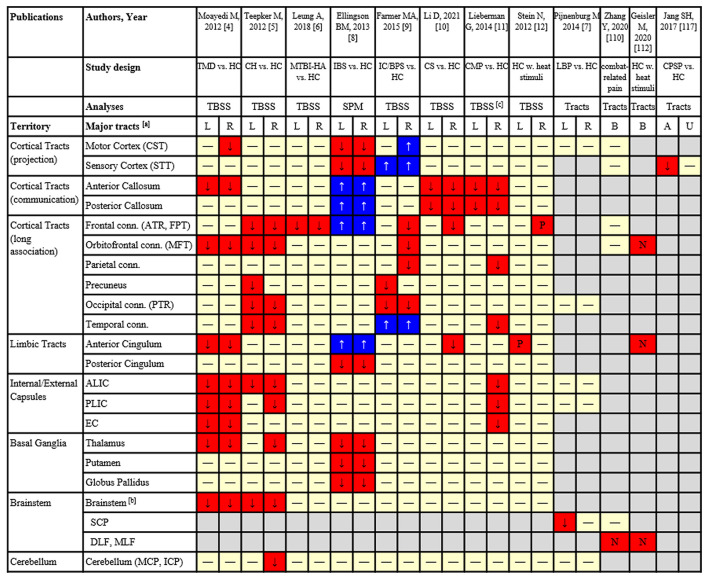
Figure 1.
Results from tract-based analyses based on DTI of pain studies:  FA significantly reduced in patients;
FA significantly reduced in patients;  FA significantly increased in patients;
FA significantly increased in patients;  FA was not significantly different;
FA was not significantly different;  Reduced FA signficantly correlated with increased pain intensity/sensitivity;
Reduced FA signficantly correlated with increased pain intensity/sensitivity;  Increased FA significantly correlated with greater analgesic response;
Increased FA significantly correlated with greater analgesic response;  Not analyzed. [a] Cortical and subcortical areas of major fiber tracts (specific tracts included); [b] Some areas in the brainstem without specific definition of tracts. [c] Significant findings are presented based on RD instead of FA which showed a weaker significance. TMD, temporomandibular disorder; HC, healthy control; CH, cluster headache; MTBI, mild traumatic brain injury; IBS, irritable bowel syndrome; IC/BPS, interstitial cystitis/bladder pain syndrome; CS, cervical spondylosis with pain; CMP, chronic musculoskeletal pain; LBP, low back pain; CPSP, central post-stroke pain; TBSS, tract-based spatial statistics; SPM, statistical parametric mapping; CST, corticospinal tract; STT, spinothalamic tract; ATR, anterior thalamic radiation; FPT, frontopontine tract; MFT, medial forebrain tract; PTR, posterior thalamic radiation; ALIC, anterior limb of internal capsule; PLIC, posterior limb of internal capsule; EC, external capsule; SCP, superior cerebellar peduncle; DLF, dorsal longitudinal fasciculus; MLF, medial longitudinal fasciculus; MCP, middle cerebellar peduncle; ICP, inferior cerebellar peduncle.
Not analyzed. [a] Cortical and subcortical areas of major fiber tracts (specific tracts included); [b] Some areas in the brainstem without specific definition of tracts. [c] Significant findings are presented based on RD instead of FA which showed a weaker significance. TMD, temporomandibular disorder; HC, healthy control; CH, cluster headache; MTBI, mild traumatic brain injury; IBS, irritable bowel syndrome; IC/BPS, interstitial cystitis/bladder pain syndrome; CS, cervical spondylosis with pain; CMP, chronic musculoskeletal pain; LBP, low back pain; CPSP, central post-stroke pain; TBSS, tract-based spatial statistics; SPM, statistical parametric mapping; CST, corticospinal tract; STT, spinothalamic tract; ATR, anterior thalamic radiation; FPT, frontopontine tract; MFT, medial forebrain tract; PTR, posterior thalamic radiation; ALIC, anterior limb of internal capsule; PLIC, posterior limb of internal capsule; EC, external capsule; SCP, superior cerebellar peduncle; DLF, dorsal longitudinal fasciculus; MLF, medial longitudinal fasciculus; MCP, middle cerebellar peduncle; ICP, inferior cerebellar peduncle.