Abstract
Study Design
Retrospective cohort study.
Objectives
The objective of this study is to compare the likelihood of missing a scheduled telemedicine and in-person appointments for spine patients. The secondary objective is to assess the impact of socioeconomic status on missed telemedicine and in-person appointments.
Methods
Patients with scheduled outpatient appointments with orthopedic spine faculty between 2019 and 2021 were divided by appointment type: telemedicine (N = 4,387) and in-person (N = 3810). Socioeconomic status was assessed using Area Deprivation Index (ADI) stratified based on percentile: low (<25), medium (25–75), and high (>75) levels of socioeconomic disadvantage. The primary outcome measure was missed clinic appointments, which was defined as having at least one appointment that was cancelled or labeled “no show.”
Results
Patients with in-person appointments missed appointments more often than patients with telemedicine visits (51.3% vs 24.7%, P < .001). Patients with high ADI missed their in-person appointments more often than patients with medium and low ADI (59.5% vs 52.2% and 47.5%, P < .001). There was no difference in missed telemedicine visits between patients with high, medium, and low ADI (27.6% vs 24.8% vs 23.8%, P = .294). Patients that missed an appointment were 41.9% more likely to be high ADI (OR 1.42, 95% CI 1.20–1.68, P < .001) and 13.4% more likely to be medium ADI (OR 1.13, 95% CI 1.03–1.26, P = .015) compared with low ADI patients.
Conclusions
Telemedicine may serve a role in reducing disparity in appointment attendance. While further studies are needed to validate these findings, spine surgeons should consider offering telemedicine as an option to patients.
Keywords: telemedicine, COVID-19 pandemic, orthopedic spine, area deprivation index, missed appointments
Introduction
Telemedicine was initially developed to expand healthcare access to patients in rural areas.1,2 However, the adoption had been slow as of 2017, with an estimated prevalence of 7 telemedicine visits per year per 1000 providers in the United States. 3 During the height of the coronavirus disease 2019 (COVID-19) pandemic, in-person appointments were restricted, necessitating the rapid implementation of telemedicine. 4 Spine surgeons had to rely on telemedicine to continue post-operative follow-ups and provide consultation for new patients. Multiple studies have demonstrated that telemedicine is more cost-effective, increases clinic efficiency, and reduces wait times compared to traditional in-person appointments.5-7 Furthermore, telemedicine has also been shown to have high satisfaction among spine patients and a low rate (4–6%) of surgical plan changes following in-person preoperative evaluation.8-10 Modified neurological exam protocols were also developed for telemedicine visits to address the limitation of the traditional spine exam.11-13 As the pandemic gradually wanes and the COVID restrictions are relaxed, in-person appointments have resumed for spine patients. Despite the reported benefits, the incorporation of telemedicine into the post-COVID spine practice is still unclear, particularly with identifying which patients would benefit the most from telemedicine.
Telemedicine has been promoted as a potential solution to reduce healthcare inequities. Patients with low socioeconomic status face many barriers to healthcare access. In addition to financial constraints and lack of health insurance, these patients often rely on inconsistent transportation or limited public transportation to access outpatient follow-up care. 14 They are also more likely to have inflexible jobs that limit their ability to attend clinic during work hours.14,15 Studies have shown that lower socioeconomic status is associated with higher missed appointment rates.16,17 Furthermore, poor follow-up has been associated with delayed diagnosis and treatment, inferior control of chronic diseases, and worse outcomes across multiple patient populations.18-22 Attending post-operative follow-up appointments is critical for monitoring and preventing post-operative complications. 17 Furthermore, missed appointments also decrease clinical efficiency through unfulfilled appointment times, decreased revenue, and lower staff satisfaction. 23 Therefore, telemedicine may serve a key role in helping disadvantaged patients attend their appointments while maintaining standard patient care and improved continuity of care.
The primary objective of this study is to compare the likelihood of missing scheduled telemedicine visits and in-person appointments for spine patients. The secondary objective is to assess the impact of socioeconomic status on missing telemedicine and in-person appointments. Using this retrospective single institution study, we hypothesize that telemedicine improves appointment attendance, particularly for spine patients with low socioeconomic status.
