort of 202 male college students (ranging from 17 to 27 years of age, mean age =19.83 years, SD = 1.32) was recruited by posting advertisements. All participants volunteered to complete the MRI scans and the PSQI scale. All subjects were right-handed, with normal vision or corrected vision. None of the participants had a history of neurological, psychiatric diseases, substance abuse, medical disorders, or nicotine/alcohol. Our data was collected before COVID-19, so it could not be affected by major pandemic related restrictions. This study was approved by the Institutional Human Participants Review Board of the Southwest University Imaging Center for Brain Research, and the protocol was approved by the Ethics Committee of Southwest University, Chongqing. Each participant provided written informed consent before the study.
Behavioral assessment
All participants’ sleep quality was assessed by the PSQI (Cronbach’s α = 0.83) (Buysse et al., 1989; Carter et al., 2017). The PSQI was an appropriate instrument to measure sleep quality and sleep patterns among college students (Lund et al., 2010). The PSQI consists of a 19-item questionnaire and intends to measure sleep quality and disturbance over the past month. The 19 items measure seven factors. Each factor score is weighted equally on a 0–3, with lower scores indicating no problems and higher scores indicating gradually worsening problems as follows: (1) Subjective sleep quality: Self-reported satisfaction with sleep quality in the past month. The higher the score, the more dissatisfied the subject felt. (2) Sleep latency: the higher score signifies a more prolonged time required for falling asleep after going to bed. (3) Sleep duration: the higher score shows the shorter sleep duration. (4) Sleep efficiency: the higher score shows the lower efficiency. (5) Sleep disturbances: the higher score shows the more severe disturbance. (6) Use of sleep medication: the higher score represents a more frequent requirement. (7) Daytime dysfunction: the higher score shows the more problems one encounters when engaging in daily activities (e.g., staying awake while driving, or participating in social activities (Buysse et al., 1989; Lin et al., 2019). The seven component scores are added together to get a total PSQI score with a range of 0 to 21, with the higher score indicating the worse sleep quality. A total score of greater than 5 is an indicator of poor sleep quality. The PSQI scale has high sensitivity (89.6%) and specificity (86.5%) in assessing sleep quality (Buysse et al., 1989).
MRI data acquisition
All the data were collected from the Southwest University Center for Brain Imaging using a 3.0-T Siemens Trio MRI scanner (Siemens Medical, Erlangen, Germany) (Ran et al., 2017). During the resting-state MRI scanning, the subjects were instructed to lie down, close their eyes, rest without thinking about a particular thing, but not fall asleep. The 8-minute scan of 242 conterminous whole-brain resting-state functional images were obtained utilizing a gradient echo-planar imaging (EPI) sequence with the following parameters: repetition time = 2000 ms; slices = 32; echo time = 30 ms; thickness = 3 mm; resolution matrix = 64 × 64; flip angle = 90°; field of view = 220 × 220 mm2 ; slice gap = 1 mm; and voxel size = 3.4 × 3.4 × 4 mm3.
Imaging pre-processing
Image pre-processing was performed in the MATLAB 2014a (Math Works, Natick, MA) platform. All resting-state image data were analyzed using SPM8 (http://www.fil.ion.ucl.ac. uk/spm) and the Data Processing Assistant for resting-state software (DPARSF V3.2) (Yan et al., 2016; Zhang et al., 2020a, b). First, the first 10 EPI scans were discarded due to the environmental adaptation of subjects and the instability of the initial signal for each subject. Next, the T1 images were co-registered and segmented into the gray matter, white matter, and cerebrospinal fluid. Then, the remaining 232 images were preprocessed by slice timing, realigned, and normalized to a MNI (Montreal Neurological Institute) template and resampled to 3 × 3 × 3 mm3. Subsequently, the cerebrospinal fluid signal, white matter signal, global signal, and the Friston 24-parameter model (Friston et al., 1996) were regressed to cancel out the potential impact of physiological artifacts. During the image preprocessing, the scrubbing procedure was conducted according to the method of Power et al. (2012). Finally, the data were smoothed with a 6 mm full width at half maximum (FWHM) Gaussian kernel. The smoothed images were filtered using a band pass (0.01-0.1HZ) to decrease the influence of low-frequency fluctuation and high-frequency noise. The pre-processing of resting-state images was similar to the process in previous work (He et al., 2020; Zhang et al., 2020a, b).
Functional connectivity analysis
Functional connectivity was investigated using a region of interest (ROI) based method performed in the Resting-State fMRI Data Analysis Toolkit (REST) software package (Song et al., 2016). To generate the functional connectivity, a 264-functional-node template defined by Power was used (Power et al., 2011). This template accurately divides nodes into communities to enable us to investigate canonical functional networks. Moreover, the homogeneity of the nodes is better than most parcellations (Gordon et al., 2016), and this template has been widely used in FC studies (Doré et al., 2019; Zhang et al., 2020a, b). Therefore, considering the above advantages we selected the Power-264 template. Power 264 functional ROIs was composed of 14 functional networks including sensory/somatomotor hand, sensory/somatomotor mouth, cingulo-opercular task control, auditory, default mode, memory retrieval, ventral attention, visual, frontoparietal task control, salience, subcortical, cerebellar, dorsal attention, and uncertain (He et al., 2020). Previous fMRI studies demonstrated that sleep quality was significantly correlated with the PCUN, PoCG, SMA, PreCG, and PCL (Cheng et al., 2018; Liu et al., 2015). These regions could be reflected in a large-scale SSN. According to these findings, the present study selected the SSN as the network-of-interest and concerned functional connectivities within this network. 28 regions belonging to the SSN were selected to build the functional connectivity, established a 28 × 27 correlation matrix according to the 264-template of Power (Power et al., 2011), and obtained 12 significantly related functional connectivities.
