Abstract
Background
The COVID-19 outbreak has generated many negative psychological outcomes, such as depression, in adolescents. Exploration of protective factors for adolescent mental health is urgently needed, and no research has examined the role of parental involvement.
Methods
From March to April 2020, valid data were collected from 1663 Chinese adolescents through online demographic and other questionnaires. Parental involvement at home was assessed by an adapted questionnaire on parental support in learning at home, stress since the COVID-19 outbreak was measured by the Perceived Stress Scale, and three negative psychological outcomes (i.e., depression, anxiety, and posttraumatic stress symptoms (PTSS)) were measured by the Center for Epidemiologic Studies Depression Scale, Zung Self-rating Anxiety Scale, and PTSD Check List-Civilian Version, respectively.
Results
In total, 35.4%, 21% and 25% of adolescents had depression symptoms, anxiety symptoms, and PTSS, respectively. Three moderated mediation models consistently showed the following: a. Parental involvement indirectly reduced the three psychological problems by alleviating perceived stress, and the indirect effects were not moderated by sex. b. There were negative direct effects of parental involvement on the three psychological problems, and the links were not moderated by sex. c. Sex moderated the associations between perceived stress and the three psychological problems.
Limitations
The cross-sectional design and the sampling of all participants from one junior high school impeded causal inferences and the generalization of our findings, respectively.
Conclusions
We found similar indirect and direct protective roles of parental involvement in boys' and girls' mental health, and girls were more vulnerable to stress.
Keywords: Parental involvement, Mental health, Stress, Depression, Anxiety, Posttraumatic stress symptoms
1. Introduction
After the outbreak of novel coronavirus disease 2019 (COVID-19) in Wuhan, COVID-19 spread throughout China during the Chinese New Year at the beginning of 2020. The Chinese government implemented many policies to effectively stop the further spread of the virus (Hsiang et al., 2020). Although policies to encourage face mask use played a positive role in Chinese mental health (Wang et al., 2020a), other policies, such as closing schools, closing public areas where people congregate (e.g., restaurants and places of entertainment), and implementing home quarantine, together with the threat of COVID-19, have been shown to have a widespread negative impact on people's mental health, such as depression, anxiety, and posttraumatic stress disorder (Li et al., 2020; Zhao et al., 2020; S.-J. Zhou et al., 2020).
Adolescence is identified as a sensitive period that is critical for biosocial development (e.g., hormonal changes, an increasing need for social connections and self-identity development), and individuals are also more vulnerable to psychological problems during this period (Orben et al., 2020). Additionally, during the COVID-19 epidemic, adolescents have faced not only drastic changes in their daily lives (e.g., online schooling, social distancing, worries about being infected) but also academic pressures. Therefore, the stressful events caused by COVID-19 may affect the psychological health of adolescents more than that of other age groups (Ren et al., 2021, Ren et al., 2021). It is important to identify what factors could protect adolescents from such stressful events, which would allow educators, parents, and public health service workers to conduct more effective interventions on this issue.
To date, some studies have examined several risk factors and protective factors for adolescent mental health during COVID-19. For example, numerous cross-sectional studies have reported that female gender, older grade, and less physical exercise increased the risks of suffering psychological problems such as depression and anxiety symptoms (F. Chen et al., 2020; S. Chen et al., 2020; Chen et al., 2021; Gazmararian et al., 2021; Lu et al., 2020; Qin et al., 2021; Tang et al., 2021; J. Zhou et al., 2020; S.-J. Zhou et al., 2020). Other risk factors were also found to include being an ethnic minority, having a lower family socioeconomic status, and having limited living space (Gazmararian et al., 2021; Ravens-Sieberer et al., 2021). In terms of protective factors, resilience and positive coping (Zhang et al., 2020), discussions with parents about COVID-19 (Tang et al., 2021), a problem-focused coping style, and positive attitudes toward home quarantine (Duan et al., 2020) were found to be protective against adolescents' psychological problems.
Although there have been some studies on the risk and protective factors of psychological problems in adolescents during the epidemic, little is known about the protective role that parental involvement at home plays in psychological problems. Parental involvement at home refers to a wide range of behaviors that parents perform at home to help their children achieve better psychological development and academic success (Seginer, 2006). The protective role of adolescents' parents may be more salient during the COVID-19 pandemic than at other times. First, school closure and home quarantine have made it more difficult for adolescents to gain peer support. At the same time, adolescents have had to interact more passively with their parents at home, making parental help the most prominent resource available. Second, in an effort to maintain the pace of teaching, the new teaching method of online learning was launched in early March 2020 in the context of home isolation and school closure policies. This has posed a new challenge for middle school students in terms of learning, as they have had to complete homework online, take exams online, and stay focused while studying on electronic devices. Parental involvement can help to identify the difficulties that adolescents face in a timely manner and provide help to solve these difficulties, thus alleviating the psychological problems caused by such challenges.
Thus, parental involvement should be one of the most important protective factors for adolescents' mental health during the COVID-19 pandemic. Indeed, studies have shown that higher parental involvement is associated with fewer mental illnesses in adolescents (Pengpid and Peltzer, 2018; Tian et al., 2021; Wang and Sheikh-Khalil, 2014). It is believed that parental involvement (e.g., obtaining learning materials (e.g., applications, software, study guides) for their children and eating the main meal around a table with their children) helps adolescents deal with difficulties and maintain a healthy lifestyle, which could directly prevent psychological problems.
