Abstract
Objectives
To evaluate the effect of intraperitoneal normal saline instillation (INSI) of 15 mL/kg body weight on postoperative pain after a gynaecological laparoscopic procedure.
Design
Randomised controlled trial.
Setting
University Hospital in Kuala Lumpur, Malaysia.
Participants
Patients aged 18–55 years, with American Society of Anaesthesiologists (ASA) classification I–II, scheduled for an elective gynaecological laparoscopic procedure for a benign cause.
Intervention
The patients were randomly allocated to two groups. In the intervention group, 15 mL/kg body weight of normal saline was instilled intraperitoneally, while the control group received the conventional combination of open laparoscopic trocar valves with gentle abdominal pressure to remove the retained carbon dioxide.
Main outcome measures
The outcomes measured were the mean pain scores for shoulder and upper abdominal pain at 24 h, 48 h, and 72 h postoperatively.
Results
A total of 68 women completed the study, including 34 women in each group. There was no difference in the shoulder pain score at 24 h, 48 h, and 72 h postoperatively. However, a significant improvement in the upper abdominal pain score after 48 h (95% confidence interval [CI] 0.34–1.52, p = 0.019) and 72 h (95% CI 0.19–0.26, p = 0.007) postoperatively were observed.
Conclusions
INSI of 15 mL/kg body weight does not lower postoperative shoulder pain compared to no fluid instillation. A modest pain score improvement was observed in the upper abdominal area at 48 h and 72 h after surgery. An INSI of up to 30 mL/kg body weight may be required to eliminate shoulder pain. Care must be taken before administering a higher amount of INSI, considering the potential risk of peritoneal adhesions.
Clinical registration ISRCTN Identifier: 87898051 (Date: 26 June 2019) https://doi.org/10.1186/ISRCTN87898051
Keywords: Laparoscopic surgery, Gynaecological surgery, Postoperative pain
Background
Postoperative pain should be addressed effectively as it can complicate a patient’s recovery process. Inadequate postoperative pain control is associated with impaired quality of life, delayed recovery, and prolonged use of opioids, with a concurrent increase in healthcare costs [1]. Despite the emergence of many intraoperative techniques and manoeuvres to reduce postoperative pain, pain after gynaecological laparoscopic procedures remains high [2–4]. To date, at least 11 strategies have been demonstrated to be effective in controlling post-laparoscopy pain [5, 6]. One of these strategies involves instilling fluid into the peritoneal cavity [5–8].
Intraperitoneal normal saline instillation (INSI) is a pain reduction method that functions by washing out residual carbon dioxide [7–9]. Moreover, it can act as a physiological buffer whereby residual carbon dioxide is dissolved in the fluid [9–11]. The removal of the retained carbon dioxide is crucial because it can be converted to carbonic acid via the peritoneal carbonic anhydrase enzyme [12]; this process reduces the pH level, causing irritation or damage to the diaphragmatic peritoneal nerves, leading to pain [9–12].
In gynaecological surgery, this pain reduction technique has been implemented in several different studies. It was found that INSI significantly reduced shoulder and upper abdominal pain compared to no fluid instillation [7–11, 13]. Although these studies were performed by the same researchers, the amount of fluid instilled varied between 15–30 mL/kg body weight [10, 11]. Under these circumstances, a 60 kg weighted woman could either be receiving 900 mL (15 mL/kg) or up to 1800 mL (30 mg/kg) of INSI, which is twice the amount.
A laparoscopic surgeon should take extra precautions when considering INSI. The peritoneum is composed of a single layer of mesothelial cells and is responsible for facilitating the gliding of the bowel via its microvilli, glycosaminoglycans, and surfactants [14]. Peritoneal mesothelial cells react to trauma and chemical irritants quickly [15, 16]. Normal saline, for example, detaches mesothelial cells, leading to a loss of fibrinolytic activity [17]. This negative effect from saline has been confirmed in vitro [18–20] and in vivo [21] Additionally, studies have demonstrated that normal saline dwelling in the peritoneal cavity during peritoneal dialysis or laparotomy wash-out can lead to the formation of peritoneal adhesions [20, 21]; these adhesions can cause chronic and life-threatening symptoms such as abdominal distension, pain, nausea, and abnormal bowel movements [22]. In animal models, intraperitoneal normal saline increases lymphatic flow [23]. In this study, we attempted to produce the pain relief effect of INSI by fixing the lowest amount of normal saline to be instilled into the peritoneal cavity at 15 mL/kg body weight, which was the lowest previously tested dose [10, 11, 13].