Statistical analysis
The data were analyzed using IBM SPSS statistical package, version 23 (IBM Corp., Armonk, N.Y., USA). An analysis of variance with the factors “age” on total PSQI scores was performed. Meanwhile, the Pearson’ s correlation and the multiple regression analysis were performed with SPSS23.0 to test linear relationships between sleep quality and the FC within SSN. Additionally, because the number of comparisons (i.e., > 100) was high, the result may have multiple testing problems (Benjamini & Hochberg, 1995). To avoid this issue, we used the Benjamini-Hochberg procedure to adjust the false discovery rate (FDR) and report correlation along with FDR-adjusted p-values in our analysis.
Results
Behavioral results
The mean, Min, Max, and standard deviation (SD) for each PSQI factor score and the total PSQI score were presented in Table 1. The mean age of participants was 19.83 (SD = 1.32). The distribution of the participants’ age was shown in Fig. 1. An analysis of variance indicated no significant age differences in PSQI scores (F = 2.601, p > 0.01).
Table 1.
The mean, Min, Max, standard deviation (SD), scores for each PSQI factor, and the total PSQI score.
| measure | N | Mean | Min | Max | SD |
|---|---|---|---|---|---|
| age | 202 | 19.83 | 17 | 27 | 1.32 |
| the subjective sleep quality factor | 202 | 1.04 | 0 | 3 | 0.69 |
| sleep latency factor | 202 | 1.20 | 0 | 3 | 0.97 |
| sleep duration factor | 202 | 1.08 | 0 | 3 | 0.78 |
| sleep efficiency factor | 202 | 0.25 | 0 | 3 | 0.58 |
| sleep disturbance factor | 202 | 0.97 | 0 | 2 | 0.39 |
| use of sleep medication factor | 202 | 0.03 | 0 | 3 | 0.26 |
| daytime dysfunctions factor | 202 | 1.43 | 0 | 3 | 0.82 |
| Total PSQI | 202 | 6.00 | 0 | 16 | 2.75 |
N: Number: SD: standard deviation, PSQI: Pittsburgh Sleep Quality Index.
Fig. 1.

The distribution of the participants’ age.
Relationship between the functional connectivity within SSN and the total PSQI score
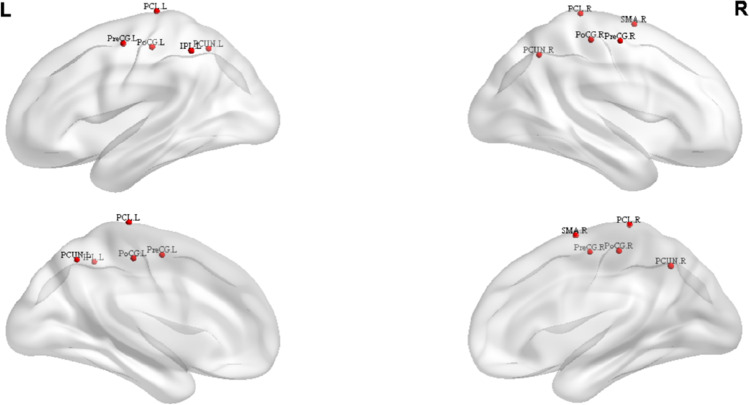
First, we performed the correlation analysis and the multiple regression analysis to explore the relationship between the SSN and the total PSQI score among young male samples, revealing a positive correlation between the SSN and the global PSQI score (β = 0.143, t = 2.041, p < 0.05). The results were visualized with BrainNet Viewer (Xia et al., 2013). Visual inspection was shown in Fig. 2. Subsequently, further rsFC analysis indicated 12 significant links after controlling age, and these correlated links involved the PCL, the inferior paracentral lobule (IPL), the PreCG, the PCUN, PoCG, and SMA. The multiple regression analysis showed the positive correlation between the total PSQI score and the mean strength of significant functional connectivity (β = 0.246, t = 3.586, p < 0.001) (See Fig. 3), indicating that the higher PSQI score showed the stronger functional connectivity within SSN.
Fig. 2.
The brain regions showed all the nodes within the SSN which were associated with the PSQI score. These regions (red hot colored area) included right paracentral lobule (PCL.R), the right precentral gyrus (PreCG.R), the right postcentral gyrus (PoCG.R), the right precuneus (PCUN.R), the right supplementary motor area (SMA.R), the left paracentral lobule (PCL.L), the left precentral gyrus (PreCG.L), left postcentral gyrus (PoCG.L), the left precuneus (PCUN.L) and the left inferior paracentral lobule (IPL.L).
