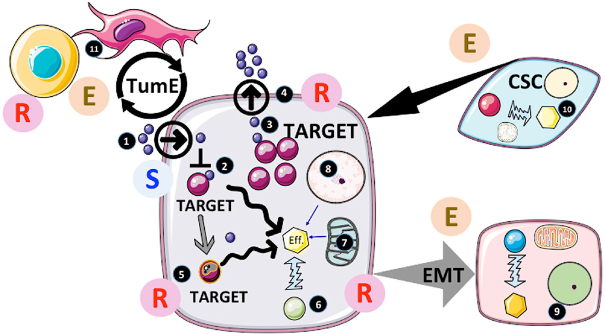
Figure 1.
Actors and factors implicated in cancer resistance to treatments. 1. The accessibility of the drug to cancer cells is usually determined during clinical assays (pharmacokinetics, pharmacodynamics…). In the case of intracellular targeting, the transit of the drug across the plasma membrane can also be critical and is usually tested during pre-clinical studies. However, the drug distribution can be affected by both elements in the tumor microenvironment (TME) as well as by changes in the body response, which will result in resistance by forfeit; 2. If the drug is delivered and affects the activity of the target, several factors could intervene modifying the structure of the drug and/or its delivery to another compartment (e.g., endosomes) thereby decreasing its efficiency. If the target is upstream of a major cellular effector (Eff.) responsible for cancer progression, other pathways can be activated to sustain this activity. This would result in circumventing the treatment efficacy and induce escape; 3. Overexpression of the target would also limit the efficiency of the inhibitor and trigger resistance if an increased dose (due to side-effects) is not possible; 4. If the drugs were substrates of the multidrug resistance (MDR) pumps, activation of MDR would limit the intracellular concentration and impede its therapeutic activity; 5. One of the most-documented resistance mechanisms is mutation of the target as often observed with tyrosine kinase inhibitors (TKI) such as EGFRi or BRAFi. Per se, mutated cells insensitive to treatment slowly emerge from the treated tumor mass and become predominant after an initial tumor regression. Of note, the process implicated is still not completely understood (preexisting clones, induced mutations or selected random mutations); 6. Another common process observed with TKI is the bypassing of the target for the activation of the effector. Often another tyrosine kinase pathway can be amplified to compensate for the inhibition of the target. In addition, deep modifications of the cellular phenotype/genotype induced by the treatment directly or indirectly can also contribute to resistance; 7. Mitochondria are central to resistance through two distinct processes. First by rewiring metabolism; cancer cells can adapt to the inhibitory effects on target under many circumstances (providing alternative sources of core elements for the cells to proliferate such as nucleic acids, amino acids, ATP sources…) or epigenetic modifiers (see below). Secondly, mitochondria are central to apoptosis and other cell death programs[44]. Consequently, modification of mitochondrial activity can also play an active role in cancer cell survival through the life/death response following the inhibition/modulation of target. In fact, resistance to apoptosis is one of the hallmarks of cancer and plays an important role in in the escape by cancer cell to immune-surveillance; 8. Cancer genome modifications can occur through DNA mutations as mentioned but also through changes in epigenetic regulation such as miRNA production, DNA methylation and histone modifications. In this respect the metabolic input is of major importance providing key co-factors called oncometabolites, which includes alpha keto-glutarate or succinate necessary for the function of epigenetic enzymes. These oncometabolites participate in the cellular reprogramming often observed under the selective pressure induced by treatments[93]; 9. Another phenomenon triggered by the treatment is the epithelial-mesenchymal transition (EMT). EMT is a well-known process in the context of pathophysiological conditions, such as repair of injured tissue. EMT leads to the dissolution of cell-cell contacts, morphogenetic changes, increased motility and invasiveness. In cancer, EMT is accompanied by metabolic, epigenetic, and differentiation reprograming, all of which participate in drug resistance[94]. In GBM, a transition to mesenchymal phenotype is often observed[95]. This EMT-like process provides a selective advantage to cancer cells culminating in an escape from treatment[96]; 10. In many tumors (but not all), the existence of cells with some “stem cell” properties (such as stem cells markers, self-renewal, high DNA repair capacity, resistance to cell death) has been shown. Because of the aforementioned properties, cancer stem cells (CSC) have been proposed to be the cornerstone of both cancer heterogeneity and treatment resistance and the main culprit responsible for recurrence[87]; 11. Tumor microenvironment (TME) is an essential component of cancer growth and survival. The implication of TME in cancer resistance as well as sensitivity to treatment has been proposed[96]. Non-tumor cells present in the microenvironment are multiple and thus a change in TME composition is likely to influence cancer response to therapy in both ways (i.e., escape and resistance). TME can secrete factors or directly provide elements by cell-cell interactions that could participate in tumor growth and acquisition/selection of resistant cells[96]. In addition, it should be kept in mind that immune cells are part of TME and that cancer cells usually inhibit their function. The actual importance and role of TME still needs more evaluation but it is clear that it represents a major axis of research for new therapies. E: escape; R: resistance; S: sensitivity to treatment