Methods
Setting and participants
This study was carried out in the general operating theatre of the University Malaya Medical Centre, Kuala Lumpur, Malaysia. Written informed consent was obtained during patient visits to the gynaecology clinic a few weeks before the date of surgery or during ward admission a day before the surgery. Patients assigned to the American Society of Anaesthesiologists (ASA) physical classification [24] of I or II, aged between 18 and 60 years, and scheduled to undergo a laparoscopic procedure for benign gynaecological conditions were considered eligible for participation. The definitions of ASA are as follows: ASA I, normal healthy patient; ASA II, mild systemic disease without substantial functional limitations (body mass index < 40 kg/m2, well-controlled diabetes mellitus/mild hypertension, mild lung disease). Patients with known drug allergies to substances in parecoxib, celecoxib, paracetamol, or having received analgesia 12 h before the scheduled procedure were excluded. This study was registered and approved by the Ministry of Health Research and Ethics Committee (MREC) of the National Medical Research Register (NMRR) and the Clinical Research Centre, Malaysia (NMRR-19-1532-48232) on 06/03/2019 and the Medical Research Ethics Committee of the University Malaya Medical Centre (MREC ID No: 201926-7106) on 20/03/2019. Furthermore, the International Standardised Randomised Controlled Trial Number (ISRCTN) for this study was registered with an ID of ISRCTN87898051 (https://doi.org/10.1186/ISRCTN87898051), dated 26/06/2019. This trial was conducted in accordance with the Declaration of Helsinki (2000) for human studies.
Randomisation and blinding
Women were assigned to two groups in a 1:1 ratio using a random-permuted block randomisation algorithm via a web-based system (www.randomization.com) by a research assistant (RA-A) who was not involved in the recruitment process. The same research assistance kept the master list for the randomised treatment allocation sequences. Concealment was performed using serially numbered opaque, sealed envelopes containing a paper with the legend ‘INSI’ or ‘Control’. The following available randomisation number was assigned to the patient once she consented to participate. Upon arrival at the theatre, the allotted envelope was subsequently given to the operating theatre nurse, who was not involved in managing the patient. The envelope was opened at the end of the surgery before the removal of laparoscopic trocars. Patients who withdrew from the study before surgery were replaced by the next consenting patient. However, patients who withdrew from the study at the end of surgery were counted as dropouts, and no replacement was made.
Intervention
A standard preoperative anaesthesia form was completed in accordance with the Department of Anaesthesia’s protocol. All laparoscopic surgeries were performed in the general operation theatre at Universiti Malaya Medical Centre, Kuala Lumpur. No pre-medication or any form of analgesia was administered prior to the procedure. The standard anaesthetic agents used were propofol (1.5–2.5 mg/kg), fentanyl (1–2 mcg/kg), metoclopramide (10 mg), and atracurium (0.3–0.6 mg/kg). Anaesthesia was maintained with 50% nitric oxide, 50% oxygen, and 1–2% sevoflurane. No other analgesic was administered intraoperatively.
For each laparoscopy, while the patient was in the supine position, a sub-umbilical incision was made, and a 10-mm trocar was inserted sub-umbilically under direct vision. Pneumoperitoneum was created by insulating 2.5 L of carbon dioxide into the peritoneal cavity. Another 5-mm trocar was inserted into the right iliac fossa, left iliac fossa, or suprapubic region. At the end of the surgery, patients allocated to both groups were placed in the Trendelenburg position (30°). Subsequently, trial protocols were carried out as follows:
The intervention group (INSI): Intraperitoneal normal saline (15 mL/kg body weight) [10, 11] was infused at the upper part of the abdominal cavity evenly by the surgeon through a 5-mm trocar. The trocar sleeve valves were left open during the instillation of normal saline to allow carbon dioxide to escape from the abdominal cavity. The instilled normal saline solution was left in situ.
The control group: Trocar sleeve valves were left open to allow carbon dioxide to escape from the abdominal cavity with gentle abdominal pressure.
In both groups, the trocar incision site was closed in two layers using Vicryl 3/0 or Monosyn 3/0. Patients were then placed in a neutral position, and standard protocols of anaesthesia reversal were carried out.
Postoperative management
The patients received standard postoperative care in the ward and were discharged according to the discretion of each managing team. A standard regime of analgesia was administered to all women, in which 1 g of paracetamol and 40 mg of parecoxib were administered intravenously, or 75 mg of suppository diclofenac acid was administered at the end of the surgery. This was followed by standard regular doses of 1 g paracetamol every 6 h for 5 days. Additional doses of analgesia (oral celecoxib 200 mg twice a day), when administered, were recorded.
Measurement of pain score
The outcomes of this study were the severity of pain in the shoulder and upper abdominal areas at 24 h, 48 h, and 72 h after the laparoscopic surgery. It was measured using a 0–10 visual analogue score (VAS), where 0 = no pain and 10 = worst possible pain. The VAS has been adapted by the Ministry of Health Malaysia as a pain assessment tool [25].
Women rated their postoperative pain using the VAS at rest and during movement, at a specific location (shoulder and upper abdomen) and time (24 h, 48 h, and 72 h) postoperatively. The occurrence of nausea, vomiting, and abdominal distension was documented as secondary outcomes. The data were recorded by another research assistant (RA-B), who was blinded to the patients' assigned group. If the patients were discharged before day 3 (72 h), the patients were contacted over the phone by the research assistant RA-B, who was blinded to the assigned group of patients to obtain their pain scores.
Statistical analysis
The sample size was calculated using the G*Power software version 3.1.94. Based on a previous study [11], the mean shoulder pain (standard deviation [SD]) of VAS at 48 h post laparoscopic procedure was pain 1.26 [1.95] and 3.21 [2.78] for INSI and control groups, respectively. With a two-sided significance level of 5% and power of 85%, the minimum number needed for each group was 28. By estimating a 20% dropout rate and rounding up, we planned to recruit 68 patients (34 women in each arm).
