Abstract
Background:
Social determinants of health are associated with asthma prevalence and healthcare utilization in children with asthma, but are multifactorial and complex. Whether social determinants similarly influence exacerbation severity is not clear.
Objective:
Composite measures of social determinants of health and readmission outcomes were evaluated in a large regional cohort of 1403 school-age children admitted to a pediatric intensive care unit (PICU) for asthma.
Methods:
Residential addresses were geocoded and spatially joined to census tracts. Composite measures of social vulnerability and childhood opportunity, PICU readmission rates, and hospital length of stay were compared between neighborhood “hot spots,” where PICU admission rates per 1000 children are at or above the 90th percentile, versus non-hot spots.
Results:
228 (16%) of children resided within a neighborhood hot spot. Hot spots were associated with a higher (i.e., poorer) composite social vulnerability index ranking, reflecting differences in socioeconomic status, household composition and disability, and housing type and transportation. Hot spots also had a lower (i.e., poorer) composite childhood opportunity index percentile ranking, reflecting differences in the education, health and environment, and social and economic domains. Higher social vulnerability and lower childhood opportunity were associated with PICU readmission. Residing within a hot spot was further associated with a longer duration of hospital stay, individual inpatient bed days, and total census tract inpatient bed days.
Conclusions:
Social determinants of health identified by geospatial analyses are associated with more severe asthma exacerbation outcomes in children. Outpatient strategies that address both biological and social determinants of health are needed to optimally care for and prevent PICU admissions in children with asthma.
Keywords: social determinants of health, disparities, status asthmaticus, social vulnerability index, childhood opportunity index, pediatric intensive care unit, census tract, neighborhood, geocoding
INTRODUCTION
Asthma currently affects one out of every twelve children in the United States, with wide variations in prevalence within the pediatric population.1 It is increasingly recognized that social determinants of health, defined by the World Health Organization as the non-medical factors that influence health,2 impact asthma prevalence and associated outcomes in children.3 Indeed, social and environmental factors such as ethnicity, poverty, childhood adverse conditions, air pollution, discrimination due to race or ethnicity, and economic deprivation have been associated with health disparities in childhood asthma.4–9 However, these social determinants of health are complex and multiple environmental and psychosocial exposures may interact synergistically and lead to poor population outcomes.10 For example, although asthma exacerbations and hospital readmissions are disproportionately higher in black versus white children, these disparities are reduced when considering other variables of socioeconomic status, neighborhood features, and hardship.11, 12
Critical and near-fatal asthma are defined as an asthma exacerbation serious enough to be life-threatening and that results in admission to a pediatric intensive care unit (PICU) or in endotracheal intubation and care in a PICU, respectively. We13 and others14 have previously shown that poverty and black race are associated with PICU admission for critical and near-fatal asthma in children.13 However, few studies to date have focused on more comprehensive population-level analysis of social determinants of PICU admission in this population. The Social Vulnerability Index15 (SVI) is a composite measure of neighborhood (census tract) themes based on socioeconomic status, household composition and disability, minority status and language, and housing and transportation. The SVI has been used to determine the association of social determinants of health with risk for multisystem inflammatory syndrome associated with COVID-19 (MIS-C), postoperative surgical outcomes and preterm birth among pregnant women living in areas of high social vulnerability.16–18 The Child Opportunity Index (COI) 2.019 quantifies the relative opportunity of neighborhood-based environment, education, socioeconomic conditions, and resources that would encourage healthy child development for nearly every census tract in the United States. The COI has been used to determine the association between the many aspects of neighborhood-level child opportunity and pediatric hospitalization rates for asthma. The COI has also been used to predict the use of urgent and emergency care services and hospitalization rates for common ambulatory conditions.20–22
The objective of this study was to identify census tract neighborhood “hot spots” using geospatial analysis where PICU admission rates (per 1000 children) are at or above the 90th percentile. We hypothesized that neighborhood hot spots would have poorer population-based indices of social determinants of health, evidenced by a higher composite measure of social vulnerability and a lower composite measure of child opportunity. We further hypothesized that neighborhood hot spots would have greater PICU readmission rates for an asthma exacerbation and longer total neighborhood-level total inpatient bed days.
METHODS
Study Setting and Design
Using the electronic health record (EHR), we identified children ages 6 through 17 years of age with asthma on their problem list who were admitted to the PICU at Children’s Healthcare of Atlanta’s Egleston campus (a 36-bed academic quaternary care PICU) and Scottish Rite campus (a 56-bed tertiary care community PICU) between January 1 2015 and May 31, 2020. Children throughout Georgia are referred to both hospitals for specialized care. The EHR was independently reviewed for each identified child and only children admitted for status asthmaticus were included in the study. Residential addresses for each child were extracted from the EHR. Children with more than one PICU admission for status asthmaticus were included only once in the analysis.
Ethics Statement
This study was approved by the Children’s Healthcare of Atlanta Institutional Review Board with a waiver of informed consent due to the retrospective observational study design prior to the request and retrieval of any EHR data.
Geocoding, Distance Measures, and Census Tract Data
Patient residential addresses were geocoded to census tracts using the R package tidygeocoder, and the U.S. Census 2018 GEOIDs for each census tract in Georgia were captured using the R package tigris.23, 24 The 2019 Topologically Integrated Geographic Encoding and Referencing/Line (TIGER/Line) shapefile for the primary and secondary roads in Georgia were obtained using the R package tigris.24 The Euclidian distance, or the shortest distance between a point (residence) and a line segment (roadway) as “the crow flies”, was measured in meters (m) using the R package sf.25 Distances were verified by mapping the geographical coordinates of the residential address and the TIGER/LINE road shapefile using the R package mapview.26
Socioeconomic data for each census tract was obtained using the R package tidycensus.27 The Social Vulnerability Index (SVI) data for 2018 were downloaded from the CDC website and joined to the patient data using the census tract GEOID.15 Social vulnerability refers to the potential negative effects on communities caused by external stresses on human health such as natural or human-caused disasters or disease outbreaks.28 The SVI uses fifteen U.S. census variables within four thematic domains: social and economic, household composition and disability, minority status and language, and housing type and transportation.28 The Child Opportunity Index 2.0 (COI 2.0) for 2015 was downloaded from the diversitydatakids.org website and joined to the patient data using the census tract GEOID.19, 29 The COI 2.0 measures neighborhood resources and conditions that impact a child’s healthy development, and the COI 2.0 allows the level of opportunity to be compared at the U.S. and state levels in a single metric.30 The COI 2.0 consists of twenty-nine indicators grouped into three domains: education, health and environment, and social and economic resources and opportunities. The state-based rankings for Georgia were used in the analysis.
