Abstract
Background.
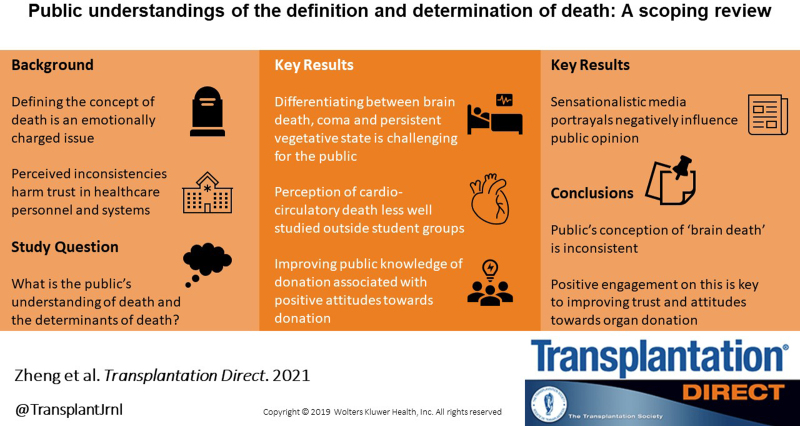
Advances in medicine and technology that have made it possible to support, repair, or replace failing organs challenge commonly held notions of life and death. The objective of this review is to develop a comprehensive description of the current understandings of the public regarding the meaning/definition and determination of death.
Methods.
This scoping review was conducted in compliance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews checklist. Online databases were used to identify articles published from 2003 to 2021. Two reviewers (S.S. and K.Z.) screened the articles using predefined inclusion and exclusion criteria, extracted data for specific content variables, and performed descriptive examination. Complementary searches of reference lists complemented the final study selection. A search strategy using vocabulary of the respective databases was created, and criteria for the inclusion and exclusion of the articles were established.
Results.
Seven thousand four hundred twenty-eight references were identified. Sixty were retained for analysis, with 4 additional references added from complementary searches. A data extraction instrument was developed to iteratively chart the results. A qualitative approach was conducted to thematically analyze the data. Themes included public understanding/attitudes toward death and determination of death (neurological determination and cardiocirculatory determination of death), death and organ donation, public trust and legal variability, and media impacts.
Conclusions.
This review provides a current and comprehensive overview of the literature related to the general public’s understanding and attitudes toward death and death determination and serves to highlight the gaps in this topic.
INTRODUCTION
Advances in medicine and technology have made it possible to support, repair, or replace failing organs, challenging commonly held notions of life and death.1 For example, mechanical ventilation replaced respiration and supported heart function to prevent cardiac arrest, which interrupted the way death occurred. The boundaries between being alive, dying, or being dead became blurred, and this has sparked ongoing controversy and debate in the literature among ethicists, scholars, and clinicians along with confusion among the general public. The inconsistencies in the concept and practice in determining death, particularly brain death, both nationally and internationally, coupled with the emotionally charged nature of the topic, further complicate discussions on death and the determination of death.1,2 In this article, the terms circulatory determination of death, cardiocirculatory death, and cardiac death are interchangeable and are used as referred to in the original publication. Similarly, brain death, death by neurological criteria, neurological determination of death, and brainstem death are interchangeable for the same reason.
In recent years, high-profile cases between families and healthcare providers have been prominently featured by the media and consequently have highlighted public interest in brain death and death diagnosis.3-11 Prominent cases include several involving both children, like the McMath case in California in 2013, Lopez in Kentucky in 2014,3,10,11 and Re A (a child) in the United Kingdom in 2015,4 and adults, like the Munoz case in Texas in 20133,11 and the Hailu cause in Nevada in 2015.9 Prominent Canadian cases include McKitty and Ouanounou, both in 2017.12 These events are heavily published; although some have affected outcomes to resolve other brain death conflicts, others have caused increased suspicion and challenges of the diagnosis.
Spurred on by early work on the Uniform Determination of Death Act by the Uniform Law Commission, many scholars have called for an international consensus on the determination of death that could provide a number of benefits, including promoting evidence-based practices, protecting the rights of both patients and healthcare professionals, improving public and professional confidence in the process of deceased donation, and increasing the number of organs obtained for transplantation in an ethically legitimate manner.1,2 An important first step in any attempt at developing a consensus on the definition of death is to better understand the general public’s current views on the topic. The goal of this scoping review is to develop a comprehensive description of the current understanding(s) of the public regarding the meaning, definition, and determination of death.
MATERIALS AND METHODS
This scoping review was undertaken in accordance with the Joanna Briggs Institute methodology for scoping reviews13 and in compliance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) extension for Scoping Reviews checklist.14 As a scoping review rather than a systematic review, study inclusion was not limited by study quality or methodology, and all aspects of public understanding of death definition and determination were included.
Literature Search
We used a 2-step process for this review. The first step was to identify whether there exist similar systematic or scoping reviews on the topic of brain death meaning, definition, and determination. We searched online databases Ovid MEDLINE and Psych INFO to identify a known set of studies relevant to the topic. The topic was refined on the basis of identification of research gaps in the systematic review literature. Two independent reviewers (S.S. and L.H.) screened titles and abstracts in duplicate.
We then used key search terms identified from the systematic reviews during part 1 to refine the search strategy for a second search of online databases and gray literature sources. An information specialist searched electronic databases—Ovid MEDLINE, Ovid PsycINFO, and CINAHL—using controlled vocabulary (eg, Medical Subject Headings) and text words for concepts: death, organ donation, determination, and attitudes. R.F. also searched Conference Proceedings Citation Indices for meeting abstracts, ProQuest Dissertations and Theses Global for academic dissertations, and Google Scholar for any studies missed by the database searches. Search results were limited to studies published since 2003 in English. Duplicates were removed.
We included studies that explicitly discussed the public’s attitudes toward concepts around brain death or circulatory death. We defined the “public” to include the citizens of any given country. Our search yielded many articles that described people’s understanding of death/determination of death within the context of organ donation. In the context of organ donation and transplantation, the “public” and “families” became synonymous as many studies sought the opinion of families as their loved one progressed through the organ donation/transplantation processes. We excluded studies that only focused on either the organ donation/transplantation process itself or palliative care/end-of-life care without any discussion about the understanding of or attitudes toward death.
Screening
Two independent reviewers (S.S. and K.Z.) screened titles and abstracts using predefined inclusion and exclusion criteria. Articles were divided by stakeholder groups, healthcare providers, and the public. The focus of this scoping review is on the public perspective subset of the search. Both reviewers extracted data for specific content variables and performed the descriptive examination. The full text of selected citations was then retrieved and assessed in detail against the criteria by the 2 independent reviewers. Any disagreements were resolved through discussion.