Furthermore, parental involvement might indirectly reduce psychological problems by alleviating perceived stress due to COVID-19. Stress is considered to be a core risk factor in the development of psychological problems (Grant et al., 2004; Yarcheski and Mahon, 2000), and existing studies have shown that higher stress perceived by adolescents contributes to the later development of a mental disorder (Charles et al., 2013; Lindholdt et al., 2021). Furthermore, the perceived stress caused by COVID-19 has also been found to be associated with depressive symptoms in adolescents (Liu and Wang, 2021). However, to the best of our knowledge, there is no direct evidence that parental involvement reduces adolescents' perceived stress when facing stressful life events such as COVID-19. However, existing studies have shown that parental involvement benefits children in a variety of aspects, including better social skills (El Nokali et al., 2010) and emotional self-regulation skills (Shumow and Lomax, 2002), which may help adolescents better cope with stress when facing a stressful event.
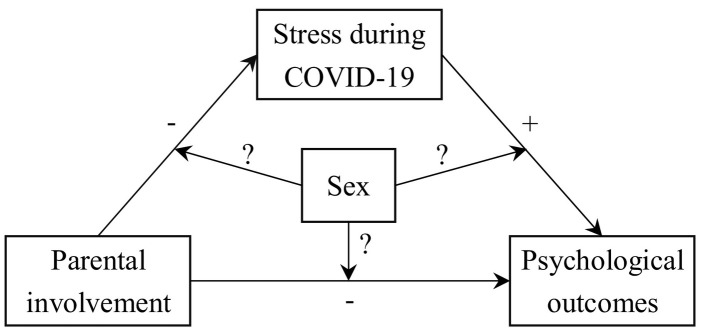
In summary, in the current study, an online survey was conducted during school closures from March–April 2020; the aim was to investigate the associations between parental involvement in adolescents' learning at home, adolescents' perceived stress, and negative psychological outcomes (i.e., depression, anxiety, and posttraumatic stress symptoms (PTSS)). The first hypothesis of the present study was that higher parental involvement at home would be related to fewer psychological problems among adolescents during the COVID-19 outbreak (H1). We also hypothesized that parental involvement would reduce psychological problems by reducing the stress that adolescents perceived. Specifically, we expected that higher parental involvement would relate to lower perceived stress and that lower perceived stress in turn would be associated with fewer psychological problems (H2). Given that some studies have shown sex differences in adolescents' depression, anxiety and posttraumatic symptoms when facing traumatic events (Tang et al., 2019; Zhang et al., 2014; S.-J. Zhou et al., 2020), the current study also investigated whether sex moderated the mediation. In conclusion, the above hypotheses were summarized into one model, and a research question was raised as to whether sex plays a moderating role in the three hypothesized relationships (see Fig. 1 ).
Fig. 1.
Conceptual model.
2. Method
2.1. Participants and procedure
After obtaining permission from a middle school in Southwest China, we conducted an online survey from March to April 2020, when the school was closed and all adolescents were in online schooling at home. With the help of the school, a link to the questionnaire was sent to the students to fill out only with the consent of the students and their parents. All participants were debriefed on the first page of the online questionnaire with the following information: a. the purpose of the study was to understand the mental health of middle school students after the epidemic; b. they were participating in the study anonymously, voluntarily and without pay; and c. if they refused to participate in the survey, they could simply withdraw from the questionnaire.
Finally, 1744 junior high school students completed the questionnaire. Eighty-one students were excluded because they had chosen all the same responses throughout the questionnaires, which included reverse-scored items. As a result, a total of 1663 valid data points (effective rate 95.35%) were obtained. There were 712 boys and 951 girls aged 11 to 18 (M age = 14.24, SD = 1.04). Of these, 713, 621, and 329 students were in Grades 7, 8, and 9, respectively.
2.2. Measures
2.2.1. Parental involvement at home
The scale to measure parental involvement at home was adapted from a questionnaire on parental support for learning in the home, which was derived from the parent questionnaire of the 2012 OECD Programme for International Student Assessment (OECD, 2012). The Chinese version of this scale has demonstrated good psychometric properties (Cheng et al., 2021; Thanh Minh et al., 2020). Students were asked, “How often have your parents done the following things with you at home since COVID-19?” They then responded to seven items (e.g., “They helped me with my homework”) on a five-point scale (1 = never or hardly ever, 2 = once or twice thus far, 3 = once or twice a month, 4 = once or twice a week, 5 = every day or almost every day). The total scores of all items were calculated to evaluate the frequencies with which parents provided support in their children's education during the COVID-19 pandemic. Higher scores represented greater support that students received from their parents. The Cronbach's α in the current sample was 0.83.
2.2.2. Stress experienced since COVID-19
The Perceived Stress Scale (PSS) (Cohen et al., 1983) was used to gauge the stress experienced by adolescents from the time of the COVID-19 outbreak to the time the current survey was administered. Good reliability and validity of the Chinese PSS have been demonstrated in previous studies (Chu et al., 2015; Liu and Wang, 2021). The instructions were adapted as follows to be suitable to measure the level of stress since COVID-19: “The questions on this scale ask you about your feelings and thoughts since COVID-19. In each case, you will be asked to indicate how often you felt or thought a certain way”. Fourteen items were rated by students (e.g., “How often have you felt difficulties were piling up so high that you could not overcome them?”) on a five-point scale (0 = never, 1 = almost never, 2 = sometimes, 3 = fairly often, 4 = very often). After 7 reverse-scored items were reverse coded, all items were added, and higher scores indicated a higher level of stress that students experienced. The Cronbach's α in the current sample was 0.79.
2.2.3. Depression
The current study employed the Center for Epidemiologic Studies Depression Scale (CES-D) (Radloff, 1977) to measure the severity of depressive symptoms. The CES-D scale contains 20 items (e.g., “I felt depressed”), and the Chinese version has also been proven to be valid and reliable in many studies (Chen et al., 2021; Wang et al., 2018). The instructions were as follows: “Below is a list of the ways you might have felt or behaved. Please tell me how often you have felt this way during the last month”. Students rated the items using the following four-point scale: 0 = rarely or none of the time (less than 1 day for each week), 1 = some or little of the time (1–2 days for each week), 2 = occasionally or a moderate amount of time (3–4 days for each week), and 3 = most or all of the time (5–7 days for each week). Four items referring to positive feelings were coded in reverse. The total scores were then calculated by summing all the items, with higher scores representing more severe depression. The Cronbach's α in the current sample was 0.93.
