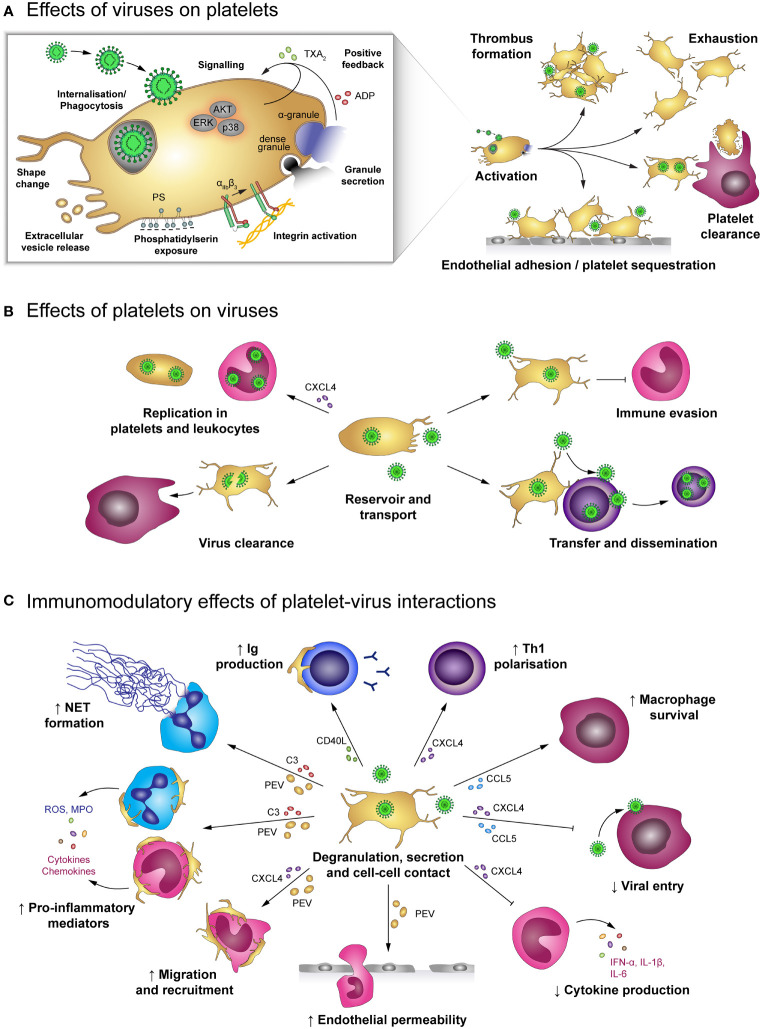
Figure 3.
Effects of platelet-virus interaction. (A) Virus binding or internalisation/phagocytosis stimulates platelet activation including degranulation, integrin activation, phosphatidylserin exposure and extracellular vesicle release. Virus-induced platelet activation enhances endothelial adhesion and thrombus formation, but may also lead to platelet exhaustion and clearance from the circulation. (B) Platelets serve as virus reservoir and transport vehicle by supporting viral replication in leukocytes or within platelets themselves and by transferring virus to other host cells, thereby augmenting viral dissemination. Furthermore, platelets shelter intracellular virions from immune-mediated degradation, though degradation of virus-containing platelets contributes to virus clearance. (C) Virus-stimulated platelets modulate immune responses by cell-cell contact and/or soluble mediators. Platelet-derived factors block viral entry into leukocytes and prolong macrophage survival. Platelets also facilitate leukocyte extravasation by augmenting endothelial permeability, leukocyte migration and recruitment. Furthermore, platelets regulate leukocyte effector functions such as IgG production, T cell polarization, NET formation and release of inflammatory mediators, thereby either enhancing or diminishing immune defences. ADP, adenosine diphosphate; AKT, Protein kinase B; C3, complement factor 3; CCL5, chemokine (C-C motif) ligand 5; CD40L, CD40 ligand; CXCL4, chemokine (C-X-C motif) ligand 4; ERK, Extracellular signal-regulated kinase; IFN-α: Interferon α; IgG, immunoglobulin; IL-1β: Interleukin 1β; MPO, myeloperoxidase; NET, neutrophil extracellular trap; p38, p38 mitogen-activated protein kinase; PEV, Platelet-derived extracellular vesicle; PS, phosphatidylserine; ROS, reactive oxygen species; Th1, T helper cell type 1; TXA2, thromboxane A2.