Abstract
The COVID-19 pandemic and its restrictions have led to a shift in how people connect with others. This study investigated (a) profiles of social contact change across social ties and modes of contact, (b) predictors of these profiles, and (c) the association between these profiles and mental health during the pandemic. Participants (N = 2,098; Age mean = 50.94, range = 18–98; 48.3% female) were surveyed online twice, once prior to the pandemic (January 31–February 10, 2020) and again early in the outbreak (March 18–29, 2020). A latent profile analysis identified profiles of social contact change across social ties and communication methods. Additional analyses identified predictors of group membership and their association with mental health. Three latent groups were identified: (1) the “majority group” (77%) slightly restricted in-person contact and had a small increase in phone and text use, (2) the “high technology use group” (13%) restricted in-person contact and increased the use of all technology-based methods, and (3) the “isolated group” (10%) decreased in both in-person and technology-based contact. Compared to the majority group, the high technology use group reported higher depression and anxiety, whereas the isolated group reported higher loneliness. There were three distinct profiles of how adults in the United States changed their communication patterns with others early in the pandemic that were linked to distinct patterns of mental health. The results have implications for the development and the delivery of mental health treatment in times of social (physical) distancing.
Keywords: coronavirus disease, COVID-19, loneliness, mental health, social contact, technology-based communication
Statement of Relevance:
With social distancing policies, people had to adjust the ways they connect with family, friends, and colleagues. This study examined a sample of Americans’ social contact change and usage of various communication technologies early in the COVID-19 pandemic. We found unique behavioral profiles that help understand how people maintain their personal relationships, select communication methods, and ultimately how these patterns are associated with mental health outcomes.
1 |. INTRODUCTION
The coronavirus that causes COVID-19 is highly contagious and has spread across the world. In the United States, “stay-at-home” orders were put in place to urgently control the spread of the virus in March 2020 (White House, 2020). The Centers for Disease Control and Prevention (CDC) advised the public to follow the “social distancing” guidelines to limit in-person contact with people outside of one’s household, work from home if possible, avoid large crowds or mass gatherings, and keep at least 6 feet apart in public spaces (CDC, 2020). While social distancing measures are vital for preventing the transmission of an infectious virus (Ahmed et al., 2018), vulnerable groups for severe illness due to COVID-19 (e.g., older adults, those with preexisting medical conditions) are at higher risk for social isolation and its mental health consequences (American Psychological Association, 2020; Brooks et al., 2020; Miller, 2020).
The limitation of in-person contact may have brought a massive shift in the ways people interact with each other. Those who are under the lockdown or following strict social distancing guidelines, for example, were expected to restrain from meeting others outside of their household, and they may have turned to technology-based communication tools to maintain social connection. Before the pandemic, the majority (96%) of Americans owned mobile phones (smartphones 81%; mobile phones 15%) and had access to the Internet (90%), suggesting that various technology-based communication methods are readily available to stay connected with social ties instead of face-to-face contact (Schumacher & Kent, 2020). Such communication technologies can be classified into synchronous (i.e., face-to-face, phone call, video chat) versus asynchronous (i.e., social media, Email) communication in terms of real-time connection or by the types (i.e., text, voice, video) and “richness” of the information transferred (Tillema et al., 2010). According to media richness theory (Daft & Lengel, 1984), the degree to which the modality can carry non-verbal information (e.g., vocal cues and facial expressions) affects whether the person can successfully maintain relationships using that modality. While in-person communication is richest in terms of verbal and non-verbal cues in high synchrony, technology-based communication modalities differ in their degree of social presence (Hall et al., 2021). Deciding which technology-based methods to use in place of in-person contact depend on relational roles, emotional closeness, and communication needs (Burholt et al., 2020; Westmyer et al., 1998). For instance, communication tools that can transmit nonverbal information in synchronous manner such as phone calls or video chat are more likely to be used in urgent matters and with relationally close social ties (Tillema et al., 2010). Asynchronous methods, such as emails, tend to play a larger role in maintaining formal or obligatory relationships (Tillema et al., 2010). In addition, the use of online-based communication methods may differ considerably by digital literacy and accessibility (van den Berg et al., 2012). Internet use, for example, is lower among those who are older, less affluent, have less education, are from a racial minority, and live in rural areas (Anderson et al., 2019).
People innately seek social contact to meet the needs for belonging and sense of closeness with others (Hall & Merolla, 2020). Less frequent social contact is associated with a 13% higher risk of mortality, independent of subjective loneliness (Shor & Roelfs, 2015). The effect of stay-at-home orders and social distancing on mental health may be due, in part, to limitations on in-person social contact. Social isolation imposed on a societal level is an unfamiliar experience to many people, which entails unwanted physical separation from close others and disruption in many daily activities (Usher et al., 2020). Before the pandemic, previous research has focused primarily on the effects of limited in-person contact on mental health among those experiencing higher levels of social isolation. For example, among midlife and older adults, those who meet infrequently with close others (every few months or less) were more likely to have depressive symptoms 2 years later than adults who had in-person contact at least once per month (Teo et al., 2015). In contrast, the frequency of phone calls and email use was not related to depressive symptoms (Teo et al., 2015). Similarly, frequent in-person contact with family and friends was robustly associated with less loneliness, whereas frequent online social contact was linked to higher loneliness (Luhmann & Hawkley, 2016). These findings suggest that in-person contact is a unique form of social contact that has stronger protective effects and that not all forms of social contact may effectively compensate for social distancing. Indeed, a survey of adults in the United States in March 2020 found that while three-quarters (76%) of Americans used email or messaging services, the majority of people (65%) reported that these communication tools would not replace face-to-face communications and some (8%) even stated that internet or phone use would not help much (Anderson & Vogel, 2020; Auxier, 2020). To this end, identifying patterns in social contact shifts, who adopts which changes in social contact, and whether these changes are protective for mental health and feeling connected is critical for understanding how the pandemic has changed interpersonal communication. Further, the communication patterns observed in this study will be informative for public health experts to develop strategies to support the mental health of the population.
1.1 |. The current study
The purpose of this study is threefold. First, we examine latent profiles of social contact change across social ties and mode of contact in response to the COVID-19 outbreak. Participants reported on the direction of change (more, same, less than before) with family, friends, and colleagues on in-person contact and five technology-based communication (phone, text, video chat, social networking services [SNS], Email). Second, we examine demographic, health, living arrangement, and general contact frequency predictors of the change profiles. Third, we investigate how profiles are linked to mental health (i.e., loneliness, depression, and anxiety) and emotional closeness with others during the early stages of the pandemic.
2 |. METHODS
2.1 |. Participants and procedure
The data come from the first two waves of a longitudinal survey with an online panel of US adults. Participants were recruited through Dynata (www.dynata.com) and invited to complete a Qualtrics survey. The sampling strategy was to include adults living in the United States with a roughly even distribution across all States, seven age brackets (18–19, 20–29, 30–39, 40–49, 50–59, 60–69, and 70 and older), 50% female, and 20% African American. The overall study is preregistered at https://osf.io/vqnh8; the current analysis is not included in the preregistration. Material and procedures were reviewed and approved by the Institutional Review Board of Florida State University.