2.2.4. Anxiety
The Chinese version of the Zung Self-rating Anxiety Scale (SAS) (Zung, 1971) was used to measure adolescents' levels of anxiety. The introduction of this scale stated that participants should indicate “how the listed items applied to you within the last month”. Then, 20 items about physical and psychological symptoms of anxiety were rated on a 4-point scale, where 1 = none or a little the time, 2 = some of the time, 3 = a good part of the time, and 4 = most or all of the time. All items were added to calculate the original score after the 5 reverse items had been reverse coded. Then, the standard score was calculated as the rounded number of the original scores multiplied by 1.25. In the present study, the Cronbach's α was 0.83.
2.2.5. Posttraumatic stress symptoms (PTSS)
The PTSS that adolescents experienced during the COVID-19 pandemic were measured with the PTSD Check List-Civilian Version (PCL-C), which is suitable for assessing reexperiencing, avoidance/numbing and hyperarousal symptoms caused by any traumatic event. This scale contains 17 items with no reverse coded items. All items were self-rated by adolescents on a 5-point scale (1–5) from “not at all” to “extremely”. The PCL-C has also been widely applied with Chinese samples, showing good psychometric performance (Liang et al., 2020; Zhang et al., 2011). In the current study, the Cronbach's α was 0.95.
3. Results
3.1. Prevalence of depression, anxiety and posttraumatic stress symptoms
To determine the prevalence of depression, anxiety and PTSS, we used the following criteria: a. CES-D scores ≥20 represented depression symptoms; b. SAS scores of 50–59 represented mild anxiety, 60–69 represented moderate anxiety, and above 69 represented severe anxiety; and c. PCL-C scores ≥38 represented PTSS. Among 1663 adolescents, 35.4% (41.0% girls vs. 27.9% boys) had depression symptoms, 16.8% (18.5% girls vs. 14.6% boys) had mild anxiety, 3.9% (5.0% girls vs. 2.4% boys) had moderate anxiety, 1.0% (1.5% girls vs. 0.4% boys) had severe anxiety, and 25% (26.0% girls vs. 23.7% boys) had PTSS.
3.2. Descriptive statistics and correlational analysis
We performed descriptive statistical analysis and Pearson correlation analysis in SPSS 26. As presented in Table 1 , parental involvement during school closure was negatively associated with adolescents' perceived stress and symptoms of depression, symptoms of anxiety and PTSS. Perceived stress was positively related to symptoms of depression, symptoms of anxiety and PTSS.
Table 1.
Descriptive statistics and correlations.
| 1 | 2 | 3 | 4 | 5 | 6 | |
|---|---|---|---|---|---|---|
| 1. PI | – | |||||
| 2. PS | −0.39⁎⁎⁎ | – | ||||
| 3. DEP | −0.39⁎⁎⁎ | 0.64⁎⁎⁎ | – | |||
| 4. ANX | −0.34⁎⁎⁎ | 0.60⁎⁎⁎ | 0.78⁎⁎⁎ | – | ||
| 5. PTSS | −0.31⁎⁎⁎ | 0.60⁎⁎⁎ | 0.71⁎⁎⁎ | 0.69⁎⁎⁎ | – | |
| 6. Age | −0.07⁎⁎ | 0.01 | 0.06⁎ | 0.04 | 0.01 | – |
| M | 20.92 | 26.83 | 16.93 | 41.95 | 30.81 | 14.24 |
| SD | 6.80 | 9.48 | 10.45 | 9.52 | 13.52 | 1.04 |
Note. PI = Parental involvement, PS = Perceived stress, DEP = Depression symptoms, ANX = Anxiety symptoms, PTSS = Posttraumatic stress symptoms.
p < .001.
p < .01.
p < .05.
3.3. Test of the moderated mediation models
Three moderated mediation models with depression (Model 1), anxiety (Model 2) and PTSS (Model 3) as the dependent variables were conducted in PROCESS 3.5 (Model 59) for SPSS. Age was added as a covariate, and the continuous variables that constructed interactions were mean centered. To estimate the 95% confidence intervals, 5000 percentile bootstrap samples were performed. The results for models 1–3 are summarized in Tables 2 and 3 . First, for those paths shared in models 1–3, we found that higher parental involvement at home was associated with lower perceived stress among adolescents and that girls perceived more stress than boys. The negative association between parental involvement and stress was similar for boys and girls.
Table 2.
The regression results in three moderated mediation models.