Methods
Patient Selection and Data Collection
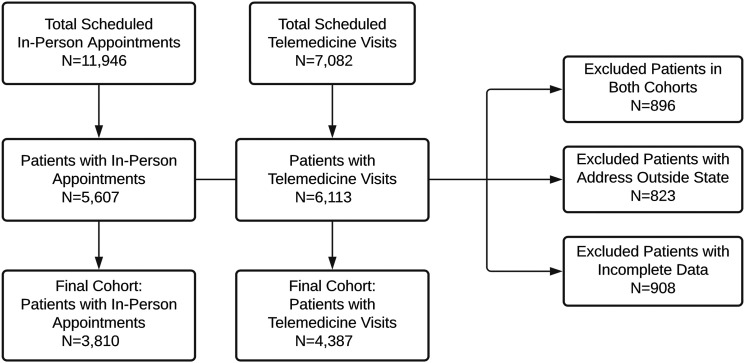
Our Institutional Review Board approved this study (HP-00091846) and granted exemption from informed consent for this retrospective study. Patients with scheduled outpatient appointments with the orthopedic spine division at an urban tertiary care academic center were identified. We followed the Strengthening the Report of Observational Studies in Epidemiology (STROBE) Guidelines to ensure high quality of this study. 24 11 946 in-person appointments from January 2019 to December 2019 and 7082 telemedicine visits from April 2020 to April 2021 were identified via electronic medical record (EMR) query of all appointments scheduled with the orthopedic spine faculty. Patients were included if they were 18 years of age and older. Patients were excluded if (1) their primary residence was out of state (N = 823), (2) they fell into both study cohorts (N = 896), or (3) they had missing demographic data (N = 908). Patients were divided into two cohorts by appointment type: telemedicine or in-person appointment. Due to the onset of the COVID pandemic in late March 2020, the telemedicine cohort included all patients who had at least one telemedicine appointment scheduled between April 2020 and April 2021. The in-person cohort included patients who had at least one in-person appointment scheduled prior to the COVID pandemic, between January 2019 and December 2019. The final cohorts consisted of 4387 patients with telemedicine visits and 3,810 patients with in-person appointments. A flowchart of the patient selection methodology is included in Figure 1.
Figure 1.
Flowchart of the study population selection criteria demonstrating included and excluded patients for the telemedicine and in-person appointment cohorts.
Demographic information, such as age, sex, race, insurance type, and primary residential address were obtained from the patient’s EMR. Patients’ addresses were used to calculate the Area Deprivation Index (ADI), which is a validated measure of socioeconomic status based on the United States census data. The ADI is a standardized score with mean of 100 and standard deviation of 20. 25 The ADI is more often reported as a percentile across all neighborhoods in the US. In this study, an ADI of 0 represents the 0th percentile or the least disadvantaged neighborhood, whereas 100 represents the 100th percentile or the most disadvantaged neighborhood.26,27 ADI was also stratified into low (<25), medium (25–75), and high (>75) levels of socioeconomic disadvantage. The demographic characteristics of the overall study cohort are presented in Table 1.
Table 1.
Demographic Characteristics of Patients with Scheduled Appointments by Type.
| Telemedicine Visit | In-Person Appointment | P-value | |
|---|---|---|---|
| Total Patients | 4387 | 3810 | |
| Age | 55.6 ± 15.5 [95% CI, 55.2–56.1] | 55.0 ± 16.7 [95% CI, 54.5–55.5] | .101 |
| Age (>65) | 1349 (30.8%) | 1148 (30.1%) | .544 |
| Sex | .003 | ||
| Male | 1882 (42.9%) | 1759 (46.2%) | |
| Female | 2505 (57.1%) | 2051 (53.8%) | |
| Race | <.001 | ||
| White | 2837 (64.7%) | 2298 (60.3%) | |
| Black | 1142 (26.0%) | 1034 (27.1%) | |
| Asian | 58 (1.32%) | 65 (1.71%) | |
| Other | 350 (7.98%) | 413 (10.8%) | |
| Insurance | .358 | ||
| Commercial | 1856 (42.3%) | 1661 (43.6%) | |
| Medicare | 1438 (32.8%) | 1199 (31.5%) | |
| Medicaid/MCO | 797 (18.2%) | 704 (18.5%) | |
| Other | 296 (6.75%) | 246 (6.46%) | |
| ADI | 36.3 ± 22.3 [95% CI, 35.7–37.0] | 37.1 ± 23.3 [95% CI, 36.3–37.8] | .502 |
| ADI Stratified a | .051 | ||
| Low | 1590 (36.2%) | 1384 (36.3%) | |
| Medium | 2420 (55.2%) | 2041 (53.6%) | |
| High | 377 (8.59%) | 385 (10.1%) |
aArea Deprivation Index (ADI) was stratified into Low (<25), Medium (25–75), and High (>75).