The first wave of data collection was conducted between January 31 and February 10, 2020, with general questionnaires on well-being and health. This wave of the survey did not include any questions related to the COVID-19 pandemic. The physical and mental health variables from the first wave serve as baseline control. A total of 4078 participants completed the survey with valid responses. The second survey was administered between March 18–29, 2020, during the White House’s “15 Days to Slow the Spread” campaign (White House, 2020). The variables of interest for the current paper were included in this wave as part of the measures related to early behavioral and psychological responses to the pandemic.
In the second wave, n = 2,234 had valid responses in the survey (55.2% response rate from wave 1). Valid cases had no evidence of speeding (survey completion time less than 5 min) and straight-lining (giving the same response to measures that include reverse coded items) in both waves. We also excluded participants who reported inconsistent demographic variables across both waves (n = 56), those with missing data on all social contact change variables (n = 80). Thus, the final sample for the current study was 2,098 participants.
Compared to the final sample, participants without a second wave assessment or excluded due to data inconsistency were more likely to be female (χ2 = 46.26, p < .001), younger (Cohen’s d = .97, p < .001), had less education (d = .38, p < .001), more likely to be African American (χ2 = 31.08, p < .001), more likely to be Latinx ethnicity (χ2 = 52.66, p < .001), reported higher depressive symptoms (d = 0.40, p < .001), and higher loneliness at the first wave (d = 0.31, p < .001). There were no differences in the number of chronic diseases (d = .02, p = .464).
2.2 |. Measures
2.2.1 |. General frequency of social contact
At wave 2, participants were asked, “In general, how often do you communicate with your (a) family and relatives, (b) friends, and (c) colleagues?” For each of these three relationship types, frequency of contact using six different modes of communication was reported separately: meet in person, talk on the phone, text message, video chat (Facetime, WhatsApp etc.), SNS (Facebook, Twitter, or other social media), and email/write. The items were on a 7-point scale (1 = daily, 2 = several times a week, 3 = once a week, 4 = several times a month, 5 = at least once a month, 6 = every few months, and 7 = very rarely or never). Items were reversed coded so that higher scores indicated more frequent contact.
2.2.2 |. Change in frequency of social contact
The focus of the study was to capture self-reported changes in social contact patterns. The direction of change was directly asked in relation to the pandemic, rather than estimating change in comparison to general level of contact. As such, the direction of change in contact with close others during the pandemic was measured with the question, “Since the coronavirus outbreak, how has communication changed with your (a) family and relatives, (b) friends, and (c) colleagues?” Response options were 1 (less than before), 2 (same as before), and 3 (more than before). For each relationship type, the six modes of communications were asked separately.
2.2.3 |. Mental health
Loneliness and depressive symptoms were measured at both waves; anxiety and perceived change in emotional closeness to others were measured at wave 2.
Loneliness was measured with an 11-item version of the UCLA Loneliness scale (Hawkley et al., 2005; Russell, 1996). Items (e.g., “How much of the time do you feel that you lack companionship?”) were rated on a 3-point scale from 1 (hardly ever or never) to 3 (often). Loneliness was computed as the average of the 11 items; higher values indicated higher loneliness (Cronbach’s α W1 = .89, W2 = .88).
Depression was measured with the Patient Health Questionnaire-2 (PHQ-2; (Löwe et al., 2005). The PHQ-2 is a well validated depression screen with good criterion and convergent validity (Löwe et al., 2005). The stem question asked: “Over the last two weeks, how often have you been bothered by any of the following problems?” The two items were “little interest or pleasure in doing things” and “feeling down, depressed, or hopeless.” Response options ranged from 0 (not at all) to 3 (nearly every day). The sum was taken across the two items; higher scores indicated higher depressive symptoms (Cronbach’s α W1 = .84, W2 = .83).
Anxiety was measured with the 7-item Generalized Anxiety Disorder Scale (GAD-7; (Spitzer et al., 2006). The GAD-7 has high reliability and validity as a measure of anxiety for the general population (Löwe et al., 2008). Participants were asked how often, during the past 2 weeks, they were bothered by, for example, “feeling nervous, anxious or on edge,” “not being able to stop or control worrying” or “worrying too much about different things” on a 4-point scale that ranged from 0 (not at all) to 3 (nearly every day). The sum was taken across the seven items; higher scores indicated higher symptoms of anxiety (Cronbach’s α W2 = .94).
Perceived change in the emotional closeness to family and friends was measured with two items, “Since the coronavirus outbreak, I feel emotionally closer to my (a) family and relatives, (b) friends.” Each item was rated on a 3-point scale that was recoded into −1 (less than before), 0 (same as before), and 1 (more than before).
2.2.4 |. Covariates
Demographic, health, living arrangement, and quarantine status were included as covariates. Gender (0 = male, 1 = female), age (in years), education (on a 7-point scale from 0 = less than high school to 6 = PhD or equivalent), race (dummy coded variables were 1 = Black, 1 = Other, compared to 0 = White), and Latinx ethnicity (1 = Latinx, 0 = not Latinx), income (6 level; self-reported, on a scale from 0 = less than $20,000 to 5 = $100,000 or more), and working status1 (1 = currently working, 0 = not working). Disease burden was measured as the sum of 11 chronic health conditions reported at wave 1. Living arrangement (0 = does not live alone, 1 = lives alone) was assessed at wave 2 from report of household size, having children under age 18 at home (0 = no, 1 = yes), and having an older adult aged over 70 at home (0 = no, 1 = yes). Quarantine/isolation status was assessed at wave 2 with the question, “In the last month, I have been in quarantine/isolation because of the coronavirus (0 = no, 1 = yes).”
2.3 |. Analytic plan
Descriptive analyses were conducted in SPSS Version 25.0 (IBM, 2017). The main analyses were performed in a structural equation modeling framework using Mplus 8.3 (Muthén & Muthén, 1998–2017). Full-information maximum likelihood (FIML) method was used to account for the missing data (Enders, 2011). The analyses followed three steps.
First, latent profile analysis (LPA) was conducted to capture distinctive profiles of change in social contact with family, friends, and colleagues across six modes of communication reported by the participants at wave 2 (total of 18 indicators). The recoding scheme of change in social contact was −1 (less than before), 0 (same as before), and 1 (more than before), so that the scales are interpretable in terms of the direction of change in the LPA. A series of models were fitted sequentially that estimated one to six groups. A set of model fit indices was compared to select the optimal number of latent groups (Ram & Grimm, 2009). Models were compared with relative fit information criteria, the Bayesian information criteria (BIC), and sample-size adjusted BIC (ABIC). A better fitting model had lower values on these indices (Nylund et al., 2007). The entropy is a summary indicator that is useful to determine the confidence of class membership of each individual (Jedidi et al., 1993). The higher entropy value (ranging from 0.00 to 1.00) indicates adequate separation between the latent classes. The adjusted Lo–Mendell–Rubin likelihood ratio test (Adjusted LRT) was used to compare the number of classes. The significance (p < .05) indicated a model with c number of classes fit better than the model with one less (c-1) class (Lo et al., 2001; Nylund et al., 2007).