| Regression models | Paths | R2 | F (df1, df2) | Unstandardized coefficients | 95% CI |
|---|---|---|---|---|---|
| Shared parts in Model 1–3 | PI → PS | 0.16 | 79.91⁎⁎⁎ (4, 1658) |
−0.53⁎⁎⁎ | −0.61, −0.45 |
| Sex → PS | −1.41⁎⁎ | −2.26, −0.56 | |||
| Age → PS | −0.19 | −0.59, 0.21 | |||
| PI × Sex → PS | −0.04 | −0.17, 0.09 | |||
| Model 1 | PI → DEP | 0.45 | 226.25⁎⁎⁎ (6, 1656) |
−0.23⁎⁎⁎ | −0.31, −0.16 |
| PS → DEP | 0.69⁎⁎⁎ | 0.63, 0.74 | |||
| Sex → DEP | −1.86⁎⁎⁎ | −2.62, −1.10 | |||
| Age → DEP | 0.43⁎ | 0.07, 0.79 | |||
| PI × Sex → DEP | −0.02 | −0.14, 0.10 | |||
| PS × Sex → DEP | −0.15⁎⁎ | −0.24, −0.06 | |||
| Model 2 | PI → ANX | 0.38 | 166.70⁎⁎⁎ (6, 1656) |
−0.16⁎⁎⁎ | −0.24, −0.09 |
| PS → ANX | 0.60⁎⁎⁎ | 0.55, 0.65 | |||
| Sex → ANX | −0.81⁎ | −1.55, −0.08 | |||
| Age → ANX | 0.23 | −0.12, 0.58 | |||
| PI × Sex → ANX | −0.01 | −0.13, 0.11 | |||
| PS × Sex → ANX | −0.13⁎⁎ | −0.22, −0.05 | |||
| Model 3 | PI → PTSS | 0.37 | 163.76⁎⁎⁎ (6, 1656) |
−0.19⁎⁎⁎ | −0.30, −0.09 |
| PS → PTSS | 0.89⁎⁎⁎ | 0.82, 0.97 | |||
| Sex → PTSS | −0.09 | −1.14, 0.96 | |||
| Age → PTSS | −0.03 | −0.53, 0.46 | |||
| PI × Sex → PTSS | 0.01 | −0.16, 0.18 | |||
| PS × Sex → PTSS | −0.15⁎⁎ | −0.37, −0.12 |
Note. PI = Parental involvement, PS = Perceived stress, DEP = Depression symptoms, ANX = Anxiety symptoms, PTSS = Posttraumatic stress symptoms. Sex was coded as 0 = girls, 1 = boys.
p < .001.
p < .01.
p < .05.
Table 3.
The mediation effects and the paths from perceived stress to psychological outcomes among boys and girls.
| Paths | Sex | Unstandardized effects | 95% CI | Indexes of moderated mediation (95% CI) |
|---|---|---|---|---|
| PI → PS → DEP | Girls | −0.36 | −0.43, −0.30 | 0.06 (−0.04, 0.15) |
| Boys | −0.31 | −0.39, −0.24 | ||
| PI → PS → ANX | Girls | −0.32 | −0.38, −0.26 | 0.05 (−0.03, 0.13) |
| Boys | −0.26 | −0.32, −0.21 | ||
| PI → PS → PTSS | Girls | −0.47 | −0.56, −0.38 | 0.10 (−0.03, 0.23) |
| Boys | −0.37 | −0.46, −0.28 | ||
| PS → DEP | Girls | 0.69 | 0.63, 0.74 | NA |
| Boys | 0.54 | 0.47, 0.61 | ||
| PS → ANX | Girls | 0.60 | 0.55, 0.65 | NA |
| Boys | 0.46 | 0.40, 0.53 | ||
| PS → PTSS | Girls | 0.89 | 0.82, 0.97 | NA |
| Boys | 0.65 | 0.55, 0.75 |
Note. PI = Parental involvement, PS = Perceived stress, DEP = Depression symptoms, ANX = Anxiety symptoms, PTSS = Posttraumatic stress symptoms.
Then, we found some consistent results for depression, anxiety and PTSS across models 1–3. On the whole, higher perceived stress was related to more severe psychological symptoms, and this relationship was more salient for girls than for boys (the simple slopes are presented in Table 3 and plotted in Fig. 2 ). Moreover, after we controlled for the mediator (perceived stress), there was still a negative direct effect of parental involvement on the three psychological outcomes, and this relationship was similar for girls and boys. Some inconsistent results across models 1–3 were that a. girls suffered higher depression and anxiety symptoms than boys, but they had similar levels of PTSS, and b. only depression levels increased with age, while anxiety and PTSS levels were unrelated to age.
Fig. 2.
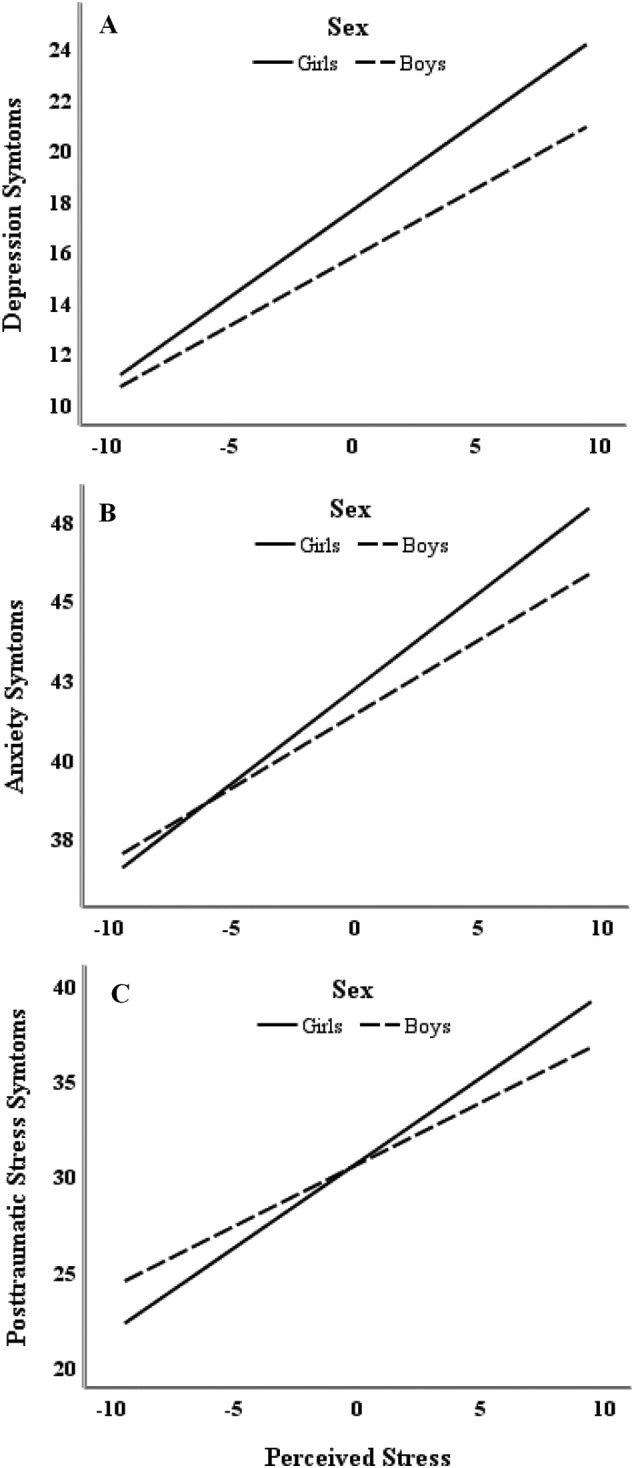
The moderating effect of sex on the association between perceived stress and negative psychological outcomes.