Outcome
The primary outcome measure was missed appointments, which was defined as having at least one appointment that was cancelled or labeled as “no show.”
Statistical Analysis
Data was managed using Microsoft Excel (Microsoft, Redmond, WA, USA). Mean, standard deviation, median, and 95% confidence intervals (CI) were calculated for continuous variables. The Shapiro–Wilk test was used to assess for normality of continuous variables. Student’s T-test was used to evaluate continuous variables with normal distribution and Wilcoxon’s rank-sum test was used as the non-parametric alternative for continuous variables. Frequencies were calculated for categorical variables. Fisher’s exact test and Chi-square analysis were used to evaluate relationships between categorical variables. An a priori alpha was set at .05 for significance.
To identify the strongest drivers of missing appointments, patients’ age, sex, and ADI were analyzed using the gamma distribution with log link function (within PROC GLIMMIX in SAS statistical software) since these variables were highly skewed. Odds ratios (OR) with 95% CI were reported for missed appointments, a binary outcome. All analyses were performed using SAS v9.4 statistical software (SAS Institute, Cary, NC).
Results
Overall, patients with scheduled telemedicine visits, compared to in-person appointments, were more often female (57.1% vs 53.8%, P = .003) (Table 1). There was also a significant difference in race between the telemedicine and in-person cohorts (P < .001). However, there was no significant difference in insurance (P = .358) or ADI, both as a percentile (P = .502) and as a stratified variable (P = .051).
While the two cohorts had a similar number of scheduled appointments (P = .795), patients with in-person appointments were more likely to miss an appointment compared with patients with telemedicine visits (51.3% vs 24.7%, P < .001). Across all levels of ADI (low, medium, and high), patients were more likely to miss an in-person appointment than a telemedicine visit (Table 2).
Table 2.
Missed Visit by Appointment Type and Socioeconomic Status.
| Telemedicine Visit | In-Person Appointment | P-value | |
|---|---|---|---|
| Total Patients | 4387 | 3810 | |
| Total Scheduled Visits (median, IGR) | 2.00 (1.00–3.00) | 2.00 (1.00–3.00) | .795 |
| Missed Visit | 1080 (24.7%) | 1953 (51.3%) | <.001 |
| Missed Visit by ADI a | |||
| Low | 378 (23.8%) | 658 (47.5%) | <.001 |
| Medium | 601 (24.8%) | 1066 (52.2%) | <.001 |
| High | 104 (27.6%) | 229 (59.5%) | <.001 |
aArea Deprivation Index (ADI) was stratified into Low (<25), Medium (25–75), and High (>75).
Patients with high ADI were more likely to have an in-person appointment scheduled than patients with medium and low ADI (50.5% vs 45.8% and 46.5%, P < .001) (Table 3). Patients with high ADI were also more likely to miss an in-person appointment than patients with medium and low ADI (59.5% vs 52.2% and 47.5%, P < .001). However, there was no significant difference in the likelihood of missed telemedicine visit between patients with high, medium, and low ADI (P = .294).
Table 3.
Appointment Type and Missed Visit by Socioeconomic Status.
| ADI Low a | ADI Medium | ADI High | P-value | |
|---|---|---|---|---|
| Total Patients | 2974 | 4461 | 762 | |
| Appointment Type | <.001 | |||
| In-Person | 1384 (46.5%) | 2041 (45.8%) | 385 (50.5%) | |
| Telemedicine | 1590 (53.5%) | 2420 (54.2%) | 377 (49.5%) | |
| Missed Visit | 1036 (34.8%) | 1667 (37.4%) | 333 (43.7%) | <.001 |
| In-Person | 658 (47.5%) | 1066 (52.2%) | 229 (59.5%) | <.001 |
| Telemedicine | 378 (23.8%) | 601 (24.8%) | 104 (27.6%) | .294 |
aArea Deprivation Index (ADI) was stratified into Low (<25), Medium (25–75), and High (>75).