Data Extraction and Synthesis
A data extraction instrument was developed to iteratively chart the results of the review. Extracted fields included authors, year of publication, country of origin (where the study was published or conducted if available, or country of the lead author), type of text, language, aims/purpose, study population, methodology, and key findings relating to the scoping review. All data were extracted from articles in duplicate (S.S. and K.Z.). S.S. and K.Z. also extracted data on the evolution of the death definition and public attitudes toward death and undertook qualitative content analysis of included studies. The codes were collapsed into themes that were used to write narrative summaries of each named theme.13 Additional articles were identified from review of the reference lists of included articles and added for data extraction and complimentary searches of the literature.
RESULTS
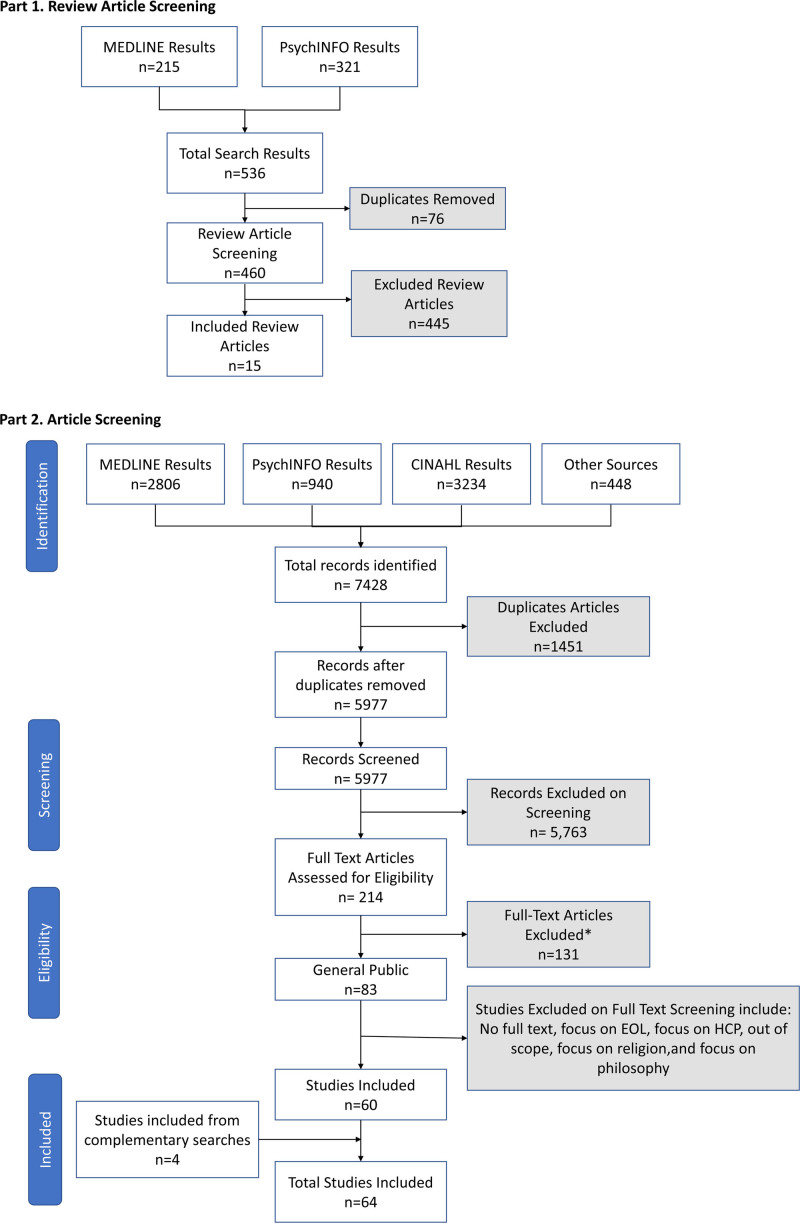
Figure 1 (PRISMA diagram) summarizes the search process and results, culminating in a total of 7428 citations. After removing 1451 duplicate citations, another 5763 were excluded on the basis of their title and on review of their abstracts. Full-text screening was undertaken on 214 articles. A further 23 articles were removed on the basis of full-text screening; reasons included focus on religion, end of life, healthcare provider, philosophy, and a duplicate article. A total of 60 met the inclusion criteria. Four additional articles were added from hand searches, resulting in 64 total articles included (see Supplemental Digital Content 1, SDC, http://links.lww.com/TXD/A406 for list of articles) for data extraction (see again Figure 1 for the PRISMA diagram). Table 1 provides a listing of the characteristics of included articles. The most common study type was narratives (25), followed by reviews (11), and the most common method for collecting data from the public was through quantitative studies (17). Most studies originated from North America (33) and Europe (14). Emergent themes are presented in Table 2.
FIGURE 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist. CINAHL, Cumulative Index to Nursing and Allied Health Literature; EOL, end of life; HCP, healthcare provider. *Also includes excluded articles relating to public or religious perceptions included during the abstract screening process.
TABLE 1.
Characteristics of included articles (n = 64)
| Descriptor | N | |
|---|---|---|
| Source | Initial search | 60 |
| Complimentary searches | 4 | |
| Type of article | Narrative/opinion | 25 |
| Review | 11 | |
| Quantitative | 17 | |
| Panel report | 2 | |
| Qualitative | 6 | |
| Mixed methods | 3 | |
| Country of publicationa | United States | 30 |
| Europe | 17 | |
| Canada | 4 | |
| Asia | 4 | |
| Oceania | 3 | |
| Other | 6 | |
| Language | English | 64 |
| Publication date | 2003–2013 | 23 |
| 2013–2020 | 41 |
aCountry where the study was conducted or, when not available, the country of the lead author.
TABLE 2.
Themes discovered through qualitative analysis of included reference
| Theme | Brief definition |
|---|---|
| Public understanding toward death and death determination: NDD | How the public comprehends death and how death is declared with regard to neurological criteria |
| Public understanding toward death and death determination: DCD | How the public comprehends death and how death is declared with regard to circulatory criteria |
| Brain death and organ donation | The public’s understanding of brain death and its relation to organ donation |
| Public trust in HCPs and the healthcare system | The relationship between public confidence in care at the hospital level and healthcare system level |
| Media, colloquialisms, and brain death | How the media acts to inform (or disinform) the public about brain death |
DCD, donation after circulatory death; HCP, healthcare provider; NDD, neurological determination of death.
Public Understanding Toward Death and Death Determination: Neurological Determination of Death
Since its inception in 1968, the concept of whole-brain death has been contentious.15 Although it is recognized and widely accepted as death in North America and elsewhere across the globe, there exists “medical, moral, and philosophical” disagreement mainly from healthcare professionals.16 This review found that the public has a general awareness and acceptance of brain death; however, they have a poor understanding of the meaning of brain death and confusion with other brain conditions such as coma and persistent vegetative state. Brain death is defined as a loss of function of the brain, but declaring brain death does not require the death of every neuron.17 This only serves to highlight the ongoing confusion over the current definition of brain death and fuels the need for an international change in the legal definition of death.