Finally, the indirect paths from parental involvement to depression, anxiety and PTSS via perceived stress were consistently significant for both boys and girls. The size of the indirect effect was not moderated by sex in any of the three models, suggesting that the protective effect of parental involvement on psychological outcomes through reducing perceived stress was similar for both boys and girls.
4. Discussion
The present study replicated some of the findings of previous studies but, more importantly, contributed new findings on the protective factors against adolescent psychological problems during COVID-19. First, compared with the prevalence of depression (24.3%) (Tang et al., 2019) and anxiety (13.0%) (Jin et al., 2014) in Chinese adolescents who had not experienced traumatic events, the prevalence of depression (35.4%) and anxiety (21.7%) symptoms was relatively high among the current adolescent sample from southern China. The prevalence was similar to that of other cross-sectional studies that used the same scales as the current study and that were conducted with Chinese adolescents during the COVID-19 outbreaks (Chen et al., 2021; J. Zhou et al., 2020). In addition, the prevalence of PTSS in the current sample (25.0%) was also comparable to the meta-prevalence of PTSS (28.34%) in 106,713 people experiencing the COVID-19 outbreak (Qiu et al., 2021). Notably, the meta-analysis did not include data from people under 18 years old, suggesting that no attention has been given to adolescents' PTSS. In summary, this study demonstrates that psychological problems in adolescents during isolation cannot be ignored and need intervention just as urgently as those of any other group.
Furthermore, our research highlights that for adolescents, parental involvement, as a source of social support, should be more salient during home quarantine and school closures than during other times, as other social support from peers or teachers, for example, has been interrupted and new challenges have occurred (e.g., online schooling). This claim was supported by our empirical results, which were consistent with the buffering and main effect models of social support (Cohen and Wills, 1985). Consistent with the buffering model (Cohen and Wills, 1985), when adolescents faced the stressful events of COVID-19, parental support helped attenuate their stress responses, which in turn prevented three negative psychological outcomes (i.e., depression, anxiety and PTSS). As we mentioned in the introduction, through parental involvement at home, such as spending time just talking to adolescents and helping with homework, parents could discover the difficulties that adolescents faced in both life and study in a timely manner and help them cope with them.
Additionally, we also found a direct negative effect of parental involvement on the three negative psychological outcomes after controlling for age, sex, and the mediating role of perceived stress. According to the main effect model (Cohen and Wills, 1985), social support has generalized benefits or a direct main protective effect on mental health irrespective of whether the individual has faced stress. Regular support provides a sense of self-worth, stability, and predictability and maintains a positive mood and healthy lifestyle that directly benefits adolescent mental health. Based on the current study, parental involvement, such as eating the main meal around a table with adolescents and spending time just talking to adolescents, may help adolescents maintain a healthy behavioral pattern and positive sense of the situation and the self, which help maintain mental health. This result is consistent with Tang et al. (2021), which showed that just talking to parents about COVID-19 reduced adolescents' depression and anxiety symptoms. Importantly, the direct paths and indirect paths from parental involvement to the three negative psychological outcomes showed no differences between sexes, suggesting that the stress-buffering role and direct protective role of parental involvement are effective for both boys and girls.
We also consistently found sex differences in perceived stress and depression and anxiety symptoms, with girls perceiving more stress and experiencing more depression and anxiety symptoms. This is consistent with existing studies finding that being female was associated with a higher risk of depression and anxiety (F. Chen et al., 2020; S. Chen et al., 2020; Gazmararian et al., 2021; Wang et al., 2020b; S.-J. Zhou et al., 2020). In addition to replicating previous studies, we also found a moderating effect of sex on the pathways from perceived stress to the three negative psychological outcomes. Specifically, perceived stress had a greater impact on depression, anxiety and PTSS among girls than among boys. In other words, girls were more vulnerable to perceived stress associated with COVID-19.
In conclusion, we provided new evidence about the role of parental involvement in protecting adolescents' mental health during the COVID-19 pandemic, and the protective effects were similar for both boys and girls. To date, COVID-19 still threatens the lives of many people around the world. In China, for example, the epidemic continues to break out in some areas, and parts of the country still face the prospect of home quarantine at any time. Therefore, although the data from this study are one year old, the results still have important implications for current mental health interventions for adolescents, especially when facing the challenges of home quarantine and school closure. Our results provide insights for educators and even public psychology services, showing that improving parental involvement, such as telling parents to chat with their children about their lives or studies, to provide help with learning, and to eat a meal together with their children around a table, would be effective in preventing psychological problems during the COVID-19 pandemic. Moreover, since girls were more vulnerable to COVID-19 stress, more attention should be given to girls who experience high stress when intervening in adolescent mental health. In addition to the intervention strategies derived from the findings of this study, it is worth noting the advantages and effectiveness of internet cognitive behavior therapy (iCBT) to improve mental health during the COVID-19 pandemic. iCBT not only has been proven to be effective in improving insomnia and PTSS (Sijbrandij et al., 2016; Soh et al., 2020) but also is an important means of obtaining professional help for adolescents in quarantine (Ho et al., 2020a; Zhang and Ho, 2017).