Hot spot Identification
The PICU asthma admission rate (per 1000 children in the census tract) was calculated by summing the number of first PICU admissions for each unique child from a specified census tract and dividing by the number of children residing within that census tract as estimated by the 2015 - 2019 5-year American Community Survey (2019 ACS-5). Neighborhood hot spots were defined as those with PICU asthma admission rates in the 90th percentile or greater.
Outcome Measures
The primary patient-level outcome measure was PICU readmission for an asthma exacerbation. A secondary patient-level outcome measure was an individual hospital length of stay. Population-level secondary outcomes were the median aggregate inpatient bed days for children residing within a specific census tract and the total inpatient bed days per 1000 children in a census tract (inpatient bed day rate). The inpatient bed day rate was calculated by dividing the total number of days children from a specified census tract spent in the hospital by the number of children residing within that census tract estimated from the 2019 ACS-5.
Statistical analyses
Data were analyzed using R version 4.0.2.31 Wilcoxon rank sum test and chi-square tests were used for group differences. A p-value less than 0.05 was considered significant.
RESULTS
Study population
During the study period, there were 4,425 children admitted to the PICU with a diagnosis of asthma listed on their problem list. After individual review of each EHR, there were 1,705 admissions for status asthmaticus comprising 1,403 unique children with at least one PICU admission between January 1, 2015 and April 16, 2020 with matching SVI and COI census tract level data. There were 228 children (16.3%) living within a neighborhood hot spot. The patient-level demographic and clinical characteristics of the children, stratified by hot spot residence, are shown in Table 1. There was no difference in median age, sex, ethnicity, admission hospital, prior asthma diagnosis, or duration of hospitalization between children who lived inside versus outside a hot spot. However, children living in hot spots had a higher proportion of public/government-sponsored health insurance, were more likely to be admitted at the Egleston hospital campus, and lived in a home closer to a primary or secondary roadway compared to children living outside of a hot spot (Table 1).
Table 1.
Patient-Level Demographics and Clinical Characteristics of Children with Critical Asthma by Residence within a Hot Spot Neighborhood
| Characteristic | Patients Residing in a Hot Spota | |
|---|---|---|
| No n = 1175 (84%) |
Yes n = 228 (16%) |
|
|
| ||
| Age (years), median (Q1, Q3)) | 9.96 (7.63, 12.57) | 9.75 (7.77, 12.10) |
|
| ||
| Sex, n (%) | ||
| Female | 484 (41.2) | 90 (39.5) |
| Male | 691 (58.8) | 138 (60.5) |
|
| ||
| Race, n (%) | ||
| Black | 736 (62.6) | 195 (85.5) |
| White | 314 (26.7) | 22 (9.7) |
| Multiple | 25 (2.1) | 3 (1.3) |
| Asian | 34 (2.9) | 0 (0) |
| Other | 5 (0.4) | 1 (0.4) |
| Unknown | 61 (5.2) | 7 (3.1) |
|
| ||
| Ethnicity, n (%) | ||
| Non-Hispanic / Latino | 1032 (87.8) | 201 (88.2) |
| Hispanic / Latino | 139 (11.8) | 27 (11.8) |
| Declined / Unknown | 4 (0.34) | 0 (0) |
|
| ||
| Primary Language, n (%) | ||
| English | 1091 (92.9) | 209 (91.7) |
| Spanish | 78 (6.6) | 18 (7.9) |
| Other | 6 (0.5) | 1 (0.4) |
|
| ||
| Insuranced, n (%) | ||
| Public | 720 (61.3) | 186 (81.6)** |
| Private | 365 (31.1) | 26 (11.4) |
| Military | 16 (1.4) | 3 (1.3) |
| None / Self-pay | 74 (6.3) | 13 (5.7) |
|
| ||
| Hospital Location, n (%) | ||
| Egleston Campus | 415 (35.3) | 120 (52.6)** |
| Scottish Rite Campus | 760 (64.7) | 108 (47.4) |
|
| ||
| Prior History of Asthma, n (%) | 1112 (94.6) | 216 (94.7) |
|
| ||
| Medically Complex, n (%) | 35 (3.0) | 5 (2.2) |
|
| ||
| Heliox, n (%) | 358 (30.5) | 70 (30.7) |
|
| ||
| Intubated, n (%) | 66 (5.6) | 7 (3.1) |
|
| ||
| Isoflurane, n (%) | 15 (1.3) | 3 (1.3) |
|
| ||
| Extracorporeal Life Support, n (%) | 1 (0.09) | 1 (0.4) |
|
| ||
| Pulmonary Consultation, n (%) | 1164 (99.1) | 226 (99.1) |
|
| ||
| Distance to a major roadway (m), median (Q1, Q3) | 826 (377, 1542) | 506 (228, 1178)** |
Hotspot is a census tract ranked at or above the 90th percentile for the highest number of children admitted to intensive care with status asthmaticus per 1000 children living in the census tract
Inpatient Bed Day Rate is the sum of total days in the hospital for children living in a census tract per 1000 children living in the census tract
Hospital Admission Rate is the number of children admitted to intensive care for status asthmaticus living in a census tract per 1000 children living in the census tract; this is how hotspots were defined
p < 0.05,
p < 0.0001 Chi-squared test
Social Vulnerability Index is higher in children residing in neighborhood hot spots and with readmissions
The SVI consists of four thematic domains and fifteen indicators within those domains. The social vulnerability indicators for children stratified by neighborhood hot spot residential status are summarized in Table 2. All individual indicators were significantly different by neighborhood hot spot status along with the composite percentile ranking of three out of the four themes including socioeconomic status, household composition and disability, and housing type and transportation. Within the socioeconomic theme, the percentage of households below poverty and unemployment contributed the most to the disparity between the groups (Table 2). Support for high school graduation and improving the support for the quality of education seem to be societal targets to lessen the poverty gap. Within the housing and transportation theme, high-density housing and lack of access to a household vehicle contributed the most to disparity between the groups (Table 2). For these three themes, the percentile ranking of the composite SVI was higher, indicating more social vulnerability, for children living inside versus outside a neighborhood hot spot.
Table 2.