Fig. 3.
The functional connectivity of the brain regions (PCL. L, PCL. R, SMA. R, PoCG. L, PoCG. R, PreCG. L, PreCG. R, PCUN. L, PCUN. R, IPL. L, color red) within SSN and its correlation with PSQI score.
Specifically, the results revealed that the total PSQI scores was positively correlated with the strength of rsFC between the right SMA and the bilateral PreCG (p < 0.05). The total PSQI score was positively correlated with the strength of rsFC in left PoCG - bilateral PCL and in left PreCG-bilateral PCL (p < 0.05). The correlations of these rsFC with the total PSQI score were still significant, including the PoCG and IPL (left PoCG with bilateral PCUN, p < 0.05; left PoCG with right SMA, p < 0.05; right PoCG with left PCL, p < 0.05; right PoCG with left IPL, p < 0.05). Table 2 showed that the 12 functional connectivities were related to the total PSQI score, including regions, correlation coefficient (r), and p values. No other significant results were identified by this multiple regression analysis.
Table 2.
Functional connectivity of nodes links correlated with the total PSQI score.
| Region 1 | Region 2 | r | p(corrected) |
|---|---|---|---|
| PCL (L) | PoCG (L) | 0.189 | 0.025 |
| PCL (L) | PreCG (L) | 0.151 | 0.043 |
| SMA (R) | IPL (L) | 0.143 | 0.047 |
| PoCG (R) | IPL (L) | 0.139 | 0.049 |
| PreCG (R) | SMA (R) | 0.141 | 0.048 |
| PreCG (L) | SMA (R) | 0.185 | 0.025 |
| PreCG (L) | PCL (R) | 0.146 | 0.043 |
| PoCG (L) | PCUN (R) | 0.157 | 0.043 |
| PoCG (L) | PCL (R) | 0.204 | 0.025 |
| PoCG (L) | SMA (R) | 0.162 | 0.038 |
| PoCG (L) | PCUN (L) | 0.163 | 0.038 |
| PoCG (R) | PCL (L) | 0.140 | 0.043 |
Relationship between the rsFC within SSN and the sub-component of the PSQI score
Moreover, we further conducted the correlation analysis and the multiple regression analysis controlling for age to explore the relationship between the rsFC and sub-component scores. Our findings revealed that the subjective sleep quality factor was positively correlated with the strength of rsFC between the left PCL and bilateral PoCG as well as the left PreCG and right PCL (p < 0.05). The subjective sleep quality factor was positively correlated with the strength of rsFC in left PreCG- right SMA and right PCUN - left PoCG (p < 0.05). The specific results were shown in Table 3 and Fig. 4. The sleep disturbances factor score was positively correlated with the strength of rsFC in left PCL - right PoCG (p < 0.05) and left PCL-left PreCG (p < 0.05). The daytime dysfunction factor was positively related to the strength of rsFC in the left PCL - bilateral PoCG, the right PCL-left PoCG and the right SMA - bilateral PreCG. The sleep latency factor score was positively correlated with the strength of rsFC between the left PoCG and right PCUN (β = 0.146, t = 2.091, p < 0.05).
Table 3.
Functional connectivity of nodes links correlated with the sub-component of PSQI score
| The sub-component of PSQI | Region 1 | Region 2 | r | p(corrected) |
|---|---|---|---|---|
| the subjective sleep quality factor | PCL (L) | PoCG (L) | 0.151 | 0.043 |
| PCUN (R) | PoCG (L) | 0.190 | 0.025 | |
| PreCG (L) | PCL (R) | 0.195 | 0.025 | |
| PreCG (L) | SMA (R) | 0.249 | 0.000 | |
| PoCG (L) | PCL (R) | 0.183 | 0.025 | |
| PoCG (R) | PCL (L) | 0.167 | 0.038 | |
| sleep latency factor | PoCG (L) | PCUN (R) | 0.146 | 0.043 |
| sleep disturbances factor | PCL (L) | PoCG (R) | 0.164 | 0.038 |
| PCL (L) | PreCG (L) | 0.147 | 0.043 | |
| the daytime dysfunction factor | PCL (L) | PoCG (L) | 0.187 | 0.025 |
| PCL (L) | PoCG (R) | 0.192 | 0.025 | |
| PreCG (R) | SMA (R) | 0.188 | 0.025 | |
| PreCG (L) | SMA (R) | 0.148 | 0.043 | |
| PoCG (L) | PCL (R) | 0.173 | 0.035 |
Fig. 4.
The functional connectivity of the brain regions within SSN and its correlation with the sub-component of PSQI score. A: The correlations between the subjective sleep quality and the rsFC of regions (i.e., left PCL, left PoCG, right PCUN, left PreCG, right PCL, right PoCG, right SMA); B: The correlations between the sleep latency and the rsFC of regions (i.e., left PoCG, right PCUN); C: The correlations between the sleep disturbances and the rsFC of regions (i.e., left PCL, right PoCG, left PreCG); D: The correlations between the daytime dysfunction and the rsFC of regions (i.e., left PCL, left PoCG, right PoCG, left PreCG, right PreCG, right SMA, right PCL).
No other results were found in sleep duration, use of sleep medication, and habitual sleep efficiency factor.