Twenty-two studies located reveal that the overall public understanding of brain death is indeed poor.3,11,17-37 Twenty-four empirical studies were identified that examined the public’s understanding of death and its determination using quantitative, qualitative, and mixed methodologies (Table 3). Siminoff et al17 found that a sizable number of people (30%) in their study agreed with the statement “a person is dead only when the heart has stopped beating.” Even among those who had good knowledge of the brain death diagnosis, it is often difficult to accept it as a true death.33,36,45 The appearance of life in brain death, with warm skin, a heartbeat, and breathing even with the help of a machine, complicates the family’s acceptance of the death of their loved ones and the diagnosis.5,15 Brain death creates cognitive dissonance and conflicts with the schema of a dead body (cold, motionless, does not breathe). In these situations, temporary ventilator disconnection, a routine part of the examination to confirm the absence of the ability to breathe to establish the brain death diagnosis, may be an effective way of helping families understand and accept brain death.2,45
TABLE 3.
Empirical studies examining the public’s understanding of death and death determination (n = 26)
| References | Country | Study design | Type | Method of data collection | Study population | Aims | Findings |
|---|---|---|---|---|---|---|---|
| Al Bshabshe et al24 | Saudi Arabia | Quantitative | BD | Survey | 873 university students | To explore university students’ understandings of BD. | Ninety-three percent of students had heard of BD and 73% believe that there is no difference from natural death; 22.5% thought a BD patient might recover, whereas 34.8% did not. |
| Akbulut et al31 | Turkey | Quantitative | BD | Survey | 3000 adults | To evaluate the attitudes, awareness, and knowledge levels of the Turkish adult population about organ donation. | Only 47.2% of participants said they had inadequate information about BD, and 85.2% refused to consent to donating organs of family members declared brain dead. The majority of participants said they got their information about BD from television. |
| Daoust and Racine38 | United States and Canada | Qualitative | BD | Document review | 940 newspaper articles in United States and Canada | To examine the depictions of BD in major American and Canadian print media. | Discovered problematic aspects in both Canadian and US media. In 39% of the articles, DNC was used colloquially. The NDD was mentioned in <10% of the articles and life support in 20% of the articles. |
| DuBois and Schmidt25 | United States | Mixed methods | BD | Structured telephone interviews using case scenarios, open-ended questions, and 15 Likert-type questions. | 1000 heads of households (aged ≥18 y), English speaking | To assess willingness to donate under the higher brain-death criteria and factors influencing those attitudes. | Only 8% said BD is death, but most offered incomplete but accurate descriptions; 2% offered statements suggesting possibility of recovery. Sixty percent agreed patients could be dead while the heart was still beating, almost all when machines keep them breathing. Public support for NDD has more to do with belief that the brain has irreversibly lost all function and trust in the HCP rather than legal criteria. |
| DuBois et al39 | United States | Mixed methods | Both | Focus groups and surveys, before and after being educated about Rapid Organ Recovery | 70 African American, Caucasian, and Latino participants (St. Louis, MO) | To investigate what the public thinks about key ethical and policy questions associated with rapid organ recovery. | Some participants expressed concerns over the length of resuscitative efforts before cardiac death determination. Nobody expressed concerns about DCD donors being truly dead, whereas there were some concerns and doubts regarding NDD, many of which were based on misinformation. |
| Febrero et al27 | Europe | Quantitative | BD | Survey | 3547 adolescents in southeast Spain across 10 schools | To analyze the concept of BD among adolescents in the southeast of Spain. | Thirty-eight percent of adolescents knew the BD concept and considered it to be the death of an individual. Fifty-four percent did not know the BD concept, and 8% thought it did not mean a person’s death. There was an association between older age and knowledge of BD. There was no association with audiovisual sources but negatively associated with negative information from television. |
| Febrero et al28 | Europe | Quantitative | BD | Survey | 351 older adults (aged >65 y) in southeast Spain | To analyze the level of understanding of BD in people aged >65 y. | Thirty-six percent of older adults understood the BD concept as the death of a person (similar level to adolescents and immigrants but lower than the general population). Necessary to carry out informative campaigns to explain this concept. |
| Haddow22 | Europe | Qualitative | BD | Semistructured interviews | 19 Scottish donor families | To explore families’ beliefs about death, the dead body, and impact on donation decision. | Many knew about BSD from televised medical dramas. Some family members had a realization of when death occurred even before medical confirmation, “social death,” because of HCP communication, attending to ICU technology, and awareness of BD from medical TV dramas. |
| The majority of Canadians sampled support cardiac DCD. Most respondents supported the implementation of direct procurement and perfusion (73.7%) and normothermic regional perfusion (65.4%) in Canada. | |||||||
| Joffe et al40 | Canada | Quantitative | Cardiac | Survey | University students (medical n = 142, nursing n = 76, and philosophy n = 102) | To determine whether university students consider the DCD donor as dead. | Most university students were not confident that a DCD donor was actually dead. In at least 1 of 4 patient scenarios involving donors after circulatory death, 65% of those who gave detailed information and 50% of those who gave brief background information were not confident or did not believe the patient was definitely dead (P < 0.001). |
| Lim et al32 | Malaysia | Quantitative | BD | Questionnaires | 400 patients | To assess knowledge and determine factors influencing attitudes toward organ donation. | The greater the knowledge of BD and organ donation, the more positive attitude toward organ donation. |
| Long23 | Europe | Qualitative | BD | Interviews | 28 family members of BD patients | To explore the concept of BSD and its meaning to family members. | For family members, a continuing heartbeat and respiration is a trigger for emotional and cognitive conflict. BD diagnosis may represent irreversible loss of mental life but not actual death (cessation of heartbeat and respiration). Technology of life support contradicts diagnosis of BSD. Technology obscures impending death and amplifies family member’s schema of a dead body (cold, motionless, does not breathe). |
| Neiders and Dranseika41 | Europe | Quantitative | Both | Online vignette-based survey | 1416 Latvians | To better understand people’s preferences about death determination criteria. | There is a wide range of preferences regarding death determination criteria, which suggests that the pluralist solution may be the best representation of participants’ perceptions. Interestingly, participants were less restrictive with criteria for their own death determination than those of their closest relatives. |
| Nowak et al19 | Europe | Quantitative | BD | Survey | 400 medical and 400 nonmedical students from 4 public universities in Poland | To assess young peoples’ knowledge and attitudes toward death and impact on organ donation and transplantation. | Level of trust in BD diagnosis is relatively low among nonmedical respondents (38.5% vs 78.5%). Reasons included doubts about BD criteria (31.5%) and distrust of medical staff’s education (25%). Unwillingness to accept BD as the death of a human being was related to one’s opinion about the reliability of the diagnosis. |