Statistical analysis was performed using standard parametric and non-parametric statistics with JMP Pro 14.1 (SAS Institute Inc., Cary, NC, USA). Data were expressed as mean ± SD or number (%). Fisher’s exact test was used to analyse categorical variables, while the independent sample t-test or one-way ANOVA test was used to analyse continuous variables. A two-sided p-value < 0.05, was considered as the threshold for significance.
Results
Patients’ characteristics
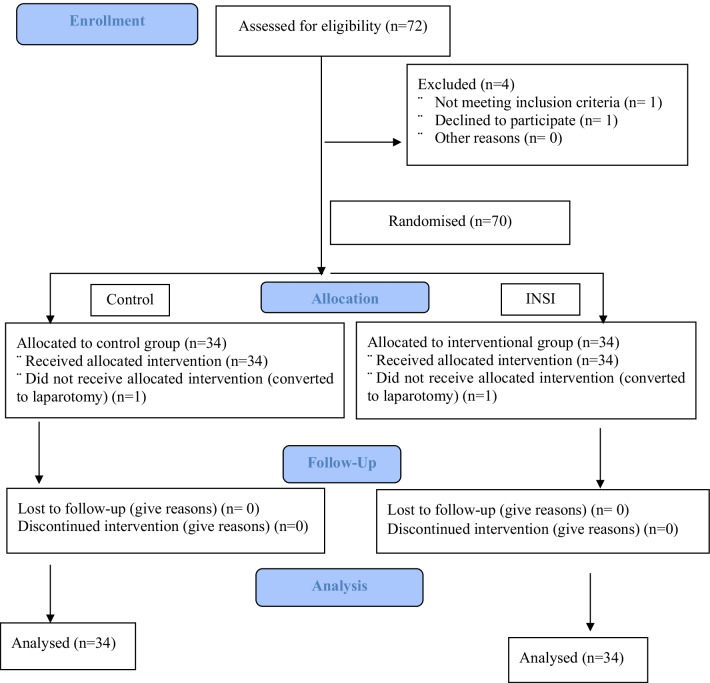
A total of 72 patients with benign gynaecological conditions scheduled for laparoscopic surgeries from April 2019 to October 2019 were recruited. One patient declined participation, and one patient was excluded based on the exclusion criteria (allergy to parecoxib, n = 1). Subsequently, 70 patients were included; however, two patients had their laparoscopy procedure converted to laparotomy (control, n = 1; INSI, n = 1). Therefore, 68 patients completed the study (Fig. 1). Baseline characteristics, including age, parity, marital status, ethnicity, body mass index, ASA classification, and indication for surgery, were comparable between the groups. The surgical outcomes, including operative time, drain insertion, estimated blood loss, number of trocars inserted, and length of postoperative hospital stay were not significantly different between the groups (Table 1).
Fig. 1.
Consort flow chart
Table 1.
Subject characteristics and surgical outcomes
| Variables | Control | Intraperitoneal normal saline (INSI) |
|---|---|---|
| n = 34 | n = 34 | |
| Age (mean ± SD) | 36.1 (± 8.9) | 35.6 (± 8.9) |
| Parity, n (%) | ||
| Nulliparous | 16 (47.1%) | 12 (35.3%) |
| Parous | 18 (52.9%) | 22 (64.7%) |
| Ethnicity n (%) | ||
| Malay | 19 (55.9%) | 22 (64.7%) |
| Chinese | 8 (23.5%) | 3 (8.8%) |
| Indian | 4 (11.8%) | 7 (20.6%) |
| Others | 3 (8.8%) | 2 (5.9%) |
| Body mass index (kg/m2) (mean ± SD) | 25.2 (± 5.4) | 27.9 (± 6.7) |
| ASA classification, n (%) | ||
| I | 22 (64.7%) | 20 (58.8%) |
| II | 12 (35.3%) | 14 (41.2%) |
| Previous abdominal surgery, n (%) | 10 (29.4%) | 10 (29.4%) |
| Indication for surgery, n (%) | ||
| Hysterectomy | 0 (0%) | 1 (2.9%) |
| Myomectomy | 2 (5.9%) | 1 (2.9%) |
| Ovarian cystectomy | 8 (23.5%) | 10 (29.4%) |
| Tubal ligation | 2 (5.9%) | 1 (2.9%) |
| Diagnostic laparoscopy | 5 (14.7%) | 2 (5.9%) |
| Salpingectomy | 8 (23.5%) | 13 (38.2%) |
| Salpingo-oophorectomy | 5 (14.7%) | 1 (2.9%) |
| TLHBSO | 4 (11.8%) | 4 (11.8%) |
| Operative time (min), (mean ± SD) | 80.2 (± 37.2) | 93.2 (± 40.5) |
| Estimated blood loss (mL), (mean ± SD) | 409 (± 453) | 365 (± 232) |
| Trocars inserted, n (%) | ||
| 2 | 4 (11.8%) | 0 (0.0%) |
| 3 | 25 (73.5%) | 29 (85.3%) |
| 4 | 5 (14.7%) | 4 (14.7%) |
| Postoperative hospital stays (days), n (%) | 1.8 (± 0.7) | 1.8 (± 0.8) |
ASA, American Society of Anaesthesiologists; INSI, intraperitoneal normal saline; SD, standard deviation; TLHBSO, total laparoscopic hysterectomy with bilateral salpingo-oophorectomy
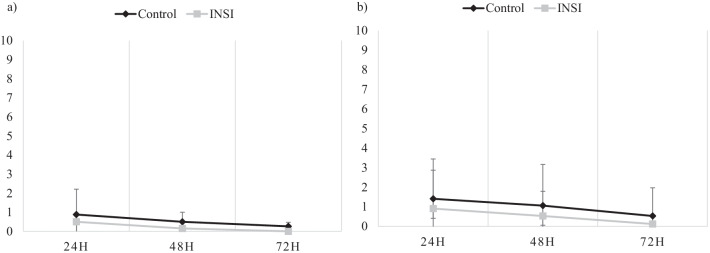
Shoulder pain
The severity of shoulder pain at 24 h, 48 h, and 72 h post-laparoscopic surgery was not significantly different between the two groups, both at rest and during movement, as shown in Table 2. However, the mean pain score recorded in the control group was persistently higher throughout the study (Fig. 2).
