Abstract
With nearly 36% of hand fractures occurring at the metacarpal, a variety of treatment interventions have been developed. Although many nondisplaced metacarpal fractures can be treated with conservative management, displaced, unstable, open, and extra-articular fractures require surgical attention. Compared with open reduction with plate fixation, closed reduction with intramedullary fixation has shown advantages of a simplified technique, minimal soft tissue dissection, and reduced tendon irritation and scar formation. The current study reports on the improved surgical technique associated with the use of novel instrumentation for the closed reduction and intramedullary fixation of extra-articular metacarpal fractures. The design and surgical technique of the premeasured Secure Intramedullary Nail improves fracture fixation, minimizing rotation and backing out, while reducing concerns for soft tissue irritation complications at the base of the metacarpal. Our reported case series suggests procedural efficiency, a low complication rate, and fast recovery for those with indicated extra-articular fractures.
Key words: Fracture, Intramedullary, Metacarpal, Trauma
Hand fractures are the second most common fracture of the upper extremity.1 With nearly 36% of hand fractures occurring at the metacarpal, a variety of interventions have been developed to treat these injuries.2,3 Although many nondisplaced metacarpal fractures can be treated with conservative management, displaced, unstable, open, and extra-articular fractures require surgical attention.4 Current concepts have been described for the surgical fixation of unstable, displaced, and multiple metacarpal fractures including intramedullary nail (IM Nail) fixation, open reduction internal fixation (ORIF), and a variety of plate and screw fixation techniques.2,3 Open reduction with plate fixation and closed reduction with intramedullary fixation (CRIF) have been reported to have comparable functional outcomes for extra-articular metacarpal fractures.5, 6, 7, 8 However, intramedullary fixation provides the advantages of a simplified technique, minimal soft tissue dissection, a smaller incision, reduced tendon irritation, and decreased scar formation.8
Foucher5 first introduced CRIF using flexible IM Nails in 19769 before introducing the bouquet technique in 1995.5 However, the bouquet technique’s indications for solely transverse shaft and neck fractures limits a surgeons ability to treat spiral or comminuted fractures with this intervention.5 Since then, multiple intramedullary fixation devices and techniques have been described in the literature, including both locking and unlocking IM Nail systems for the treatment of all fracture types of the metacarpal neck, shaft, and base.6,7,10, 11, 12 More recently, Orbay11 and Orbay and Touhami12 reported on the use of flexible, locked IM Nails for the treatment of unstable metacarpal fracture types.11,12 With this technique, the IM Nail is percutaneously introduced into the medullary cavity fixating the fracture, and the proximal end of the nail is bent, locked, cut, and buried.11 The locked IM Nail design prevents metacarpal shortening and backing out of the nail during rehabilitation.11,12 In addition, it allows for the use of a single nail, compared with unlocked nails that required multiple nails to fixate one fracture.12
When using this technique, Mirza et al7 found a 10% complication rate of IM Nail backing out, tendon irritation, and one case of a tendon rupture.7 These complications required either revision or nail removal.7 Mirza et al also reported that patients commonly reported experiencing postoperative prominence and swelling near the base of the metacarpal. It is suggested that these complications were the fault of the protruding bent nail causing tendon irritation at the metacarpal base. Currently, we present an improved IM Nail fixation technique for the use of a premeasured IM Nail system that eliminates the need to bend, cut, and lock the IM Nail. This technique offers the same benefits of minimally invasive fixation of metacarpal fractures and early mobilization, without the concerns regarding backing out or soft tissue irritation.
Surgical Anatomy
With a dorsal approach to the carpometacarpal joint, attention must be paid to the extensor digitorum communis tendons and the dorsal sensory branches of the radial and ulnar nerves. During dissection, it is important to identify the extensor tendons and retract them away from the base of the metacarpal of focus. When approaching the bases of metacarpals 1, 2, and 3, one should also be aware of the dorsal sensory branches of the radial nerve. Contrarily, when dissecting at the bases of metacarpals 4 and 5, one should be cautious of the dorsal sensory branches of the ulnar nerve. Naturally, the medullary cavity of the fourth metacarpal is narrow. One should be cognizant of this when treating a fourth metacarpal fracture with a 1.6-mm IM Nail. It is suggested to use a 1.2-mm nail if this is the case.