Population-Level Social Vulnerability Index for Children with Critical Asthma by Hot Spot Residence
| Characteristic | Patients Residing in a Hot Spota | |||
|---|---|---|---|---|
| No n = 1175 |
Yes n = 228 |
|||
| Median | Q1, Q3 | Median | Q1, Q3 | |
| Socioeconomic Status | ||||
| Below Poverty, % | 13.40 | 7.40, 20.35 | 22.10* | 15.50, 28.60 |
| Unemployment, % | 5.70 | 4.10, 8.70 | 8.80* | 5.20, 12.10 |
| Per Capita Income, $ | 26,796 | 21,177; 33,032 | 21,302* | 18,560; 26,621 |
| No High School Diploma (≥ 25 years), % | 10.70 | 6.50, 10.70 | 12.40* | 8.78, 17.20 |
|
| ||||
| Household Composition & Disability | ||||
| Age ≥ 65 years, % | 10.50 | 7.90, 13.50 | 11.00* | 7.90, 16.12 |
| Age ≤ 17 years, % | 26.60 | 23.70, 29.20 | 24.00* | 20.20, 28.20 |
| Disability, % | 10.10 | 7.30, 12.90 | 13.30* | 10.52, 17.08 |
| Single Parent Households, % | 11.30 | 7.50, 16.30 | 14.70* | 10.50, 17.00 |
|
| ||||
| Minority Status & Language | ||||
| Minority, % | 63.30 | 35.30, 85.60 | 91.60* | 82.35, 95.70 |
| Limited English, % | 1.70 | 0.60, 5.00 | 0.70* | 0.40, 3.00 |
|
| ||||
| Housing Type & Transportation | ||||
| Housing with ≥ 10 units, % | 4.80 | 0.00, 18.20 | 12.20* | 6.30, 31.90 |
| Mobile Homes, % | 0.90 | 0.00, 3.60 | 0.00* | 0.00, 1.40 |
| Housing units with more people than rooms, % | 1.80 | 0.60, 3.60 | 2.30* | 1.20, 3.10 |
| Households with no vehicle, % | 4.00 | 1.70, 8.00 | 10.00* | 5.50, 20.72 |
| Persons living in group quarters, % | 0.10 | 0.00, 0.30 | 0.10* | 0.00, 0.70 |
|
| ||||
| Overall Percentile Ranking Summary by Theme | ||||
| Theme 1: Socioeconomic Status | 0.41 | 0.23, 0.66 | 0.66* | 0.39, 0.85 |
| Theme 2: Household Composition & Disability | 0.44 | 0.25, 0.64 | 0.65* | 0.27, 0.85 |
| Theme 3: Minority Status & Language | 0.72 | 0.46, 0.89 | 0.74 | 0.53, 0.89 |
| Theme 4: Housing Type & Transportation | 0.43 | 0.19, 0.68 | 0.63* | 0.41, 0.79 |
| Overall Percentile Ranking (scale: 0 – 1) | 0.46 | 0.24, 0.73 | 0.67* | 0.49, 0.87 |
Hot spot = census tracts ranked at or above the 90th percentile for the highest number of children admitted to intensive care with status asthmaticus per 1000 children living in the census tract
Wilcoxon Rank sum test with continuity correction, p < 0.05
Child Opportunity Index is lower in children residing in neighborhood hot spots and with readmissions
The COI 2.0 consists of three thematic domains and twenty-nine indicators within those domains. The raw COI 2.0 indicators for children stratified by neighborhood hot spot residential status are summarized in Table 3. The standardized and scaled z-scores for the census tracts in Georgia are reported in Table E1. Some indicators are reversed such that a higher z-score always indicates more child opportunity. The composite individual domains and the overall COI 2.0 scores are ranked by percentile from 1 to 100. The mapped intensive care admissions were distributed throughout Georgia; however, the majority of children admitted to an intensive care unit resided in the 29 county Atlanta-Sandy Springs-Roswell metropolitan statistical area (ATL MSA) (Figure 1A). A map of the ATL MSA shows that intensive care admissions are clustered in tracts with lower COI 2.0 (Figure 1B).
Table 3.
Population-Level Childhood Opportunity Index Raw Score Indicators by Domain for Children with Critical Asthma by Hot Spot Residence
| Characteristic | Patients Residing in a Hot Spota | |||
|---|---|---|---|---|
| No n = 1175 |
Yes n = 228 |
|||
| Median | Q1, Q3 | Median | Q1, Q3 | |
| Education | ||||
| Early Childhood Education Centers, n | 3.95 | 3.22, 4.47 | 4.63* | 4.19, 4.99 |
| High Quality Early Childhood Education Centers, n | 0.63 | −0.56, 1.55 | 1.80* | 0.69, 2.62 |
| Early Childhood Education Enrollment, % | 52.40 | 34.95, 68.00 | 53.40 | 32.70,75.60 |
|
| ||||
| Third Grade Reading Proficiencyb | 192.51 | 137.14, 252.86 | 119.10* | 97.90, 167.98 |
| Third Grade Math Proficiencyb | 206.32 | 142.96, 267.10 | 125.60* | 94.23, 164.78 |
| High School Graduation Rate, % | 78.47 | 71.50, 85.15 | 75.25* | 68.29, 79.84 |
| Advanced Placement Course Enrollmentc, ratio | 0.53 | 0.41, 0.69 | 0.42* | 0.34, 0.53 |
| College Enrollment in Nearby Institutions, % | 39.64 | 37.29, 41.32 | 40.81* | 38.49, 44.72 |
|
| ||||
| School Poverty, % | 70.00 | 49.30, 87.09 | 93.47* | 80.21, 99.11 |
| Teacher Experience, % | 10.75 | 6.14, 17.54 | 18.03* | 11.06, 21.34 |
| Adult Educational Attainment, % | 27.72 | 19.57, 39.17 | 23.74* | 17.41, 31.61 |
|
| ||||
| Health and Environment | ||||
| Access to healthy food, % (reversed) | 3.18 | 1.28, 5.80 | 6.38* | 2.33, 20.97 |
| Access to green space, % (reversed) | 16.60 | 7.75, 24.00 | 25.30* | 17.10, 35.40 |
| Walkability, Indexd | 7.15 | 5.83, 8.73 | 10.22* | 6.93, 12.42 |