Table 2.
Postoperative shoulder pain
| Postoperative duration (h) | Control, n = 34 | INSI, n = 34 | p-value | ||
|---|---|---|---|---|---|
| Pain score (mean ± SD) | 95% CI | Pain score (mean ± SD) | 95% CI | ||
| At rest | |||||
| 24 | 0.88 ± 1.49 | 0.36, 1.40 | 0.50 ± 1.33 | 0.04, 0.96 | 0.269 |
| 48 | 0.50 ± 1.14 | 0.10, 0.90 | 0.15 ± 0.50 | − 0.03, 0.32 | 0.102 |
| 72 | 0.26 ± 0.90 | − 0.05, 0.58 | 0.00 ± 0.00 | 0.00, 0.00 | 0.90 |
| On movement | |||||
| 24 | 1.41 ± 2.03 | 0.70, 2.12 | 0.91 ± 1.96 | 0.23, 1.60 | 0.305 |
| 48 | 1.06 ± 2.10 | 0.33, 1.79 | 0.53 ± 1.26 | 0.09, 0.97 | 0.212 |
| 72 | 0.53 ± 1.44 | 0.03, 1.03 | 0.12 ± 0.537 | − 0.07, 0.31 | 0.123 |
Data expressed as mean ± SD (standard deviation) and 95% CI (confidence interval for mean). The test of significance was performed by one-way ANOVA test
CI, confidence interval; INSI, intraperitoneal normal saline; SD, standard deviation
Fig. 2.
Mean visual analogue scores for shoulder pain at 24 h, 48 h, and 72 h after the procedure at a rest and b on movement. Data are presented as mean (standard deviation). The test of significance was performed by one-way ANOVA test. H, hours; *p < 0.05; INSI, intraperitoneal normal saline instillation
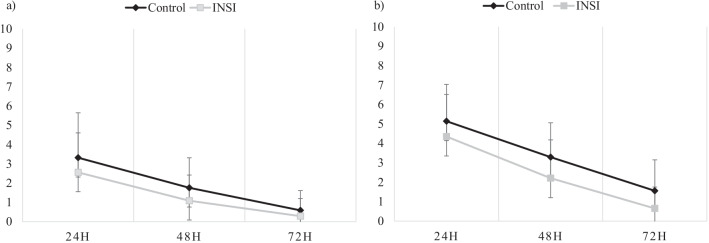
Upper abdominal pain
The severity of the upper abdominal pain after laparoscopic surgery was statistically insignificant at 24 h postoperatively. However, the pain score was significantly lower in the INSI group at 48 h (p = 0.019) and 72 h (p = 0.007) postoperatively during movement than those in the control group. The mean (± SD) pain score recorded at postoperative 48 h was 3.29 ± 1.77 (95% confidence interval [CI]: 0.30–2.68) and 2.21 ± 1.97 (95% CI: 0.34–1.52) in the control and INSI groups, respectively. After postoperative 72 h, the mean (± SD) pain score was 1.56 ± 1.5 (95% CI: 0.27–1.01) and 0.65 ± 1.1 (95% CI: 0.19–0.26) in the control and INSI groups, respectively (Table 3 and Fig. 3).
Table 3.
