In recent decades, numerous initiatives have been dedicated to assessing gender balance in the workplace. Evidence demonstrates that gender diversity is associated with better organization of daily work, continuing employment of exceptional workers, and higher institutional financial income [1, 2]. Furthermore, specifically in the healthcare system, gender balance has been associated with better clinical outcomes [3, 4].
However, despite these facts, there is still a large gap between careers of men and women in the public and private sectors, both in healthcare and non-healthcare systems [5]. This appears to also be the case in the field of nuclear medicine. To facilitate the involvement of women professionals in nuclear medicine and to encourage their active participation in the initiatives of the European Association of Nuclear Medicine (EANM), the Women Empowerment Task Force (WE-TF) was founded [6]. The WE-TF has two main goals: first, to increase networking among women in the field of nuclear medicine worldwide, and second, to provide a space for women to share their experiences regarding scientific, educational, and career development. Activities aiming to achieve these goals will be coordinated by the WE-TF team, supported by the EANM office.
The challenges encountered by the WE-TF were to first determine possible reasons for the underrepresentation of women in EANM activities, and second to understand the need to promote equal gender participation as perceived by the nuclear medicine community.
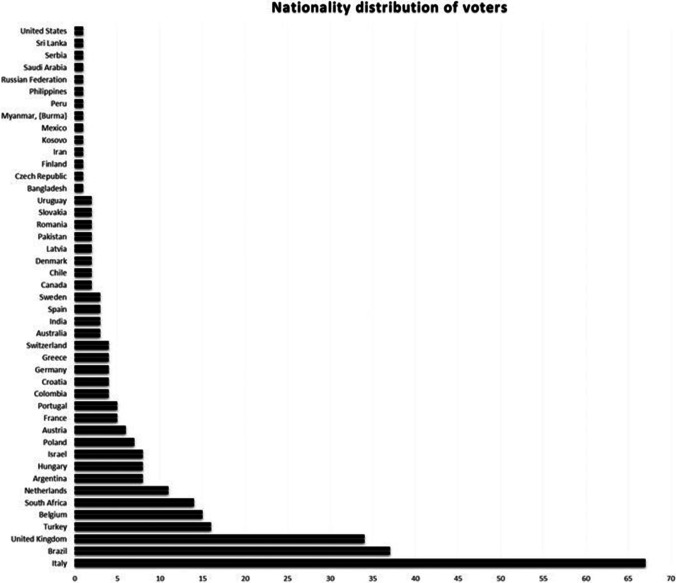
In order to obtain the above-mentioned information, an electronic prospective online survey was conducted. It was composed of 14 questions proposed and approved by the WE-TF members (Table 1), using the QuestionPro survey software. The link for the access to the questionnaire was sent electronically through the EANM newsletter, social media, and personal contacts, between November 4th and 29th 2021 to nuclear medicine professionals, both women and men, including physicians, technologists, radiochemists, and physicists. The online distribution process was facilitated by the EANM communication and publication team. The responses were collected anonymously. The following step was that of a detailed analysis of the replies to the questionnaires. Open questions were analyzed separately and categorized by four members of the TF. Gender data were analyzed as stated by the participants. Three hundred and three individuals participated in the survey, including 236 female and 53 male responders. An additional 14 participants did not disclose their gender. Participants came from 45 different countries, with the highest numbers from Italy, Brazil, UK, Turkey, Belgium, and South Africa (Fig. 1). In four cases, the data were incomplete and were excluded from the final analysis. Therefore, the final respondent group was 299 participants including 234 women, 52 men, and 13 with undisclosed gender. The studied group was heterogeneous with respect to age distribution and workplace of respondents.
Table 1.