| Ríos et al36 | Europe | Quantitative | BD | Survey | 9598 Spanish medical students | To assess whether Spanish medical students understand the concept of BD. | Sixty-seven percent of respondents understood the BD concept, and the rest did not know what it meant.The variables related to correct understanding were (1) being older, (2) studying at a public university, and (3) studying at one of the universities in the south of Spain. |
| Ríos et al30 | Europe | Quantitative | BD | Survey (validated) |
259 respondents born in Puerto Rico and residing in Florida (aged ≥15 y) | To analyze the knowledge of BD concept among the Puerto Rican population in Florida. | Thirty-five percent knew the BD concept and considered it the death of an individual. Forty-four percent do not know the BD concept and 21% do not consider it death. Sex, marital status, and religion were significantly related to correct knowledge of BD. |
| Ríos et al29 | Europe | Quantitative | BD | Survey | 461 residents of Spain born in Ecuador (aged ≥15 y) | To analyze the knowledge of the BD concept among the Ecuadorian population resident in Spain. | Only 22% knew the BD concept and accepted it as the real death of the person. Sixty-one percent do not know the BD concept. Older age and marital status (separated, widowed, or divorced vs single) are associated with greater knowledge of BD (P < 0.05). |
| Ríos et al33 | Europe | Quantitative | BD | Survey | 441 Algerians living in Spain | To analyze the knowledge and acceptance of BD among the Algerian population living in Spain. | The Algerian population immigrating to Spain has little knowledge of the BD concept, which has a direct relationship with their attitude toward organ donation. |
| Ríos et al37 | Europe | Quantitative | BD | Survey | 636 Cubans living in Spain | To analyze the knowledge and acceptance of BD among the Cuban population living in Spain. | Approximately 50% of the Cuban population living in Spain knows and accepts the concept of BD as the actual death of the individual, and they have a favorable attitude toward organ donation. |
| Pessoa et al42 | Brazil | Quantitative | BD | Survey | 868 participants | To evaluate the knowledge of the population about BD and organ donation. | Participants had conflicting knowledge of BD. For example, 26.8% of the population believed that BD was reversible. |
| Siminoff et al17 | United States | Qualitative | BD | Focus groups | 403 families of organ donor-eligible patients with a BD relative | To examine factors related to families’ understanding of BD and how those factors affect decisions about organ donation. | Ninety-six percent of families were told their relative was BD and only 28.4% were able to provide a completely correct definition of BD. Thirty percent agreed that a person is dead only when the heart stops beating. Those who donated were less likely to agree with the statement that someone is dead only when the heart stops. The term BD has a variety of meanings in everyday speech, undermining the public’s understanding of the medical meaning. |
| Siminoff et al43 | United States | Qualitative | BD | Randomly selected and surveyed using random digit dialing | 1351 Ohio residents (aged ≥18 y) | To examine the public attitudes and beliefs about the determination of death and its relationship with organ transplantation. | Ninety-eight percent had heard of BD, but only 33.7% believed that someone who was BD was legally dead. 86.2% identified the BD patient as dead, 57.2% identified the patient in a coma as dead, and 34.1% identified the patient in a persistent vegetative state as dead. A majority were unaware, misinformed, or held beliefs incongruent with current definitions of BD. |
| Stadlbauer et al34 | Austria and Switzerland | Quantitative | BD | Survey | 754adolescents (aged 11–20 y) | To assess knowledge and attitudes toward organ donation. | Only 59% of adolescents believed that a person is really dead when he/she is declared brain dead. |
| Tarzi et al35 | Syria | Quantitative | BD | Survey | 303 adults | To evaluate the attitude and knowledge of organ donation among Syrians and the willingness of this population to donate their organs. | When assessing knowledge about BD, only 40% answered 3 or more questions correctly (out of 5). Although a more positive attitude toward organ donation was found in those with better BD knowledge, this did not translate into more willingness to donate organs in this group of participants. |
| Tessmer et al20 | South America | Quantitative | BD | Survey | 3159 participants in urban area of Brazil (aged ≥20 y) | To examine public understanding of BD and how the term BD affects decisions about organ donation. | 80.1% would authorize organ donation after the death of a relative who had declared a willingness to do so. When death is substituted with BD, willingness to donate decreased 20%, showing individuals did not understand or accept the term BD. Women are less accepting of or understand less about BD than men. |
| Verble et al44 | United States | Qualitative | DCDD | Self-report documentanalysis | 4 different OPO agencies from148 cases (patients) | To determine the concerns of families approached for DCD and explore how those might be addressed to increase DCD donation rates. | Family concerns that block DCD differs in many ways from those of BD families. Results from DCD family concerns were grouped into 3 overlapping categories: practicalities, suffering, and process. |
BD, brain death; BSD, brain stem death; DCD, donation after circulatory death; DCDD, donation after the circulatory determination of death; DNC, death determination by neurological criteria; HCP, healthcare provider; ICU, intensive care unit; NDD, neurological determination of death; OPO, organ procurement organization.
Studies show that public comprehension of the distinctions between brain death, a coma (temporary gross impairment in brain function), and a persistent vegetative state (a permanent unconscious state with retention of the ability to breathe without assistance and preservation of some brainstem reflexes) is poor.3,11,21,46,47
Other studies have reported similar findings in that people believe that brain death does not mean a person is dead and that it is not the same as “natural death.”17,24,27,29,30,43,48 Other studies showed that people believed that brain-dead patients were still alive or would recover.25,43,48 In other countries like Japan, the cessation of brain function is not necessarily felt to be representative of the cessation of life while other organs such as the heart continue to function.49
Public Understanding Toward Death and Death Determination: Circulatory Determination of Death
Circulatory determination cases involve declaration of death very quickly after loss of circulation, whereas without donation, there is extended time to observe death after loss of circulation. Of the few studies located regarding the public’s understanding of death by circulatory criteria, all were in the context of organ donation and transplantation.39,40,50,51 Only 3 studies explicitly focused on asking participants about the determination and timing of death.40,41 Neiders and Dranseika41 found that circulatory criteria of death were the least preferred by participants compared with whole brain and higher brain death for their own death determination but preferred over higher brain death criteria for their relatives. Joffe et al40 asked university students (undergraduate medical students, nursing students, and philosophy students) to consider if patients who donate organs after circulatory death are really dead. The majority of students in all 3 groups were not confident that a donation after circulatory death (DCD) donor was actually dead. Interestingly, it was the medical student group who were less likely to agree that the DCD patient was dead45 and mainly cited the concept of irreversibility as adding to the confusion. This study concludes by stating that depending on how questions are asked, there is no uniform acceptance that the DCD patient is dead.40
A third study by Verble et al44 sought to determine the primary concerns of families who were approached for DCD. The authors found that family concerns regarding DCD differed in significant ways than in donation after brain death. Of the 16 main concerns,44 not one focused on difficulties in understanding death. Overall, there have been minimal investigations regarding public perceptions in the domain of circulatory determination of death.