Postoperative abdominal pain
| Postoperative duration (h) | Control, n = 34 | INSI, n = 34 | p-value | ||
|---|---|---|---|---|---|
| Pain score (mean ± SD) | 95% CI | Pain score (mean ± SD) | 95% CI | ||
| At rest | |||||
| 24 | 3.32 ± 2.33 | 0.40, 2.51 | 2.56 ± 2.05 | 0.35, 11.84 | 0.155 |
| 48 | 1.76 ± 1.56 | 0.27, 1.22 | 1.09 ± 1.33 | 0.23, 0.62 | 0.059 |
| 72 | 0.59 ± 1.02 | 0.18, 0.23 | 0.29 ± 0.91 | − 0.02, 0.61 | 0.213 |
| On movement | |||||
| 24 | 5.14 ± 1.90 | 0.33, 4.51 | 4.35 ± 2.17 | 0.37, 3.56 | 0.101 |
| 48 | 3.29 ± 1.77 | 0.30, 2.68 | 2.21 ± 1.97 | 0.34, 1.52 | 0.019 |
| 72 | 1.56 ± 1.59 | 0.27, 1.01 | 0.65 ± 1.10 | 0.19, 0.26 | 0.007 |
Data expressed as mean ± SD (standard deviation) and 95% CI (confidence interval for mean). The test of significance was performed by one-way ANOVA test
CI, confidence interval; INSI, intraperitoneal normal saline; SD, standard deviation
Fig. 3.
Mean visual analogue scores for abdominal pain at 24 h, 48 h, and 72 h after the procedure at a rest and b on movement. Data are presented as mean (standard deviation). The test of significance was performed by one-way ANOVA test. H, hours; *p < 0.05; INSI, intraperitoneal normal saline instillation
Nausea, vomiting, and analgesia requirement
There were no statistically significant differences in the incidence of nausea, vomiting, abdominal distension, and the need for additional analgesia. Specifically, no patient required additional analgesia in either group throughout the study duration. At postoperative 24 h, 7 patients (control, n = 3; INSI, n = 4) complained of nausea, and 3 (control, n = 2; INSI, n = 1) complained of vomiting. In terms of initiation of oral feed, 31 patients from the control group and 33 patients from the INSI group began to ingest meals per orally 24 h after surgery. At postoperative 24 h, 13 patients from the control group and 8 patients from the INSI group complained of abdominal distension, of which only 3 patients experienced distension up to 48 h after surgery (control, n = 2; INSI, n = 1). Majority of the patients from both the groups were able to pass flatus at postoperative 24 h (control, n = 28; INSI, n = 32). No other complications, such as fluid leakage through the incision site or infection, were observed in the interventional or control groups. Most patients were discharged between day 1 and day 2 post-surgery (control, n = 31; INSI, n = 27). Only one patient was discharged 4 days after surgery because of personal logistic issues.
Discussion
Main findings
In contrast to other studies, the results obtained from this trial demonstrated that 15 mL/kg of INSI did not significantly reduce shoulder pain compared to no fluid instillation at 24 h, 48 h, or 72 h post gynaecological laparoscopy procedure. However, similar to previous trials, our data revealed that upper abdominal pain was significantly improved at 48 h and 72 h after INSI of 15 mL/kg.
Strengths and limitations
In our opinion, this trial was designed with adequate precaution to eliminate preventable bias and modestly fill the research gap on the efficacy of INSI 15 mL/kg body weight in reducing postoperative pain, the lowest dose tested by previous researchers.
Our study has certain limitations. First, the sample size of this study was relatively small, limiting the generalisation of the results. Second, the differences in patient characteristics were a source of bias that could affect the stability of the results. Moreover, although all surgeons were advised to actively evacuate the retained carbon dioxide with gentle pressure on the abdomen, some surgeons may have performed it better than others, contributing to another source of bias.
Another major limitation is lack of blinding of the laparoscopic surgeons. Complete blinding is not practical as the act of not instilling and instilling fluid is not concealable from the surgeons performing the surgery.
Interpretation
Our findings were inconsistent with the findings of previous researchers, which could be due to the amount of INSI we chose to instil and/or characteristic differences in our patients.
We opted for a lower amount of INSI in order to minimise excessive indwelling normal saline in the peritoneal cavity. In the trials carried out by Tsai et al. [10, 11], the amount of saline instilled was up to 30 mL/kg body weight. The team suggested that intraperitoneal absorption is estimated to be approximately 30–60 mL/h [19, 26]; therefore, the concern about fluid shifts is reduced. However, the absorption rate cited was for Ringer’s Lactate [19, 26], whose composition differs from that of normal saline. The rate of intraperitoneal absorption of normal saline is still being investigated. However, when 1 L of normal saline was instilled into the peritoneal cavity laparoscopically, it was fully absorbed after 16 h [20, 27]. In our trial, the normal saline fluid instilled ranged between 500 and 1500 mL depending on the patient’s weight.
Excessive indwelling intraperitoneal normal saline promotes formation of peritoneal adhesions [20, 21, 28]. Despite its non-physiological composition [20] normal saline is commonly used to wash the abdominal cavity during open and laparoscopic surgeries to remove remnants of blood and other fluids [29]. However, complete removal of the fluid during surgery is not always possible. A previous study demonstrated that patients undergoing laparoscopic surgery had at least 25% of residual normal saline in the abdominal cavity despite the surgeon's best effort to evacuate it, and this residual saline undergoes gradual absorption [21]. However, it was observed that as the saline dwelling in the peritoneal cavity undergoes compositional changes, it becomes less biocompatible to mesothelial cells, promoting peritoneal adhesion. Additionally, elastase activity is also increased in the indwelling fluid, reflecting an intraperitoneal inflammatory reaction [28]. However, the use of normal saline continues, especially for postoperative pain reduction during laparoscopy procedures due to a vast amount of available data validating its safety and efficacy [7, 8, 10, 11, 13, 30, 31]. Furthermore, when Hartmann’s or Ringer’s lactate solution was used instead of normal saline, there was no noticeable improvement in pain score [32].
