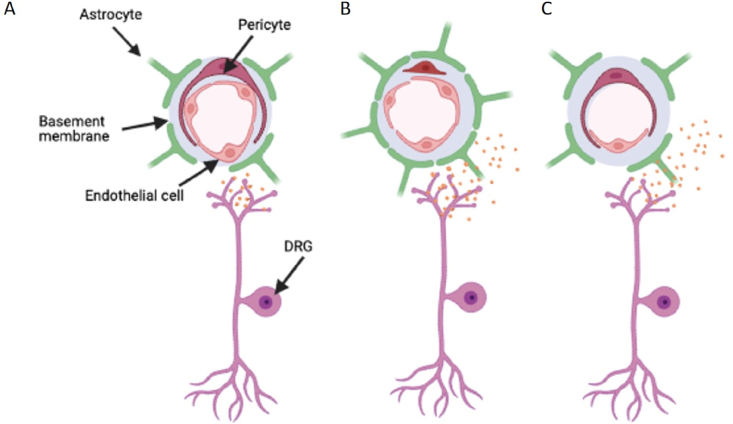
Fig. 2.
Disturbances in the blood spinal cord barrier
The blood spinal cord barrier (BSCB) plays an essential role in monitoring the spinal cord microenvironment. [A] The capillary network consists of the endothelial cells that form the lining of the vessel lumen, controlling passage of varying solutes and cells through into the spinal cord via stringent filtering processes that line the endothelium (Glycocalyx and tight junctional proteins). Additionally, these capillaries interact with surrounding mural cells, pericytes and astrocytes, to further regulate the BSCB integrity and function. [B] Enhanced vascular permeability is strongly associated with increases in the inflammatory profile of the spinal cord during chronic pain ie inflammatory pain and traumatic sensory nerve lesion. This is typified by the opening of interendothelial cell junctions due to diminished tight junction expression. Furthermore, astrogliosis, activation of dorsal horn astrocytes, accompanies an enhanced interaction with the endothelium. Upregulation of astrocytic foot processes depicted by elevated GFAP expression influence BSCB permeability through diminished expression of tight junctional proteins and elevated infiltration of cells and solutes. Similarly, damage to the peripheral C fibre nociceptors ie through traumatic nerve injury induces enhanced BSCB permeability through increased release of neurogenic inflammatory mediators. [C] Conversely, the endothelium degenerates, presented as a reduction in endothelium and the number of blood vessels. This is associated with reduced tissue perfusion of the spinal cord. This is associated with cytotoxicity of neuropathological conditions such as hyperglycaemia, driving endothelial cell death.