Indications and Contraindications
Indications for premeasured IM Nail fixation of metacarpal fractures includes displaced and nondisplaced fractures of the metacarpal shaft, base, or neck: transverse, oblique, spiral, comminuted, and boxer’s fractures. This technique should be considered for all fractures when CRIF is feasible and/or ORIF is not desired. Malunions, chronic fractures, and thumbs are all good indications for the premeasured IM Nail technique. In cases in which multiple digits of the same hand are fractured, this is a great indication to use premeasured IM Nails. Premeasured IM Nail fixation is also indicated in select cases of unstable soft tissue envelopes where ORIF may further damage already compromised tissue. Compared with multiple plate fixations, performing IM Nail fixation on multiple fractures of the same hand allows for reduced morbidity, dissection, tendon irritation, and surgical time.8 Contraindications include infection, intra-articular fractures, highly comminuted fractures, and fractures irreducible by CRIF. Metacarpals with medullary cavities less than 1.2 mm in diameter are also not indicated.
Surgical Technique
Surgeries are performed on an outpatient basis under local anesthesia and a forearm tourniquet. Patients are placed in a supine position on the operating table with the arm fully extended, and the hand is placed pronated with a bolster underneath. The Secure IM Nail system (A.M. Surgical, Inc, Smithtown, NY) includes premeasured IM Nails measuring 1.6 or 1.2 mm in diameter and ranging from 40 to 60 mm in length, a custom-designed clamp, and an awl. The fracture is first manually reduced under fluoroscopic guidance. A bone clamp may be used to hold the closed reduction, particularly in cases of spiral fractures in which reduction is more challenging. Radiologic assessment and measurements are done before surgery to determine the correct IM Nail length and diameter to use. Nail size can also be determined during surgery by using a radiolucent tool, such as a freer, and fluoroscopy to measure the length of the suspected metacarpal (Fig. 1). Confirmation of the correct nail length and diameter may be assessed during surgery by placing the IM Nail over the suspected metacarpal and using fluoroscopy to guide the selection. The determined nail should be 3 to 5 mm shorter than the length of the metacarpal, and measurement of the medullary canal should be made to confirm that a 1.6-mm-diameter nail shaft will fit. In cases in which the medullary canal is too narrow for a 1.6-mm nail, a 1.2-mm nail should be considered.
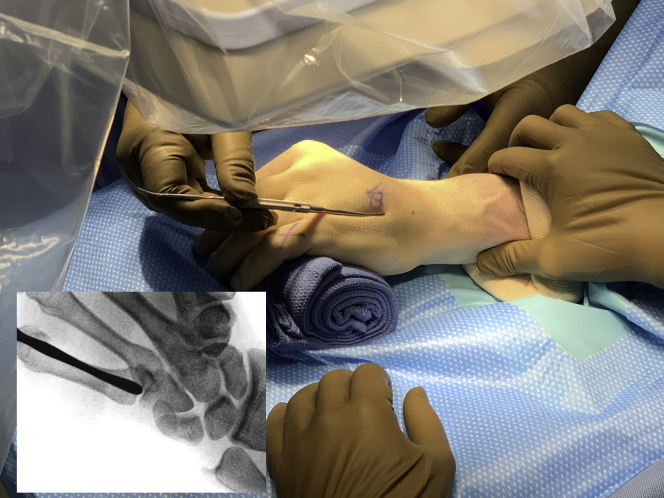
Figure 1.
A radiolucent tool (freer) and fluoroscopy are used to intraoperatively measure the length of the suspected metacarpal.
A 1- to 2-cm longitudinal incision is then made at the base of the suspected metacarpal. Superficial dissection is performed down to the dorsal cortex, exposing the carpometacarpal joint. The extensor tendons are identified and retracted while making sure any dorsal branches of the radial or ulnar nerves are protected. To access the medullary cavity, a custom awl is used to penetrate 3 to 5 mm through the proximal metaphysis and a unicortical pilot hole is made at the base of the metacarpal (Fig. 2). During this process, fluoroscopic images should be taken to ascertain the location of the awl and confirm its location in the medullary cavity (Fig. 2). Care is taken not to penetrate the far cortex. Once confirmed, the awl is gently removed.