Second, multinomial logistic regression (MLR) models were used to examine how predictors were linked to the social contact change groups. Using one group as a reference, the model estimated the association of a given predictor and the relative probability of belonging to a particular group compared to the reference group. Predictors were the demographic factors, health, living arrangement, and the general frequency of social contact before the pandemic.
Finally, linear regression models examined whether different social contact change groups were associated with concurrent mental health outcomes (i.e., loneliness, depression, anxiety) and perceived change in emotional closeness to family and friends. Dummy variables were created to indicate the latent groups with the reference group as zero. Demographic variables were entered in the model as covariates. For loneliness and depression, the wave 1 measures were included as control variables. For all analyses, significance was set to p < .05.
3 |. RESULTS
3.1 |. Descriptive statistics
Descriptive statistics for the sample are in Table 1. The direction of change in social contact of participants in response to COVID-19 is presented in Figure 1. About one-half of participants reported meeting family (46%) and friends (50%) in person less than before. About one-third (37%) of participants reduced in-person meetings with colleagues. The majority of participants (69%–80%) reported using technology-based modes of contact at the same frequency as before the pandemic. Up to one-quarter of participants reported increases in phone calls and text messages with family and friends and phone calls, texting, and emailing with colleagues.
TABLE 1.
Study variable statistics for participants
| Mean or N | SD or % | Response range | |
|---|---|---|---|
| Demographic characteristics | |||
| Age (years) | 50.94 | 16.64 | 18–98 |
| Female | 1014 | 48.3% | |
| Race: White | 1447 | 69.0% | |
| Race: Black | 340 | 16.2% | |
| Race: Other | 311 | 14.8% | |
| Ethnicity: Latinx | 225 | 10.7% | |
| Educationa | 4.18 | 1.49 | 1–7 |
| Incomeb | 2.97 | 1.74 | 0–6 |
| Employment | 1192 | 56.8% | |
| Disease burden | 1.40 | 1.53 | 0–11 |
| Living arrangement | |||
| Living alone | 472 | 22.5% | |
| Children (age <18) in householdc | 571 | 35.1% | |
| Older adult (age ≥70) in householdc | 338 | 20.8% | |
| Quarantine/Isolation status | 512 | 24.4% | |
| General social contact frequency | |||
| Meet in-person: family | 4.32 | 2.08 | 1–7 |
| Meet in-person: friends | 4.05 | 1.96 | 1–7 |
| Meet in-person: colleagues | 3.72 | 2.47 | 1–7 |
| Technology-based contact: family | 20.48 | 7.51 | 5–35 |
| Technology-based contact: friends | 18.07 | 7.70 | 5–35 |
| Technology-based contact: colleagues | 14.88 | 9.06 | 3–35 |
| Mental health | |||
| Loneliness W1 | 1.74 | 0.51 | 1–3 |
| Loneliness W2 | 1.76 | 0.50 | 1–3 |
| Depression W1 | 1.29 | 1.66 | 0–6 |
| Depression W2 | 1.26 | 1.66 | 0–6 |
| Anxiety W2 | 4.95 | 5.54 | 0–21 |
| Perceived changes in emotional closeness | |||
| Family and relatives W2 | 0.18 | 0.51 | −1, 0, 1 |
| Friends W2 | 0.08 | 0.50 | −1, 0, 1 |
Note: N = 2,098. W1 = wave 1; January 31–February 10, 2020, W2 = wave 2; March 18–29, 2020.
Education was assessed on a scale from 1 (less than high school) to 7 (PhD or equivalent).
Income was measured on a scale from 0 (less than $20,000) to 5 ($100,000 or more).
Proportions are based on those who live with others (n = 1681).
FIGURE 1.
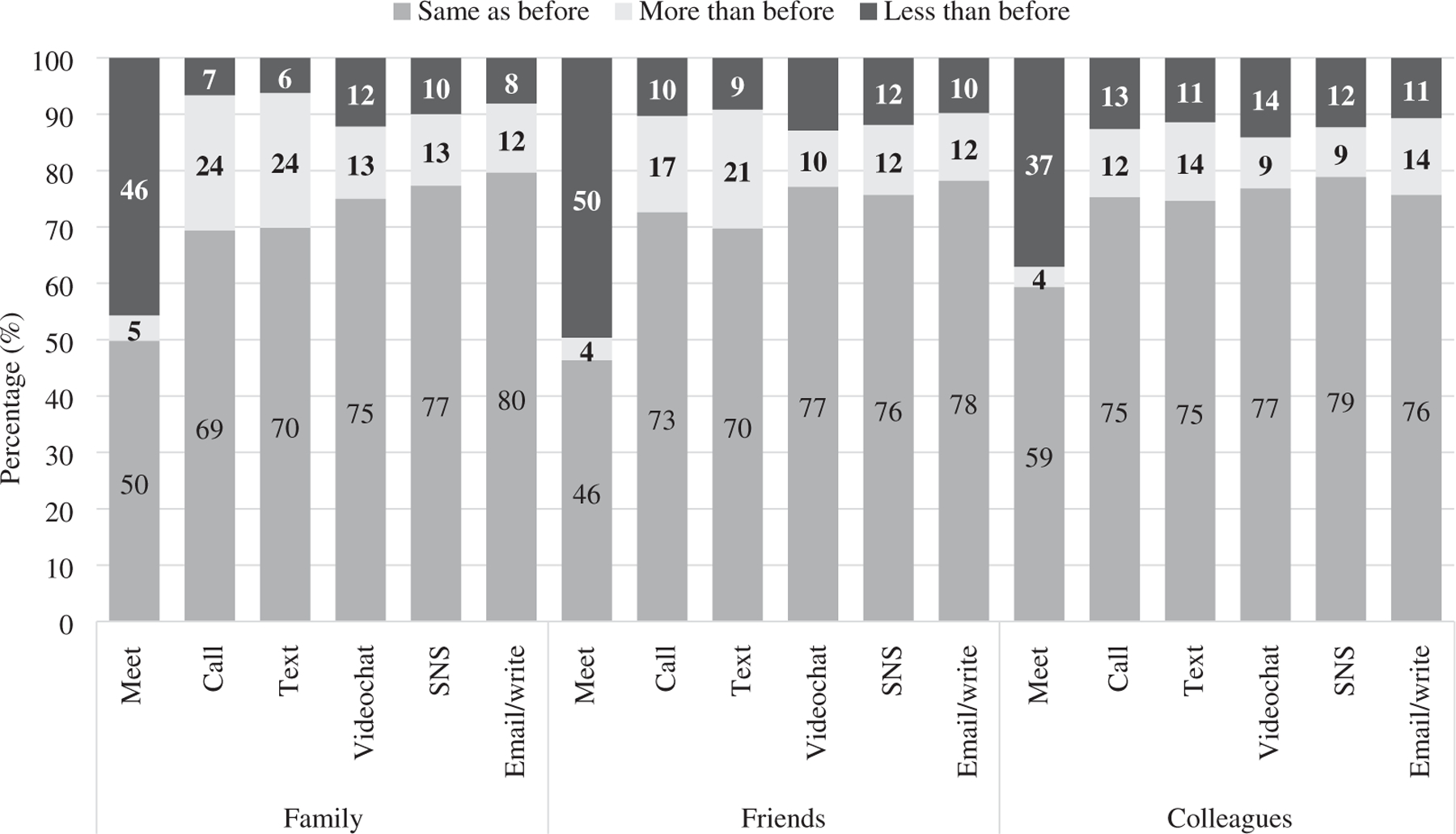
Direction of changes in social contact in response to COVID-19 outbreak
3.2 |. Profiles of social contact change across relationship type and communication mode
We explored the overall pattern of social contact change with family, friends, and colleagues across the six different modes of communication. Results of the latent profile analyses are in Table 2. Comparison of model fit indices suggested that the three-class or four-class solution had the best fit. Specifically, the gradual decrease in BIC and ABIC from of one- to six-solutions indicated that model fit generally improved. The significant LMR test showed that increasing the number of classes provided a better fit to the data when compared to the previous model until the four-class solution. Although each model had an entropy value above 0.80, the three-class model had the highest entropy value, which indicated the most confidence in the classification. The parsimonious three-class solution was chosen as the optimal model.