Death and Organ Donation
The literature on the public’s understanding of death and death determination is closely linked to organ donation and transplantation. Given this context, it is important to understand how death, particularly brain death, may be perceived by family members when approached about organ donation. The majority of studies located focus on brain death and organ donation and, in particular, the public’s lack of knowledge surrounding brain death determination when making donation decisions.31-35 Studies have demonstrated that some people feel that if they agree to organ donation for their loved one, those patients may be diagnosed as dead too soon.17,52 One study showed that although 80.1% of family members would allow for organ donation after the death of a consenting relative, this rate dropped by 20% when the word death was substituted with brain death, revealing a lack of either understanding or acceptance of the concept and their legal equivalence.20 Four recently published empirical studies found that the greater the knowledge of brain death and organ donation, the more families shared a positive impression or attitude toward donation.31-33,35
A Latvian study found that study participants had widely different preferences concerning death determination criteria between higher brain, whole brain, or circulatory criteria. Interestingly, participants preferred less restrictive criteria for both their own death determination and organ transplantation than for their relatives (P < 0.001).41 Similarly, Siminoff et al17 illustrated how the general public have different conceptions of death than medical criteria, for example, brain death is a technical and medical term to signify a person is dead by neurological criteria. However, brain death is also used in common language as meaning that a patient is severely brain injured.17 The fact that a sizable number (60% of the sample) of people were willing to donate organs of people who were not legally dead is of importance and suggests that more education is necessary to further educate the public to better understand the concept.17
Implications for Public Trust and Legal Variabilities
Public trust in the healthcare system and its providers is an essential factor for public buy-in to brain death regulation and for the public to subsequently trust in the brain death diagnosis.19,23,53,54 In instances where there is a lack of trust in the healthcare system, there is decreased support for and trust in the brain death diagnosis. This was especially found in Eastern countries like Japan and China, where there have been past or present physician–patient conflicts,49,52-54 with surveys in Japan showing only a 40% support for defining brain death as legal death.49 Racial minorities in Western countries have also shown to have less support for brain death, attributable to decreased trust in the healthcare system.3,18,39 This distrust seems to have persisted despite legal and medical acceptance of brain death, thus suggesting that trust in healthcare providers and the medical system may be a more significant factor for public buy-in to brain death than the legal status of the diagnosis.25 DuBois and Schmidt found that the general public is hesitant to have death be determined through legal criteria. In contrast, a significant proportion (66%) trusted the healthcare system, and several suggested that the criteria for determining death should be undertaken by physicians and the public instead of the law.25
Legal variability in the determination of brain death may also give a sense of arbitration that perpetuates the confusion and mistrust in the diagnosis. This has fueled many high-profile court cases challenging it, which may contribute to increased erosion of public trust in the concept.8 For example, in the United States, the legal standard for brain death determination is variable between states, with a few (ie, New Jersey, California, New York) recognizing moral or religious objections to the determination of brain death to varying degrees and occasional deferral to the circulatory criteria.8
On the contrary, a Polish survey found that trust in the brain death diagnosis among nonmedical respondents was significantly lower than medical respondents (38.5% versus 78.5%),19 which could not be solely explained by lack of knowledge. Doubts over the criteria itself (31.5%) and distrust of medical staff’s education (25%) and objectivity (20%) also contributed.19 Educational background was also shown to affect the level of trust.19,40 Joffe et al40 found that medical students were less likely than nursing or philosophy students to trust that physicians were truthful in describing DCD patients as dead.
Ultimately, when lack of trust among the general public exists, several key concerns have also been linked, including that brain death may be erroneously and prematurely diagnosed, that the patient will not be dead at the time of organ donation, that care may be withheld or prematurely terminated in favor of organ donation,10,20,39,44,49,55 or that they themselves were uncertain about the concept of brain death.19,20
One potential solution in situations where there is a lack of trust in healthcare providers could be to obtain independent confirmation of the diagnosis to have family present at the time of brain death assessment and diagnosis,9 including during temporary ventilator disconnection that occurs as part of brain death determination. Such an approach may help families better understand and accept brain death.46 Building the public’s trust in the reliability of the diagnosis seems to be pivotal to increasing their acceptance of brain death.19
Data from other countries have shown that public consultation may further intensify the rift and be ineffective for achieving a resolution. Despite significant public discourse and legal changes favoring brain death determination, brain death remains a highly controversial topic among the public, such as in Japan.28 Similarly, in Denmark, after brain death was opened up for public examination, the result, surprisingly, was greater uncertainty and lower organ donation rates, despite the huge economic investment by the government to sponsor large public hearings, public debates, educational films, and programs on national television.23,48
Media, Colloquialisms, and Brain Death
The majority of references identified with respect to media representations of death typically focus on brain death.5,10,19,22-24,27,31,55-58 Brain death is often used colloquially and represented in the media, shown on the news or in medical dramas on television (see Table 4). The depiction of brain death via the media is one of the most significant factors in spreading awareness of the brain death concept among the public. One study showed that 85% of students who had already heard of brain death had heard of it from the media (35.7% from television, 8.3% from radio, 41.2% from the internet),24 whereas another showed that because of televised medical dramas, families sometimes felt a personal realization that their relative had died, even before the medical confirmation of brain death.22 In a nationwide Turkish survey, adult participants identified that their main source of information about brain death was the television, and 85% of participants indicated that they refused to consent to donating organs of family members declared brain dead.31
TABLE 4.