| Housing vacancy rate, % | 7.67 | 4.83, 11.69 | 14.58* | 9.40, 19.47 |
|
| ||||
| Hazardous waste dump sites, average n | −13.82 | −13.82, −13.82 | −13.82 | −13.82, −13.82 |
| Industrial pollutants in air, water, or soil, Index | 9.28 | 8.26, 9.62 | 9.63* | 9.47, 9.88 |
| Airborne microparticles, mean estimated PM2.5 | 11.18 | 10.90, 11.36 | 11.43* | 11.27, 11.55 |
| Ozone Concentrations, mean estimated 8h-average | 38.45 | 38.24, 38.84 | 38.14* | 37.97, 38.34 |
| Extreme Heat Exposure, summer days n | 58.33 | 53.00, 62.33 | 59.67* | 58.67, 61.00 |
|
| ||||
| Health Insurance Coverage, % | 83.61 | 77.69, 89.01 | 79.98* | 74.52, 84.03 |
|
| ||||
| Social and Economic | ||||
| Employment rate, % | 77.93 | 73.71, 81.51 | 74.30* | 69.15, 80.72 |
| Commute duration > 1h one-way, % | 33.90 | 25.70, 43.61 | 30.44* | 23.45, 37.46 |
|
| ||||
| Poverty rate, % | 14.09 | 8.29, 22.07 | 22.63* | 13.31, 28.97 |
| Public assistance rate, % | 13.62 | 7.36, 22.19 | 23.67 | 15.23, 30.47 |
| Homeownership rate, % | 68.82 | 46.77, 81.07 | 47.85* | 34.81, 64.79 |
| High-skill employment, % | 13.73 | 10.02, 17.57 | 12.23* | 9.37, 16.95 |
| Median household income, dollars | 57,204 | 43,097.5; 72663 | 41,375* | 31,078; 52,631.5 |
| Single-headed households, % | 37.65 | 24.22, 53.71 | 61.01* | 48.34, 74.26 |
|
| ||||
| Overall Percentile Ranking Summary by Domain e | ||||
| Domain 1: Education | 52 | 23, 75 | 18* | 10, 36 |
| Domain 2: Health and Environment | 49 | 26, 73 | 12* | 3, 44 |
| Domain 3: Social and Economic | 49 | 25.5, 73 | 21* | 9, 46.5 |
| Overall Percentile Ranking (scale: 1 - 100) | 48 | 24, 75 | 17* | 7, 43 |
Hotspot = census tracts ranked at or above the 90th percentile for the highest number of children admitted to intensive care with status asthmaticus per 1000 children living in the census tract
Converted to NAEP scale score points
Ratio of students enrolled in at least one AP course to the number of 11th and 12th graders
Walkability Index ranging from 1 (least walkable) to 20 (most walkable)
State normed values for Georgia were used
Wilcoxon Rank sum test with continuity correction, p < 0.05
Figure 1. Maps of Georgia (A) and the Atlanta-Sandy Springs-Roswell metropolitan statistical area (B) including the Overall Child Opportunity Index (COI) 2.0 Georgia-based rankings for each of the census tracts.
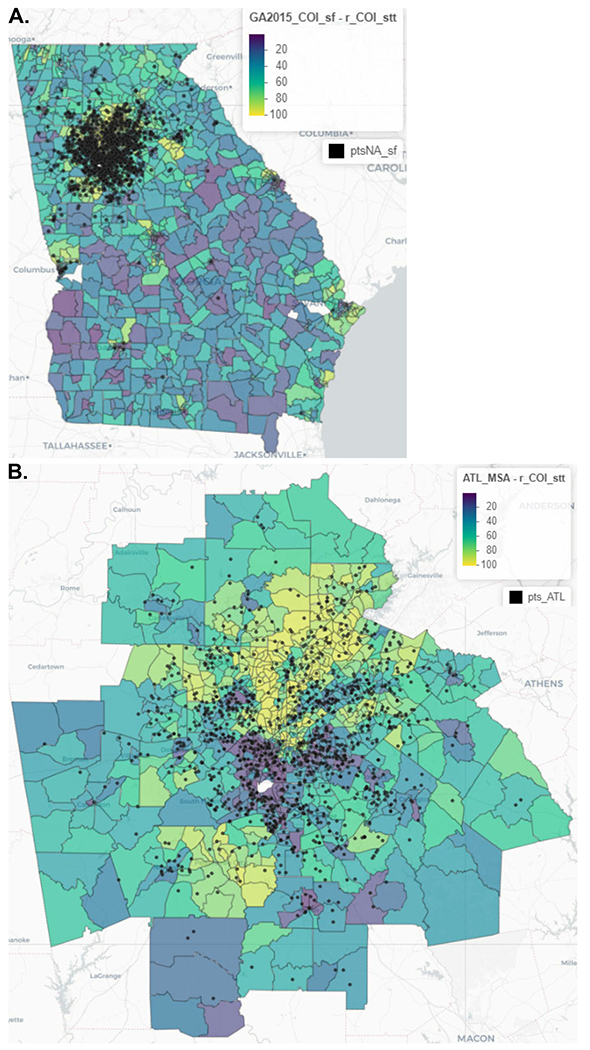
Admissions to a Children’s Healthcare of Atlanta pediatric intensive care unit for status asthmaticus occurring during the 2015 – 2020 study period are shown. Census tracts are percentile ranked relative to other Georgia census tracts using the COI 2.0 from 1 – 100. Yellow indicates a census tract with a low COI 2.0. Purple indicates a census tract with a high COI 2.0.
Outcomes
Of the 1,403 children included in the analysis, there were 185 (13.2%) children with PICU readmission for status asthmaticus during the study period (range: two to twenty-one PICU admissions). PICU readmission rates were not different by hot spot (Table 4). However, children with multiple PICU admissions were more likely to have higher social vulnerability in all four individual thematic domains and the composite index (Figure 2). Additionally, children with multiple PICU admissions were more likely to have less childhood opportunity in all three individual thematic domains and the composite index (Figure 3).
Table 4.
Patient-Level and Population-Level Outcomes by Hot Spot Status
| Characteristic | Patients Residing in a Hot Spota | |
|---|---|---|
| No n = 1175 (84%) |
Yes n = 228 (16%) |
|
| Patient-Level | ||
| Died, n (%) | 19 (1.6) | 2 (0.9) |
| Hospital Length of Stay (days), median (Q1, Q3) | 3.5 (2.6, 4.7) | 3.0 (2.3, 4.6)* |
| Multiple Admissions, n (%) | 154 (13.1) | 31 (13.6) |
| Number of Admissions, median (Q1, Q3) | 1 (1, 1) | 1 (1, 1) |
|
| ||
| Population-Level | ||
| Inpatient Bed Days | 8.8 (5.3, 15.8) | 14.8 (8.2, 22.6)** |
| Inpatient Bed Days Rateb | 5.0 (3.1, 7.5) | 13.0 (9.6, 21.0)** |
| Hospital Admission Ratec | 1.3 (0.9, 1.8) | 3.6 (3.0, 4.7)** |
Hotspot is a census tract ranked at or above the 90th percentile for the highest number of children admitted to intensive care with status asthmaticus per 1000 children living in the census tract
Inpatient Bed Day Rate is the sum of total days in the hospital for children living in a census tract per 1000 children living in the census tract
Hospital Admission Rate is the number of children admitted to intensive care for status asthmaticus living in a census tract per 1000 children living in the census tract; this is how hotspots were defined
p < 0.05,
p < 0.0001 Wilcoxon Rank sum test or Chi-squared test
Figure 2. Social Vulnerability Index census tract ranking for Georgia for children with and without two or more pediatric intensive care admissions for status asthmaticus.