Despite the contributions we made, the current study also suffers from several limitations. First, the cross-sectional design fails to show the causal effect of parental involvement on psychological outcomes. It is possible that adolescents with better mental health encouraged higher parental involvement. Future studies should employ a longitudinal design to further verify the results we found. Second, all variables were self-reported by adolescents, which may have strengthened or weakened the actual relationships between variables. Although self-perceived support from parents is important for adolescents, it would be better for future studies to collect parents' reported parental involvement to replicate our results. Furthermore, this study used self-report questionnaires to measure psychiatric symptoms and did not make clinical diagnoses. The gold standard for establishing psychiatric diagnosis, involving structured clinical interviews and functional neuroimaging (Ho et al., 2020b; Husain et al., 2020, Husain et al., 2020), should be considered in future studies. Finally, although the sample size in our study was not small, our sample still limited the ability of our results to be generalized to all adolescents because all of the participants were from one junior high school in southwestern China. A more representative sample is necessary for future research.
CRediT authorship contribution statement
Fangyuan Ding undertook the statistical analysis and wrote the first draft of the manuscript. Yucheng Jia managed the literature searches, Xianmeng Xiong, Peichao Chen, and Shulin Xiong conducted the investigation, and Gang Cheng wrote design the study and wrote the protocol. All authors contributed to the revision of the draft.
Role of the funding source
The funders had no role in study design, data collection, and analysis, decision to publish, or preparation of the manuscript.
Conflict of interest
None.
Acknowledgements
This work was supported by the Research Project of Humanities and Social Sciences in Colleges and Universities of Guizhou Province (Master Program) supported by the Department of Education of Guizhou Province [grant number 2020SSD017]; the Special Project for Academic Novice Cultivation and Innovative Exploration [grant number QianKeQuanPingTaiRenCai [2017]5726-16], supported by Guizhou Provincial Science and Technology Foundation (GPSTF); PhD early development program of Guizhou Normal University (2017).
References
- Charles S.T., Piazza J.R., Mogle J., Sliwinski M.J., Almeida D.M. The wear and tear of daily stressors on mental health. Psychol. Sci. 2013;24(5):733–741. doi: 10.1177/0956797612462222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen F., Zheng D., Liu J., Gong Y., Guan Z., Lou D. Depression and anxiety among adolescents during COVID-19: a cross-sectional study. Brain Behav. Immun. 2020;88:36–38. doi: 10.1016/j.bbi.2020.05.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen S., Cheng Z., Wu J. Risk factors for adolescents' mental health during the COVID-19 pandemic: a comparison between Wuhan and other urban areas in China. Glob. Health. 2020;16(1) doi: 10.1186/s12992-020-00627-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen X., Qi H., Liu R., Feng Y., Li W., Xiang M., Cheung T., Jackson T., Wang G., Xiang Y.-T. Depression, anxiety and associated factors among Chinese adolescents during the COVID-19 outbreak: a comparison of two cross-sectional studies. Transl. Psychiatry. 2021;11(1) doi: 10.1038/s41398-021-01271-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng G., Liu J., Yang Y., Wang Y., Xiong X., Liu G. Stressful events and adolescents’ suicidal ideation during the COVID-19 epidemic: a moderated mediation model of depression and parental educational involvement. Child Youth Serv. Rev. 2021;127 doi: 10.1016/j.childyouth.2021.106047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu J., Khan M., Jahn H., Krämer A. Only-child status in relation to perceived stress and studying-related life satisfaction among university students in China: a comparison with international students. PLoS One. 2015;10 doi: 10.1371/journal.pone.0144947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S., Wills T.A. Stress, social support, and the buffering hypothesis. Psychol. Bull. 1985;98(2):310–357. doi: 10.1037/0033-2909.98.2.310. [DOI] [PubMed] [Google Scholar]
- Cohen S., Kamarck T., Mermelstein R. A global measure of perceived stress. J. Health Soc. Behav. 1983;24(4):385–396. doi: 10.2307/2136404. [DOI] [PubMed] [Google Scholar]
- Duan L., Shao X., Wang Y., Huang Y., Miao J., Yang X., Zhu G. An investigation of mental health status of children and adolescents in China during the outbreak of COVID-19. J. Affect. Disord. 2020;275:112–118. doi: 10.1016/j.jad.2020.06.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El Nokali N.E., Bachman H.J., Votruba-Drzal E. Parent involvement and children's academic and social development in elementary school. Child Dev. 2010;81(3):988–1005. doi: 10.1111/j.1467-8624.2010.01447.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gazmararian J., Weingart R., Campbell K., Cronin T., Ashta J. Impact of COVID-19 pandemic on the mental health of students from 2 semi-rural high schools in Georgia*. J. Sch. Health. 2021;91(5):356–369. doi: 10.1111/josh.13007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant K.E., Compas B.E., Thurm A.E., McMahon S.D., Gipson P.Y. Stressors and child and adolescent psychopathology: measurement issues and prospective effects. J. Clin. Child Adolesc. Psychol. 2004;33(2):412–425. doi: 10.1207/s15374424jccp3302_23. [DOI] [PubMed] [Google Scholar]
