Abstract
The incidence of skeletal tuberculosis is about 1%-5% of all tuberculous infections. The most common sites are the spine, hip, knee, foot, elbow, hand, and shoulder, whereas the sternum, ribs, sternoclavicular joint, and calvaria are rarely affected. Because of the emergence of skeletal tuberculosis in therapeutic management, radiologists need to be aware of the imaging findings in pulmonary and extrapulmonary tuberculosis. Conventional X-ray plays an important role in diagnosing pulmonary and skeletal tuberculosis. Tuberculosis is known as the ‘great mimicker’, however, thus computed tomography and magnetic resonance imaging may provide additional details that assist the radiologist in distinguishing this tubercular infection from others. We report the case of a young male patient with skeletal tuberculosis who presented with general weakness, paraplegia, and a calvarial mass.
Keywords: Skeletal tuberculosis, Computed tomography, Magnetic resonance imaging, Extrapulmonary tuberculosis
Introduction
Tuberculosis (TB) is highly endemic in Indonesia, which has the second largest tuberculosis burden globally, with 845,000 cases of disease and 98,000 cases of mortality in 2018. Overall, TB is the fourth highest cause of death in Indonesia. Currently, it remains a challenge to diagnose tuberculosis at an early stage, particularly at extrapulmonary sites such as the skeleton. Skeletal infection represents only 1%-5% of all tuberculosis infections and may present as a malignancy in a differential diagnosis. We present the case of a young male patient with skeletal tuberculosis who presented with general weakness, paraplegia, and a calvarial mass.
Case report
Admission: February 2019
A 24-year-old male patient presented at the emergency department with a seizure, following four days of fever prior to admission. The fever was preceded by a chronic productive cough with yellowish sputum and gradual weight loss for a month. Four months prior to admission, the patient was hospitalised with inferior paraparesis and a calvarial mass considered to be a metastasis, with a malignant lung mass suspected as the primary cause.
Enhanced multi-slice computed tomography (MSCT) and magnetic resonance imaging (MRI) of the head showed left parietal bone destruction and soft tissue rim enhancement extended to the intracranial region and focal meningoencephalitis at the parietal lobe (Fig. 1). Both enhanced and unenhanced thoracolumbar MRI was performed, due to the presence of inferior paraparesis, and showed posterior vertebral destruction involving the lamina, pedicle, and the transverse and spinous processes, with a mass forming at the level of Th 5-6 that extended to the spinal canal and compressed the myelum with visible dural enhancement. An additional MRI finding showed an irregular mass on the right lung suggested as lung mass (Fig. 2).
Fig. 1.
Axial and coronal reformatted enhanced head MSCT (A,B) and axial T1 weighted images on enhanced MRI show left parietal bone destruction with soft tissue rim enhancement extending to the intracranial region, resulting in focal meningoencephalitis of the parietal lobe with slightly restricted diffusion on diffusion-weighted images (DWI) (E).
Fig. 2.
Posterior vertebral destruction involving the lamina, pedicle, and the transverse and spinous processes, with a mass forming at the level of Th 5-6 that extended to the spinal canal and compressed the myelum with visible dural enhancement in axial T1 (A), coronal T1 weighted image (B), and sagittal T2 weighted image (C), Suspicion of a lung mass in axial T1 weighted image with contrast (D).
Moreover, laboratory analysis showed the following results: CRP: 263 mg/L; 60 WBC: 19,300; Potassium: 5.5 mmol/L.
Enhanced and unenhanced thoracic MSCT was performed due to the lung mass and revealed a solid lung mass in the right mediobasal segment with multiple conglomerated lymphadenopathy at the right parabronchial, subcarinal, and right lower paratracheal (Fig. 3).
Fig. 3.
