Fig. 4.
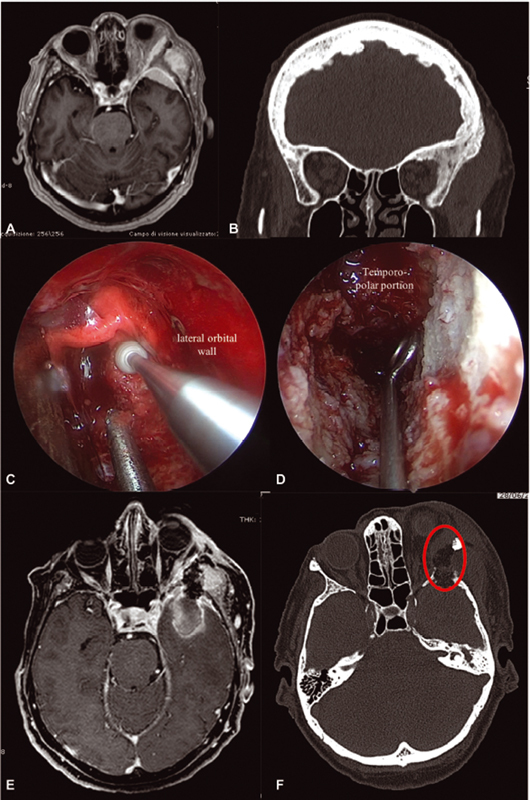
Exemplificative case of a left spheno-orbital meningioma (SOM) treated through an endoscopic superior eyelid approach (SEA). This 75 year–old-woman presented complaining of recent visual acuity reduction, left sixth cranial nerve deficit, diplopia, proptosis, and temporal region tumefaction. Magnetic resonance imaging (MRI) and computed tomography (CT) disclosed a left SOM characterized by extensive pterional, lateral orbital, and bifrontal bone invasion, with meningiomatosis spread to the middle cranial fossa (MCF), temporal and infratemporal fossa, and lateral orbital compartment ( A,B ). Anamnesis revealed triple cardiac stenting, obstructive chronic bronchitis, renal insufficiency, and severe smoking history. When proposed, the patient accepted to undergo an endoscopic SEA aimed at subtotal resection, controlling her visual symptoms. Surgery was then performed, removing the intraorbital part of the lesion along with the lateral orbital wall ( red circle in F ); a small opening in the temporopolar dura permitted to partially resect the meningioma in MCF ( C,D ). Postoperative imaging demonstrated an acceptable lateral orbital decompression, with subtotal resection of the temporopolar portion of the meningioma. The portion of the lesion in the temporal/infratemporal fossa was left untouched ( E,F ). The patient went home on fifth postoperative day, without any new neurological deficit. Progressive improvement of both cranial nerve deficit and visual acuity at 6 months was noticed. Her Karnofsky Performance Status improved from a preoperative value of 80 to 90 at 1 year, mainly due to improvement in visual acuity.