Discussion
In the present study, we utilized resting-state functional connectivity analysis to investigate the intrinsic FC of brain regions within SSN associated with sleep quality among young male samples. The multiple regression analysis showed a positive correlation between the total PSQI score and the mean strength of significant functional connectivity. Our results suggested that the FC of the regions within the SSN was related to the sleep quality of man, which were generally consistent with our hypothesis. The specific FC of these important brain regions will be discussed in the following paragraphs.
Firstly, the current study has identified a positive correlation between the intrinsic SSN connectivity and the total PSQI score. The brain regions (i.e., PCUN, PCL, PreCG, PoCG, and SMA) involved in these intrinsic SSN connectivities had been identified as being parts of the SSN (Londei et al., 2010). This finding is in agreement with previous studies (Cheng et al., 2018; Huang et al., 2012; Killgore et al., 2013; Zhao et al., 2019). For instance, Cheng et al. (2018) reported that the FC between the PreCG and SMA was associated with the PSQI. In other words, the stronger FC might lead to poorer sleep quality. This was interpreted in the framework of the hyperarousal model of insomnia, which indicated that insomnia was associated with heightened arousal of the central nervous system (Killgore et al., 2013; Perlis et al., 1997; Riemann et al., 2010). Meanwhile, Killgore et al. (2013) found that difficulty in falling asleep was associated with increased FC between the primary visual cortex (i.e., cuneus) and other sensory regions such as the PreCG, the PCL and the SMA. One possible explanation was that the increased activity in the bilateral PreCG might be associated with high sensitivity during the falling asleep period. Based on the hyperarousal theory of insomnia, the greater functional connectivity among these sensory and motor activating regions could conceivably sustain arousal and enhance unwanted sensory awareness, resulting in difficulty falling asleep or awakening easily from sleep (Killgore et al., 2013; Nachev et al., 2008). Moreover, another study showed that the FCs between the anterolateral region and bilateral PreCG, SMA, PCL, PCUN, and PoCG changed more negatively after sleep deprivation (Zhao et al., 2019). Especially, we noted that the PoCG was the main receptive region for external stimuli as the location of the SSN. This region might generate an excessive hyperarousal state, which led to increased sensory information processing (Perlis et al., 2001). Thus, one possible speculation was that increased FC between the PoCG and the other regions might reflect their poor sleep quality.
Secondly, the current study mainly focused on the sleep quality of male samples and found that the FC of the brain regions within the SSN was related to male sleep quality. Recent studies had demonstrated that the SSN was the key brain network associated with sleep among male participants (Dai et al., 2012; Wang et al., 2021; Wu et al., 2021). For instance, Wang et al. (2021) analyzed whole-brain functional connectivity changes in the putamen and caudate nucleus as seed points in the neostriatum after 36 hours of complete sleep deprivation in healthy adult men by rs-fMRI. Results found that the left putamen had decreased FC in the bilateral PreCG and bilateral PoCG compared to individuals after sleep deprivation in the normal wakefulness state. At the same time, Wu et al. (2021) analyzed resting state alpha-band EEG and found that male sleep deprivation significantly reduced the alpha lagged linear connectivity in most cortical areas, especially in PCUN and PCL. The PCUN and PCL belonged to the parietal lobe, which was involved in a variety of complex functions and was critical for somato-motor processing (Zhang et al., 2020a, b). These reports were almost in line with those obtained in our study. Also, the male sleep deprivation showed significantly the higher regional homogeneity (ReHo) in the right PCL as compared with the female control group (Dai et al., 2012). The PCL was mainly located in the frontal lobe and the continued part of the PreCG and PoCG, which belonged to the area of SSN (Jung et al., 2017; Roy et al., 2009). Killgore et al.(2013) found that difficulty in maintaining sleep was associated with greater FC within SSN. The positive correlation between the increased rsFC of brain regions within SSN and the changes of sleep quality in males indicated that these rsFC might be neuromarkers for males sleep quality.
Finally, the sleep quality was measured by PSQI, which consisted of seven factors. Thus, it could be possible that sleep quality-FC associations in these studies were driven by one of these sub-factor (e.g., sleep disturbance). Our results indicated that the sub-component of PSQI was also positively correlated with the FC within SSN. In line with previous studies (Li et al., 2015; Londei et al., 2010), these regions mainly included the brain regions within SSN, such as the PoCG, PCL, PreCG, PCUN, and SMA. In total, these results might replicate functional connectivity related to the total PSQI score.
Additionally, several limitations may be mentioned. First, the available sleep-related data is restricted to the PSQI (Buysse et al., 1989), so there are no other questionnaires, polysomnography, or actigraphy data. Nevertheless, the PSQI is a widely used questionnaire with good psychometric properties that appropriately measures sleep quality in the nonclinical population (Hinz et al., 2017). Second, due to only male participants are evaluated, we cannot make generalizations to females. Thus, these results should be interpreted with caution. Meanwhile, considering that this study mainly focus on the young male samples, brain development and aging on sleep is relatively small. In future study should pay more attention to other the samples (i.e., the elderly, child) to comprehensively explore the relationship between functional connectivity and sleep. Finally, the present study indicates that the correlation between the SSN and the total PSQI score is relatively high (β = 0.143, t = 2.041, p < 0.05). However, this does not address the directionality of the association, which can be in both directions. We note that the causal relations between the FC and sleep are an important topic that deserves further exploration. Additionally, future research should combine network analysis to provide a more comprehensive view of the network.
