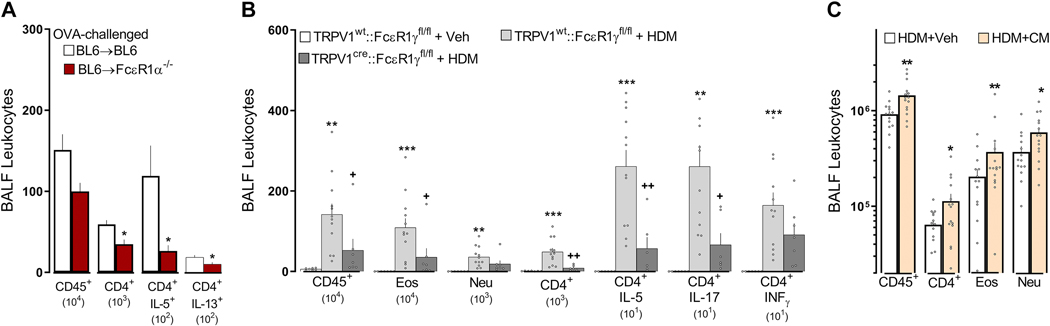
Figure 6: FcεR1+ nociceptor neurons initiate type 2 airway inflammation.
One day after an acute OVA challenge, allergen-sensitized FcεR1α−/− chimeric mice (BL6⟶FcεR1α−/−) displayed a reduced level of AAI (lowered numbers of BALF-infiltrating leukocytes, CD45+, CD4+) and polarization (IL-5+, IL-13+) in comparison with allergen-sensitized control (BL6⟶BL6) mice (A). Next, we used the cre/lox toolbox to generate the first cell- specific FcεR1γ knockdown (TRPV1Cre::FcεR1γfl/fl) and littermate control (TRPV1wt::FcεR1γfl/fl) mice. TRPV1Cre::FcεR1γfl/fl mice were protected from HDM-challenge-induced BALF infiltration of CD45+, eosinophils, and CD4+ as well as CD4 polarization (IL-5, IL-17; B). HDM-challenged mice exposed to neuron-conditioned media harvested from IgE-OVA-stimulated allergen-sensitized JNC neurons demonstrated increased AAI (BALF influx of CD45+, CD4+, eosinophils, neutrophils; C). Mean ± S.E.M; Two-tailed unpaired Student’s t-test (A, C); one-way ANOVA post-hoc Bonferroni (B); n = 5–14 animals/group, 2 cohorts.