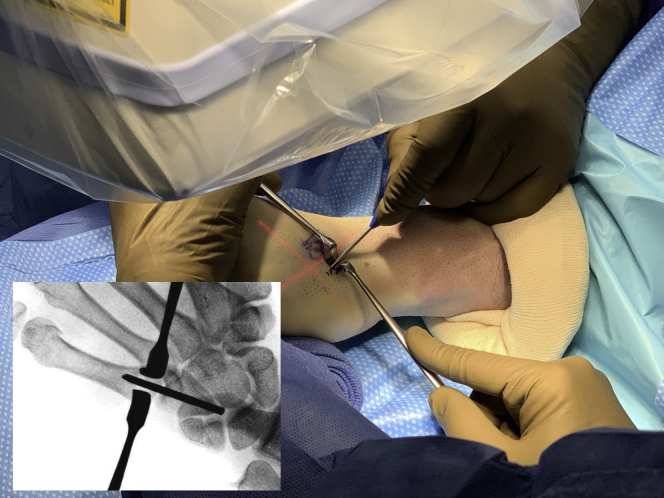
Figure 2.
To access the medullary cavity of the metacarpal, under fluoroscopic guidance, a custom awl is used to penetrate 3 to 5 mm through the proximal metaphysis.
Using the custom-designed clamp, the premeasured IM Nail is driven through the pilot hole into the medullary cavity (Fig. 3A). A different clamp may be used as long as it can securely accommodate the hemispheric cap of the premeasured IM Nail. Under fluoroscopic guidance, the custom clamp is used to twist and push the IM Nail gently through the cavity. It is important that the fracture be sufficiently reduced before driving the nail across the fracture site (Fig. 3B). The nail is passed though the fracture site into the distal fragment until the distal aspect of the nail reaches the distal metaphysis (Fig. 3C). Care is taken to avoid penetrating the subchondral bone of the distal metaphysis. If there is difficulty engaging the medullary cavity of the distal fragment, the procedure may be repeated. Under extenuating circumstances, the fracture could be opened with a small incision to guide the nail into the distal fragment.
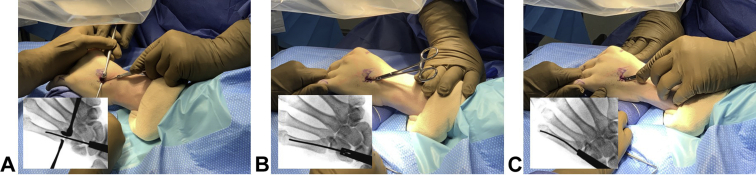
Figure 3.
A After removal of the awl, a customary clamp is used to aid in securely inserting the IM Nail. B The IM Nail is driven through the medullary cavity under fluoroscopic guidance. C The IM Nail is driven past the fracture site until the distal aspect of the nail reaches the distal metaphysis.
The operating surgeon has the choice of leaving the nail buried or removing the nail after fracture healing. To bury the nail, a bone tamp can be used to drive the proximal head of the IM Nail as tightly as possible to the base of the metacarpal, fixated within the periosteum. To allow for easy removal, the head of the IM Nail can be left proud and proximal to the base of the metacarpal, but beneath the extensor tendons. Intraoperative anteroposterior and oblique radiographs are taken again to confirm proper placement (Fig. 4); once confirmed, the wound is thoroughly irrigated. The wound is then closed with a subcuticular closure and the patient’s hand is placed in an ulnar gutter orthosis.
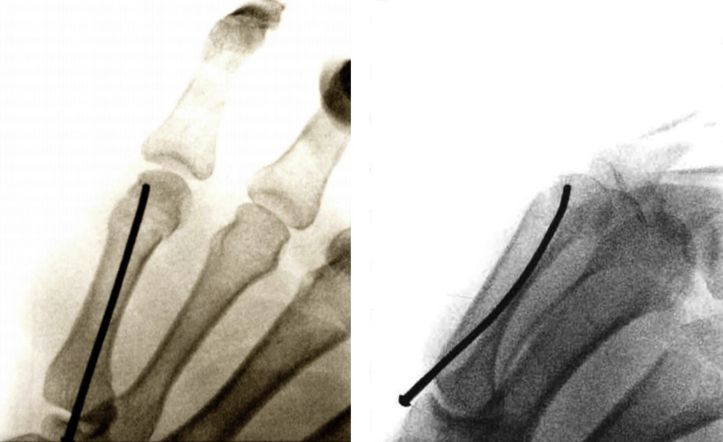
Figure 4.