To sum up, the strengths of this study are to investigate the FC within SSN related to male sleep, rather than evaluate the neural function of discrete brain regions. The FC within SSN is essential for many key cognitive functions (Lim and Dinges, 2010; Londei et al., 2010) and emotional reactivity (Goldin et al., 2009).
Conclusion
In conclusion, the present study investigated the associations between the sleep quality of man and the rsFC of brain regions within the SSN. It can be concluded from this study that man's sleep quality may depend on the rsFC within SSN involving PCL, PreCG, PoCG, and SMA. Subjects with poorer sleep quality appeared to show stronger rsFC between the nodes and border areas of the SSN. By discussing the rsFC of the brain regions within SSN, this study may expand our knowledge and provide new insight into a deeper understanding of the neurobiological mechanisms of male sleep or sleep problem.
Author contribution
Youling Bai and Jiawen Tan conducted the studies, Youling Bai, Jiawen, Xiaoyi Liu, and Xiaobing Cui collected and analyzed the data, Youling Bai, Jiawen Tan, Xiaoyi Liu, Xiaobing Cui, Dan Li, and Huazhan Yin prepared and revised the manuscript.
Funding
This work was supported by the Research Foundation of Education Bureau of Hunan Province, China (Grant No.18A029) and the Education Planning foundation of Hunan Province, China (Grant No. XJK20AXL01) and the Hunan social science achievement evaluation committee, china (Grant No.XSP22YBC047).
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Informed consent statement
All procedures followed were in accordance with the Helsinki Declaration of 1975, and the applicable revisions at the time of the investigation. Informed consent was obtained from all participants included in the study.
Consent to participate
Informed consent was obtained from all participants included in the study.
Consent for publication
Not applicable
Conflict of Interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Dan Li, Email: lidantina@163.com.
Huazhan Yin, Email: yhz1979@sina.com.
References
- Becker SP, Dvorsky MR, Holdaway AS, Luebbe AM. Sleep problems and suicidal behaviors in college students. Journal of Psychiatric Research. 2018;99:122–128. doi: 10.1016/j.jpsychires.2018.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. Journal of the Royal Statistical Society: Series B (Methodological) 1995;57(1):289–300. [Google Scholar]
- Berkout OV, Young JN, Gross AM. Mean girls and bad boys: Recent research on gender differences in conduct disorder. Aggression and Violent Behavior. 2011;16(6):503–511. doi: 10.1016/j.avb.2011.06.001. [DOI] [Google Scholar]
- Bixler, E. O., Papaliaga, M. N., Vgontzas, A. N., & LIN, H. M., Pejovic, S., Karataraki, M., & Chrousos, G. P. (2009). Women sleep objectively better than men and the sleep of young women is more resilient to external stressors: effects of age and menopause. Journal of Sleep Research, 18(2), 221–228. [DOI] [PMC free article] [PubMed]
- Bootzin RR, Epstein DR. Understanding and treating insomnia. Annual Review of Clinical Psychology. 2011;7:435–458. doi: 10.1146/annurev.clinpsy.3.022806.091516. [DOI] [PubMed] [Google Scholar]
- Buysse DJ, Reynolds CF, III, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Research. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- Cao XL, Wang SB, Zhong BL, Zhang L, Ungvari GS, Ng CH, Xiang YT. The prevalence of insomnia in the general population in China: A meta-analysis. PloS One. 2017;12(2):e0170772. doi: 10.1371/journal.pone.0170772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter B, Chopak-Foss J, Punungwe FB. An analysis of the sleep quality of undergraduate students. College Student Journal. 2017;50(3):315–322. [Google Scholar]
- Cheng W, Rolls ET, Ruan H, Feng J. Functional connectivities in the brain that mediate the association between depressive problems and sleep quality. JAMA Psychiatry. 2018;75(10):1052–1061. doi: 10.1001/jamapsychiatry.2018.1941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colrain IM. Sleep and the brain. Neuropsychology review. 2011;21(1):1–4. doi: 10.1007/s11065-011-9156-z. [DOI] [PubMed] [Google Scholar]
- Courtenay WH. Constructions of masculinity and their influence on men's well-being: a theory of gender and health. Social Science & Medicine. 2000;50(10):1385–1401. doi: 10.1016/S0277-9536(99)00390-1. [DOI] [PubMed] [Google Scholar]
- Curtis BJ, Williams PG, Jones CR, Anderson JS. Sleep duration and resting fMRI functional connectivity: examination of short sleepers with and without perceived daytime dysfunction. Brain and Behavior. 2016;6(12):e00576. doi: 10.1002/brb3.576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dai XJ, Gong HH, Wang YX, Zhou FQ, Min YJ, Zhao F, Xiao XZ. Gender differences in brain regional homogeneity of healthy subjects after normal sleep and after sleep deprivation: a resting-state fMRI study. Sleep Medicine. 2012;13(6):720–727. doi: 10.1016/j.sleep.2011.09.019. [DOI] [PubMed] [Google Scholar]