Questions submitted in the survey
| Number of query (Q) | Content | Potential answers |
|---|---|---|
| Q1 | Do you feel women’s contribution to nuclear medicine could and should be more valued? |
a) No. If no, why? b) Yes c) I do not know |
| Q2* | In your opinion, what are the major areas in nuclear medicine in which women are undervalued? |
a) Scientific work/research b) Academic/university career c) Daily clinical practice d) international societies and organizations e) Other (please specify) |
| Q3 | What would you expect from the EANM Women´s EmpoWErment Task Force? | |
| Q4* | What do you perceive to be the challenges, if any, women are struggling with in their professional careers? |
a) Maintaining the work-life balance b) Being equally involved in professional collaborations and authorship c) Receiving funding for scientific/professional projects d) Missing professional support e) Lacking mental health support f) I do not see any challenges g) Other (please specify) |
| Q5* | If the WE Task Force would offer training opportunities, which form of training would you prefer the most? |
a) Topic related meetings during major events b) Virtual round-table discussions c) Mentoring webinars with experts d) Other (please specify) |
| Q6* | Which topics should be brought up during the training? |
a) Developing stronger leadership skills in clinical/scientific field (daily practice, projects) b) Group dynamics: how to successfully position oneself c) Scientific publications: how to successfully write, edit, submit, and interact with other authors, reviewers, editors e) Others (please specify) |
| Q7 | Your gender is: |
a) Female b) Male c) Other d) I would prefer not to say |
| Q8 | Where do you currently work? |
a) Region: Europe, Asia, Americas, Africa, Oceania b) Country: (dropdown) |
| Q9 | Where do you reside? |
a) Region: Europe, Asia, Americas, Africa, Oceania b) Country: (dropdown) |
| Q10 | Please indicate your age range: |
a) < 25 b) 25–38 c) 39–50 d) 51–60 e) > 60 |
| Q11* | Please let us know where you are currently working: |
a) Public institution b) University c) Private institution d) Many different medical units e) Other (please specify) |
| Q12 | What is your background? |
a) Medical Doctor b) Nurse/Technologist c) Radiopharmacist d) Medical Physicist e) Physician in training f) Scientist in training g) Other (please specify) |
| Q13* | What is your current position? |
a) Resident b) PhD student c) Assistant d) Professor e) Other (please specify) |
| Q14 | If you would like to stay in contact, please leave your email address: |
*Multiple answers were accepted
Fig. 1.
Distribution of the participant based on the country
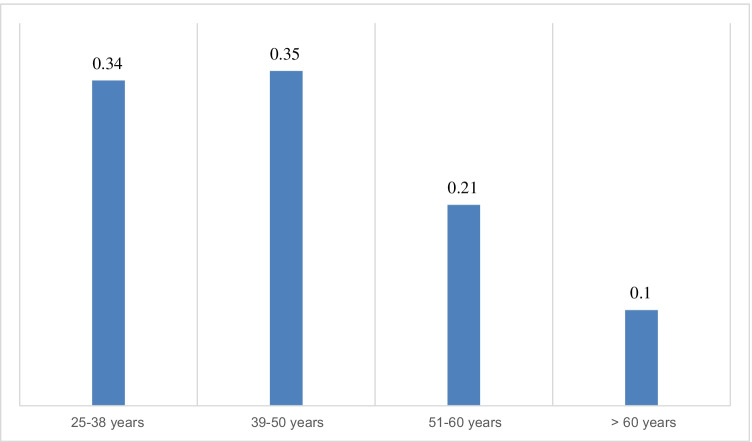
The following age groups were analyzed: 25–38 years, 39–50, 51–60, and above 60 years. Figure 2 shows the distribution of age among participants in the survey. Based on responders’ answers, the following sub-specialties were analyzed: physician, medical physicist/engineer, technologist/radiographer, and radiopharmacist/radiochemist. One nurse responded as well. The most significant group of participants consisted of physicians (67%). Technologists, physicists, and radiopharmacy professionals represented 17%, 10%, and 5% of respondents respectively.
Fig. 2.
Response rates based on age category
The following groups of professional positions were analyzed: senior professionals, including head of department, professor, specialist, and consultants, junior professionals, including assistants, residents, and trainees, students, including PhD students, as well as retired specialists. The largest group of respondents were senior professionals (63%), followed by 31% juniors, 4% students, and 2% retired personnel. Almost half of the responders (48%) work in public institutions, 25% in universities, and 21% for private healthcare providers, while 6% did not disclose their workplaces. Table 2 summarizes the distribution of the professional position and workplace for each age category of responders.
Table 2.