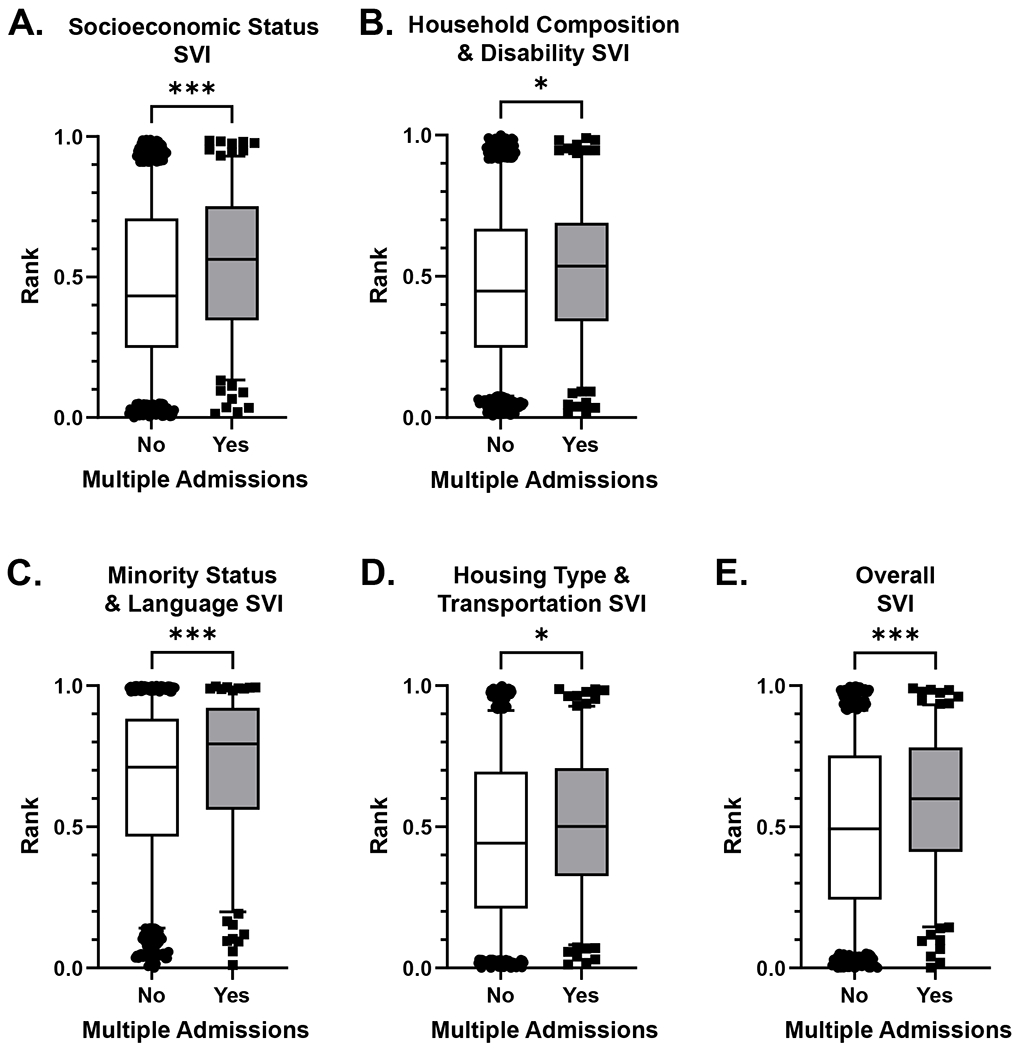
Box and whisker plots of A) socioeconomic status, B) household composition and disability, C) minority status and language, D) housing type and transportation, E) overall composite percentile ranking. Center line is the median, outer box is the 25th and 75th percentile, whiskers are the 95% confidence intervals. There were n = 185 children with multiple admissions and n = 1219 children with one admission. *p < 0.05, ***p < 0.001
Figure 3. Childhood Opportunity Index 2.0 census tract ranking for Georgia for children with and without two or more pediatric intensive care admissions for status asthmaticus.
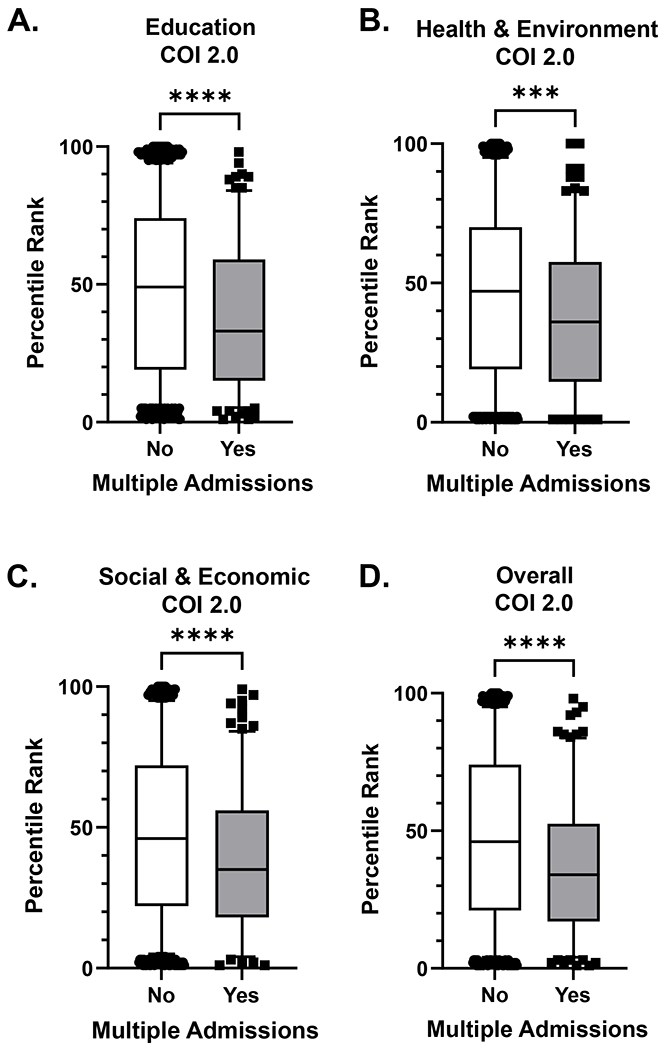
Box and whisker plots of A) Education domain, B) Health and Environment domain, C) Social and Economic domain, D) Overall Composite Index. There were n = 185 children with multiple admissions and n = 1219 children with one admission. Center line is the median, outer box is the 25th and 75th percentile, whiskers are the 95% confidence intervals. ***p < 0.001, ****p < 0.0001
Other outcomes, stratified by neighborhood hotspot residence, are shown in Table 4. PICU length of stay for individual participants was not higher in neighborhood hot spots. However, the total number of inpatient bed days by census tract and the inpatient bed day rate (total inpatient bed days per 1000 children in the census tract) were higher for neighborhood hot spots (Table 4). Deaths were rare, occurring in less than 2% of the cohort, and there were no differences in the proportion of deaths whether a child lived inside or outside a neighborhood hot spot.