Media representation and impact on public understanding of brain death (n = 12)
| References | Type of article | Country | Comments |
|---|---|---|---|
| Al Bshabshe et al24 | Quantitative/Survey | Saudi Arabia | Eighty-five percent of students who had heard about BD got information from the media sources (35.7% from television, 8.3% from radio, 41.2% from the internet, and 14.6% from friends). |
| Akbulut et al31 | Quantitative/Survey | Turkey | Only 47.2% of participants said they had inadequate information about BD, and 85.2% refused to consent to donating organs of family members declared brain dead. The majority of participants said they got their information about BD from television. |
| Crippen5 | Review | United States | Misleading media statements and terminology such as “sleeping,” “on life support,” and interpretation of movement as life as well as sensational media headlines color the concept of BD. |
| Daoust and Racine38 | Qualitative/Focus Group | Canada | Analysis of 940 American and Canadian newspaper articles showed similarities in their coverage of BD. It showed that BD is used colloquially in 39% (n = 366) of articles and the medical meaning is infrequently defined (2.7% and 3.6% in the United States and Canada). NDD criteria are mentioned in <10%, and life support in 20%. There is a need to bridge media representations of NDD with experts’ views. The media often misunderstands that BD is not death until cessation of cardiopulmonary functions. |
| Febrero et al27 | Quantitative/Survey | Spain | Knowledge of BD was not associated with having received information through audiovisual means (radio, daily press, magazines, films, advertising hoardings) or talks in education centers. It was associated only with having received negative information through television, which led to a worse knowledge of BD compared with when no information was received through television (36% vs 41%). |
| Haddow22 | Qualitative/Focus Group | United Kingdom | Semistructured interviews with 19 Scottish donor families revealed that many participants knew about brain stem death from televised medical dramas. This previous awareness from medical dramas helped relatives gain a personal realization of when death had occurred, sometimes even before the medical confirmation. |
| Kilcullen55 | Review | United States | Media significantly influences public view of organ donation, often mischaracterizing BD and fostering confusion (medical shows like Grey’s Anatomy, major newspapers). |
| Knox58 | Review | Australia | Screen representations evidence the preoccupation, culturally with mechanisms by which individual identity may be preserved in death. |
| Laureys56 | Narrative/Opinion | Belgium | Misleading term of BD as suggesting 2 different types of deaths may explain public and professional confusion about BD. Much of the controversy results from confusion/ignorance by the public or policy-makers about the medical reality of BD. |
| Long23 | Qualitative/Focus Group | United Kingdom | Qualitative studies show that use of terminology like “kept alive on a ventilator” and “life support” to describe BD undermines the message that death was inevitable. |
| Nowak et al19 | Quantitative/Survey | Poland | The media has reported instances of patients in a persistent vegetative state spontaneously awakening; however, this has been misrepresented as awakening from BD. |
| Pope10 | Review | United States | Families regularly bring lawsuits to mandate continued physiological support, religious objections, or just mistrusts the diagnosis. Confusion in how media reports on BD has damaged public confidence. Reports of genuine BD misdiagnosis/premature diagnosis (intention or negligent) have received intense media coverage and subsequently caused public alarm. |
| Thomas57 | Narrative/Opinion | Australia | Public debate about BD often leads to oversimplified media statements, with the potential to undermine public support for organ donation. |
BD, brain death; NDD, neurological determination of death.
On the other hand, it is apparent that although the media plays an important role in shaping the views of death, it does not often provide an accurate representation of either its definitions or implications. When brain death is discussed in the news, the actual diagnostic criterion is rarely mentioned, and when it is, it is often misrepresented as purely the cessation of cardiorespiratory function.38 The media has also played a significant role in perpetuating distrust over the irreversibility of brain death, with reports of patients in a persistently vegetative state spontaneously awakening being confused with the brain death state and undermining trust in the diagnosis.19 Popular medical dramas like Grey’s Anatomy have also been found to misrepresent and dramatize reality by exploiting and perpetuating people’s fears of having organs recovered for transplantation while falsely declared brain dead.55
Furthermore, the language around death and dying used in the media continues to perpetuate the confusion and misunderstandings among the general public17,23 and to further degrade public confidence.10 For example, terminology such as “sleeping,” “being kept alive on the ventilator,” and being on “life support” grossly misrepresents an individual who is brain dead, and the use of such terms undermines the message that death has already occurred.5,23
Headlines in the media are often either sensationalized or oversimplified, which further colors the public’s understanding and perception of brain death.5,57 Media reports of rare cases of genuine misdiagnosis of brain death have received intense coverage that has harmed public perceptions.10 Studies have found that receiving negative information on brain death from television was in fact associated with less acceptance of brain death as actual death of the patient than among those who did not receive such information from television.27,31
DISCUSSION
The 64 references identified in this scoping review revealed important themes and highlighted gaps in the literature regarding the public’s perceptions of death and death determination. Although the public generally concedes the concept of brain death (ie, they accept it), their overall understanding is poor. More specifically, public misunderstanding stems more from confusion about the medical and legal facts concerning death determination, particularly in brain death cases.3,11,17-37,41,45 Death in the context of organ donation introduced more complexity.10,17,20,31-35,40,42,43,56 A recent literature review indicates that “the existing data on public attitudes regarding brain death and organ donation reflect substantial public confusion” about medical and legal facts,59 which is not surprising given the complexity of this issue. More specifically, in the context of a brain death diagnosis, a family member’s acceptance of the diagnosis of death “of someone who is still breathing and whose heart is still beating seems to violate a basic understanding of what constitutes life.”45 Freeman45 explains that it takes an “unnatural leap of faith to understand brain death cognitively based on the word of a complete stranger, rather than based on direct observation.”
The media acts to further confuse the general public with loose use of terminology and portrayals of death in medical dramas and newspapers, which are often sensationalized, oversimplified, or inaccurate in their representation of death.22,24,31 It is important to ensure that there is adequate public education and awareness of brain death and also that the sources and quality of the information more closely match reality. Data suggest that the public generally concedes the concept of brain death, that is, they accept the diagnosis from physicians; it is important to note that this is not a uniform finding. Specific countries/contexts/populations may be less accepting of this definition of death. Limited global data resulting from our search criteria make drawing conclusions impossible.
More empirical inquiry needs to focus on understanding the public’s attitudes and perceptions on death in the contexts of death determination by neurological and circulatory criteria, as well as ongoing public understanding of the distinctions between death determination and organ donation. More investigation into determining the optimal strategy for ongoing, meaningful public engagement on this topic is needed. Only 2 empirical studies in this review, 1 Canadian40 and 1 American,44 explored the views of participants regarding understanding of death and death determination from a circulatory determination perspective.40,44 Interestingly, this review has served to highlight the fact that public engagement alone may not lead to a more cohesive and unified definition of death, suggesting that how the public is engaged may be just as important as if they are engaged. From experiences of other countries such as in Denmark and Japan, a lesson learned is that in itself, increasing the involvement of the general public in the debates and legislation around death determination may not necessarily increase public acceptance and may perpetuate heated discourse not necessarily based on a strong conceptual foundation.10,23,48,53,60,61
In contrast, the public should not be overlooked in attempting to implement health-related policy. As Bruni et al62 noted, “the public is the most important stakeholder in the healthcare system” and “members of the public can provide a crucial perspective about the values of a community which should lead to higher quality decisions in priority setting.” And, preserving public trust in healthcare providers and the medical system in general should be one of a country’s highest priorities.
Limitations
Although comprehensive in scope, the review was limited to English language publications. Also, we are limited in that our review search was conducted until July 31, 2021, and as a result, we may have missed articles published after that initial search. Finally, our search strategy included studies that focused on the public’s understanding of death and death determination both outside of and within the context of organ donation and transplantation that may have an impact on the attitudes of people in these studies.
CONCLUSIONS
This scoping review provides a comprehensive overview of the published literature related to the general public’s understanding and attitudes toward neurological and cardiocirculatory determination of death. We have affirmed that the literature on the public’s understanding of death and death determination is closely linked to the organ donation and transplantation domain, and there need to be ongoing efforts to clarify the processes surrounding death determination and organ donation practices. We have identified a need for empirical research, in particular Canadian research, on the attitudes and views of the public on death determination with specific focus on death by circulatory determination. The issue around public trust in healthcare providers and the healthcare systems and the impact of popular media on the awareness and understanding of brain death have both significantly impacted how death determination is perceived by the general public. In particular, trust in healthcare providers and the medical system at large may be a more significant factor for public buy-in to death determination than the legal status of the diagnosis. There is much to be learned from experiences of other countries with public engagement around death determination. However, as part of any initiative for general understanding, the public should be consulted in death determination discussions, and thus, any agenda for death determination must engage with and include the public representation.