- DelRosso LM, Hoque R. The cerebellum and sleep. Neurologic Clinics. 2014;32(4):893–900. doi: 10.1016/j.ncl.2014.07.003. [DOI] [PubMed] [Google Scholar]
- Doré B, Scholz C, Baek E, Garcia J, O’Donnell M, Bassett D, Falk E. Brain activity tracks population information sharing by capturing consensus judgments of value. Cerebral Cortex. 2019;29:3102–3110. doi: 10.1093/cercor/bhy176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferentinos P, Porichi E, Christodoulou C, Dikeos D, Papageorgiou C, Douzenis A. Sleep disturbance as a proximal predictor of suicidal intent in recently hospitalized attempters. Sleep Medicine. 2016;19:1–7. doi: 10.1016/j.sleep.2015.10.021. [DOI] [PubMed] [Google Scholar]
- Fox MD, Raichle ME. Spontaneous fluctuations in brain activity observed with functional magnetic resonance imaging. Nature Reviews Neuroscience. 2007;8(9):700–711. doi: 10.1038/nrn2201. [DOI] [PubMed] [Google Scholar]
- Fransson P. Spontaneous low-frequency BOLD signal fluctuations: An fMRI investigation of the resting-state default mode of brain function hypothesis. Human Brain Mapping. 2005;26(1):15–29. doi: 10.1002/hbm.20113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friston KJ, Williams S, Howard R, Frackowiak RS, Turner R. Movement-related effects in fMRI time-series. Magnetic Resonance in Medicine. 1996;35(3):346–355. doi: 10.1002/mrm.1910350312. [DOI] [PubMed] [Google Scholar]
- Gelaye B, Okeiga J, Ayantoye I, Berhane HY, Berhane Y, Williams MA. Association of suicidal ideation with poor sleep quality among Ethiopian adults. Sleep and Breathing. 2016;20(4):1319–1326. doi: 10.1007/s11325-016-1418-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldin PR, Manber T, Hakimi S, Canli T, Gross JJ. Neural bases of social anxiety disorder: Emotional reactivity and cognitive regulation during social and physical threat. Archives of General Psychiatry. 2009;66(2):170–180. doi: 10.1001/archgenpsychiatry.2008.525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon EM, Laumann TO, Adeyemo B, Huckins JF, Kelley WM, Petersen SE. Generation and evaluation of a cortical area parcellation from resting-state correlations. Cerebral Cortex. 2016;26:288–303. doi: 10.1093/cercor/bhu239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He, L., Chen, G., Zheng, R., Hu, Y., Chen, X., & Ruan, J. (2020). Heterogeneous acupuncture effects of taixi (KI3) on functional connectivity in healthy youth and elder: a functional mri study using regional homogeneity and large-scale functional connectivity analysis. Neural Plasticity, 2020. [DOI] [PMC free article] [PubMed]
- Hinz A, Glaesmer H, Brähler E, Löffler M, Engel C, Enzenbach C, Sander C. Sleep quality in the general population: psychometric properties of the Pittsburgh Sleep Quality Index, derived from a German community sample of 9284 people. Sleep Medicine. 2017;30:57–63. doi: 10.1016/j.sleep.2016.03.008. [DOI] [PubMed] [Google Scholar]
- Horwitz B, Warner B, Fitzer J, Tagamets MA, Husain FT, Long TW. Investigating the neural basis for functional and effective connectivity. Application to fMRI. Philosophical Transactions of the Royal Society B: Biological Sciences. 2005;360(1457):1093–1108. doi: 10.1098/rstb.2005.1647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang Q, Li Y, Huang S, Qi J, Shao T, Chen X, Chen H. Smartphone use and sleep quality in Chinese college students: a preliminary study. Frontiers in Psychiatry. 2020;11:352. doi: 10.3389/fpsyt.2020.00352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang Z, Liang P, Jia X, Zhan S, Li N, Ding Y, Li K. Abnormal amygdala connectivity in patients with primary insomnia: evidence from resting state fMRI. European journal of Radiology. 2012;81(6):1288–1295. doi: 10.1016/j.ejrad.2011.03.029. [DOI] [PubMed] [Google Scholar]
- Jiang JH, Jung WH, Kang DH, Byun MS, Kwon SJ, Choi CH, Kwon JS. Increased default mode network connectivity associated with meditation. Neuroscience Letters. 2011;487(3):358–362. doi: 10.1016/j.neulet.2010.10.056. [DOI] [PubMed] [Google Scholar]
- Jiang XL, Zheng XY, Yang J, Ye CP, Chen YY, Zhang ZG, Xiao ZJ. A systematic review of studies on the prevalence of insomnia in university students. Public Health. 2015;129(12):1579–1584. doi: 10.1016/j.puhe.2015.07.030. [DOI] [PubMed] [Google Scholar]