DISCUSSION
This study evaluated composite social determinants of PICU admission for critical and near-fatal asthma in school-age children in metropolitan Atlanta through geospatial analyses. Children residing within a neighborhood hot spot, defined as those census tracts with a PICU asthma admission rate ≥ 90th percentile, had greater social vulnerability and less child opportunity that were further associated with future PICU readmission and aggregate inpatient length of stay. The disparities between hot spot neighborhoods and non-hot spot neighborhoods were pronounced. For example, the median SVI for a typical child living outside a hot spot neighborhood was 0.46, while the median SVI for a child living within a hot spot neighborhood was 0.67. Likewise, the COI 2.0 score for a typical child living within the metropolitan Atlanta region is 48, and by national rankings, is considered a moderate-opportunity area.32 However, the median COI 2.0 score for a child residing in a neighborhood hot spot in the present study was in the lowest quintile, with a score of 17. These findings add to the literature on social determinants of health and hospital admission for asthma and advance that prior work by focusing exclusively on a population with critical and near-fatal asthma, which has not been well studied.
Inequities in health care are well-established and long-standing.33, 34 Adverse childhood events, disruptive neighborhood living conditions, and unhealthy environmental factors, such as close proximity to a high-traffic major roadway, all contribute to chronic childhood asthma. Black and Hispanic children are also more likely to be hospitalized with life-threatening asthma compared with non-Hispanic white children;11 however, social deprivation and lower socioeconomic status alone do not explain all of the risk associated with higher illness burden, severity of illness, and worse outcomes.34–37 The SVI was recently used to determine factors beyond education and income that contribute to disparities in Massachusetts children diagnosed with MIS-C.18 Furthermore, the protective effects of socioeconomic status on health are not experienced equally across racial and ethnic groups.34, 35 As shown by Javaljar and colleagues, increased risk of MIS-C in children from racial and/or ethnic minorities extended beyond their socioeconomic and education status, as indicated by the SVI which also includes measures of housing composition, transportation and primary spoken language.18 As a result, attention to the social determinants of health and structural racism that contribute to critical illness in children is being intensified.33, 38 For example, Andrist and colleagues showed that there were an unequal proportion of neighborhood PICU admission rates and inpatient bed day rates in neighborhoods with higher child poverty rates in Cincinnati and the area surrounding Hamilton County, Ohio.33
The effect of race and ethnicity on health disparities and multiple interrelated complex factors, including access to care, provider bias, effects of racial discrimination, and resulting chronic stress, was recently demonstrated by Beck and colleagues who used the COI to associate neighborhood disparities with population-level and patient-level asthma morbidity across the Cincinnati metropolitan area encompassed by Hamilton County, Ohio.20 Similar findings associating low child opportunity index rankings with higher acute care use in San Francisco, California and higher pediatric hospitalizations in Kansas City, MS and Cincinnati, OH have been reported.21, 22 Geospatial hot spot identification may inform a neighborhood-level understanding of health disparities to encourage a public health and systems approach to reduce inequities and foster community-healthcare system partnerships to trial interventions aimed at a reduction in the use of critical care resources and improve health.
Pediatric critical care services are at the bottom of the cliff in a sequence of societal and healthcare failures that include social determinants of health, equity, and access of preventive and non-emergency health care.39–41 Our study shows that these societal failures lead to a disproportionate use of pediatric critical care resources for life-threatening asthma by black children living in poverty in Atlanta and throughout Georgia; however, low-income status does not fully explain the health disparities experienced by black children in Georgia and the Atlanta metropolitan region. Our study also highlights neighborhood-level environmental characteristics, such as higher exposure to industrial pollutants in air, water and soil, higher levels of airborne microparticles (PM2.5), and higher ozone concentrations that contribute to life-threatening asthma exacerbations in Atlanta’s children. The homes of children living in hot spots were on average 1.6 times and within a median distance of 500 meters to a major roadway compared with children with critical asthma who lived outside of a neighborhood hot spot. The two neighborhoods with the highest rates of PICU admissions for asthma were next to a military base airfield and Hartsfield-Jackson International Airport, one of the busiest passenger airports in the world.
Previous studies have shown that proximity to a major roadway contributes to increased airway and systemic inflammation, higher markers of airway tissue remodeling and poor asthma control.42 The results of this study consistent with prior findings that residential proximity to a major roadway is associated with asthma severity in children. Residents living in the proximity to a commercial airport are also at increased risk of hospitalization for respiratory conditions.43 Environmental modeling studies of ozone, particulate matter, and air pollutants from traffic sources are associated with pediatric emergency department visits in Atlanta, Georgia.44 In a study conducted by the Environmental Health Bureau of the Massachusetts Department of Public Health, children living in neighborhoods bordering Logan International Airport in Boston, Massachusetts were four times more likely to experience asthma symptoms and to be hospitalized for asthma compared with children living farther away from the airport.45,46 The respiratory symptoms are attributed to higher levels of nitrogen oxides and particulate matter with a diameter of less than 2.5 micrometer in areas near the airport.
Incorporating social determinants of health screening into clinical practice would seemingly uncover adverse conditions that require more resources and multi-disciplinary care coordination that cannot be adequately addressed during routine clinical care. How does a clinician tackle larger issues of affordable housing, public transportation, employment training and access to quality education within the limits of their medical setting? First, despite adverse social determinants, strengths and assets of patients and families should be identified and a practical approach that refers and links families to community-based nonmedical services should be taken. Second, input from families about their desire for assistance should be sought. Third, screening should be universal and not limited to those profiled to face adverse social determinants to prevent stigmatization and stereotyping. To improve access and quality of medical services, clinicians need to foster a community-based network approach and partner with community services to meet the needs of their patients and families. For example, are there school-based health programs or mobile health programs that can take the clinic to the patient? Are there subsidized medical appointment transportation programs to aid families to make it to clinic appointments. Can medication be delivered or mailed to the patient’s residence? Can an on-site pharmacy dispense the medication at the clinic appointment? Do medical-legal aid partnerships exist to address housing and environmental exposures and hazards? Clinicians must become advocates for their patients and families and work within a larger community scope involving collaboration with community partners to improve and promote the health of patients and families.