ACKNOWLEDGMENTS
Thank you to Robin Featherstone and Risa Shorr, both information specialists, for their expertise in crafting and executing search strategies. We would also like to thank our peer reviewers for their insightful comments and recommendations.
Supplementary Material
Footnotes
This study was funded by Canadian Blood Services and Health Canada via the Canadian Critical Care Society.
L.H. is a paid consultant for Canadian Blood Services. The other authors declare no conflicts of interest.
All authors have made substantial contributions to the conception and design of this study. Similarly, all authors have contributed equally to the analysis of data and drafting of the text for this article. All authors are in agreement to be accountable for all aspects of this work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Supplemental digital content (SDC) is available for this article. Direct URL citations appear in the printed text, and links to the digital files are provided in the HTML text of this article on the journal’s Web site (www.transplantationdirect.com).
REFERENCES
- 1.Shemie SD, Hornby L, Baker A, et al. ; The International Guidelines for Determination of Death phase 1 participants, in collaboration with the World Health Organization. International guideline development for the determination of death. Intensive Care Med. 2014;40:788–797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Greer DM, Shemie SD, Lewis A, et al. Determination of brain death/death by neurologic criteria: the World Brain Death project. JAMA. 2020;324:1078–1097. [DOI] [PubMed] [Google Scholar]
- 3.Bernat JL. Whither brain death? Am J Bioeth. 2014;14:3–8. [DOI] [PubMed] [Google Scholar]
- 4.Brierley J. UK court accepts neurological determination of death. Lancet. 2015;385:2254. [DOI] [PubMed] [Google Scholar]
- 5.Crippen D. Changing interpretations of death by neurologic criteria: the McMath case. J Crit Care. 2014;29:870–871. [DOI] [PubMed] [Google Scholar]
- 6.De Georgia MA. History of brain death as death: 1968 to the present. J Crit Care. 2014;29:673–678. [DOI] [PubMed] [Google Scholar]
- 7.Luce JM. The uncommon case of Jahi McMath. Chest. 2015;147:1144–1151. [DOI] [PubMed] [Google Scholar]
- 8.Pope T. Brain death and the law: hard cases and legal challenges. Hastings Cent Rep. 2018;48(suppl 4):S46–S48. [DOI] [PubMed] [Google Scholar]
- 9.Pope TM. Brain death forsaken: growing conflict and new legal challenges. J Leg Med. 2017;37:265–324. [DOI] [PubMed] [Google Scholar]
- 10.Pope TM. Legal briefing: brain death and total brain failure. J Clin Ethics. 2014;25:245–257. [PubMed] [Google Scholar]
- 11.Bernat JL. The concept and practice of brain death. Prog Brain Res. 2005;150:369–379. [DOI] [PubMed] [Google Scholar]
- 12.Lewis A. Contentious ethical and legal aspects of determination of brain death. Semin Neurol. 2018;38:576–582. [DOI] [PubMed] [Google Scholar]
- 13.Peters MD, Godfrey CM, Khalil H, et al. Guidance for conducting systematic scoping reviews. Int J Evid Based Healthc. 2015;13:141–146. [DOI] [PubMed] [Google Scholar]
- 14.Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for Scoping Reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169:467–473. [DOI] [PubMed] [Google Scholar]
- 15.Friedrich AB. More than “spending time with the body”: the role of a family’s grief in determinations of brain death. J Bioeth Inq. 2019;16:489–499. [DOI] [PubMed] [Google Scholar]
- 16.Johnson LSM. The case for reasonable accommodation of conscientious objections to declarations of brain death. J Bioeth Inq. 2016;13:105–115. [DOI] [PubMed] [Google Scholar]
- 17.Siminoff LA, Mercer MB, Arnold R. Families’ understanding of brain death. Prog Transplant. 2003;13:218–224. [DOI] [PubMed] [Google Scholar]
- 18.Siminoff LA, Burant C, Youngner SJ. Death and organ procurement: public beliefs and attitudes. Kennedy Inst Ethics J. 2004;14:217–234. [DOI] [PubMed] [Google Scholar]
- 19.Nowak E, Pfitzner R, Koźlik P, et al. Brain death versus irreversible cardiac arrest—the background and consequences of young people’s opinions on stating death in Polish transplantology. Transplant Proc. 2014;46:2530–2534. [DOI] [PubMed] [Google Scholar]
- 20.Tessmer CS, da Silva AR, Barcellos FC, et al. Do people accept brain death as death? A study in Brazil. Prog Transplant. 2007;17:63–67. [DOI] [PubMed] [Google Scholar]
- 21.Lewis A, Pope TM. Physician power to declare death by neurologic criteria threatened. Neurocrit Care. 2017;26:446–449. [DOI] [PubMed] [Google Scholar]
- 22.Haddow G. The phenomenology of death, embodiment and organ transplantation. Sociol Health Illn. 2005;27:92–113. [DOI] [PubMed] [Google Scholar]
- 23.Long T. Brain-based Criteria for Diagnosing Death: What Does it Mean to Families Approached About Organ Donation? [doctoral thesis]. University of Southhampton; 2007. [Google Scholar]
- 24.Al Bshabshe AA, Wani JI, Rangreze I, et al. Orientation of university students about brain-death and organ donation: a cross-sectional study. Saudi J Kidney Dis Transpl. 2016;27:966–970. [DOI] [PubMed] [Google Scholar]
- 25.DuBois JM, Schmidt T. Does the public support organ donation using higher brain-death criteria? J Clin Ethics. 2003;14:26–36. [PubMed] [Google Scholar]
- 26.DuBois JM, Anderson EE. Attitudes toward death criteria and organ donation among healthcare personnel and the general public. Prog Transplant. 2006;16:65–73. [DOI] [PubMed] [Google Scholar]
- 27.Febrero B, Ríos A, Martínez-Alarcón L, et al. Knowledge of the brain death concept among adolescents in southeast Spain. Transplant Proc. 2013;45:3586–3588. [DOI] [PubMed] [Google Scholar]
- 28.Febrero B, Ros I, Almela-Baeza J, et al. Knowledge of the brain death concept among older people. Transplant Proc. 2020;52:506–508. [DOI] [PubMed] [Google Scholar]
- 29.Ríos A, López-Navas AI, Flores-Medina J, et al. Ecuadorian population residing in Spain and their knowledge of brain death concept. Transplant Proc. 2020;52:432–434. [DOI] [PubMed] [Google Scholar]
- 30.Ríos A, López-Navas AI, Flores-Medina J, et al. Knowledge of the brain death concept among the Puerto Rican population residing in Florida. Transplant Proc. 2020;52:449–451. [DOI] [PubMed] [Google Scholar]