Intraoperative A anteroposterior and B oblique radiographic images are taken to confirm the placement of the IM Nail.
Postoperative Management
The patient is brought back 5 to 7 days later in the office for a change of dressing. Wounds are inspected and the patient is placed in a custom-made orthosis. For fractures of the metacarpal base, a short-arm orthosis is applied, which frees the metacarpophalangeal (MCP), proximal interphalangeal (PIP), and distal interphalangeal (DIP) joints, and the involved fingers are placed together in an orthosis. For metacarpal shaft or neck fractures, a hand-based orthosis immobilizing the MCP joint is applied. For fractures located at the base of the metacarpal, the wrist should be immobilized in a volar orthosis, leaving the MCP, PIP, and DIP joints free. If the fracture is located at the midshaft, the wrist and MCP joints are immobilized in a volar orthosis and the PIP and DIP joints are left free. Fractures located at the distal third of metacarpal, the wrist, and the PIP and DIP joints can be free; however, the MCP joint should remain immobilized. It is always advisable to placed the affected finger together with an adjacent uninjured finger in an orthosis. At this point, occupational therapy is prescribed and patients are instructed to begin active range of motion (AROM) exercises. Active range of motion should be evaluated at 4 weeks, 8 to 12 weeks, and 6 months after surgery. Strength exercises should progress with radiographic healing.
At 4 weeks after surgery, x-rays are taken in the office to observe maintenance of reduction and fracture healing. If the patient is compliant after 6 weeks, the custom orthosis is removed and worn only for high-risk activities. At 8 to 12 weeks, the patient returns for a follow-up visit and another set of x-rays is taken. Upon fracture union, we recommend removing the IM Nail in younger, more active patients. Otherwise, the nail does not require removal.
Case Series
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008. Informed consent and approval of photography were obtained from all patients for inclusion in the study. There was no external source of funding for this study.
A single-institution, retrospective chart review was performed on all patients who underwent this technique for the treatment of metacarpal fractures from January 2018 to September 2019. We analyzed 17 patients with 18 metacarpal fractures who met our inclusion criteria of a reducible metacarpal fracture(s), no concomitant injuries or additional procedures on the affected hand, and follow-up of at least 8 weeks. Patients were examined before and after surgery at 5 to 7 days, 4 weeks, 8 to 12 weeks, and 6 months. Patient objective clinical outcome measures were collected after surgery by our in-house occupational therapist, and subjective outcome measures were recorded both before and after surgery. Objective outcome measures included grip and pinch strengths, AROM of the wrist, and total active motion of the phalanges. Patient subjective outcome measures included visual analog scale pain scores from 0 to 10 and Disabilities of the Arm, Shoulder, and Hand (DASH) questionnaire.
All surgeries were performed by our authors (A.M. and J.B.M). Eleven males and 6 females, mean age 39.7 years (range, 14–68 years) were included in our retrospective analysis. Most injuries were of the dominant hand and of the little finger (Table 1). The most common fracture type was an oblique fracture, and the most prominent fracture location was fractures of the metacarpal shaft (Table 1). Patient healing time is defined as the time taken to obtain clinical healing (no localized tenderness) and radiographic healing (callus formation). On average, patient fractures took 6.7 weeks to heal, and there were no cases of delayed unions or nonunions (Table 2). Figure 5 shows a case illustration of typical patient healing. Seventeen patients had the IM Nail(s) removed after surgery (Table 2). The one patient who did not have the nail removed was satisfied with the outcome and opted against a removal procedure. One patient from the cohort was treated for multiple metacarpal fractures in the same hand, experienced further displacement of one fracture, and required a revision (Fig. 6). No patients from the cohort experienced complications of malrotation, extensor tendon irritation, tendon rupture, or nerve complications.
Table 1.