Although the geospatial analyses applied in the present study are unique, this study does have limitations. The Children’s Healthcare of Atlanta system has two large pediatric intensive care units that serve a racially and ethnically diverse pediatric population throughout Georgia; however, the majority of children studied lived within the 29 county Atlanta metropolitan statistical area. Traffic density was also not measured directly. Instead, we used the U.S. Department of Transportation definition of a primary or secondary roadway as a proxy of high traffic volume. Because children in this study were also obtained through a query of electronic health records, the stability of the residence is not available for children admitted only once during the study period. We also used neighborhood-level socioeconomic factors defined by census tracts from the U.S Census American Community Survey to standardize measures for our study rather using individual level measures such as family income and education level as these data are not available from the electronic health record. Boundaries defined by census tracts may not accurately represent geographical and neighborhood communities; however, this is the more practical way to link geographical information with socioeconomic data for the U.S. Census. Finally, there were also higher-poverty census tracts with lower rates of asthma admissions identified. An exploration of protective factors in these areas could help motivate intervention efforts.47–49 Likewise, lower-poverty census tracts with higher rates of critical asthma were also identified. Future studies are needed to determine whether weather patterns, thunderstorms, high temperatures, and air pollutants such as nitrogen oxides, ozone and fine particulates contribute to pediatric critical asthma admissions in these areas.
In conclusion, children who live in hot spot neighborhoods, on average, live in areas with a high social vulnerability index and low childhood opportunity index. They live in homes closer to major roadways that could result in environmental triggers of critical asthma. Attention to these geospatial social determinants of health may provide further understanding of how physical and social environments contribute to critical asthma in children. Ultimately, comprehensive assessment and mitigation of these social determinants in outpatient settings may help improve health equity and the need for PICU admission in children with acute exacerbations of asthma.
Supplementary Material
Highlights Box.
What is already known about this topic? (word count = 35)
Social determinants of health are associated with asthma prevalence and hospitalization in children, but are multifactorial and complex. Social determinants of pediatric intensive care unit (PICU) admission and readmission for asthma are not well described.
What does this article add to our knowledge? (word count = 28)
Neighborhood “hot spots” with high social vulnerability and low childhood opportunity identified through geospatial analyses are associated with PICU admissions for critical and near-fatal asthma and longer hospital stays in school-age children.
How does this study impact current management guidelines? (word count = 31)
Comprehensive assessment and mitigation of social determinants of health, in addition to biological factors, may improve health equity and the need for PICU admission in children with acute exacerbations of asthma.
This study was supported in part by:
K24 NR018866 awarded to AF; K23HL151897-01 and an Emory University Pediatrics Research Alliance Junior Faculty Focused Pilot award awarded to JG.
ABBREVIATIONS
- COI
Childhood Opportunity Index
- EHR
Electronic health record
- PICU
Pediatric intensive care unit
- SVI
Social Vulnerability Index
- TIGER
Topologically Integrated Geographic Encoding and Referencing
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Author Disclosures: The authors have nothing to disclose.
REFERENCES
- 1.Hastie AT, Moore WC, Meyers DA, Vestal PL, Li H, Peters SP, et al. Analyses of asthma severity phenotypes and inflammatory proteins in subjects stratified by sputum granulocytes. J Allergy Clin Immunol 2010; 125:1028–36 e13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Slejko JF, Ghushchyan VH, Sucher B, Globe DR, Lin SL, Globe G, et al. Asthma control in the United States, 2008-2010: indicators of poor asthma control. J Allergy Clin Immunol 2014; 133:1579–87. [DOI] [PubMed] [Google Scholar]
- 3.Federico MJ, McFarlane AE 2nd, Szefler SJ, Abrams EM. The Impact of Social Determinants of Health on Children with Asthma. J Allergy Clin Immunol Pract 2020; 8:1808–14. [DOI] [PubMed] [Google Scholar]
- 4.Parikh K, Berry J, Hall M, Mussman GM, Montalbano A, Thomson J, et al. Racial and Ethnic Differences in Pediatric Readmissions for Common Chronic Conditions. J Pediatr 2017; 186:158–64 e1. [DOI] [PubMed] [Google Scholar]
- 5.Beck AF, Huang B, Ryan PH, Sandel MT, Chen C, Kahn RS. Areas with High Rates of Police-Reported Violent Crime Have Higher Rates of Childhood Asthma Morbidity. J Pediatr 2016; 173:175–82 e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Beck AF, Huang B, Simmons JM, Moncrief T, Sauers HS, Chen C, et al. Role of financial and social hardships in asthma racial disparities. Pediatrics 2014; 133:431–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Beck AF, Sandel MT, Ryan PH, Kahn RS. Mapping Neighborhood Health Geomarkers To Clinical Care Decisions To Promote Equity In Child Health. Health Aff (Millwood) 2017; 36:999–1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Eldeirawi K, Kunzweiler C, Rosenberg N, Zenk S, Tarlov E, Hebert-Beirne J, et al. Proximity to traffic and asthma among Mexican American children: Independent and interactive effects. J Allergy Clin Immunol 2018; 141:2306–8 e1. [DOI] [PubMed] [Google Scholar]
- 9.Keet CA, Matsui EC, McCormack MC, Peng RD. Urban residence, neighborhood poverty, race/ethnicity, and asthma morbidity among children on Medicaid. J Allergy Clin Immunol 2017; 140:822–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sullivan K, Thakur N. Structural and Social Determinants of Health in Asthma in Developed Economies: a Scoping Review of Literature Published Between 2014 and 2019. Curr Allergy Asthma Rep 2020; 20:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Beck AF, Huang B, Auger KA, Ryan PH, Chen C, Kahn RS. Explaining Racial Disparities in Child Asthma Readmission Using a Causal Inference Approach. JAMA Pediatr 2016; 170:695–703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fitzpatrick AM, Gillespie SE, Mauger DT, Phillips BR, Bleecker ER, Israel E, et al. Racial disparities in asthma-related health care use in the National Heart, Lung, and Blood Institute’s Severe Asthma Research Program. J Allergy Clin Immunol 2019; 143:2052–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Grunwell JR, Travers C, Fitzpatrick AM. Inflammatory and Comorbid Features of Children Admitted to a PICU for Status Asthmaticus. Pediatr Crit Care Med 2018; 19:e585–e94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lee DS, Gross E, Hotz A, Rastogi D. Comparison of severity of asthma hospitalization between African American and Hispanic children in the Bronx. J Asthma 2020; 57:736–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Social Vulnerability Index Data Documentation. 2021.] Available from https://www.atsdr.cdc.gov/placeandhealth/svi/data_documentation_download.html.