Gender- and age-based distribution of professional positions and workplace of questionnaire responders
| Women | Age category in years | ||||
|---|---|---|---|---|---|
| 25–38 | 39–50 | 51–60 | > 60 | ||
| All | 234 | 87 | 81 | 48 | 18 |
| Professional positions*, n (%) | |||||
|
Supervisor/head of department Professor Senior specialist/consultant Assistant/resident/trainee Student (including PhD students) Retired specialists |
18 (8) 36 (15) 95 (41) 73 (31) 17 (7) 2 (1) |
6 (7) 3 (3) 35 (40) 36 (41) 7 (8) 0 (0) |
4 (5) 13 (16) 37 (46) 23 (28) 10 (12) 0 (0) |
5 (10) 17 (35) 15 (31) 12 (25) 0 (0) 0 (0) |
3 (17) 3 (17) 8 (44) 2 (11) 0 (0) 2 (11) |
| Workplace*, n (%) | |||||
|
Public institutions University Private healthcare providers Other |
117 (50) 55 (24) 52 (22) 10 (4) |
30 (34) 28 (32) 26 (30) 3 (3) |
44 (54) 17 (21) 17 (21) 2 (2) |
31 (64) 7 (14) 7 (14) 5 (10) |
12 (67) 3 (17) 2 (11) 0 (0) |
*Multiple answers were accepted
In reply to Q1, 79% of the respondents agreed that women’s contribution to nuclear medicine should be more valued, 11% disagreed, and 10% were not sure how to reply.
In reply to Q2, 164 (55%) specified that the major area in nuclear medicine in which women are undervalued is the academic career, 143 (48%) specified involvement in international societies, 138 (46%) scientific work, and 27% the routine clinical practice, while 3% suggested other tasks such as editorial activities, and work opportunities.
In reply to Q4, most participants perceived maintaining the work-life balance (n = 218, 73%) as the main challenge women are struggling with their professional careers, 48% as being equally involved in professional collaborations, 29% funding for scientific/professional projects, 33% are missing professional support, and 20% lack of support for mental well-being. An additional 8% did not see any challenges and 3% mentioned other factors such as competition among women, maternity, and cultural country-based factors.
In reply to Q5, 52% of respondents opted for mentoring webinars run by experts as their preferred training opportunity, 27% opted for topic-related meeting during major events, 16% for virtual round-table discussions, and 5% for an online blog, chat groups, or workshops. According to age groups, the younger, below the age of 50 years, responders preferred mentoring webinars with experts, while participants above the age of 50 voted for topic-related meeting during major events.
In reply to Q6, 66% of participants chose developing stronger leadership skills in the clinical/scientific field as their preferred training topic, 53% voted for group dynamics on how to successfully position oneself, 50% how to successfully write, edit, submit, and interact with other authors, reviews, and editors regarding scientific publications, and 7% for other activities such as preparing and lecturing in meetings. Younger respondents preferred the development of leadership skills while participants 50 years or above chose mainly group dynamics.
One of the most thought-provoking parts of the survey was an open-end question (Q3) regarding expectations related to the WE-TF activities. Responses that could generate new ideas were sent along with very important comments by the participants. A high number of participants (40%) requested official actions by the EANM and other societies, through international collaborations. Approximately one in every 5 participants (19%) asked for support for women scientists in their academic careers and research. Other responses highlighted the need for improving leadership and management skills, implementing mentorship programs, or meeting with experts for support in clinical practice. Establishing a childcare unit during congresses was also suggested as an example on how to assist in achieving a balance between private life and work as a scientist. Beyond doubts, these answers provide a benchmark for future goals.
The number of women deciding to step into medical practice is constantly increasing [7–9]. Nevertheless, their representation in leadership positions is still low. Many generational, interpersonal, and societal factors may cause this imparity [10]. A good gender balance among professionals of different medical specialties is essential not only for a better representation of the overall demographics but also to ensure the delivery of high-quality routine clinical work as well as to encourage medical innovation [8]. Many barriers have to be faced. The first one, as emerged from the survey, is to maintain the work-life balance. Data based on previously published studies with similar surveys [11] show that women are less likely to share their struggles of balancing work and family life with their male colleagues. This is linked in part to difficult cultural stereotypes and to fear of being treated differently [11]. According to Quak et al. [12], the COVID-19 pandemic proved the numerous challenges that women experience in their professional as well as family life. Woitowich et al. also emphasized that these challenges became more apparent during pandemics [13]. While women are expected to share many responsibilities, their position is still underestimated. Being an excellent employee, creative scientist, and, at the same time, a loving mother and spouse should be highly appreciated, but the efforts women make to achieve these goals in all areas are often dismissed or not accepted at their real value.