After controlling for age, patients with telemedicine visits were 14.6% more likely to be female (OR 1.15, 95% CI 1.05–1.25, P = .002) and 15.6% less likely to be a patient with high ADI (OR .84, 95% CI .72–.99, P = .039) (Table 4). After controlling for age and sex, patients with at least one missed appointment were 41.9% more likely to be high ADI (OR 1.42, 95% CI 1.20–1.68, P < .001) and 13.4% more likely to be medium ADI (OR 1.13, 95% CI 1.03–1.26, P = .015) compared with patients with low ADI, and 68.9% less likely to have a telemedicine visit (OR .31, 95% CI .28–.34, P < .001) than an in-person appointment.
Table 4.
Multivariate Analysis for Predictors of Missed Visit.
| Category | Reference | Odds Ratio | 95% Confidence Interval | P-value | |
|---|---|---|---|---|---|
| Age | >65 years old | 18–65 years old | .991 | .895–1.098 | .864 |
| Sex | Female | Male | 1.038 | .945–1.141 | .434 |
| Appointment Type | Telemedicine | In-person appointment | .311 | .284–.342 | <.001 |
| ADI Stratified a | Medium | Low | 1.134 | 1.025–1.255 | .015 |
| High | Low | 1.419 | 1.198–1.681 | <.001 |
aArea Deprivation Index (ADI) was stratified into Low (<25), Medium (25–75), and High (>75).
Discussion
Telemedicine allowed spine surgeons to continue providing patient care and post-operative follow-up amid the COVID-19 pandemic. As society slowly transitions back to traditional care models and in-person appointments resume, questions remain regarding the future role of telemedicine in spine practice. This retrospective review of more than 8000 outpatient orthopedic spine appointments found that patients were less likely to miss telemedicine visits compared to in-person appointments regardless of socioeconomic status.
Missed appointments and poor follow-up have been associated with worse outcomes in multiple specialties.17-22 In orthopedics, regular follow-up appointments ensure patients receive proper treatment for their musculoskeletal conditions and prevent over-reliance on pain medication. Post-operative appointments are important for early identification of complications, such as impaired wound healing and wound infections. Consistent post-operative follow-up also facilitates close monitoring of functional status and radiographic outcomes. 28 Therefore, it is hypothesized that poor follow-up is associated with worse outcomes in orthopedics. Murray et al. followed 2268 total hip arthroplasty patients and reported a 20% cumulative loss to follow-up rate after 15 years. The patients who were lost to follow-up had worse pain, more stiffness, and more radiographic evidence of deterioration at their last recorded follow-up. 29
The effect of poor appointment attendance on outcomes following spine surgery is less clear. Solberg et al. studied 633 patients who underwent surgery for degenerative lumbar conditions and recontacted the 22% of patients who were lost to follow-up at 2 years. They found no significant difference in VAS for back pain and EQ-5D in patients lost to follow-up compared to those who were not. 30 While this short-term study covers early post-operative complications, long-term studies are needed to assess the impact of poor follow-up on long-term outcomes, such as reoperation rates, symptomatic adjacent segment disease, and long-term opioid-use. Furthermore, there is growing evidence that patients lost to follow-up may have more severe and symptomatic spinal disease. Bisson et al. reported that of the 608 patients who underwent one- or two-level decompression and fusion surgery, the 14.5% of patients who were lost to follow-up at 2 years had higher baseline back pain scores, higher Oswestry Disability Index (ODI), and lower EQ-5D scores. 31 Therefore, greater effort should be made to identify these patients and encourage appointment attendance.
In this study, spine patients with telemedicine appointments were 69% less likely to miss an appointment than patients with in-person appointments. While this finding has yet to be reported in the spine literature, this reduction of missed appointment for telemedicine visits has been reported in other specialties, such as diabetes management, high-risk obstetrics, and orthopedic trauma.32,33 Notably, telemedicine alleviates some of the barriers to access for patients with low socioeconomic status, who might rely on limited public transportation, have inflexible work hours, or have family obligations that hinder their ability to attend in-person appointments. 34 In this study, spine patients with lower socioeconomic status were 42% more likely to miss in-person appointments than patients with high socioeconomic status. While there is a lack of spine literature on this topic, the relationship between socioeconomic status and poor clinic follow-up has been extensively studied in the orthopedic trauma population. A retrospective review of 2165 patients who underwent orthopedic trauma surgery at a level I trauma center found that tobacco use, non-commercial insurance, and increased distance (>100 miles) from the clinic were independently associated with failure to follow-up. 35 Notably, the trauma population is younger (48.4 vs 55.0 years old), male (61% vs 46%), and had higher mean ADI (42.6 vs 37.1) compared to the patients seeking elective spine appointments in this study. 36 Even still, the impact of socioeconomic status on poor follow-up was still observed in this spine population.