- 31.Akbulut S, Ozer A, Gokce A, et al. Attitudes, awareness, and knowledge levels of the Turkish adult population toward organ donation: study of a nationwide survey. World J Clin Cases. 2020;8:2235–2245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lim KJ, Cheng TTJ, Jeffree MS, et al. Factors influencing attitude toward organ and tissue donation among patients in primary clinic, Sabah, Malaysia. Transplant Proc. 2020;52:680–686. [DOI] [PubMed] [Google Scholar]
- 33.Ríos A, Carrillo J, López-Navas AI, et al. Does knowledge of the concept of brain death affect the attitude toward donation of Algerians residing in Spain? Transplant Proc. 2020;52:465–468. [DOI] [PubMed] [Google Scholar]
- 34.Stadlbauer V, Zink C, Likar P, et al. Family discussions and demographic factors influence adolescent’s knowledge and attitude towards organ donation after brain death: a questionnaire study. BMC Med Ethics. 2020;21:57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tarzi M, Asaad M, Tarabishi J, et al. Attitudes towards organ donation in Syria: a cross-sectional study. BMC Med Ethics. 2020;21:123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ríos A, López-Navas A, López-López A, et al. Do Spanish medical students understand the concept of brain death? Prog Transplant. 2018;28:77–82. [DOI] [PubMed] [Google Scholar]
- 37.Ríos A, López-Navas AI, Carrillo J, et al. Population of Cienfuegos (Cuba) and their knowledge about the concept of brain death: multivariate analysis of the associated psychosocial factors. Transplant Proc. 2020;52:480–483. [DOI] [PubMed] [Google Scholar]
- 38.Daoust A, Racine E. Depictions of ‘brain death’ in the media: medical and ethical implications. J Med Ethics. 2014;40:253–259. [DOI] [PubMed] [Google Scholar]
- 39.DuBois JM, Waterman AD, Iltis A, et al. Is rapid organ recovery a good idea? An exploratory study of the public’s knowledge and attitudes. Am J Transplant. 2009;9:2392–2399. [DOI] [PubMed] [Google Scholar]
- 40.Joffe AR, Byrne R, Anton NR, et al. Donation after cardiac death: a survey of university student opinions on death and donation. Intensive Care Med. 2009;35:240–247. [DOI] [PubMed] [Google Scholar]
- 41.Neiders I, Dranseika V. Minds, brains, and hearts: an empirical study on pluralism concerning death determination. Monash Bioeth Rev. 2020;38:35–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pessoa SFP, Barroso VS, Duarte AV, et al. Public knowledge and attitudes toward organ donation and transplantation: a survey from a medium-sized Brazilian city. Transplant Proc. 2020;52:1223–1225. [DOI] [PubMed] [Google Scholar]
- 43.Siminoff LA, Burant C, Youngner SJ. Death and organ procurement: public beliefs and attitudes. Soc Sci Med. 2004;59:2325–2334. [DOI] [PubMed] [Google Scholar]
- 44.Verble M, Worth J, Gulli L, et al. A study of concerns of families of potential donation after circulatory death donors and recommendations for raising donation rates. Transplant Proc. 2020;52:2867–2876. [DOI] [PubMed] [Google Scholar]
- 45.Freeman TB. Death perception: how temporary ventilator disconnection helped my family accept brain death and donate organs. Narrat Inq Bioeth. 2015;5:9–12. [DOI] [PubMed] [Google Scholar]
- 46.Long T, Sque M, Addington-Hall J. Conflict rationalisation: how family members cope with a diagnosis of brain stem death. Soc Sci Med. 2008;67:253–261. [DOI] [PubMed] [Google Scholar]
- 47.Veatch RM. Abandon the dead donor rule or change the definition of death? Kennedy Inst Ethics J. 2004;14:261–276. [DOI] [PubMed] [Google Scholar]
- 48.Crowley-Matoka M, Arnold RM. The dead donor rule: how much does the public care.and how much should we care? Kennedy Inst Ethics J. 2004;14:319–332. [DOI] [PubMed] [Google Scholar]
- 49.Asai A, Kadooka Y, Aizawa K. Arguments against promoting organ transplants from brain-dead donors, and views of contemporary Japanese on life and death. Bioethics. 2012;26:215–223. [DOI] [PubMed] [Google Scholar]
- 50.Bastami S, Matthes O, Krones T, et al. Systematic review of attitudes toward donation after cardiac death among healthcare providers and the general public. Crit Care Med. 2013;41:897–905. [DOI] [PubMed] [Google Scholar]
- 51.Volk ML, Warren GJ, Anspach RR, et al. Foreigners traveling to the U.S. for transplantation may adversely affect organ donation: a national survey. Am J Transplant. 2010;10:1468–1472. [DOI] [PubMed] [Google Scholar]
- 52.Long T, Sque M, Addington-Hall J. What does a diagnosis of brain death mean to family members approached about organ donation? A review of the literature. Prog Transplant. 2008;18:118–125. [DOI] [PubMed] [Google Scholar]
- 53.Chua HC, Kwek TK, Morihara H, et al. Brain death: the Asian perspective. Semin Neurol. 2015;35:152–161. [DOI] [PubMed] [Google Scholar]
- 54.Yang Q, Miller G. East-West differences in perception of brain death. Review of history, current understandings, and directions for future research. J Bioeth Inq. 2015;12:211–225. [DOI] [PubMed] [Google Scholar]
- 55.Kilcullen JK. “As good as dead” and is that good enough? Public attitudes toward brain death. J Crit Care. 2014;29:872–874. [DOI] [PubMed] [Google Scholar]
- 56.Laureys S. Science and society: death, unconsciousness and the brain. Nat Rev Neurosci. 2005;6:899–909. [DOI] [PubMed] [Google Scholar]
- 57.Thomas AG. Continuing the definition of death debate: the report of the president’s council on bioethics on controversies in the determination of death. Bioethics. 2012;26:101–107. [DOI] [PubMed] [Google Scholar]
- 58.Knox SL. Death, afterlife, and the eschatology of consciousness: themes in contemporary cinema. Mortality. 2006;11:233–252. [Google Scholar]
- 59.Shah SK, Kasper K, Miller FG. A narrative review of the empirical evidence on public attitudes on brain death and vital organ transplantation: the need for better data to inform policy. J Med Ethics. 2015;41:291–296. [DOI] [PubMed] [Google Scholar]
- 60.Racine E. Revisiting the persisting tension between expert and lay views about brain death and death determination: a proposal inspired by pragmatism. J Bioeth Inq. 2015;12:623–631. [DOI] [PubMed] [Google Scholar]
- 61.Kato Y. Conscience in health care and the definitions of death. Croat Med J. 2013;54:75–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Bruni RA, Laupacis A, Martin DK; University of Toronto Priority Setting in Health Care Research Group. Public engagement in setting priorities in health care. CMAJ. 2008;179:15–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.