The second barrier that has to be overcome is to increase the number of women in academic institutions. This gap persists over the years, as demonstrated by some authors [14]. The creation of specific national and international programs may have the potential to enhance the ability and motivation of women to advance in their careers and provide them with new opportunities [15].
The third barrier to be dealt with is to increase the involvement of women in scientific manuscript authorship. Women should be supported by promoting their active participation in research projects, subsequently leading to a consequent increase of their representation in authors’ panels. A recent study has demonstrated that a greater participation of female authors tends to produce more readable papers [16]. A report by Crowe et al. showed that in the Australia and New Zealand medical physics workforce the number of women who participated in authorship and editorial boards, as well as invited speakers in conferences, is lower as compared to men [17].
Finally, it is important to develop stronger leadership skills in the clinical and scientific field. Based on the systematic review of the literature, Fichera et al. demonstrate the limited role of women in mentorship as well as the relatively low number of female leaders in these areas [9].
How to overpass the above-mentioned obstacles is certainly a challenge. Some proposals to reach a more balanced representation at the workplace may include different approaches. Work schedules as well as events organized by professional associations such as the EANM should move towards respecting private time and facilitating remote access. The inclusion of women into decision-making groups is important. Initiatives and active policies towards greater visibility to the contribution of women in medicine and science, and specifically in nuclear medicine, to be promoted also by non-profit organizations, should be promoted to offer equal involvement opportunities for women in a wide scale of projects and leadership positions.
In the end, the authors realize that many of the items perceived and discussed may not be specific to women and be applicable to men trying to grow in their profession. Still we think that even independently they may be considered particularly relevant, as they reflect the experiences of female professionals in our field and provide areas for potential enablers in the context of the progress still to be made in all domains of our specialty for the empowerment of female colleagues at the benefit of all stakeholders involved.
Acknowledgements
This paper is a share effort of Laura Evangelista, Agata Pietrzak, Ozgul Ekmekcioglu, Petra Petranovic Ovcaricek, Ora Israel. The manuscript has been improved and approved by all authors. The authors are thankful to Silvia Marchetti and Catherine Friendly from EANM Office for their support in creating, diffusing, and collecting the survey’s data.
Declarations
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Conflict of interest
The authors declare no competing interests.
Informed consent
Informed consent was not required for the present study.
Footnotes
This article is part of the Topical Collection on Editorial
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Woetzel J. The power of parity: how advancing women’s equality can add $12 trillion to global growth. Work Pap. 2015 [cited 2022 Feb 6]; Available from: https://ideas.repec.org/p/ess/wpaper/id7570.html.
- 2.Reinventing the workplace for greater gender diversity | McKinsey. [cited 2022 Feb 6]. Available from: https://www.mckinsey.com/featured-insights/gender-equality/reinventing-the-workplace-for-greater-gender-diversity.
- 3.Tsugawa Y, Jena AB, Figueroa JF, Orav EJ, Blumenthal DM, Jha AK. Comparison of hospital mortality and readmission rates for Medicare patients treated by male vs female physicians. JAMA Intern Med. 2017 [cited 2022 Feb 6];177(2):206–13. Available from: https://pubmed.ncbi.nlm.nih.gov/27992617/. [DOI] [PMC free article] [PubMed]
- 4.Wallis CJ, Ravi B, Coburn N, Nam RK, Detsky AS, Satkunasivam R. Comparison of postoperative outcomes among patients treated by male and female surgeons: a population based matched cohort study. BMJ. 2017;10(359). 10.1136/bmj.j4366. [DOI] [PMC free article] [PubMed]
- 5.Gender diversity, a corporate performance driver | McKinsey. [cited 2022 Feb 6]. Available from: https://www.mckinsey.com/business-functions/people-and-organizational-performance/our-insights/gender-diversity-a-corporate-performance-driver.