Both enhanced and unenhanced thoracic MSCT show (A,B) an irregular solid mass at the right mediobasal segment, (C) multiple conglomerated lymphadenopathy from the right parabronchial to the lower paratracheal and subcarinal, (D) destruction of Th 5-6 (white arrow) and sternal bone (red arrow) with a rim-enhanced soft tissue mass. These findings are suggestive of a malignant solid lung mass with multiple bone metastases.
Histopathological evaluation of the right lung mass revealed a granulomatous inflammation (Fig. 4), and the calvarial tissue biopsy identified a granulomatous inflammation with positive staining of acid-fast bacilli (Fig. 5).
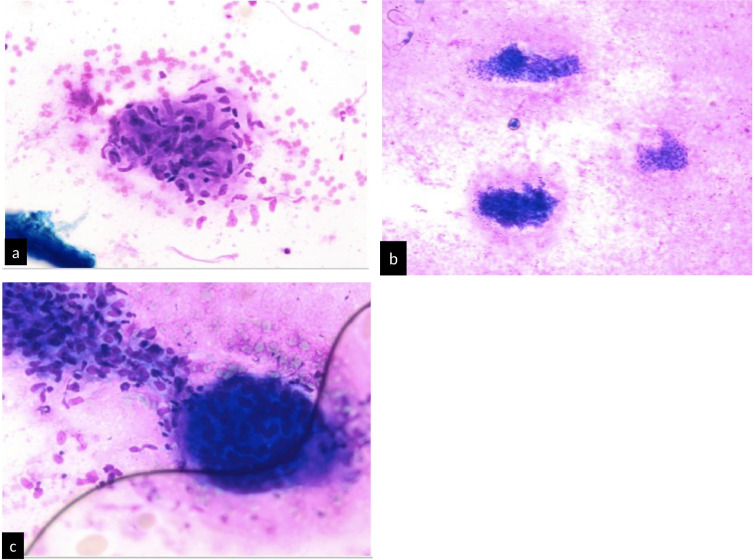
Fig. 4.
A fine needle aspiration biopsy (FNAB) of the right lung mass using Diff-Quick staining are shown in images A and C at 200x magnification and in image B at 100x magnification, which mononuclear cells and PMNs, clusters of epithelioid histiocytes forming granulomas, and multinucleated giant cells.
Fig. 5.
Histopathological evaluation of calvarial excision with haematoxylin eosin staining, with images A and B at 40x magnification showing granulomatous tissue, and C and D images at 100x magnification showing positive acid-fast bacilli staining.
Discussion
Calvarial tuberculosis
The most common location of calvarial tuberculosis is in the frontoparietal area. Radiological findings typically show identically round or oval-shaped osteolytic lesions with sclerotic edges. The occurrence of subgaleal swelling (Pott's puffy tumour) in calvarial tuberculosis is also commonly observed. In addition, a sinus is formed when calvarial tuberculosis involves the external table of the skull. Involvement of the internal table is associated with the formation of granulation tissue in the infected area of the extradural space [2,3].
Chest wall tuberculosis
Despite TB being a curable disease, due to the availability of efficacious treatment, about 1%-5% of skeletal tuberculosis arises on the chest wall. The sternum is the second most common location of chest wall tuberculosis, after the rib, and is commonly found in immunocompromised individuals. Notable CT scan findings include bone destruction and soft tissue mass that passes through the fascia. In addition, abscesses and calcifications in the affected pleuro-parenchymal area are typically observed. In such cases, it is important to assess the involvement of the sternoclavicular joint. MRI may reveal marrow changes in the sternum and clavicula (hypointense T1W and hyperintense T2W) [4].
Infection in the costae is defined as rib tuberculosis in which bony erosion, destruction, and abscesses occur in the affected costae. According to reports in the literature, in regions that are accessible to sonography there is enough sensitivity to detect rib tuberculosis as a hypoechoic structure with a heterogeneous internal echo. A bone fragment from the destructive process will present as echogenic foci. In areas not accessible to sonography, a CT or MRI evaluation can be performed. Various complications of tuberculous sternal osteomyelitis may include secondary infections, fistula, tracheal compression, or tuberculous abscess rupture to the mediastinum cavity, pleura, or subcutaneous tissue [4,5].