Second, compared to Tsai et al. [10], the patients’ characteristics in this trial showed a higher prevalence of nulliparous women (control, 47.1%; INSI, 35.3%) than multiparous women. Abdominal wall laxity significantly influences the type of pain perceived by the patient [33]. The shoulder and upper abdominal pain are results of distension and irritation of the peritoneum. Multiparous women tend to have less stretching and irritation of the peritoneum than nulliparous women. Therefore, it is reasonable to say that the rigid abdominal wall of nulliparous women leads to higher incidences of postoperative pain [33]. Additionally, other studies [34, 35] also reported being unsuccessful in reducing postoperative pain with some manoeuvres.
Other advantages of INSI include its potential to provide long-lasting and persistent pain relief [10]. Similar to previous trials, our data revealed that upper abdominal pain was significantly improved at 48 h and 72 h post-INSI of 15 mL/kg body weight. The rationale for observing pain scores up to 72 h was that pain after a laparoscopic procedure may last up to 3 days and even up to 5 weeks [32, 36, 37]. However, no studies have assessed pain scores beyond 48 h post gynaecological laparoscopic procedures. Here, we provide data on pain scores 72 h after gynaecological surgery.
Conclusions
In conclusion, instillation of normal saline of 15 mL/kg body weight at the end of any benign gynaecological laparoscopic surgery does not improve shoulder pain. However, a modest improvement in pain score was observed in the upper abdominal area 48 h and 72 h post-procedure. The option to increase the amount of saline instillation to up to 30 mL/kg body weight in order to improve pain score should be carefully evaluated, considering that INSI may result in development of peritoneal adhesions even at lower amounts. Thus, a longitudinal controlled randomised trial should be conducted to address the occurrence of postoperative peritoneal adhesions after INSI.
Acknowledgements
The authors would like to thank all the patients who participated in this study, the health care professionals, and staff from the Department of Anaesthesia and the Department of Obstetrics and Gynaecology, University of Malaya Medical Centre (UMMC).
Abbreviations
- ASA
American Society of Anaesthesiologists
- INSI
Intraperitoneal normal saline instillation
- ISRCTN
International Standardised Randomised Controlled Trial Number
- MREC
Ministry of Health Research and Ethics Committee
- NMRR
National Medical Research Register
- RA-A
First research assistant
- RA-B
Second research assistant
- VAS
Visual analogue score
Author contributions
ASAA, JMKA, and HZMT conceived and designed the experiments. ASAA, MK, RCSL, and DSWN recruited patients and performed the experiments. JMKA and HZMT analysed the data. ASAA, JMKA, DNSW, MK, and HZMT wrote the manuscript. All authors read and approved the final manuscript.
Funding
This trial received no external funding or grants.
Availability of data and materials
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
This trial was conducted in accordance with the Declaration of Helsinki (2000) for human studies. This study was registered and approved by the Ministry of Health Research and Ethics Committee (MREC) of the National Medical Research Register and the Clinical Research Centre (NMRR), Malaysia (ID: NMRR-19-1532-48232. Date: 06/03/2019), and the Medical Research Ethics Committee of the University Malaya Medical Centre (MREC ID No: 201926-7106. Date: 20/03/2019). Additionally, the International Standardised Randomised Controlled Trial Number (ISRCTN) for this study was registered with an ID of 87898051 (https://doi.org/10.1186/ISRCTN87898051) (Date: 26/06/2019). Written informed consent was obtained from all participants prior to the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Gan TJ. Poorly controlled postoperative pain: prevalence, consequences, and prevention. J Pain Res. 2017;10:2287–2298. doi: 10.2147/JPR.S144066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kato J, Ogawa S, Katz J, Nagai H, Kashiwazaki M, Saeki H, Suzuki H. Effects of presurgical local infiltration of bupivacaine in the surgical field on postsurgical wound pain in laparoscopic gynecologic examinations: a possible preemptive analgesic effect. Clin J Pain. 2000;16(1):12–17. doi: 10.1097/00002508-200003000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Bafort C, Beebeejaun Y, Tomassetti C, Bosteels J, Duffy JM. Laparoscopic surgery for endometriosis. Cochrane Database Syst Rev. 2020;10:CD011031. doi: 10.1002/14651858.CD011031.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Duffy J, Hirsch M, Vercoe M, Abbott J, Barker C, Collura B, et al. endo:outcomes—an International Collaboration Harmonising Outcomes and Outcome Measures for Endometriosis Research. A core outcome set for future endometriosis research: an international consensus development study. BJOG. 2020;127(8):967–74. doi: 10.1111/1471-0528.16157. [DOI] [PubMed] [Google Scholar]