Patient Demographics
| Variable | Value |
|---|---|
| Age, y (mean [range]) | 39.7 (14–68) |
| Gender, n (%) | |
| Male | 11 (65) |
| Female | 6 (35) |
| Injured hand, n (%) | |
| Right | 12 (71) |
| Left | 5 (29) |
| Injured hand, n (%) | |
| Dominant | 12 (71) |
| Nondominant | 5 (29) |
| Injured metacarpal, n (%) | |
| Thumb | 0 |
| Index | 0 |
| Middle | 0 |
| Ring | 2 (11) |
| Little | 16 (89) |
| Fracture type, n (%) | |
| Transverse | 4 (22) |
| Comminuted | 5 (28) |
| Oblique | 9 (50) |
| Spiral | 2 (11) |
| Fracture location, n (%) | |
| Shaft | 12 (67) |
| Neck | 6 (33) |
| Base | 0 |
| Multiple metacarpal fractures | 1 (6) |
Table 2.
Surgical Outcomes
| Variable | Value |
|---|---|
| Time to surgery, d (mean [SD]) | 7.4 (0.7) |
| Operating time, min∗ (mean [SD]) | 23.8 (9.5) |
| Tourniquet time, min∗ (mean [SD]) | 33.4 (12.8) |
| Healing time, wk (mean [SD]) | 6.7 (2.1) |
| Delayed Unions, n (%) | 0 |
| Nonunions, n (%) | 0 |
| Revisions, n (%) | 1 (6) |
| Removal of hardware, n (%) | 17 (94) |
| Removal of hardware time, wk (mean [SD]) | 8.9 (3.2) |
| Follow-up, wk (mean [SD]) | 11.8 (4.2) |
For treatment of a single metacarpal fracture. Excludes a patient (n = 1) who had multiple metacarpal fractures treated.
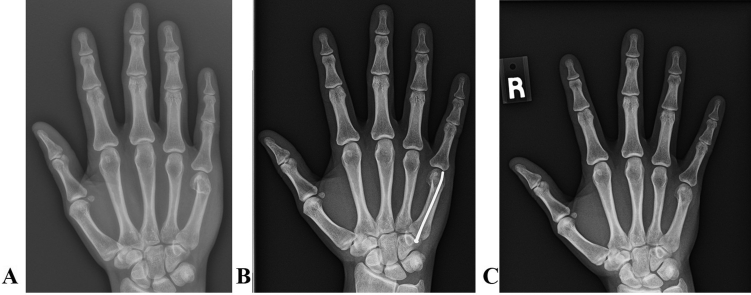
Figure 5.
A 27-year-old woman presented to our office with pain after slipping and falling onto an outstretched dominant right hand. A After preoperative x-rays, she received the diagnosis of an oblique neck fracture of the fifth metacarpal to be treated with IM Nail fixation. B After surgical IM Nail Fixation, x-rays at 4 weeks after surgery show proper fixation of the fractured metacarpal and progressed healing. At 7.9 weeks, full fracture healing was attained and the nail was subsequently removed. C Images at final follow-up (12 weeks) show a full union and anatomical healing. The patient reported a DASH score of 1.7 at final follow-up.
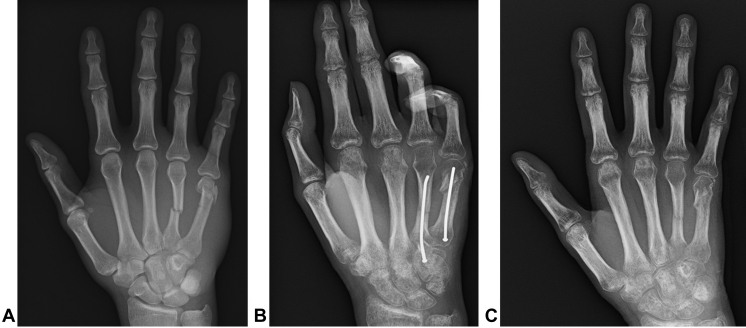
Figure 6.
A 20-year-old man presented to our office with in the dominant right hand after a snowboarding accident. A Preoperative x-rays showed a transverse shaft fracture of the fourth metacarpal and a comminuted neck fracture of the fifth metacarpal. Both fractures were treated with IM Nail fixation in the same procedure. After presenting 2 weeks later with further displacement of the fifth metacarpal fracture and migration of the nail, a revision procedure was performed in which the fifth metacarpal fracture was closed reduced and fixated with a new IM Nail. B X-rays 10 weeks after surgery from the initial procedure (8 weeks after revision) show complete healing in both fractures. The IM Nails were subsequently removed. C Images at 12 weeks (10 weeks after revision) show maintained healing and anatomical reduction. The patient reported a DASH score of 0.8 at final follow-up (6 months).