Tuberculous spondylitis
Tuberculous spondylitis is the most common manifestation of skeletal tuberculosis and is typically located on the anterior side of the corpus vertebrae. Though rare, it can also involve the posterior part of the vertebrae. The process of infection mostly occurs in the anteroinferior portion of the corpus vertebrae and spreads to the adjacent vertebral body through the longitudinal ligament. Based on reports in the literature, posterior element tuberculous spondylitis or posterior spinal tuberculosis abnormalities present in the form of solitary lesions and are caused by [10]:
-
1
The primary spread of Mycobacterium tuberculosis through the Batson plexus located in the epidural space.
-
2
Immunocompetency.
Posterior spinal tuberculosis is preceded by a primary infection that spreads haematogenously through the venous plexus. In addition, this manifestation of disease also surrounds the spinous process, transverse process, and articular process, similar to that of osteoarticular tuberculosis. Moreover, the venous plexus is characterised by an adjacent venous plexus in the posterior part of the lamina, which tends to facilitate the spread of infection from the neural arch, for example, the pedicle, lamina, processus transversus, or processus spinosus. The degree of corpus damage originates from the narrow area of the intervertebral spatium and is a secondary event. The difference between tuberculous spondylitis and bacterial spondylitis is found in the extent of disc preservation in tuberculosis infections due to the absence of proteolytic enzymes in Mycobacterium [6,7,10].
The formation of a cold abscess is an important finding in skeletal tuberculosis that also occurs in tuberculous spondylitis, and can be located in the posterior midline, para-midline, or bilateral midline. When more than one vertebra is involved (ie, pan-vertebral involvement), the condition results in the abscess forming in the paravertebral gutter, psoas, or the anterior trunk wall of Petit's triangle. These abscesses can generate sinuses and extend to the surface of the skin and cause ulceration. Furthermore, posterior spinal tuberculosis can be found together with the formation of extradural granuloma or granular tissue that lines or encloses the dural sac and resembles a spinal [8], [9], [10], [11].
Most cases are found as a form of primary TB, which is strictly limited to a flat surface, accompanied by calcification of 20%-30%, and as much as 10%-50% cavitation [4]. Imaging findings in skeletal tuberculosis vary in the extent of the locations in which scans are rarely obtained (eg, the posterior column vertebra or calvaria). Therefore, tuberculosis is known as the ‘great mimicker’ because it is commonly mistaken as one form of metastases or even a primary tumour, even though it occurs in the form of solitary lesions [1,4,9].
In the present case, the suspected lung mass was identified through incidental MRI findings of the thoracolumbar spine. The FNAB CT subsequently diagnosed the mass as a tuberculoma. Nevertheless, the presence of bone destruction with soft tissue mass, without calcification, in some places is still controversial. There was no malignancy found at the time of open biopsy obtained from the sternum and calvaria lesions that resulted in chronic inflammation. Thoracic MSCT with contrast showed a solid mass that resembled a malignant lung image with significant spicula edges. Radiological clues for the diagnosis of tuberculosis, as well as rim enhancement patterns in soft tissue masses of the calvaria and sternum, can be found in images of multiple lymphadenopathies. Based on the current literature, both the location of the suspicious area and the presence of a central hypodense area are suitable factors for diagnosis.
Conclusion
Skeletal tuberculosis in rare locations often results in radiological images that resemble non-specific masses or malignancy, which can result in delayed diagnosis. In addition, extrapulmonary TB can lead to more pronounced and deleterious manifestations of disease, with or without minimal pulmonary TB.
Patient consent and ethical approval
Informed consent for patient information included in this article was obtained. Appropriate informed consent was obtained for the publication of this case report and accompanying images. This case report has been approved by the ethical committee of Dr Soetomo General-Academic Hospital (Letter of Exemption 1202/118/4/1/2022).