Interestingly, patients with lower socioeconomic status in this study had similar likelihood of missing a telemedicine visit as patients with intermediate and high socioeconomic status, suggesting that telemedicine could help bridge the disparity gap in access for patients with low socioeconomic status. This contrasts with previous concerns that patients with low socioeconomic status may have less access to a video communication device and sufficient internet speed needed to support telemedicine, exacerbating existing healthcare inequalities. 37
As the COVID-19 pandemic gradually resolves, in-person appointments have returned for many spine patients, raising questions as to how to incorporate telemedicine into spine practice. Hurley et al. surveyed 268 orthopedic surgeons and 73% plan on using telemedicine after the COVID-19 pandemic for new patient appointments, 88% for routine follow-ups, and 90% for post-operative follow-ups. 38 Building upon the previous literature that details telemedicine’s numerous benefits, our study provides evidence that spine surgeons should incorporate telemedicine into their practice to increase appointment attendance, particularly for patients with low socioeconomic status. As telemedicine continues to evolve, further research is needed to assess the differences in clinical outcomes between telemedicine and in-person appointments.
This study has some limitations. First, this is a retrospective study that compares in-person appointments in 2019 to telemedicine visits in 2020. Although desirable, a more direct comparison with similar time frames was not available since telemedicine was not common in spine practice prior to 2020 and in-person appointments in 2020 were heavily influenced by the COVID-19 pandemic. As a result, the specific time frames for each cohort were chosen to minimize the impact of COVID-19. Another limitation was that this study looked at all appointments globally and did not distinguish between new patient, follow-up, and post-operative appointments. Further studies should specifically assess each appointment category as certain appointment types, such as post-operative checks, may be more appropriate for telemedicine. Nonetheless, this is one of the first studies of its kind to investigate how telemedicine can impact access to care.
Conclusion
Spine patients were less likely to miss their telemedicine visits than in-person appointments. While patients with low socioeconomic status were more likely to miss in-person appointments than patients of higher socioeconomic status, there was no difference in the likelihood of missing a telemedicine appointment among patients of different socioeconomic status, suggesting that telemedicine may aid in reducing the barriers to healthcare access. While further studies are needed to validate these findings outside of COVID-19 restrictions, spine surgeons should consider offering telemedicine as an option to patients, particularly those with low socioeconomic status.
Footnotes
Author’s Note: Relevant financial activities outside submitted work: board membership, grants, royalties, stocks. The Manuscript submitted does not contain information about medical device(s)/drug(s).
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by Institutional Review Board approval was obtained for this study (HP-00091846).
Data Availability: The datasets generated during and/or analyzed during the current study are not publicly available but are available from the corresponding author on reasonable request.
ORCID iDs
Alexandra E. Thomson https://orcid.org/0000-0001-5378-4417
Daniel Gelb https://orcid.org/0000-0002-7263-6177
Steven Ludwig https://orcid.org/0000-0002-3962-5724
References
- 1.Bashshur RL, Shannon GW, Krupinski EA, et al. National telemedicine initiatives: essential to healthcare reform. Telemed J E Health. 2009;15(6):600-610. doi: 10.1089/tmj.2009.9960. [DOI] [PubMed] [Google Scholar]
- 2.Gruca TS, Pyo TH, Nelson GC. Improving rural access to orthopaedic care through visiting consultant clinics. J Bone Joint Surg Am. 2016;98(9):768-774. doi: 10.2106/JBJS.15.00946. [DOI] [PubMed] [Google Scholar]
- 3.Barnett ML, Ray KN, Souza J, Mehrotra A. Trends in telemedicine use in a large commercially insured population, 2005-2017. JAMA. 2018;320(20):2147-2149. doi: 10.1001/jama.2018.12354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Peden CJ, Mohan S, Pagán V. Telemedicine and COVID-19: an observational study of rapid scale up in a US academic medical system. J Gen Intern Med. 2020;35(9):2823-2825. doi: 10.1007/s11606-020-05917-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Buvik A, Bergmo TS, Bugge E, Smaabrekke A, Wilsgaard T, Olsen JA. Cost-effectiveness of telemedicine in remote orthopedic consultations: randomized controlled trial. J Med Internet Res. 2019;21(2):e11330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Harno K, Arajärvi E, Paavola T, Carlson C, Viikinkoski P. Clinical effectiveness and cost analysis of patient referral by videoconferencing in orthopaedics. J Telemed Telecare. 2001;7(4):219-225. [DOI] [PubMed] [Google Scholar]
