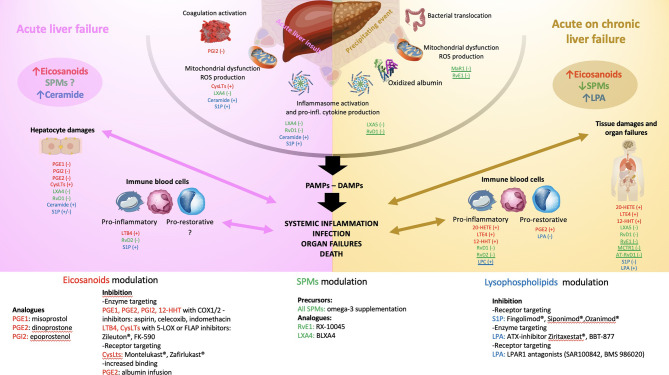
Figure 2.
Schematic illustration of the pathophysiology of acute liver failure (ALF- left panel) and acute on chronic liver failure (ACLF - right panel). The main endogenous bioactive lipids are identified with colours: eicosanoids in red, specialized pro-resolving lipid mediators (SPMs) in green, lysophospholipids in blue. Reported effects of the underlined mediators illustrate only investigation in sepsis models. Left panel: ALF starts with an acute liver insult (viral, toxic, ischemia, traumatism) occurring on a healthy liver leading to the release of danger-associated molecular patterns (DAMPS), inflammasome activation and secretion of pro-inflammatory cytokines and chemokines, coagulation activation and mitochondrial dysfunction leading to the release of reactive oxygen species (ROS). In ALF, a global increase in eicosanoids mediators and ceramide has been reported while the global trend of SPMs level is not known. The consequences are mainly those of perpetuating hepatocytes damages (cell death by necrosis, apoptosis, defect in liver regeneration aggravated by resident macrophages activation) and activation of circulating immune compartment through a pro-inflammatory phenotype (bacterial killing with phagocytosis, secretion of pro-inflammatory signals favouring leukocytes recruitment and tissue infiltration). A switch to a pro-restorative phenotype (decreased bacterial killing capacity and phagocytosis, increased efferocytosis function) occurs during the disease course exposing leading to systemic immunosuppression. All together these mechanisms lead to severe systemic inflammation and when uncontrolled infection, multi-organ failures and death. The effect investigated in experimental and translational studies of each lipid mediator is reported. (+) or (-) corresponds to its action on the pathophysiologic step (e.g., PGE1 decreases the hepatocytes damages in experimental models of ALF). Right panel: ACLF starts with a precipitating event (e.g., alcoholic hepatitis, infection, drug-induced liver injury, hepatitis B reactivation, gastrointestinal bleeding), occurring on a chronically affected liver. This leads to an increase in bacterial translocation, mitochondrial dysfunction with the generation of ROS and pro-inflammatory oxidized form of albumin, inflammasome activation and secretion of pro-inflammatory cytokines and chemokines. In ACLF, a global increase in eicosanoids mediators and LPA and a decrease in SPMs and LPC levels has been reported. The consequences are mainly a release of pathogen-associated molecular patterns (PAMPs) and DAMPs leading to intense systemic inflammation. The circulating immune compartment can be either pro-inflammatory or pro-restorative favouring infection, organ failures and death. As for the left panel, the effect investigated in experimental and translational studies of each lipid mediator is reported. (+) or (-) corresponds to its action on the pathophysiologic step (e.g., PGE2 favours the pro-restorative phenotype of the immune cell compartment). The bottom of the figure reports the different molecules that were clinically shown to modulate the action of the lipid mediator reported in the left and right panels. ATX, autotaxin, C1P, ceramide-1-phosphate; COX, cyclooxygenase; CysLTs, cysteinyl leukotrienes; DAMPs, danger-associated molecular patterns; FLAP, 5-LOX activating protein; LTB4, leukotriene B4; LOX, lipoxygenase; LPA, lysophosphatidic acid; LPAR, lysophosphatidic acid receptor; LPC, lysophosphatidylcholine; LX, lipoxin; MaR, maresin; MCTR1, maresin conjugates in tissue regeneration 1; PAMPs, pathogen-associated molecular patterns; PG, prostaglandin; RvD, D-series resolvin; RvE, E-series resolvin; S1P, Sphingosine-1-phosphate; S1PR, Sphingosine-1-phosphate receptor; SPMs, specialized pro-resolving mediator.