- Jung ME, Colletta M, Coalson R, Schlaggar BL, Lieu JE. Differences in interregional brain connectivity in children with unilateral hearing loss. The Laryngoscope. 2017;127(11):2636–2645. doi: 10.1002/lary.26587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Killgore WD, Schwab ZJ, Kipman M, DelDonno SR, Weber M. Insomnia-related complaints correlate with functional connectivity between sensory–motor regions. Neuroreport. 2013;24(5):233–240. doi: 10.1097/WNR.0b013e32835edbdd. [DOI] [PubMed] [Google Scholar]
- Krishnan V, Collop NA. Gender differences in sleep disorders. Current Opinion in Pulmonary Medicine. 2006;12(6):383–389. doi: 10.1097/01.mcp.0000245705.69440.6a. [DOI] [PubMed] [Google Scholar]
- Kong D, Liu R, Song L, Zheng J, Zhang J, Chen W. Altered long-and short-range functional connectivity density in healthy subjects after sleep deprivations. Frontiers in Neurology. 2018;9:546. doi: 10.3389/fneur.2018.00546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee YJ, Park J, Kim S, Cho SJ, Kim SJ. Academic performance among adolescents with behaviorally induced insufficient sleep syndrome. Journal of Clinical Sleep Medicine. 2015;11(1):61–68. doi: 10.5664/jcsm.4368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li L, Wang YY, Wang SB, Zhang L, Li L, Xu DD, Xiang YT. Prevalence of sleep disturbances in Chinese university students: a comprehensive meta-analysis. Journal of Sleep Research. 2018;27(3):e12648. doi: 10.1111/jsr.12648. [DOI] [PubMed] [Google Scholar]
- Li HJ, Hou XH, Liu HH, Yue CL, Lu GM, Zuo XN. Putting age-related task activation into large-scale brain networks: a meta-analysis of 114 fMRI studies on healthy aging. Neuroscience & Biobehavioral Reviews. 2015;57:156–174. doi: 10.1016/j.neubiorev.2015.08.013. [DOI] [PubMed] [Google Scholar]
- Lim J, Dinges DF. A meta-analysis of the impact of short-term sleep deprivation on cognitive variables. Psychological Bulletin. 2010;136(3):375. doi: 10.1037/a0018883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin PH, Lee YC, Chen KL, Hsieh PL, Yang SY, Lin YL. The relationship between sleep quality and internet addiction among female college students. Frontiers in Neuroscience. 2019;13:599. doi: 10.3389/fnins.2019.00599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu X, Yan Z, Wang T, Yang X, Feng F, Fan L, Jiang J. Connectivity pattern differences bilaterally in the cerebellum posterior lobe in healthy subjects after normal sleep and sleep deprivation: a resting-state functional MRI study. Neuropsychiatric Disease and Treatment. 2015;11:1279. doi: 10.2147/NDT.S84204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Londei A, D'Ausilio A, Basso D, Sestieri C, Gratta CD, Romani GL, Belardinelli MO. Sensory-motor brain network connectivity for speech comprehension. Human Brain Mapping. 2010;31(4):567–580. doi: 10.1002/hbm.20888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lund HG, Reider BD, Whiting AB, Prichard JR. Sleep patterns and predictors of disturbed sleep in a large population of college students. Journal of Adolescent Health. 2010;46(2):124–132. doi: 10.1016/j.jadohealth.2009.06.016. [DOI] [PubMed] [Google Scholar]
- Mah CD, Kezirian EJ, Marcello BM, Dement WC. Poor sleep quality and insufficient sleep of a collegiate student-athlete population. Sleep health. 2018;4(3):251–257. doi: 10.1016/j.sleh.2018.02.005. [DOI] [PubMed] [Google Scholar]
- Mallampalli MP, Carter CL. Exploring sex and gender differences in sleep health: a Society for Women's Health Research Report. Journal of Women's Health. 2014;23(7):553–562. doi: 10.1089/jwh.2014.4816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mollayeva T, Thurairajah P, Burton K, Mollayeva S, Shapiro CM, Colantonio A. The Pittsburgh sleep quality index as a screening tool for sleep dysfunction in clinical and non-clinical samples: A systematic review and meta-analysis. Sleep Medicine Reviews. 2016;25:52–73. doi: 10.1016/j.smrv.2015.01.009. [DOI] [PubMed] [Google Scholar]
- Nachev P, Kennard C, Husain M. Functional role of the supplementary and pre-supplementary motor areas. Nature Reviews Neuroscience. 2008;9(11):856–869. doi: 10.1038/nrn2478. [DOI] [PubMed] [Google Scholar]
- Neumann N, Lotze M, Domin M. Sex-specific association of poor sleep quality with gray matter volume. Sleep. 2020;43(9):zsaa035. doi: 10.1093/sleep/zsaa035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norbury R, Evans S. Time to think: Subjective sleep quality, trait anxiety and university start time. Psychiatry Research. 2019;271:214–219. doi: 10.1016/j.psychres.2018.11.054. [DOI] [PubMed] [Google Scholar]
- Okano K, Kaczmarzyk JR, Dave N, Gabrieli JD, Grossman JC. Sleep quality, duration, and consistency are associated with better academic performance in college students. NPJ Science of Learning. 2019;4(1):1–5. doi: 10.1038/s41539-019-0055-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perlis ML, Giles DE, Mendelson WB, Bootzin RR, Wyatt JK. Psychophysiological insomnia: the behavioural model and a neurocognitive perspective. Journal of Sleep Research. 1997;6(3):179–188. doi: 10.1046/j.1365-2869.1997.00045.x. [DOI] [PubMed] [Google Scholar]