- 7.Clegg A, Brown T, Engels D, Griffin P, Simonds D. Telemedicine in a rural community hospital for remote wound care consultations. J Wound Ostomy Continence Nurs. 2011;38(3):301-304. [DOI] [PubMed] [Google Scholar]
- 8.Satin AM, Shenoy K, Sheha ED, et al. Spine patient satisfaction with telemedicine during the COVID-19 pandemic: a cross-sectional study. Global Spine J. 2020. doi: 10.1177/2192568220965521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Crawford AM, Lightsey HM, Xiong GX, Striano BM, Schoenfeld AJ, Simpson AK. Telemedicine visits generate accurate surgical plans across orthopaedic subspecialties. Arch Orthop Trauma Surg. 2021. doi: 10.1007/s00402-021-03903-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lightsey HM, 4th, Crawford AM, Xiong GX, Schoenfeld AJ, Simpson AK. Surgical plans generated from telemedicine visits are rarely changed after in-person evaluation in spine patients. Spine J. 2021;21(3):359-365. doi: 10.1016/j.spinee.2020.11.009. [DOI] [PubMed] [Google Scholar]
- 11.Tanaka MJ, Oh LS, Martin SD, Berkson EM. Telemedicine in the Era of COVID-19: the virtual orthopaedic examination. J Bone Joint Surg Am. 2020;102(12):e57. doi: 10.2106/JBJS.20.00609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Iyer S, Shafi K, Lovecchio F, et al. The spine physical examination using telemedicine: strategies and best practices. Global Spine J. 2020. doi: 10.1177/2192568220944129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Goyal DKC, Divi SN, Schroeder GD, et al. Development of a telemedicine neurological examination for spine surgery: a pilot trial. Clin Spine Surg. 2020;33(9):355-369. doi: 10.1097/BSD.0000000000001066. [DOI] [PubMed] [Google Scholar]
- 14.Syed ST, Gerber BS, Sharp LK. Traveling towards disease: transportation barriers to health care access. J Community Health. 2013;38(5):976-993. doi: 10.1007/s10900-013-9681-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fradgley EA, Paul CL, Bryant J. A systematic review of barriers to optimal outpatient specialist services for individuals with prevalent chronic diseases: what are the unique and common barriers experienced by patients in high income countries? Int J Equity Health. 2015;14:52. doi: 10.1186/s12939-015-0179-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dantas LF, Fleck JL, Cyrino Oliveira FL, Hamacher S. No-shows in appointment scheduling - a systematic literature review. Health Policy. 2018;122(4):412-421. doi: 10.1016/j.healthpol.2018.02.002. [DOI] [PubMed] [Google Scholar]
- 17.Whiting PS, Greenberg SE, Thakore RV, et al. What factors influence follow-up in orthopedic trauma surgery? Arch Orthop Trauma Surg. 2015;135(3):321-327. doi: 10.1007/s00402-015-2151-8. Epub 2015 Jan 24. PMID: 25617213. [DOI] [PubMed] [Google Scholar]
- 18.Nyandiko W, Vreeman R, Liu H, et al. Non-adherence to clinic appointments among HIV-infected children in an ambulatory care program in Western Kenya. J Acquir Immune Defic Syndr. 2013;63(2):e49–e55. [DOI] [PubMed] [Google Scholar]
- 19.Keren D, Matter I, Rainis T, et al. Getting the most from the sleeve: the importance of post-operative follow-up. Obes Surg. 2011;21(12):1887–1893. [DOI] [PubMed] [Google Scholar]
- 20.Karmisholt J, Andersen S, Laurberg P. Variation in thyroid function in subclinical hypothyroidism: importance of clinical follow-up and therapy. Eur J Endocrinol. 2011;164(3):317–323. [DOI] [PubMed] [Google Scholar]
- 21.Murray MJ, LeBlanc CH. Clinic follow-up from the emergency department: do patients show up? Ann Emerg Med. 1996;27(1):56–58. [DOI] [PubMed] [Google Scholar]
- 22.Komoroski EM, Graham CJ, Kirby RS. A comparison of interventions to improve clinic follow-up compliance after a pediatric emergency department visit. Pediatr Emerg Care. 1996;12(2):87–90. [DOI] [PubMed] [Google Scholar]
- 23.Lee SR, Dix DB, McGwin G, et al. Correlation of appointment times and subspecialty with the no-show rates in an orthopedic ambulatory clinic. J Healthc Manag. 2018;63(6):e159-e169. doi: 10.1097/JHM-D-17-00199. [DOI] [PubMed] [Google Scholar]
- 24.Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med. 2007;147(8):573-577. [DOI] [PubMed] [Google Scholar]
- 25.Knighton AJ, Savitz L, Belnap T, Stephenson B, VanDerslice J. Introduction of an area deprivation index measuring patient socioeconomic status in an integrated health system: implications for population health. EGEMS (Wash DC). 2016;4(3):1238. doi: 10.13063/2327-9214.1238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kind AJH, Buckingham W. Making neighborhood disadvantage metrics accessible: the neighborhood Atlas. N Engl J Med. 2018;378:2456-2458. doi: 10.1056/NEJMp1802313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.University of Wisconsin School of Medicine Public Health . Area Deprivation Index v3.0; 2019. Downloaded from https://www.neighborhoodatlas.medicine.wisc.edu/. June 1, 2021.