Table 3 shows average postoperative recovery in subjective and objective clinical outcome measures at 4 weeks and 8 to 12 weeks. Because of fast healing and the retrospective nature of our study, patients were typically satisfied with the outcomes at 8 to 12 weeks and were often lost to follow-up afterward. Therefore, we did not have enough data to report properly on 6-month postoperative outcomes. On average, AROM of the wrist returned to normal limits at 4 weeks (Table 3). Compared with normal limits of 260°,13 phalangeal total active motion improved after surgery from 4 weeks to 8 to 12 weeks (Table 3). At 8 to 12 weeks, patient grip and pinch strength recovered to slightly over 70% compared with their contralateral, uninjured hand (Table 3). Patient visual analog scale pain scores decreased from before surgery to 4 weeks after surgery, and patients reported almost no pain by 8 to 12 weeks (Table 3). Similarly, patient DASH scores improved from before surgery to 4 weeks after surgery, and even further at 8 to 12 weeks (Table 3).
Table 3.
Postoperative Recovery in Subjective and Objective Outcome Measures at 4 Wk and 8 to 12 Wk∗
| Variable | 4 Wk | 8–12 Wk |
|---|---|---|
| Wrist AROM (normal limits) (degrees) | ||
| Dorsiflexion (40° to 80°) | 64.3 | 65.8 |
| Volar flexion (30° to 70°) | 53.8 | 64 |
| Radial deviation (10° to 30°) | 21.8 | 29.3 |
| Ulnar deviation (20° to 40°) | 24.8 | 28.8 |
| Phalangeal total active motion (degrees) | 207.5 | 254.2 |
| Grip and pinch strength (% recovery) | ||
| Gross grasp | 74.6 | |
| Lateral pinch | 74.7 | |
| Precision pinch | 72.1 | |
| Visual analog scale pain score | 1.7† | 0.7 |
| DASH questionnaire | 30.4‡ | 9.9 |
All outcomes are presented as mean values. Percent recovery of grip and pinch strength are compared with the contralateral, uninjured side (8–12 weeks after surgery). Normal limits for phalangeal total active motion: 260°.13
Improved visual analog scale score compared with mean preoperative value (5.8).
Improved DASH score compared with mean preoperative value (57.6).
Pearls and Pitfalls
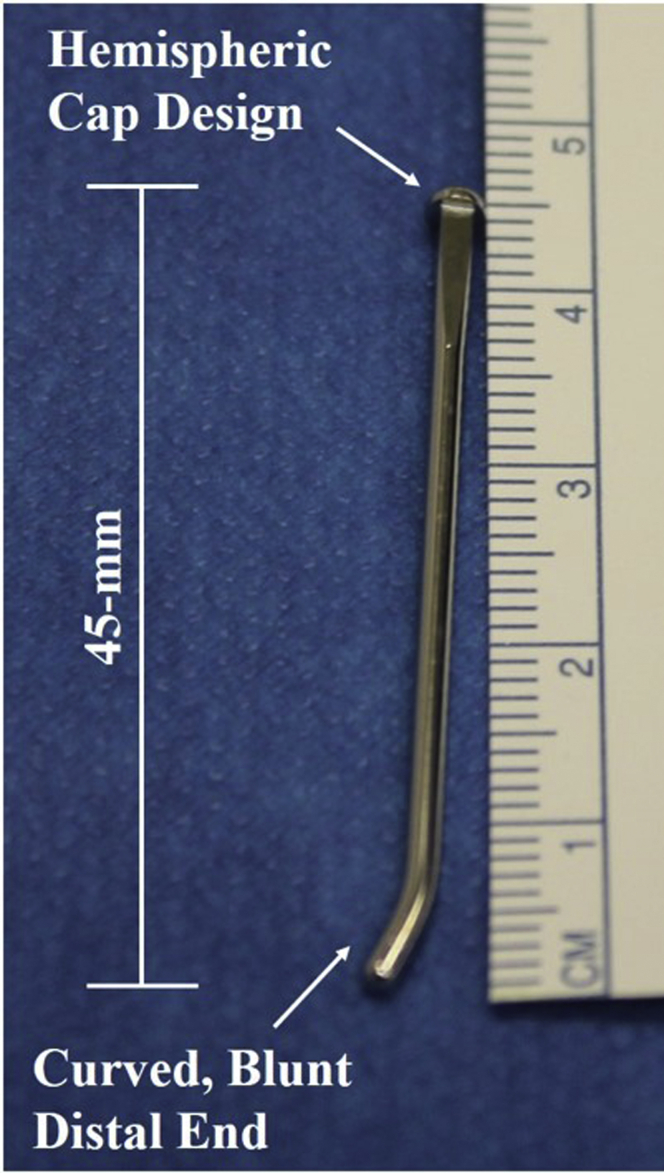
Intramedullary nail fixation provides a minimally invasive and less complex technique, faster surgical time, less morbidity, and equal fixation compared with ORIF with plates and screws.8 A smaller, less-invasive incision allows for minimal soft tissue dissection and clear visualization of the extensor tendons and nerves at the wrist, and leaves a cosmetically appealing scar. Compared with previous IM Nail techniques and instrumentation, the premeasured Secure IM Nail system offers the main advantage of no longer needing to lock, clip, or bend the IM Nail to accommodate for varying metacarpal lengths. With previous instrumentation, after fixation, a sharp articulation from the clipped IM Nail would remain proximal to the medullary canal entrance, causing tendon irritation and patient discomfort. Instead, the Secure IM Nail is equipped with a hemispheric cap at its proximal end, which simplifies insertion and eliminates concerns regarding postoperative tendon irritation (Fig. 7). The hemispheric cap design also provides dynamic use of the IM Nail. in which a surgeon can choose to safely bury the base of the nail within the metacarpal periosteum for non-removal or leave the