TABLE 2.
Latent profile analyses of changes in social contact across relationship types and mode of communication
| Fit index | 1 class | 2 classes | 3 classes | 4 classes | 5 classes | 6 classes |
|---|---|---|---|---|---|---|
| Number of parameters | 36 | 55 | 74 | 93 | 112 | 131 |
| Loglikelihood | −27233.642 | −24807.215 | −22619.029 | −22002.674 | −21495.991 | −21068.955 |
| BIC | 54742.639 | 50035.111 | 45804.065 | 44716.681 | 43848.641 | 43139.895 |
| ABIC | 54628.264 | 49860.371 | 45568.959 | 44421.211 | 43492.806 | 42723.695 |
| Entropy | — | 0.938 | 0.959 | 0.942 | 0.948 | 0.952 |
| LMR p value | — | 0.000 | 0.000 | 0.001 | 0.257 | 0.521 |
| Proportions of classesa | — | 83−17 | 77−13−10 | 70−15−10−6 | 69−14−7−6−4 | 67−13−6−6−4−4 |
Abbreviations: ABIC, sample size adjusted BIC; BIC, Bayesian information criterion; LMR, Lo-Mendel-Rubin test.
Class proportions for the latent classes based on their most likely latent class membership.
Patterns of social contact change of the three groups are illustrated in Figure 2. The largest group (76.8%; n = 1,612) had some proportions of participants reporting decrease in meeting family, friends, and colleagues in person and only increased slightly in technology-based modes of communication (primarily the use of phone and text with family and friends). This group was labeled the “majority group.” The second group (13.2%; n = 278) changed their social contact pattern drastically during the COVID-19 outbreak. This group had a significantly higher proportion of individuals reporting that they had reduced in-person contact with all three types of relationships and increased the use of technology-based contacts. This group was labeled the “high technology use group.” The third group was the smallest (9.9%; n = 208) and had higher proportions of participants restricting meeting with family, friends, and colleagues. Unlike the other groups, higher proportions of people in this group also reported decreasing contacts via all technology-based communication modes with their relationships, which led to the label, “isolated group.”
FIGURE 2.
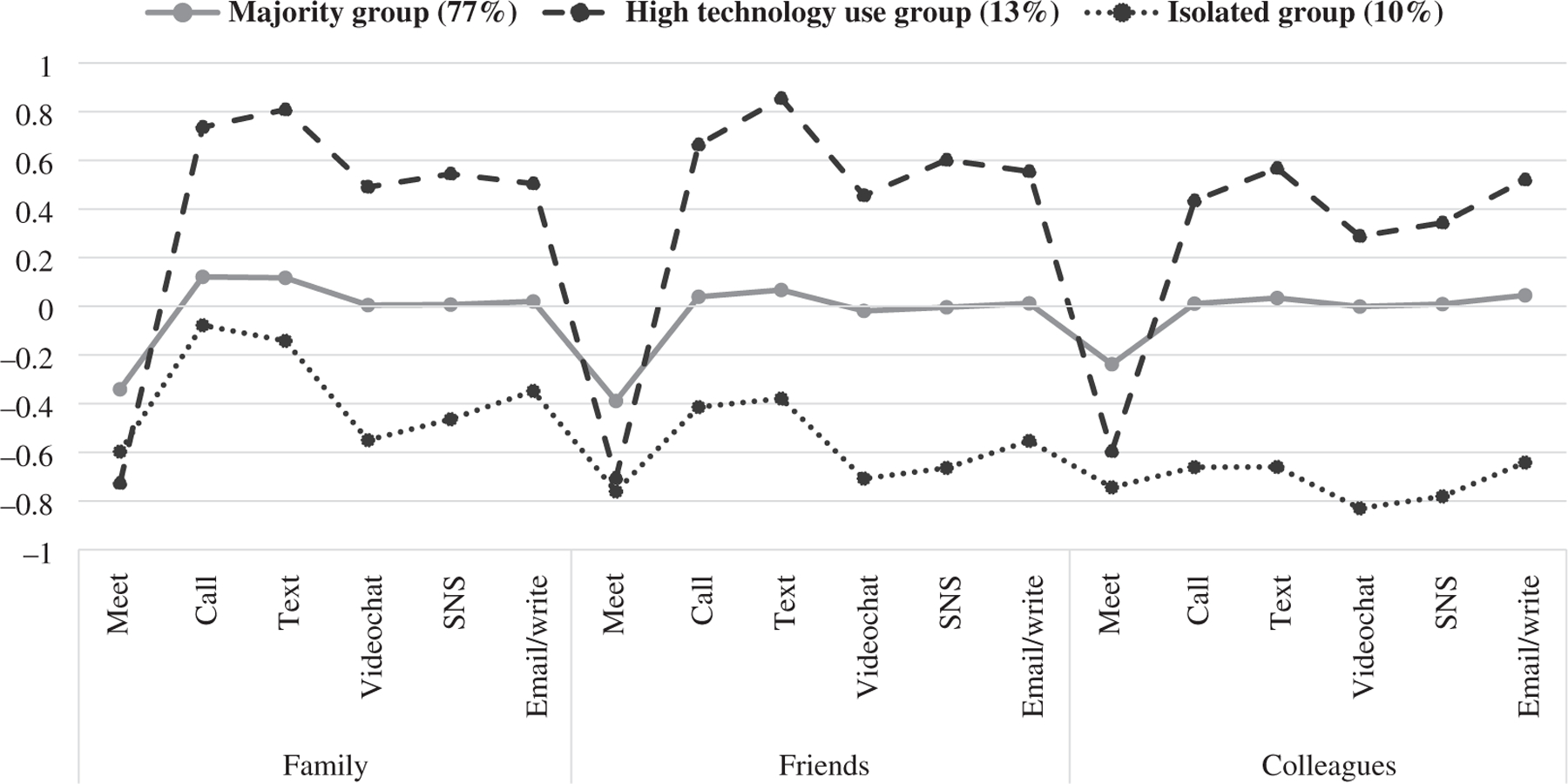
Classes of changes in social contact across relationship types and mode of communication. Scores are unstandardized. Responses on the y-axis reflect the three responses of changes in social contact: –1 (contacting less than before), 0 (same as before), 1 (contacting more than before)
3.3 |. Demographic and general contact characteristics of social contact change profiles
Second, we examined the association between participant characteristics and the social contact change profiles to understand who was more likely to have which social contact change profile. The results from the multinomial logistic regression are in Table 3. The largest majority group was used as the reference group to compare to the other two groups. Compared to the majority group, the high technology use group was more likely to be older, female, and less likely to be Black compared to the majority group. They were also more likely to have used more technology-based communication methods prior to the pandemic. The isolated group was also more likely to be older, less likely to be White, twice as likely to be Latinx, reported lower income, and were less likely to live alone. There was no difference between the isolated group and the majority group in terms of general social contact frequency.