- 6.Ekmekcioglu O, Evangelista L, Kunikowska J. Women in nuclear medicine. Eur J Nucl Med Mol Imaging. 2021 [cited 2022 Feb 6];48(9):2678–9. Available from: https://pubmed.ncbi.nlm.nih.gov/34032864/. [DOI] [PubMed]
- 7.Heiligers PJM, Hingstman L. Career preferences and the work-family balance in medicine: gender differences among medical specialists. Soc Sci Med. 2000 [cited 2022 Feb 6];50(9):1235–46. Available from: https://pubmed.ncbi.nlm.nih.gov/10728844/. [DOI] [PubMed]
- 8.Abdellatif W, Ding J, Jalal S, Nguyen T, Khorshed D, Rybicki FJ, et al. Lack of gender disparity among administrative leaders of Canadian health authorities. J Womens Health (Larchmt). 2020 [cited 2022 Feb 6];29(11):1469–74. Available from: https://pubmed.ncbi.nlm.nih.gov/32091966/. [DOI] [PubMed]
- 9.Fichera G, Busch IM, Rimondini M, Motta R, Giraudo C. Is empowerment of female radiologists still needed? Findings of a systematic review. Int J Environ Res Public Health. 2021 [cited 2022 Feb 6];18(4):1–16. Available from: https://pubmed.ncbi.nlm.nih.gov/33562881/. [DOI] [PMC free article] [PubMed]
- 10.Kubik-Huch RA, Vilgrain V, Krestin GP, Reiser MF, Attenberger UI, Muellner AU, et al. Women in radiology: gender diversity is not a metric-it is a tool for excellence. Eur Radiol. 2020 [cited 2022 Feb 6];30(3):1644–52. Available from: https://pubmed.ncbi.nlm.nih.gov/31802213/. [DOI] [PMC free article] [PubMed]
- 11.Brown JB, Fluit M, Lent B, Herbert C. Surgical culture in transition: gender matters and generation counts. Can J Surg. 2013 [cited 2022 Feb 6];56(3):153–8. Available from: https://pubmed.ncbi.nlm.nih.gov/23484466/. [DOI] [PMC free article] [PubMed]
- 12.Quak E, Girault G, Lasnon C. Can someone look after my children while I write this COVID-19 paper? Eur J Nucl Med Mol Imaging. 2021 [cited 2022 Feb 6];48(12):3751–2. Available from: https://pubmed.ncbi.nlm.nih.gov/34471935/. [DOI] [PMC free article] [PubMed]
- 13.Woitowich NC, Jain S, Arora VM, Joffe H. COVID-19 threatens progress toward gender equity within academic medicine. Acad Med. 2021 [cited 2022 Feb 6];96(6):813–6. Available from: https://pubmed.ncbi.nlm.nih.gov/33003040/. [DOI] [PMC free article] [PubMed]
- 14.Richter KP, Clark L, Wick JA, Cruvinel E, Durham D, Shaw P, Shih GH, Befort CA, Simari RD. Women physicians and promotion in academic medicine. N Engl J Med. 2020;383(22):2148–2157. doi: 10.1056/NEJMsa1916935. [DOI] [PubMed] [Google Scholar]
- 15.Mousa M, Boyle JA, Teede HJ. Women physicians and promotion in academic medicine. N Engl J Med. 2021;384(7):679–680. doi: 10.1056/NEJMc2035793. [DOI] [PubMed] [Google Scholar]
- 16.Celi LA, Charpignon M-L, Ebner DK, Kaufman AR, McCoy LG, Millado MC, et al. Gender balance and readability of COVID-19 scientific publishing: a quantitative analysis of 90,000 preprint manuscripts. medRxiv. 2021 [cited 2022 Feb 6];2021.06.14.21258917. Available from: 10.1101/2021.06.14.21258917v1.
- 17.Crowe SB, Kairn T. Women in medical physics: a preliminary analysis of workforce and research participation in Australia and New Zealand. Australas Phys Eng Sci Med. 2016;39(2):525–532. doi: 10.1007/s13246-016-0428-z. [DOI] [PubMed] [Google Scholar]