Footnotes
Competing Interests: The authors declare that they have no known competing financial interests or personal relationships that could appear to influence the findings reported in this paper.
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.radcr.2022.03.035.
Appendix. Supplementary materials
References
- 1.Gambhir S, Ravina M, Rangan K, Dixit M, Barai S, Bomanji J. Imaging in extrapulmonary tuberculosis. The International Atomic Energy Agency Extra-pulmonary TB Consortium. 2017;56:237–247. doi: 10.1016/j.ijid.2016.11.003. PMID: 27838445. [DOI] [PubMed] [Google Scholar]
- 2.Rosli FJ, Haron R. Tuberculosis of the skull mimicking a bony tumor. Asian J Neurosurg. 2016 Jan-Mar;11(1):68. doi: 10.4103/1793-5482.172594. PMID: 26889285; PMCID: PMC4732248. [DOI] [PMC free article] [PubMed]
- 3.Ravikanth R, Mathew S, Selvam RP. Calvarial tuberculosis presenting as multiple osteolytic soft tissue lesions. CHRISMED Journal of Health Research. 2017;4:278–279. doi: 10.4103/cjhr.cjhr_36_17. [DOI] [Google Scholar]
- 4.Bhalla AS, Goyal A, Guleria R, Gupta AK. Chest tuberculosis: Radiological review and imaging recommendations. Indian J Radiol Imaging. 2015 Jul-Sep;25(3):213-25. doi: 10.4103/0971-3026.161431. PMID: 26288514; PMCID: PMC4531444. [DOI] [PMC free article] [PubMed]
- 5.Saibaba B, Meena UK, Behera P, Meena RC. Multicentric spinal tuberculosis with sternoclavicular joint involvement: a rare presentation. Case Reports in Pulmonology. 2014;Oct:4. doi: 10.1155/2014/685406. PMID: 25389505; PMCID: PMC4217363. Hindawi Publishing Corporation Case Reports in Pulmonology VolumeArticle ID 685406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grover SB, Jain M, Dumeer S, Sirari N, Bansal M, Badgujar D. Chest wall tuberculosis - A clinical and imaging experience. Indian Journal of Radiology and Imaging. 2011;21(1):28–33. doi: 10.4103/0971-3026.76051. PMID: 21431030; PMCID: PMC3056366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pearce JM. The craniospinal venous system. European Neurology. 2006;56(2):136–138. doi: 10.1159/000095706. PMID: 16960456. [DOI] [PubMed] [Google Scholar]
- 8.Smith AS, Weinstein MA, Mizushima A, Coughlin B, Hayden SP, Lakin MM, et al. MR imaging characteristics of tuberculous spondylitis vs vertebral osteomyelitis. American journal of neuroradiology. 1989;10:619–625. doi: 10.2214/ajr.153.2.399. PMID: 2750627 0195-6108/89/1003-0619 © American Society of Neuroradiology. [DOI] [PubMed] [Google Scholar]
- 9.Kumar Kush, U.S. Department of Veterans Affairs, Dublin, Georgia, USA Posterior Spinal Tuberculosis: A Review. Mycobacterial Diseases. 2017;7(2):1–4. doi: 10.4172/2161-1068.1000243. ISSN:2161-1068. [DOI] [Google Scholar]
- 10.Al-Khudairi N, Meir A. Isolated tuberculosis of the posterior spinal elements: case report and discussion of management. JRSM Open. 2014;5(9):1–6. doi: 10.1177/2054270414543396. PMID: 25352992; PMCID: PMC4207282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Khattry N, Thulkar S, Das A, Khan SA, Bakhshi S. Spinal Tuberculosis Mimicking Malignancy, Atypical Imaging Features. The Indian Journal of Pediatrics. 2007;74(3):297–298. doi: 10.1007/s12098-007-0049-3. PMID: 17401273. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.