nail protruding proximal to the metacarpal base for easy access upon removal without concerns regarding extensor tendon irritation. Furthermore, the Secure IM Nail has a curved distal tip that strengthens fixation, preventing backing out and rotation, and no longer requires a locking technique (Fig. 7). The distal tip is also blunt, to help prevent penetration of the nail into the subchondral bone of the distal fragment. Overall, the premeasured Secure IM Nail system allows for a simpler technique than those previously described5,6,9,11 while reducing many concerns regarding fracture indication, fixation, backing out, and tendon irritation. A final benefit of the premeasured Secure IM Nail system is that it is cost-effective and cheaper compared with similar intramedullary techniques and implants currently available.
Figure 7.
Premeasured intramedullary nail with a proximal hemispheric cap design to prevent tendon irritation and a curved, blunt distal end to secure fixation.
Complications
The greatest concern with this technique is the potential injury to nearby vulnerable anatomy. Care must be taken to identify and retract extensor tendons and small neurovascular structures such as the subcutaneous nerves when dissecting down to the metacarpal base. For this reason, we prefer to use a minimally open incision of 1 to 2 cm instead of taking a percutaneous approach to achieve clear visualization of vulnerable anatomy. In the case of fracture fixation, comminuted fractures should be treated with caution. If anatomical reduction cannot be obtained using a closed technique, the fixation can be assessed open. At this point, it is the surgeon’s discretion whether to thread the IM Nail in an open fashion or abandon the intramedullary method altogether and treat with plate and screws. Patients with larger medullary cavities and/or osteoporotic patients should be treated with multiple nails to obtain proper fixation. This can be done using 2 1.6-mm nails, one 1.6-mm and one 1.2-mm nail, or 2 1.2-mm nails. Finally, care must be taken not to penetrate the distal end of the IM Nail through the metaphysis of the metacarpal head. The blunt and rounded end of the Secure IM Nail helps to prevent this from occurring, but special care should be taken with osteoporotic or soft bone.
Conclusions
The presented technique proposes both novel instrumentation and a method for the minimally invasive treatment of unstable metacarpal fractures. Premeasured IM Nail fixation provides the ability to fixate all metacarpal fracture types while avoiding complications of malunion, fracture displacement, extensor tendon rupture or irritation, and backing out. Our preliminary case series shows the effectiveness of the premeasured IM Nail, because it provides patients with good clinical outcomes as early as 8 to 12 weeks after surgery. It is our belief that the premeasured IM Nail is not only a simpler, more cost-effective technique than those previously described, it offers patients the benefit of early mobilization and fast recovery. We hope that our technique article and case series will advance the intramedullary treatment protocol for unstable metacarpal fractures, eliminating common concerns associated with previous techniques such as extensor tendon or dorsal sensory nerve injuries.