- 28.Rosenbaum JA, Blau YM, Fox HK, Liu XS, DiBartola AC, Goyal KS. Patient loss to follow-up after upper extremity surgery: a review of 2563 Cases. Hand (N Y). 2019;14(6):836-840. doi: 10.1177/1558944718787277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Murray DW, Britton AR, Bulstrode CJ. Loss to follow-up matters. J Bone Joint Surg Br. 1997;79(2):254-257. doi: 10.1302/0301-620x.79b2.6975. [DOI] [PubMed] [Google Scholar]
- 30.Solberg TK, Sørlie A, Sjaavik K, Nygaard ØP, Ingebrigtsen T. Would loss to follow-up bias the outcome evaluation of patients operated for degenerative disorders of the lumbar spine? Acta Orthop. 2011;82(1):56-63. doi: 10.3109/17453674.2010.548024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bisson EF, Mummaneni PV, Knightly J, et al. Assessing the differences in characteristics of patients lost to follow-up at 2 years: results from the quality outcomes database study on outcomes of surgery for grade I spondylolisthesis. J Neurosurg Spine. 2020;33:643-651. doi: 10.3171/2019.12.SPINE191155. [DOI] [PubMed] [Google Scholar]
- 32.Xu T, Pujara S, Sutton S, Rhee M. Telemedicine in the management of type 1 diabetes. Prev Chronic Dis. 2018;15:E13. doi: 10.5888/pcd15.170168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jeganathan S, Prasannan L, Blitz MJ, Vohra N, Rochelson B, Meirowitz N. Adherence and acceptability of telehealth appointments for high-risk obstetrical patients during the coronavirus disease 2019 pandemic. Am J Obstet Gynecol MFM. 2020;2(4):100233. doi: 10.1016/j.ajogmf.2020.100233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Arpey NC, Gaglioti AH, Rosenbaum ME. How socioeconomic status affects patient perceptions of health care: a qualitative study. J Prim Care Community Health. 2017;8(3):169-175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Whiting PS, Greenberg SE, Thakore RV, et al. What factors influence follow-up in orthopedic trauma surgery? Arch Orthop Trauma Surg. 2015;135(3):321-327. doi: 10.1007/s00402-015-2151-8. [DOI] [PubMed] [Google Scholar]
- 36.Ibrahim IO, Bangura A, O’Hara NN, Slobogean G, O’Toole RV, Langhammer CG. Telemedicine preserves access to post-operative care for orthopaedic trauma patients regardless of socioeconomic status. University of Maryland Department of Orthopaedics Nineteenth Annual Disputations; 2021. June 4. [Google Scholar]
- 37.Romano MF, Sardella MV, Alboni F, et al. Is the digital divide an obstacle to e-health? Ana analysis of the situation in Europe and in Italy. Telemed J E-Health Off J Am Telemed Assoc. 2015;21(1):24-35. [DOI] [PubMed] [Google Scholar]
- 38.Hurley ET, Haskel JD, Bloom DA, et al. The use and acceptance of telemedicine in orthopedic surgery during the COVID-19 pandemic. Telemed J E Health. 2021;27(6):657-662. doi: 10.1089/tmj.2020.0255. [DOI] [PubMed] [Google Scholar]