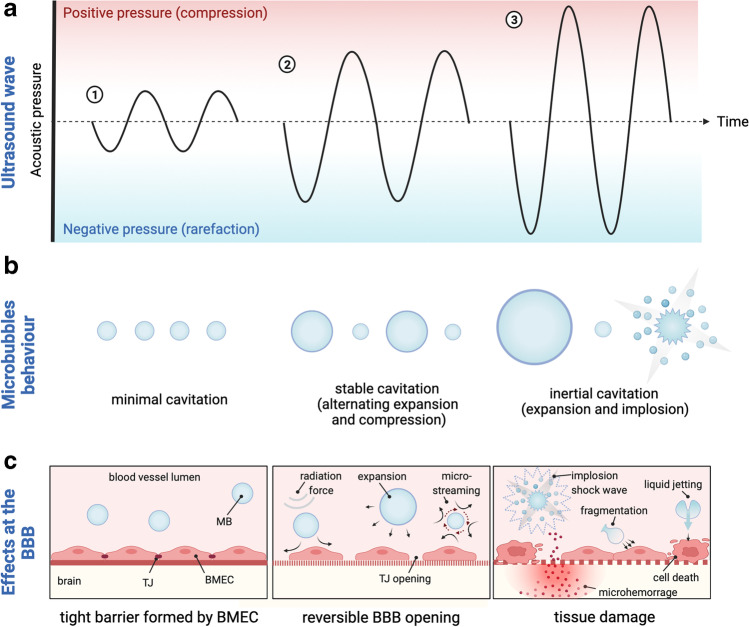
Fig. 2.
The interplay between focused ultrasound, microbubbles and cerebral vasculature. Physical interactions between ultrasonic wave (a) and microbubbles (MB) (b) determine the bioeffects at the blood-brain barrier (BBB) (c). When exposed to the ultrasound wave, MB decrease in diameter during the compression portion of the wave and increase during the rarefaction phase. (1) Ultrasound applied at insufficient acoustic pressure causes minimal volumetric oscillations of MB and the BBB remains closed. (2) Optimal ultrasound acoustic pressure induces stable MB contraction and expansion (stable cavitation) that exerts mechanical forces on brain microvascular endothelial cells (BMEC), leading to reversible BBB opening. Linearly cavitating MB generate the flow of liquid/blood around themselves (microstreaming) that in turn produces sheer stress on BMEC membrane, causing increased BBB permeability. Expanding MB create tension at tight junction (TJ) proteins leading to junction opening. Acoustic radiation force propels oscillating MB to the BMEC layer, further enhancing MB and BBB interactions. (3) At higher acoustic pressures, MB collapse violently, producing shock waves and micro-jets. This abrupt inertial cavitation generates strong mechanical stress at the BBB leading to permanent TJ disruption, irreversible BMEC membrane perforation, microhemorrhage and tissue necrosis. [24, 25, 27, 33–35]. BBB-blood-brain barrier; BMEC- brain microvascular endothelial cell; MB-microbubble; TJ-tight junction; Figure created with BioRender.com.