Acknowledgments
We would like to thank Patricia A. Meyer, MOT, OTR/L, CHT for exceptional occupational therapy work, postoperative evaluations, and assisting with the final versions of the manuscript. We would also like to acknowledge A.M. Surgical, Inc for covering publication fees for this technique article.
Footnotes
Declaration of interests: Drs A. Mirza and J.B. Mirza are associated with or financially involved with A.M. Surgical, Inc. No benefits in any form have been received or will be received by the other author related directly or indirectly to the subject of this article.
Supplementary Data
References
- 1.Karl J.W., Olson P.R., Rosenwasser M.P. The epidemiology of upper extremity fractures in the United States, 2009. J Orthop Trauma. 2015;29(8):e242–e244. doi: 10.1097/BOT.0000000000000312. [DOI] [PubMed] [Google Scholar]
- 2.Cheah A.E., Yao J. Hand fractures: indications, the tried and true and new innovations. J Hand Surg Am. 2016;41(6):712–722. doi: 10.1016/j.jhsa.2016.03.007. [DOI] [PubMed] [Google Scholar]
- 3.Meals C., Meals R. Hand fractures: a review of current treatment strategies. J Hand Surg Am. 2013;38(5):1021–1031. doi: 10.1016/j.jhsa.2013.02.017. quiz 1031. [DOI] [PubMed] [Google Scholar]
- 4.Diaz-Garcia R., Waljee J.F. Current management of metacarpal fractures. Hand Clin. 2013;29(4):507–518. doi: 10.1016/j.hcl.2013.09.004. [DOI] [PubMed] [Google Scholar]
- 5.Foucher G. “Bouquet” osteosynthesis in metacarpal neck fractures: a series of 66 patients. J Hand Surg Am. 1995;20(3 part 2):S86–S90. doi: 10.1016/s0363-5023(95)80176-6. [DOI] [PubMed] [Google Scholar]
- 6.Gonzalez M.H., Igram C.M., Hall R.F., Jr. Flexible intramedullary nailing for metacarpal fractures. J Hand Surg Am. 1995;20(3):382–387. doi: 10.1016/S0363-5023(05)80091-7. [DOI] [PubMed] [Google Scholar]
- 7.Mirza A., Mirza J., Healy C., Mathew V., Lee B. Radiographic and clinical assessment of intramedullary nail fixation for the treatment of unstable metacarpal fractures. Hand (N Y) 2018;13(2):184–189. doi: 10.1177/1558944717695747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ozer K., Gillani S., Williams A., Peterson S.L., Morgan S. Comparison of intramedullary nailing versus plate-screw fixation of extra-articular metacarpal fractures. J Hand Surg Am. 2008;33(10):1724–1731. doi: 10.1016/j.jhsa.2008.07.011. [DOI] [PubMed] [Google Scholar]
- 9.Foucher G., Chemorin C., Sibilly A. A new technic of osteosynthesis in fractures of the distal 3d of the 5th metacarpus [in French] Nouv Presse Med. 1976;5(17):1139–1140. [PubMed] [Google Scholar]
- 10.Gonzalez M.H., Hall R.F., Jr. Intramedullary fixation of metacarpal and proximal phalangeal fractures of the hand. Clin Orthop Relat Res. 1996;(327):47–54. doi: 10.1097/00003086-199606000-00008. [DOI] [PubMed] [Google Scholar]
- 11.Orbay J. Intramedullary nailing of metacarpal shaft fractures. Tech Hand Up Extrem Surg. 2005;9(2):69–73. doi: 10.1097/01.bth.0000167253.31976.95. [DOI] [PubMed] [Google Scholar]
- 12.Orbay J.L., Touhami A. The treatment of unstable metacarpal and phalangeal shaft fractures with flexible nonlocking and locking intramedullary nails. Hand Clin. 2006;22(3):279–286. doi: 10.1016/j.hcl.2006.02.017. [DOI] [PubMed] [Google Scholar]
- 13.Rayan G., A E. 4th ed. Wolters Kluwer Health; Philadelphia, PA: 2011. The Hand: Anatomy, Examination, and Diagnosis. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.