- 5.Sao CH, Chan-Tiopianco M, Chung KC, Chen YJ, Horng HC, Lee WL, et al. pain after laparoscopic surgery: focus on shoulder-tip pain after gynecological laparoscopic surgery. J Chin Med Assoc. 2019;82(11):819–826. doi: 10.1097/JCMA.0000000000000190. [DOI] [PubMed] [Google Scholar]
- 6.Azhary JMK, Adlan AA, Balakrishnan S, Baharain SRK, Zaidi SNSJH, Razali N, et al. Intraperitoneal ropivacaine for postoperative pain following laparoscopic tubal ligation: a randomised double-blind placebo-controlled trial. CEOG. 2021;48(3):654–60. [Google Scholar]
- 7.Kaloo P, Armstrong S, Kaloo C, Jordan V. Interventions to reduce shoulder pain following gynaecological laparoscopic procedures. Cochrane Database Syst Rev. 2019;1(1):CD011101. doi: 10.1002/14651858.CD011101.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Taş B, Donatsky AM, Gögenur I. Techniques to reduce shoulder pain after laparoscopic surgery for benign gynaecological disease: a systematic review. Gynecol Surg. 2013;10:169–175. doi: 10.1007/s10397-013-0791-7. [DOI] [Google Scholar]
- 9.Suginami R, Taniguchi F, Suginami H. Prevention of postlaparoscopic shoulder pain by forced evacuation of residual CO(2) JSLS. 2009;13(1):56–59. [PMC free article] [PubMed] [Google Scholar]
- 10.Tsai HW, Wang PH, Yen MS, Chao KC, Hsu TF, Chen YJ. Prevention of postlaparoscopic shoulder and upper abdominal pain: a randomised controlled trial. Obstet Gynecol. 2013;121(3):526–531. doi: 10.1097/AOG.0b013e318283fcca. [DOI] [PubMed] [Google Scholar]
- 11.Tsai HW, Chen YJ, Ho CM, Hseu SS, Chao KC, Tsai SK, Wang PH. Maneuvers to decrease laparoscopy-induced shoulder and upper abdominal pain: a randomised controlled study. Arch Surg. 2011;146(12):1360–1366. doi: 10.1001/archsurg.2011.597. [DOI] [PubMed] [Google Scholar]
- 12.Riedel HH, Semm K. Das postpelviskopische-(laparoskopische) Schmerzsyndrom [The post-laparoscopic pain syndrome (author's syndrome)] Geburtshilfe Frauenheilkd. 1980;40(7):635–643. doi: 10.1055/s-2008-1037224. [DOI] [PubMed] [Google Scholar]
- 13.Davari-Tanha F, Samimi S, Khalaj Z, Bastanhagh E. Comparison of intraperitoneal normal saline infusion with pulmonary recruitment maneuver in reducing shoulder and upper abdomen pain following gynecologic laparoscopic procedures: a randomised, controlled, triple-blind trial. Anesth Pain Med. 2019;9(3):e92444. doi: 10.5812/aapm.92444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Koninckx PR, Gomel V, Ussia A, Adamyan L. Role of the peritoneal cavity in the prevention of postoperative adhesions, pain, and fatigue. Fertil Steril. 2016;106(5):998–1010. doi: 10.1016/j.fertnstert.2016.08.012. [DOI] [PubMed] [Google Scholar]
- 15.Molinas CR, Mynbaev O, Pauwels A, Novak P, Koninckx PR. Peritoneal mesothelial hypoxia during pneumoperitoneum is a cofactor in adhesion formation in a laparoscopic mouse model. Fertil Steril. 2001;76:560–567. doi: 10.1016/S0015-0282(01)01964-1. [DOI] [PubMed] [Google Scholar]
- 16.Molinas CR, Koninckx PR. Hypoxaemia induced by CO2 or helium pneumoperitoneum is a co-factor in adhesion formation in rabbits. Hum Reprod. 2000;15:1758–1763. doi: 10.1093/humrep/15.8.1758. [DOI] [PubMed] [Google Scholar]
- 17.Ryan GB, Grobety J, Majno G. Mesothelial injury and recovery. Am J Pathol. 1973;71:93–112. [PMC free article] [PubMed] [Google Scholar]
- 18.Polubinska A, Breborowicz A, Staniszewski R, Oreopoulos DG. Normal saline induces oxidative stress in peritoneal mesothelial cells. J Pediatr Surg. 2008;43:1821–1826. doi: 10.1016/j.jpedsurg.2008.02.010. [DOI] [PubMed] [Google Scholar]
- 19.Polubinska A, Winckiewicz M, Staniszewski R, Breborowicz A, Oreopoulos DG. Time to reconsider saline as the ideal rinsing solution during abdominal surgery. Am J Surg. 2006;192:281–285. doi: 10.1016/j.amjsurg.2005.05.047. [DOI] [PubMed] [Google Scholar]
- 20.Breborowicz A, Oreopoulos DG. Is normal saline harmful to the peritoneum? Perit Dial Int. 2005;25(Suppl 4):S67–70. doi: 10.1177/089686080502504S09. [DOI] [PubMed] [Google Scholar]
- 21.Cwalinski J, Staniszewski R, Baum E, Jasinski T, Mackowiak B, Breborowicz A. Normal saline may promote formation of peritoneal adhesions. Int J Clin Exp Med. 2015;8:8828–8834. [PMC free article] [PubMed] [Google Scholar]
- 22.Tabibian N, Swehli E, Boyd A, Umbreen A, Tabibian JH. Abdominal adhesions: a practical review of an often overlooked entity. Ann Med Surg (Lond) 2017;15:9–13. doi: 10.1016/j.amsu.2017.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wang T, Heimbürger O, Qureshi AR, Waniewski J, Bergström J, Lindholm B. Physiological saline is not a biocompatible peritoneal dialysis solution. Int J Artif Organs. 1999;22(2):88–93. doi: 10.1177/039139889902200206. [DOI] [PubMed] [Google Scholar]
- 24.American society of anesthesiologists physical status classification Created October 15, 2014. https://www.asahq.org/standards-and-guidelines/asa-physical-status-classification-system?&ct=c806c69af52735d6d08f41c1504d75023cfd2375a3be08d2d0f0be1b3a6fff02e0bd5122ab83a02063a8bf5ff5978c2018dd64933c678817928fbd9ddc329cf3. Accessed 15 Feb 2022.