TABLE 3.
Demographic, health, and living arrangement predictors of social contact change groups
| High technology use groupa | Isolated groupa | |
|---|---|---|
| Age in years | 1.01* [.00, .03] | 1.02* [.00, .03] |
| Female | 1.56* [.13, .76] | .85 [−.49, .16] |
| Black (ref = White) | .65* [−.93, .07] | .90 [−.63, .41] |
| Other (ref = White) | 1.03 [−.36, .42] | 2.39* [.42, 1.32] |
| Latinx | .95 [−.50, .40] | 2.00* [.20, 1.18] |
| Education | 1.10 [−.01, .21] | .93 [−.20, .05] |
| Income | 1.10 [−.01, .20] | .86* [−.27, −.02] |
| Employment | 1.05 [−.32, .41] | 1.08 [−.34, .50] |
| Disease burden | .97 [−.12, .06] | 1.09 [−.01, .18] |
| Living alone | 1.39 [−.07, .72] | .66* [−.83, .01] |
| Live with children | 1.27 [−.12, .59] | .91 [−.49, .31] |
| Live with older adults | 1.09 [−.33, .50] | .72 [−.78, .12] |
| Quarantine status | 1.40 [.02, .66] | 1.20 [−.17, .52] |
| General social contact | ||
| Meet in-person: family | 95 [−.13, .03] | 1.01 [−.07, .10] |
| Meet in-person: friends | .94 [−.15, .04] | .99 [−.11, .08] |
| Meet in-person: colleagues | 1.00 [−.09, .08] | .98 [−.10, .06] |
| Technology-based contact: family | 1.07*** [.04, .10] | 1.00 [−.03, .03] |
| Technology-based contact: friends | 1.09*** [.05, .12] | 1.00 [−.03, .04] |
| Technology-based contact: colleagues | 1.03* [.01, .05] | 1.02 [.00, .05] |
Note: Values represent standardized odds ratios [95% confidence interval].
Reference group is Majority group.
p< .05;
p < .01;
p < .001
3.4 |. Associations between social contact change profiles and mental health
Finally, we investigated the association between the social contact change profiles and concurrent mental health and changes in emotional closeness to social ties (Table 4). The general level of loneliness and depression were added as control for those models. Compared to the majority group, the high technology use group had higher levels of depression and higher levels of anxiety. At the same time, they reported an increase in emotional closeness to family and friends. Compared to the majority group, the isolated group had higher loneliness and reported a decrease in emotional closeness to friends.
TABLE 4.
Regression results predicting mental health and changes in emotional closeness to family and friends from social contact change groups
| Loneliness | Depression | Anxiety | Family closeness changec | Friend closeness changec | |
|---|---|---|---|---|---|
| Intercept | .80*** [.68, .93] | 1.04*** [.66, 1.42] | 9.83*** [8.50, 11.15] | −.04 [−.17, .09] | −.17* [−.30, −.03] |
| Dependent variable at W1a | .08*** [.56, .63] | .51*** [.46, .56] | - | - | - |
| High technology use groupb | .00 [.06, .04] | .35*** [.17, .54] | 1.51*** [.78, 2.25] | .37*** [.30, .45] | .28*** [.20, .37] |
| Isolated groupb | −.01** [.02, .14] | .18 [−.04, .40] | .79 [−.06, 1.64] | .08 [−.17, .01] | −.09* [−.18, .00] |
| Covariates | |||||
| Age in years | .00** [.00, .00] | −.01*** [−.02, −.01] | −.11*** [−.13, −.10] | .00*** [.00, .01] | .00** [.00, .01] |
| Female | −.03 [−.07, .00] | .03 [−.10, .15] | .63* [.15, 1.11] | .05* [.00, .09] | .01 [−.04, .06] |
| Black (ref = White) | −.05 [−.11, .01] | −.03 [−.26, .20] | −.87* [−1.69, −.04] | .03 [−.06, .12] | .03 [−.05, .12] |
| Other (ref = White) | .05 [.00, .10] | −.05 [−.24, .13] | −.54 [−1.19, .12] | .01 [−.06, .08] | .03 [−.04, .10] |
| Latinx | .00 [−.06, .06] | −.05 [−.27, .18] | −.18 [−.99, .62] | .01 [−.08, .10] | .00 [−.08, .09] |
| Education | .00 [−.02, .01] | −.04 [−.08, .01] | −.12 [−.29, .06] | .00 [−.02, .02] | .01 [−.01, .02] |
| Income | −.01 [−.02, .01] | −.02 [−.07, .02] | −.24c [−.40, −.07] | −.01 [−.02, .01] | .00 [−.02, .01] |
| Employment | .02 [−.02, .05] | .14* [.01, .27] | .56* [.04, 1.08] | −.01 [−.07, .04] | .02 [−.03, .07] |
| Disease burden | .02** [.01, .03] | .07** [.03, .12] | .71*** [.55, .87] | .00 [−.02, .01] | .02* [.00, .04] |
| Living alone | .05 [.00, .09] | .19* [.03, .34] | .16 [−.44, .75] | −.09c [−.15, −.03] | −.01 [−.06, .05] |
| Children in household | .03 [−.02, .07] | .04 [−.12, .20] | .39 [−.21, .99] | −.01 [−.07, .05] | .02 [−.04, .07] |
| Older adult in household | −.03 [−.08, .02] | .19* [.02, .35] | .50 [−.10, 1.10] | −.02 [−.08, .04] | .01 [−.05, .07] |
| Quarantine status | .02 [−.02, .06] | .33*** [.18, .48] | 1.33*** [.78, 1.88] | .00 [−.06, .06] | −.05 [−.11, .01] |
Note: Coefficients are unstandardized coefficients [95% confidence intervals].
Depression and loneliness models included wave 1 measures as control.
Reference group is majority group.
Family/Friend closeness change was coded less close than before (–1), same (0), closer than before (1).
p < .05;
p < .01;
p < .001.