- 16.Givens M, Teal EN, Patel V, Manuck TA. Preterm birth among pregnant women living in areas with high social vulnerability. Am J Obstet Gynecol MFM 2021; 3:100414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Paro A, Hyer JM, Diaz A, Tsilimigras DI, Pawlik TM. Profiles in social vulnerability: The association of social determinants of health with postoperative surgical outcomes. Surgery 2021. [DOI] [PubMed] [Google Scholar]
- 18.Javalkar K, Robson VK, Gaffney L, Bohling AM, Arya P, Servattalab S, et al. Socioeconomic and Racial and/or Ethnic Disparities in Multisystem Inflammatory Syndrome. Pediatrics 2021; 147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Childhood Opportunity Index 2.0 Database. 2021.] Available from https://data.diversitydatakids.org/dataset/coi20-child-opportunity-index-2-0-database.
- 20.Beck AF, Huang B, Wheeler K, Lawson NR, Kahn RS, Riley CL. The Child Opportunity Index and Disparities in Pediatric Asthma Hospitalizations Across One Ohio Metropolitan Area, 2011-2013. J Pediatr 2017; 190:200–6 e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kersten EE, Adler NE, Gottlieb L, Jutte DP, Robinson S, Roundfield K, et al. Neighborhood Child Opportunity and Individual-Level Pediatric Acute Care Use and Diagnoses. Pediatrics 2018; 141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Krager MK, Puls HT, Bettenhausen JL, Hall M, Thurm C, Plencner LM, et al. The Child Opportunity Index 2.0 and Hospitalizations for Ambulatory Care Sensitive Conditions. Pediatrics 2021; 148. [DOI] [PubMed] [Google Scholar]
- 23.Cambon J tidygeocoder: Geocoding Made Easy. , 2020. [Google Scholar]
- 24.Walker K tigris: Load Census TIGER/Line Shapefiles. 2020. [Google Scholar]
- 25.Pebesma E Simple Features for R: Standardized Support for Spatial Vector Data. The R Journal, 2018:439–46. [Google Scholar]
- 26.Applehans T, Detsch F, Reudenbach C, Woellauer S. mapview: Interactive Viewing of Spatial Data in R. 2020. [Google Scholar]
- 27.Walker K, Herman M. tidycensus: Load US Census Boundary and Attribute Data as ‘tidyverse’ and ‘sf’-Ready Data Frames. 2020. [Google Scholar]
- 28.Social Vulnerability Index. 2021.] Available from https://www.atsdr.cdc.gov/placeandhealth/svi/index.html.
- 29.Noelke C, McArdle N, Baek M, Huntington N, Huber R, Hardy E, et al. Child Opportunity Index 2.0 Technical Documentation. Retrieved from diversitydatakids.org/research-library/research-brief/how-we-built-it., 2020. [DOI] [PubMed]
- 30.Childhood Opportunity Index 2.0. 2021.] Available from https://data.diversitydatakids.org/dataset/coi20-child-opportunity-index-2-0-database.
- 31.Team RC. R: A language and environment for statistical computing. R Foundation for Statistical Computing. 2013. [Google Scholar]
- 32.Data Visualization Childhood Opportunity Index by Metropolitan Statistical Area. 2021.] Available from https://www.diversitydatakids.org/research-library/data-visualization/snapshot-child-opportunity-across-us.
- 33.Andrist E, Riley Cl, Brokamp C, Taylor S, Beck AF. Neighborhood Poverty and Pediatric Intensive Care Use. Pediatrics 2019; 144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Assari S, Moghani Lankarani M. Poverty Status and Childhood Asthma in White and Black Families: National Survey of Children’s Health. Healthcare (Basel) 2018; 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Braveman P, Gottlieb L. The social determinants of health: it’s time to consider the causes of the causes. Public Health Rep 2014; 129 Suppl 2:19–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Merrick MT, Ford DC, Ports KA, Guinn AS, Chen J, Klevens J, et al. Vital Signs: Estimated Proportion of Adult Health Problems Attributable to Adverse Childhood Experiences and Implications for Prevention - 25 States, 2015-2017. MMWR Morb Mortal Wkly Rep 2019; 68:999–1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yan Q, Forno E, Cardenas A, Qi C, Han YY, Acosta-Perez E, et al. Exposure to violence, chronic stress, nasal DNA methylation, and atopic asthma in children. medRxiv 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pomerantz WJ, Dowd MD, Buncher CR. Relationship between socioeconomic factors and severe childhood injuries. J Urban Health 2001; 78:141–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Anand KJ, Sepanski RJ, Giles K, Shah SH, Juarez PD. Pediatric intensive care unit mortality among Latino children before and after a multilevel health care delivery intervention. JAMA Pediatr 2015; 169:383–90. [DOI] [PubMed] [Google Scholar]
- 40.Colvin JD, Zaniletti I, Fieldston ES, Gottlieb LM, Raphael JL, Hall M, et al. Socioeconomic status and in-hospital pediatric mortality. Pediatrics 2013; 131:e182–90. [DOI] [PubMed] [Google Scholar]
- 41.Fieldston ES, Zaniletti I, Hall M, Colvin JD, Gottlieb L, Macy ML, et al. Community household income and resource utilization for common inpatient pediatric conditions. Pediatrics 2013; 132:e1592–601. [DOI] [PubMed] [Google Scholar]
- 42.Brown MS, Sarnat SE, DeMuth KA, Brown LA, Whitlock DR, Brown SW, et al. Residential proximity to a major roadway is associated with features of asthma control in children. PLoS One 2012; 7:e37044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lin S, Munsie JP, Herdt-Losavio M, Hwang SA, Civerolo K, McGarry K, et al. Residential proximity to large airports and potential health impacts in New York State. Int Arch Occup Environ Health 2008; 81:797–804. [DOI] [PubMed] [Google Scholar]
- 44.Strickland MJ, Darrow LA, Klein M, Flanders WD, Sarnat JA, Waller LA, et al. Short-term associations between ambient air pollutants and pediatric asthma emergency department visits. Am J Respir Crit Care Med 2010; 182:307–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Health MDoPHBoE. Logan Airport Health Study. 2014.
- 46.Hudda N, Simon MC, Zamore W, Durant JL. Aviation-Related Impacts on Ultrafine Particle Number Concentrations Outside and Inside Residences near an Airport. Environ Sci Technol 2018; 52:1765–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chen E, Chim LS, Strunk RC, Miller GE. The role of the social environment in children and adolescents with asthma. Am J Respir Crit Care Med 2007; 176:644–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chen E, Hayen R, Le V, Austin MK, Shalowitz MU, Story RE, et al. Neighborhood Social Conditions, Family Relationships, and Childhood Asthma. Pediatrics 2019; 144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Chen E, Miller GE, Shalowitz MU, Story RE, Levine CS, Hayen R, et al. Difficult Family Relationships, Residential Greenspace, and Childhood Asthma. Pediatrics 2017; 139. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