- Perlis ML, Merica H, Smith MT, Giles DE. Beta EEG activity and insomnia. Sleep Medicine Reviews. 2001;5(5):365–376. doi: 10.1053/smrv.2001.0151. [DOI] [PubMed] [Google Scholar]
- Power JD, Barnes KA, Snyder AZ, Schlaggar BL, Petersen SE. Spurious but systematic correlations in functional connectivity MRI networks arise from subject motion. Neuroimage. 2012;59(3):2142–2154. doi: 10.1016/j.neuroimage.2011.10.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Power JD, Cohen AL, Nelson SM, Wig GS, Barnes KA, Church JA, Schlaggar BL. Functional network organization of the human brain. Neuron. 2011;72:665–678. doi: 10.1016/j.neuron.2011.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ran Q, Yang J, Yang W, Wei D, Qiu J, Zhang D. The association between resting functional connectivity and dispositional optimism. PLoS One. 2017;12(7):e0180334. doi: 10.1371/journal.pone.0180334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riemann D, Spiegelhalder K, Feige B, Voderholzer U, Berger M, Perlis M, Nissen C. The hyperarousal model of insomnia: a review of the concept and its evidence. Sleep Medicine Reviews. 2010;14(1):19–31. doi: 10.1016/j.smrv.2009.04.002. [DOI] [PubMed] [Google Scholar]
- Roy, M., Piché, M., Chen, J. I., Peretz, I., & Rainville, P. (2009). Cerebral and spinal modulation of pain by emotions. Nature Precedings, 1–1. [DOI] [PMC free article] [PubMed]
- Shehzad Z, Kelly AC, Reiss PT, Gee DG, Gotimer K, Uddin LQ, Milham MP. The resting brain: unconstrained yet reliable. Cerebral Cortex. 2009;19(10):2209–2229. doi: 10.1093/cercor/bhn256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song Z, Scullin M, Park DC. Sleep quality is associated with functional connectivity of medial prefrontal cortex in healthy middle-aged adults. Alzheimer's & Dementia. 2016;12:39–40. [Google Scholar]
- Sung D, Park B, Kim SY, Kim BN, Park S, Jung KI, Park MH. Structural Alterations in Large-scale Brain networks and their Relationship with Sleep Disturbances in the Adolescent population. Scientific reports. 2020;10(1):1–9. doi: 10.1038/s41598-020-60692-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, H., Yu, K., Yang, T., Zeng, L., Li, J., Dai, C., et al. (2021). Altered functional connectivity in the resting state neostriatum after complete sleep deprivation: impairment of motor control and regulatory network. Frontiers in Neuroscience, 1045. [DOI] [PMC free article] [PubMed]
- Wu J, Zhou Q, Li J, Chen Y, Shao S, Xiao Y. Decreased resting-state alpha-band activation and functional connectivity after sleep deprivation. Scientific Reports. 2021;11(1):1–10. doi: 10.1038/s41598-020-79816-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xia M, Wang J, He Y. BrainNet Viewer: a network visualization tool for human brain connectomics. PloS One. 2013;8(7):e68910. doi: 10.1371/journal.pone.0068910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yan CG, Wang XD, Zuo XN, Zang YF. DPABI: data processing & analysis for (resting-state) brain imaging. Neuroinformatics. 2016;14(3):339–351. doi: 10.1007/s12021-016-9299-4. [DOI] [PubMed] [Google Scholar]
- Zhai K, Gao X, Wang G. The role of sleep quality in the psychological well-being of final year undergraduatestudents in China. International journal of environmental research and public health. 2018;15(12):2881. doi: 10.3390/ijerph15122881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang L, Li D, Yin H. How is psychological stress linked to sleep quality? The mediating role of functional connectivity between the sensory/somatomotor network and the cingulo-opercular control network. Brain and Cognition. 2020;146:105641. doi: 10.1016/j.bandc.2020.105641. [DOI] [PubMed] [Google Scholar]
- Zhang, R., Zhang, L., Wei, S., Wang, P., Jiang, X., Tang, Y., & Wang, F. (2020b). Increased Amygdala-paracentral lobule/precuneus functional connectivity associated with patients with mood disorder and suicidal behavior. Frontiers in Human Neuroscience, 14. [DOI] [PMC free article] [PubMed]
- Zhao R, Zhang X, Zhu Y, Fei N, Sun J, Liu P, Qin W. Disrupted resting-state functional connectivity in Hippocampal subregions after sleep deprivation. Neuroscience. 2019;398:37–54. doi: 10.1016/j.neuroscience.2018.11.049. [DOI] [PubMed] [Google Scholar]
- Zuo XN, Kelly C, Adelstein JS, Klein DF, Castellanos FX, Milham MP. Reliable intrinsic connectivity networks: test–retest evaluation using ICA and dual regression approach. Neuroimage. 2010;49(3):2163–2177. doi: 10.1016/j.neuroimage.2009.10.080. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.