4 |. DISCUSSION
Based on timely data collected from adults in the United States, the current study investigated profiles of social contact change across social ties (family, friends, and colleagues) and modes of contact (in person and technology-based communication tools) in response to the COVID-19 outbreak. Participants reported on the direction of social contact change in a relative manner (less/same/more than before) with social ties and modes of contact during the transitional phase of the pandemic. Overall, participants decreased in-person contact and slightly increased technology-based communication methods. We identified three latent profiles with different behaviors of social contact change. Compared to the majority group that primarily used slightly more phone and text, the large proportion of persons in the high technology use group limited in-person contact and increased use of all forms of technology-based communication methods. In contrast, participants who were in the isolated group decreased in both in-person and technology-based contact with social ties. These groups had some differences in demographic characteristics and general social contact levels, as well as their mental health and perceived changes in emotional closeness to family and friends at the early stages of the pandemic.
There has been a shift in social contact behaviors since mid-March 2020, as national campaigns promoted social distancing to reduce the spread of the coronavirus. In the current sample, about half of the participants reported limiting in-person contact with family and friends and, to a lesser degree, decreased in-person contact with colleagues. It is possible that decreasing in-person contact with colleagues was not easy to implement for some people if they were health care workers or those deemed essential continued to work on site (Terrell, 2020).
Interestingly, there was variation in the changes of technology-based communication method use as in-person contact was reduced. As captured in the latent profile analysis, most participants reduced in-person contact with social ties, but their frequency of technology-based methods was largely the same as before with a slight increase in phone calls and text messages. Preference for phone calls during the pandemic have been documented in other studies (longterm care residents; Monin et al., 2020). Indeed, phone service providers described a large increase in phone call volume as well as longer call times at the beginning of the pandemic (Kang, 2020). Compared with other communication methods, phone calls may be preferred because they are widely available, inexpensive, and provide rich information through real-time voice exchange (van den Berg et al., 2012). The finding is consistent with the literature showing that phone calls are preferred in communication with relationally close social ties or in urgent situations (Tillema et al., 2010), which can describe exchanges with family members and friends at the early stages of the pandemic. In addition, we found a pattern where email use only increased with colleagues, but not with family and friends, across all latent groups, which corresponds to the preference for asynchronous methods among formal relationships (Tillema et al., 2010). While media richness theory suggested that the modality with the richest information may be preferred to substitute for the lack of in-person contact, the use of video chat did not increase much for most people. A recent study also reported the preference for phone calls over video chat during the pandemic, which does not align with the assumption of the media richness theory (Hall et al., 2021). The video chat is an emerging communication tool with a rich media, but there are reports of dislike among users, possibly due to exhaustion from requiring higher levels of attention and frequent technological malfunctions (e.g., Zoom fatigue; Wiederhold, 2020). Also, the usage of videoconference tools for personal contact would be likely shaped by accessibility and familiarity to the technology (Baig, 2020). Many older adults who are already online, for example, reported that they still need assistance in setting up and using new electronic devices (Anderson & Perrin, 2017). Similarly, a recent study showed that older adults preferred more traditional methods compared to online-based communication tools (Burholt et al., 2020). They found that phone calls, texts, and emails were used as substitutes for in-person contact and were protective of loneliness when there were low levels of in-person contact, whereas video calls were not used frequently and did not ameliorate feelings of loneliness (Burholt et al., 2020).
We identified two groups with different social contact change behavior from the majority group. First, the high technology use group maximized the use of all technology-based communication methods in combination with strictly limiting in-person contact (see also Figure 2). Note that the high technology use group frequently used technology-based tools prior to the pandemic, compared to the majority group. This pattern suggests that those who were already familiar and frequent users of internet-based communication used them to compensate for decreased in-person contact (Tillema et al., 2010). Demographically, the group was also more likely to be female and older. Similar to work showing that middle-aged females were most likely to perform the kin-keeper role in the family and provide assistance and information to larger family networks (Leach & Braithwaite, 1996), individuals in the high technology use group might have increased their relationship maintenance efforts via increasing the use of multiple modes of contact in the context of social distancing. Indeed, such increased contact may be one source of perceiving higher social support from family and friends (Luchetti et al., 2020; Tull et al., 2020). However, efforts of compensation may not be working favorably for mental health, as reflected in higher anxiety and more depressive symptoms of the high technology use group. Our study suggests that increasing the use of technology, combined with restricted in-person meeting, does not satisfactorily fulfill one’s social needs to connect and may thus result in poorer mental health. Relying on technology tools to engage with loved ones that were originally face-to-face can be mentally exhausting and effortful even if the tool is meant to deliver higher levels of social presence (Hall et al., 2021; Wiederhold, 2020). In addition, it is possible that poor mental health symptoms, such as depression or anxiety, are more closely linked to other pandemic-related stressors like health and economic concerns (Zheng et al., 2021). As anxiety was modeled cross-sectionally, those who reported to be anxious may have increased their technology use across methods. While implications for interventions should be considered with caution, the delivery of telemedicine to address anxiety and depressive symptoms seem fitting for the high technology use group as they are active users of online communication technologies (Rajkumar, 2020).
In contrast, the isolated group changed their behavior in a way that reduced not only in-person contact but also technology-based contact. They were more likely to be older, Latinx, non-White, have lower income, less likely to live alone, and experienced more loneliness than the majority group. It is worth noting that participants in this group lived with others in the household who may provide daily social interaction. As such, the need to increase technology-based communication with others could be low. The decreased communication with social ties, however, might also exacerbate isolation with larger social networks, especially if the pandemic is prolonged (Kissler et al., 2020). Indeed, participants in this group had higher loneliness and felt less emotionally close to friends, which suggests their effective connection with social networks outside the household may be weak. If the need for connecting with friends is present (i.e., desired social contact) but concerns regarding accessibility persist (i.e., actual social contact), satisfactory connection with friends or community would be difficult to maintain, which may exacerbate feelings of loneliness. In terms of identifying populations to deliver targeted mental health services, our finding indicates that people at higher risk of loneliness could have social contact behaviors that resemble the isolated group. However, the delivery of social isolation prevention treatment via online channels (e.g., Chen & Schulz, 2016) to this group could be challenging due to their low levels of usage of technology-based tools and barriers stemming from their limited resources (Seifert et al., 2021; Xie et al., 2020).
4.1 |. Strengths and limitations
The strengths of the current study include the longitudinal study design and timeline of the assessment. We surveyed participants in January and March 2020, which provided a snapshot of participants both just before and in the early phase of the pandemic. In addition to this longitudinal design, the stratified sampling based on sex, age, and race (African Americans) provided a more diverse sample from across the United States than convenience sampling. The detailed social contact measure across various communication behaviors was also a strength.