- Ho C.S.H., Chee C.Y.I., Ho R.C.M. Mental health strategies to combat the psychological impact of coronavirus disease 2019 (COVID-19) beyond paranoia and panic. Ann. Acad. Med. Singap. 2020;49(3):155–160. //WOS:000533622100007. [PubMed] [Google Scholar]
- Ho C.S.H., Lim L.J.H., Lim A.Q., Chan N.H.C., Tan R.S., Lee S.H., Ho R.C.M. Diagnostic and predictive applications of functional near-infrared spectroscopy for major depressive disorder: a systematic review. Front. Psych. 2020;11 doi: 10.3389/fpsyt.2020.00378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsiang S., Allen D., Annan-Phan S., Bell K., Bolliger I., Chong T., Druckenmiller H., Huang L.Y., Hultgren A., Krasovich E., Lau P., Lee J., Rolf E., Tseng J., Wu T. The effect of large-scale anti-contagion policies on the COVID-19 pandemic. Nature. 2020;584(7820):262–267. doi: 10.1038/s41586-020-2404-8. [DOI] [PubMed] [Google Scholar]
- Husain S.F., Tang T.B., Yu R., Tam W.W., Tran B., Quek T.T., Hwang S.H., Chang C.W., Ho C.S., Ho R.C. Cortical haemodynamic response measured by functional near infrared spectroscopy during a verbal fluency task in patients with major depression and borderline personality disorder. Ebiomedicine. 2020;51 doi: 10.1016/j.ebiom.2019.11.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Husain S.F., Yu R., Tang T.-B., Tam W.W., Tran B., Quek T.T., Hwang S.-H., Chang C.W., Ho C.S., Ho R.C. Validating a functional near-infrared spectroscopy diagnostic paradigm for major depressive disorder. Sci. Rep. 2020;10(1) doi: 10.1038/s41598-020-66784-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jin Y., He L., Kang Y., Chen Y., Lu W., Ren X., Song X., Wang L., Nie Z., Guo D., Yao Y. Prevalence and risk factors of anxiety status among students aged 13–26 years. Int. J. Clin. Exp. Med. 2014;7(11):4420–4426. [PMC free article] [PubMed] [Google Scholar]
- Li H.Y., Cao H., Leung D.Y.P., Mak Y.W. The psychological impacts of a COVID-19 outbreak on college students in China: a longitudinal study. Int. J. Environ. Res. Public Health. 2020;17(11) doi: 10.3390/ijerph17113933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang L., Ren H., Cao R., Hu Y., Qin Z., Li C., Mei S. The effect of COVID-19 on youth mental health. Psychiatry Q. 2020;91(3):841–852. doi: 10.1007/s11126-020-09744-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindholdt L., Labriola M., Andersen J.H., Kjeldsen M.M.Z., Obel C., Lund T. 2021. Perceived stress among adolescents as a marker for future mental disorders: a prospective cohort study. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Q., Wang Z. Perceived stress of the COVID-19 pandemic and adolescents' depression symptoms: the moderating role of character strengths. Personal. Individ. Differ. 2021;182 doi: 10.1016/j.paid.2021.111062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu C., Chi X., Liang K., Chen S.-T., Huang L., Guo T., Jiao C., Yu Q., Veronese N., Soares F.C., Grabovac I., Yeung A., Zou L. Moving more and sitting less as healthy lifestyle behaviors are protective factors for insomnia, depression, and anxiety among adolescents during the COVID-19 pandemic. Psychol. Res. Behav. Manag. 2020;13:1223–1233. doi: 10.2147/prbm.S284103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- OECD . 2012. PISA 2009 Technical Report. /content/book/9789264167872-en. [DOI] [Google Scholar]
- Orben A., Tomova L., Blakemore S.-J. The effects of social deprivation on adolescent development and mental health. Lancet Child Adolesc. Health. 2020;4(8):634–640. doi: 10.1016/S2352-4642(20)30186-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pengpid S., Peltzer K. Parental involvement and mental health among school-going adolescents in five Caribbean countries. J. Psychol. Afr. 2018;28(5):394–399. doi: 10.1080/14330237.2018.1501916. [DOI] [Google Scholar]
- Qin Z., Shi L., Xue Y., Lin H., Zhang J., Liang P., Lu Z., Wu M., Chen Y., Zheng X., Qian Y., Ouyang P., Zhang R., Yi X., Zhang C. Prevalence and risk factors associated with self-reported psychological distress among children and adolescents during the COVID-19 pandemic in China. JAMA Netw. Open. 2021;4(1) doi: 10.1001/jamanetworkopen.2020.35487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qiu D., Li Y.L., Li L., He J., Ouyang F.Y., Xiao S.Y. Prevalence of post-traumatic stress symptoms among people influenced by coronavirus disease 2019 outbreak: a meta-analysis. Eur. Psychiatry. 2021;64(1) doi: 10.1192/j.eurpsy.2021.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff L.S. The CES-D scale: a self-report depression scale for research in the general population. Appl. Psychol. Meas. 1977;1(3):385–401. doi: 10.1177/014662167700100306. [DOI] [Google Scholar]
- Ravens-Sieberer U., Kaman A., Erhart M., Devine J., Schlack R., Otto C. Impact of the COVID-19 pandemic on quality of life and mental health in children and adolescents in Germany. Eur. Child Adolesc. Psychiatry. 2021 doi: 10.1007/s00787-021-01726-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ren Z., Xin Y., Ge J., Zhao Z., Liu D., Ho R.C.M., Ho C.S.H. Psychological impact of COVID-19 on college students after school reopening: a cross-sectional study based on machine learning. Front. Psychol. 2021;12 doi: 10.3389/fpsyg.2021.641806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ren Z., Xin Y., Wang Z., Liu D., Ho R.C.M., Ho C.S.H. What factors are most closely associated with mood disorders in adolescents during the COVID-19 pandemic? A cross-sectional study based on 1,771 adolescents in Shandong Province China. Front. Psychiatry. 2021;12 doi: 10.3389/fpsyt.2021.728278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seginer R. Parents' educational involvement: a developmental ecology perspective. Parenting-Sci. Pract. 2006;6(1):1–48. doi: 10.1207/s15327922par0601_1. [DOI] [Google Scholar]
