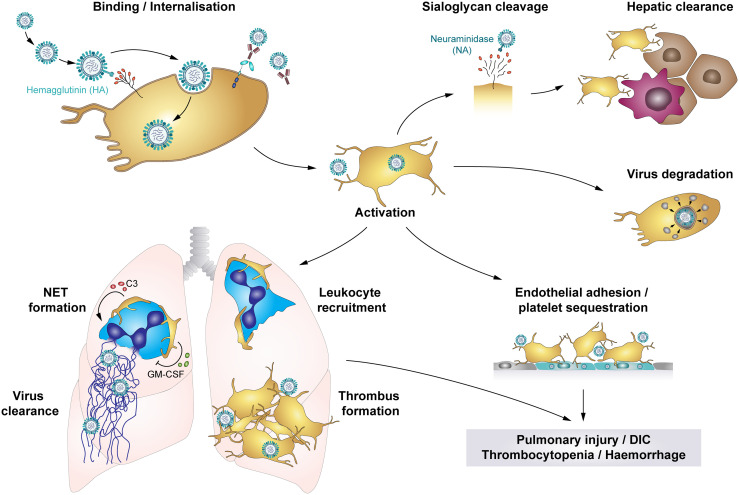
Figure 5.
The role of platelets in influenza infections: Platelets bind and internalise influenza virus via the interaction of virus hemagglutinin (HA) proteins and sialic acid (SA)-terminated glycans on the platelet surface, though platelets also bind influenza-containing immune complexes. These interactions result in platelet activation and platelet-mediated immune responses that contribute to influenza-associated pathologies. Cleavage of SA residues by viral neuraminidase (NA) induces platelet clearance by liver hepatocytes and Kupffer cells. However, rapid internalisation of viral particles leads to digestion of influenza virus when vesicles with enclosed virions fuse with platelet granules that contain antimicrobial peptides. Systemically, influenza-infected endothelial cells express pro-thrombotic factors like fibronectin or integrin α5β1, which increases platelet adhesion to the endothelium and thus fosters platelet sequestration. Locally, platelets infiltrate the lung tissue, where thrombus formation may constrict and/or occlude blood vessels or small airways. Furthermore, platelet-leukocyte aggregate formation induces leukocyte recruitment and triggers the formation of NETs to entrap viral particles, regulated by C3 and GM-CSF. However, NETs cause further tissue damage and enhance thrombus formation. Together, these platelet-mediated responses in influenza trigger pulmonary injuries, disseminated intravascular coagulation (DIC), thrombocytopenia and haemorrhages in severe influenza infections. C3, Complement factor C3; DIC, disseminated intravascular coagulation; GM-CSF, Granulocyte-monocyte colony-stimulating factor; HA, hemagglutinin; NA, neuraminidase; NET, neutrophil extracellular traps.