This study has limitations to consider. First, the survey was conducted via a web-based survey panel. It is possible that those with limited internet access and low digital literacy were not included in the study sample. Communication needs and mental health outcomes may be different and more concerning for populations who were not online. Second, there was nonrandom attrition between the two waves. Participants with less income or of a racial minority were more likely to drop out of the second wave of data collection. Income and race are factors linked to different uses and attitudes toward online-based communication during the pandemic (Schumacher & Kent, 2020). The attrition could affect the generalizability of the results. Third, while the survey assessed frequency and methods of contact with social ties, the qualitative aspects of the social interactions were not captured in this survey. Future studies with data regarding instrumental support or exchange of information among the social ties using technology-based communication methods would provide a fuller picture of the communication behavior and how well these tools compensate in-person contacts. Lastly, the study is limited to the United States and to the early phase of the pandemic. The social contact changes people make are influenced by the COVID-19 response and regulations made at regional and national levels. For example, the short duration of strict lockdown policy would impose all residents to quarantine at home, but the cultural and technological factors would have made a difference in the use of technology-based communication tools and their link to mental health outcomes. In addition, the survey was conducted in March 2020 in the United States where working-from-home policies were just beginning to take its shape and public use of video conference software for casual socialization was not yet common. Future studies can examine trends in social contact behavior over the months during the pandemic to capture the adaptive behaviors emerging from the long-term pandemic. Also, it would be worthwhile to examine the variations in communication patterns across local social distancing policies in place during the pandemic, and across countries (Zhu et al., 2021).
5 |. CONCLUSION
Under the social distancing guidelines in the early phase of the COVID-19 pandemic, Americans changed their behavior with social ties and across different modes of communication. While most reduced in-person contact, there were variations in which technology-based communication methods were utilized. Synchronous methods increased in use with family and friends. A small group increased use of all online modes of contact, and these were partially explained by higher usage in general, suggesting the preference for technologies that are familiar. Another small group decreased all social contacts and experienced higher loneliness and emotional disconnect with friends. While we observed compensatory behavior to overcome the lack of in-person contact, the higher levels of anxiety, depression, and loneliness in some groups suggest that technology-based modes of contact do not fully replace meeting people in person. To our knowledge, the current study is among the first to document social contact behavior longitudinally over the early phase of the pandemic. The finding also provides evidence that there are different communication patterns among high-risk groups for loneliness and mood/anxiety disorders. Future studies should examine the long-term effects of the pandemic on communication patterns among various settings and subgroups. Furthermore, in implementing a technology-assisted intervention to prevent loneliness and mental health problems, providers should consider diverse social contact behaviors of the clients and potential barriers to the delivery of treatments via telemedicine.
ACKNOWLEDGMENTS
This research was supported by the National Institute on Aging of the National Institutes of Health (R01AG053297 and R01AG068093). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Funding information
National Institute on Aging of the National Institutes of Health, Grant/ Award Numbers: R01AG068093, R01AG053297
Footnotes
CONFLICT OF INTEREST
The authors declare no conflicts of interest.
DATA AVAILABILITY STATEMENT
Research data are not shared.
Participants were categorized as working if they reported being employed with salaried, hourly-pay, self-employed, working while studying, and having other working arrangement. Those who responded as retired, temporarily out of work, unable to work, in school, or not working by choice were categorized as not working.
REFERENCES
- Ahmed F, Zviedrite N, & Uzicanin A (2018). Effectiveness of workplace social distancing measures in reducing influenza transmission: A systematic review. BMC Public Health, 18, 518. 10.1186/s12889-018-5446-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychological Association. (2020, March 18). COVID-19 isn’t just a danger to older people’s physical health https://www.apa.org/news/apa/2020/03/covid-19-danger-physical-health [Google Scholar]
- Anderson M, & Perrin A (2017, May 17). Tech adoption climbs among older adults Pew Research Center. https://www.pewresearch.org/internet/2017/05/17/tech-adoption-climbs-amongolder-adults [Google Scholar]
- Anderson M, Perrin A, Jiang J, & Kumar M (2019, April 22). 10% of Americans don’t use the Internet. Who are they? Pew Research Center. https://www.pewresearch.org/fact-tank/2019/04/22/some-americans-dont-use-the-internet-who-are-they/ [Google Scholar]
- Anderson M, & Vogel EA (2020, March 31). Americans turn to technology during COVID-19 outbreak, say an outage would be a problem Pew Research Center. https://www.pewresearch.org/fact-tank/2020/03/31/americans-turn-to-technology-during-covid-19-outbreak-say-an-outage-would-be-a-problem/ [Google Scholar]
- Auxier B (2020, December 18). What we’ve learned about Americans’ views of technology during the time of COVID-19 Pew Research Center. https://www.pewresearch.org/fact-tank/2020/12/18/what-weve-learned-about-americans-views-of-technology-during-the-time-of-covid-19 [Google Scholar]
- Baig E (2020, November 18). How to use zoom to stay connected during the coronavirus AARP. https://www.aarp.org/home-family/personal-technology/info-2020/how-to-use-zoom.html [Google Scholar]
- Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, & Rubin GJ (2020). The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. The Lancet, 395(10227), 912–920. 10.1016/S0140-6736(20)30460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burholt V, Windle G, Gott M, & Morgan DJ (2020). Technology-mediated communication in familial relationships: Moderated-mediation models of isolation and loneliness. The Gerontologist, 60(7), 1202–1212. 10.1093/geront/gnaa040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (2020, November 17). Social distancing keep a safe distance to slow the spread https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/social-distancing.html [Google Scholar]
- Chen YR, & Schulz PJ (2016). The effect of information communication technology interventions on reducing social isolation in the elderly: A systematic review. Journal of Medical Internet Research, 18(1), e18. 10.2196/jmir.4596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daft RL, & Lengel RH (1984). Information richness: A new approach to managerial behavior and organizational design. In Cummings LL & Staw BM (Eds.), Research in organizational behavior (pp. 191–233). JAI Press. [Google Scholar]
- Enders CK (2011). Analyzing longitudinal data with missing values. Rehabilitation Psychology, 56(4), 267–288. 10.1037/a0025579 [DOI] [PubMed] [Google Scholar]
- Hall JA, & Merolla AJ (2020). Connecting everyday talk and time alone to global well-being. Human Communication Research, 46(1), 86–111. 10.1093/hcr/hqz014 [DOI] [Google Scholar]
- Hall J, Pennington N, & Holmstrom A (2021). Connecting through technology during COVID-19. Human Communication & Technology, 2(1), 1–18. 10.17161/hct.v3i1.15026 [DOI] [Google Scholar]