- 25.Malaysia Ministry of Health. Pain as the 5th vital sign guidelines: 2nd edition. 2013.
- 26.Muzii L, Bellati F, Manci N, Zullo MA, Angioli R, Panici PB. Ringer's lactate solution remains in the peritoneal cavity after laparoscopy longer than expected. Fertil Steril. 2005;84(1):148–153. doi: 10.1016/j.fertnstert.2005.01.111. [DOI] [PubMed] [Google Scholar]
- 27.Hart R, Magos A. Laparoscopically instilled fluid: the rate of absorption and the effects on patient discomfort and fluid balance. Gynaecol Endosc. 1996;5(5):287–291. doi: 10.1046/j.1365-2508.1996.2610231.x. [DOI] [Google Scholar]
- 28.Hellman C, Lundahl J, Hylander B, Halldén G. Phenotypic alterations of recruited eosinophils in peritoneal fluid eosinophilia. Perit Dial Int. 2000;20(3):295–300. doi: 10.1177/089686080002000305. [DOI] [PubMed] [Google Scholar]
- 29.Evans DM, McAree K, Guyton DP, Hawkins N, Stakleff K. Dose dependency and wound healing aspects of the use of tissue plasminogen activator in the prevention of intra-abdominal adhesions. Am J Surg. 1993;165:229–232. doi: 10.1016/S0002-9610(05)80516-1. [DOI] [PubMed] [Google Scholar]
- 30.van Dijk JEW, Dedden SJ, Geomini PMAJ, Meijer P, van Hanegem N, Bongers MY. POstLAparoscopic Reduction of pain By combining intraperitoneal normal saline And the pulmonary Recruitment maneuver (POLAR BEAR trial). RCT to estimate reduction in pain after laparoscopic surgery when using a combination therapy of intraperitoneal normal saline and the pulmonary recruitment maneuver. BMC Womens Health. 2017;17(1):42. doi: 10.1186/s12905-017-0397-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sao CH, Chan-Tiopianco M, Chung KC, Chen YJ, Horng HC, et al. Pain after laparoscopic surgery: focus on shoulder-tip pain after gynecological laparoscopic surgery. Crit Care Med. 2019;82(11):819–826. doi: 10.1097/JCMA.0000000000000190. [DOI] [PubMed] [Google Scholar]
- 32.Jothilakshmi PK, Watson AJS, Ousta B, et al. Intra-peritoneal Hartmann’s Solution as analgesia for diagnostic laparoscopy: a pilot prospective randomised controlled trial. Gynecol Surg. 2008;5:103–107. doi: 10.1007/s10397-007-0341-2. [DOI] [Google Scholar]
- 33.Hsien CF, Wang CL, Long CY, Chen YH, Lee WY, Chen SC, et al. Factors associated with types and intensity of postoperative pain following gynecological laparoscopic surgery: a cross-sectional study. Biomed Res Int. 2017;2017:2470397. doi: 10.1155/2017/2470397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Alexander JI, Hull MG. Abdominal pain after laparoscopy: the value of a gas drain. Br J Obstet Gynaecol. 1987;94(3):267–269. doi: 10.1111/j.1471-0528.1987.tb02366.x. [DOI] [PubMed] [Google Scholar]
- 35.Dobbs FF, Kumar V, Alexander JI, Hull MG. Pain after laparoscopy related to posture and ring versus clip sterilisation. Br J Obstet Gynaecol. 1987;94(3):262–266. doi: 10.1111/j.1471-0528.1987.tb02365.x. [DOI] [PubMed] [Google Scholar]
- 36.Alexander JI. Pain after laparoscopy. Br J Anaesth. 1997;79(3):369–378. doi: 10.1093/bja/79.3.369. [DOI] [PubMed] [Google Scholar]
- 37.Dixon JB, Reuben Y, Halket C, O’Brien PE. Shoulder pain is a common problem following laparoscopic adjustable gastric band surgery. Obes Surg. 2005;15(8):1111–1117. doi: 10.1381/0960892055002149. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.