- Shumow L., Lomax R. Parental efficacy: predictor of parenting behavior and adolescent outcomes. Parenting-Sci. Pract. 2002;2(2):127–150. doi: 10.1207/s15327922par0202_03. Article Pii 785828938. [DOI] [Google Scholar]
- Sijbrandij M., Kunovski I., Cuijpers P. Effectiveness of internet-delivered cognitive behavioral therapy for posttraumatic stress disorder: a systematicreview and meta-analysis. Depress. Anxiety. 2016;33(9):783–791. doi: 10.1002/da.22533. [DOI] [PubMed] [Google Scholar]
- Soh H.L., Ho R.C., Ho C.S., Tam W.W. Efficacy of digital cognitive behavioural therapy for insomnia: a meta-analysis of randomised controlled trials. Sleep Med. 2020;75:315–325. doi: 10.1016/j.sleep.2020.08.020. [DOI] [PubMed] [Google Scholar]
- Tang X., Tang S., Ren Z., Wong D.F.K. Prevalence of depressive symptoms among adolescents in secondary school in mainland China: a systematic review and meta-analysis. J. Affect. Disord. 2019;245:498–507. doi: 10.1016/j.jad.2018.11.043. [DOI] [PubMed] [Google Scholar]
- Tang S., Xiang M., Cheung T., Xiang Y.-T. Mental health and its correlates among children and adolescents during COVID-19 school closure: the importance of parent-child discussion. J. Affect. Disord. 2021;279:353–360. doi: 10.1016/j.jad.2020.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thanh Minh N., Xiao X., Xiong S., Guo C., Cheng G. Effects of parental educational involvement on classroom peer status among chinese primary school students: a moderated mediation model of psychological Suzhi and family socioeconomic status. Child Youth Serv. Rev. 2020;111 doi: 10.1016/j.childyouth.2020.104881. [DOI] [Google Scholar]
- Tian S., Zhang T.-Y., Miao Y.-M., Pan C.-W. Psychological distress and parental involvement among adolescents in 67 low-income and middle-income countries: a population-based study. J. Affect. Disord. 2021;282:1101–1109. doi: 10.1016/j.jad.2021.01.010. [DOI] [PubMed] [Google Scholar]
- Wang M.-T., Sheikh-Khalil S. Does Parental Involvement Matter for Student Achievement and Mental Health in High School? 85(2) 2014. pp. 610–625. [DOI] [PubMed] [Google Scholar]
- Wang M., Yang W., Xiong G., Garrido L. Factor structure and criterion validity across the full scale and ten short forms of the CES-D among chinese adolescents. Psychol. Assess. 2018;30 doi: 10.1037/pas0000559. [DOI] [PubMed] [Google Scholar]
- Wang C., Chudzicka-Czupala A., Grabowski D., Pan R., Adamus K., Wan X., Hetnal M., Tan Y., Olszewska-Guizzo A., Xu L., McIntyre R.S., Quek J., Ho R., Ho C. The association between physical and mental health and face mask use during the COVID-19 pandemic: a comparison of two countries with different views and practices. Front. Psych. 2020;11 doi: 10.3389/fpsyt.2020.569981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 Coronavirus Disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health. 2020;17(5) doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yarcheski A., Mahon N.E. A causal model of depression in early adolescents. West. J. Nurs. Res. 2000;22(8):879–894. doi: 10.1177/01939450022044854. [DOI] [PubMed] [Google Scholar]
- Zhang M.W.B., Ho R.C.M. Moodle: the cost effective solution for internet cognitive behavioral therapy (I-CBT) interventions. Technol. Health Care. 2017;25:163–165. doi: 10.3233/THC-161261. [DOI] [PubMed] [Google Scholar]
- Zhang Z., Shi Z., Wang L., Liu M. One year later: mental health problems among survivors in hard-hit areas of the wenchuan earthquake. Public Health. 2011;125(5):293–300. doi: 10.1016/j.puhe.2010.12.008. [DOI] [PubMed] [Google Scholar]
- Zhang W., Liu H., Jiang X., Wu D., Tian Y. A longitudinal study of posttraumatic stress disorder symptoms and its relationship with coping skill and locus of control in adolescents after an earthquake in China. PloS one. 2014;9(2) doi: 10.1371/journal.pone.0088263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang C., Ye M., Fu Y., Yang M., Luo F., Yuan J., Tao Q. The psychological impact of the COVID-19 pandemic on teenagers in China. J. Adolesc. Health. 2020;67(6):747–755. doi: 10.1016/j.jadohealth.2020.08.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao H., He X., Fan G., Li L., Huang Q., Qiu Q., Kang Z., Du T., Han L., Ding L., Xu H. COVID-19 infection outbreak increases anxiety level of general public in China: involved mechanisms and influencing factors. J. Affect. Disord. 2020;276:446–452. doi: 10.1016/j.jad.2020.07.085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou J., Yuan X., Qi H., Liu R., Li Y., Huang H., Chen X., Wang G. Prevalence of depression and its correlative factors among female adolescents in China during the coronavirus disease 2019 outbreak. Glob. Health. 2020;16(1) doi: 10.1186/s12992-020-00601-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou S.-J., Zhang L.-G., Wang L.-L., Guo Z.-C., Wang J.-Q., Chen J.-C., Liu M., Chen X., Chen J.-X. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. Eur. Child Adolesc. Psychiatry. 2020;29(6):749–758. doi: 10.1007/s00787-020-01541-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zung W.W.K. A rating instrument for anxiety disorders. Psychosomatics. 1971;12(6):371–379. doi: 10.1016/S0033-3182(71)71479-0. [DOI] [PubMed] [Google Scholar]