- Hawkley LC, Browne MW, & Cacioppo JT (2005). How can I connect with thee? Let me count the ways. Psychological Science, 16(10), 798–804. 10.1111/j.1467-9280.2005.01617.x [DOI] [PubMed] [Google Scholar]
- IBM Corp . (2017). IBM SPSS statistics for Windows, Version 25.0 IBM Corp.Released [Google Scholar]
- Jedidi K, Ramaswamy V, & Desarbo WS (1993). A maximum likelihood method for latent class regression involving a censored dependent variable. Psychometrika, 58(3), 375–394. 10.1007/BF02294647 [DOI] [Google Scholar]
- Kang C (2020, April 9). The humble phone call has made a comeback https://www.nytimes.com/2020/04/09/technology/phone-calls-voice-virus.html [Google Scholar]
- Kissler SM, Tedijanto C, Goldstein E, Grad YH, & Lipsitch M (2020). Projecting the transmission dynamics of SARS-CoV-2 through the postpandemic period. Science, 368(6493), 860–868. 10.1126/science.abb5793 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leach MS, & Braithwaite DO (1996). A binding tie: Supportive communication of family kinkeepers. Journal of Applied Communication Research, 24(3), 200–216. 10.1080/00909889609365451 [DOI] [Google Scholar]
- Lo Y, Mendell NR, & Rubin DB (2001). Testing the number of components in a normal mixture. Biometrika, 88(3), 767–778. 10.1093/biomet/88.3.767 [DOI] [Google Scholar]
- Löwe B, Decker O, Müller S, Brähler E, Schellberg D, Herzog W, & Herzberg PY (2008). Validation and standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the general population. Medical Care, 46(3), 266–274. 10.1097/MLR.0b013e318160d093 [DOI] [PubMed] [Google Scholar]
- Löwe B, Kroenke K, & Gräfe K (2005). Detecting and monitoring depression with a two-item questionnaire (PHQ-2). Journal of Psychosomatic Research, 58(2), 163–171. 10.1016/j.jpsychores.2004.09.006 [DOI] [PubMed] [Google Scholar]
- Luchetti M, Lee JH, Aschwanden D, Sesker A, Strickhouser JE, Terracciano A, & Sutin AR (2020). The trajectory of loneliness in response to COVID-19. American Psychologist, 75(7), 897–908. 10.1037/amp0000690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luhmann M, & Hawkley LC (2016). Age differences in loneliness from late adolescence to oldest old age. Developmental Psychology, 52(6), 943–959. 10.1037/dev0000117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller G (2020). Social distancing prevents infections, but it can have unintended consequences. Science https://www.sciencemag.org/news/2020/03/we-are-social-species-how-will-social-distancing-affect-us [Google Scholar]
- Monin JK, Ali T, Syed S, Piechota A, Lepore M, Mourgues C, Gaugler JE, Marottoli R, & David D (2020). Family communication in long-term care during a pandemic: Lessons for enhancing emotional experiences. The American Journal of Geriatric Psychiatry, 28(12), 1299–1307. 10.1016/j.jagp.2020.09.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, & Muthén BO (1998–2017). Mplus user’s guide (8th ed.). Muthén & Muthén. [Google Scholar]
- Nylund KL, Asparouhov T, & Muthén BO (2007). Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Structural Equation Modeling: A Multi-disciplinary Journal, 14(4), 535–569. 10.1080/10705510701575396 [DOI] [Google Scholar]
- Rajkumar RP (2020). COVID-19 and mental health: A review of the existing literature. Asian Journal of Psychiatry, 52, 102066. 10.1016/j.ajp.2020.102066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ram N, & Grimm KJ (2009). Growth mixture modeling: A method for identifying differences in longitudinal change among unobserved groups. International Journal of Behavioral Development, 33(6), 565–576. 10.1177/0165025409343765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell DW (1996). UCLA Loneliness Scale (Version 3): Reliability, validity, and factor structure. Journal of Personality Assessment, 66(1), 20–40. 10.1207/s15327752jpa6601_2 [DOI] [PubMed] [Google Scholar]
- Schumacher S, & Kent N (2020, April 2). 8 charts on internet use around the world as countries grapple with COVID-19 Pew Research Center. https://www.pewresearch.org/fact-tank/2020/04/02/8-charts-on-internet-use-around-the-world-as-countries-grapple-with-covid-19 [Google Scholar]
- Seifert A, Cotten SR, & Xie B (2021). A double burden of exclusion? Digital and social exclusion of older adults in times of COVID-19. The Journals of Gerontology: Series B, 76(3), e99–e103. 10.1093/geronb/gbaa098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shor E, & Roelfs DJ (2015). Social contact frequency and all-cause mortality: A meta-analysis and meta-regression. Social Science & Medicine, 128, 76–86. 10.1016/j.socscimed.2015.01.010 [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, Williams JBW, & Löwe B (2006). A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine, 166(10), 1092–1097. 10.1001/archinte.166.10.1092 [DOI] [PubMed] [Google Scholar]
- Teo AR, Choi H, Andrea SB, Valenstein M, Newsom JT, Dobscha SK, & Zivin K (2015). Does mode of contact with different types of social relationships predict depression in older adults? Evidence from a nationally representative survey. Journal of the American Geriatrics Society, 63(10), 2014–2022. 10.1111/jgs.13667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terrell K (2020, December 23). Coronavirus vaccines: Who is considered an essential worker? AARP. www.aarp.org/work/working-at-50-plus/info-2020/covid-vaccine-essential-workers.html [Google Scholar]
- Tillema T, Dijst M, & Schwanen T (2010). Face-to-face and electronic communications in maintaining social networks: The influence of geographical and relational distance and of information content. New Media & Society, 12(6), 965–983. 10.1177/1461444809353011 [DOI] [Google Scholar]
- Tull MT, Edmonds KA, Scamaldo KM, Richmond JR, Rose JP, & Gratz KL (2020). Psychological outcomes associated with stay-at-home orders and the perceived impact of COVID-19 on daily life. Psychiatry Research, 289, 113098. 10.1016/j.psychres.2020.113098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Usher K, Bhullar N, & Jackson D (2020). Life in the pandemic: Social isolation and mental health. Journal of Clinical Nursing, 29(15–16), 2756–2757. 10.1111/jocn.15290 [DOI] [PubMed] [Google Scholar]
- van den Berg PE, Arentze TA, & Timmermans HJP (2012). New ICTs and social interaction: Modelling communication frequency and communication mode choice. New Media & Society, 14(6), 987–1003. 10.1177/1461444812437518 [DOI] [Google Scholar]
- Westmyer SA, DiCioccio RL, & Rubin RB (1998). Appropriateness and effectiveness of communication channels in competent interpersonal communication. Journal of Communication, 48(3), 27–48. 10.1111/j.1460-2466.1998.tb02758.x [DOI] [Google Scholar]
- House White. (2020, March 16). The President’s coronavirus guidelines for America: 15 Days to slow the spread https://www.justice.gov/doj/page/file/1258511/download [Google Scholar]
- Wiederhold BK (2020). Connecting through technology during the Coronavirus disease 2019 pandemic: Avoiding “zoom fatigue.”. Cyberpsychology, Behavior and Social Networking, 23(7), 437–439. 10.1089/cyber.2020.29188.bkw [DOI] [PubMed] [Google Scholar]
- Xie B, Charness N, Fingerman K, Kaye J, Kim MT, & Khurshid A (2020). When going digital becomes a necessity: Ensuring older Adults’ needs for information, services, and social inclusion during COVID-19. Journal of Aging & Social Policy, 32(4–5), 460–470. 10.1080/08959420.2020.1771237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng J, Morstead T, Sin N, Klaiber P, Umberson D, Kamble S, & DeLongis A (2021). Psychological distress in North America during COVID-19: The role of pandemic-related stressors. Social Science & Medicine, 270, 113687. 10.1016/j.socscimed.2021.113687 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu N, Smetana JG, & Chang L (2021). Acceptance of society-level and individual-level preventive measures during the COVID-19 pandemic among college students in three societies. Journal of Cross-Cultural Psychology, 52(7), 606–621. 10.1177/0022022121995971 [DOI] [Google Scholar]


