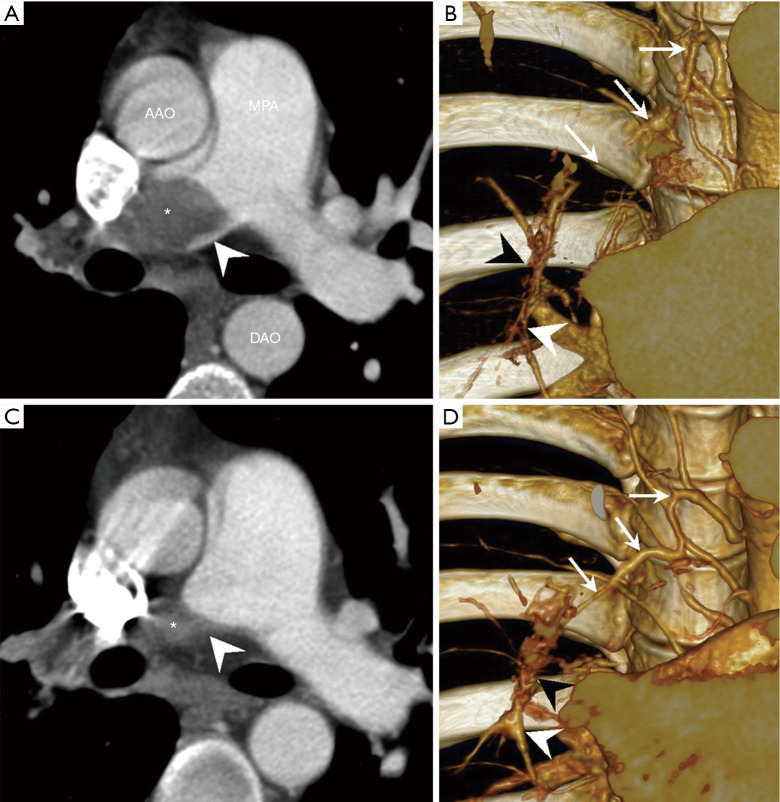
Figure 4.
Appearance of bronchial artery hypertrophy and bronchopulmonary shunts 16 months after an acute pulmonary embolism associated with the development of CTEPD [Reprinted from Imaging as a biomarker in Behçet disease: prognostic and therapeutic implications of serial pulmonary CT angiography, Tsai HY, Chin CS, Tsai IC, The American Journal of Roentgenology 2011 Jan;196:W105-6. doi: 10.2214/AJR.10.5147 (7), Copyright© 2011]. Acute PE (A,B), evolution towards CTEPH 16 months later (C,D). (A) CTPA showing a complete obstruction of the right central pulmonary artery due to acute pulmonary embolism (asterisk). Concave filling defect at the level of obstruction (arrowhead) is characteristic of acute pulmonary embolism. (B) At the same time, slab volume-rendering image showing normal size of the bronchial artery (arrows). Right distal lobar pulmonary artery (white arrowhead) distally from proximal acute pulmonary embolism is small in caliber. No obvious connection between the right bronchial artery and distal pulmonary arteries. (C) Follow-up CTPA performed 16 months later showing typical aspect of CTEPD with convex pouching aspect (asterisk and arrowhead). (D) At the same time, slab volume-rendering image showing hypertrophy of the right bronchial artery (arrows) which connects with the vasa vasora (black arrowhead) to supply the distal pulmonary artery (white arrowhead). Note anastomoses between the bronchial artery, vasa vasora, and the right pulmonary artery are now larger. CTEPH, chronic thromboembolic pulmonary hypertension; CTEPD, chronic thromboembolic pulmonary disease; CTPA, computed tomography pulmonary angiography; AAO, ascending aorta; MPA, main pulmonary artery; DAO, descending aorta.