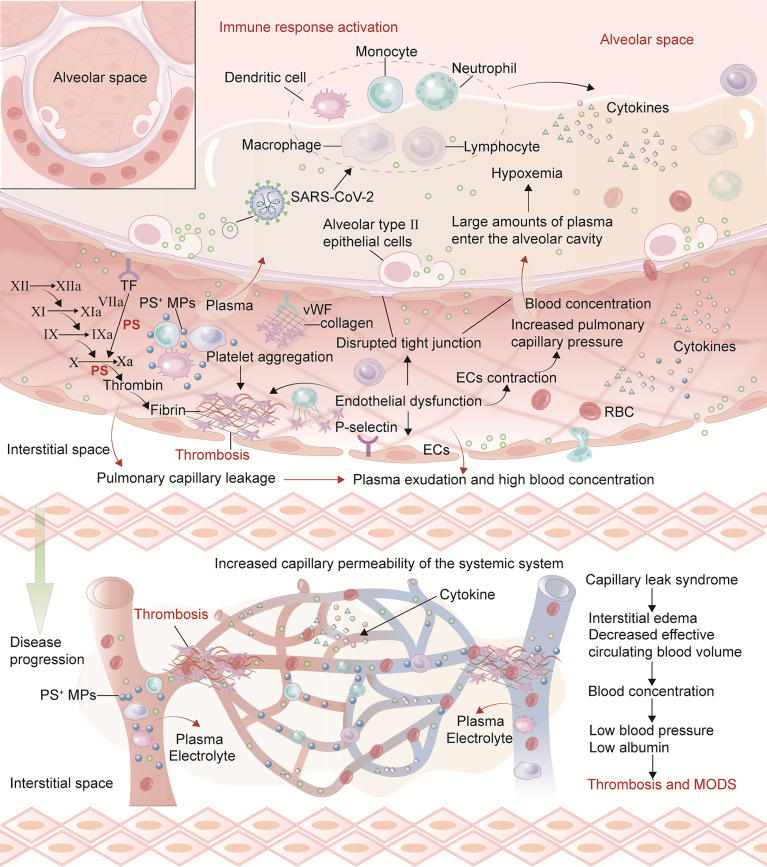
Figure 2.
Mechanisms of endothelial injury promoting thrombosis and CLS in acute COVID-19 and long COVID. After vascular endothelial injury, there may be weakened anticoagulant properties, increased permeability and leukocyte adhesion. TF expression on ECs surface is up-regulated. Antithrombin III, TF pathway inhibitor and protein C system are damaged and lose anticoagulant properties. Injured ECs can release vWF, factor VIII and PS exposure to promote a hypercoagulable state. Furthermore, ECs can increase the expression of chemokines on their surface, promote neutrophil recruitment, and participate in thrombosis. SARS-CoV-2 and cytokines (such as TNF-α, IL-1, IL-6) damage the vascular endothelium, resulting in ECs contraction, connections separating and the appearance of intracellular gaps. The general increase in capillary permeability forms a local or SCLS. The increased permeability of pulmonary capillary endothelial injury can lead to plasma entering the alveolar cavity and form hypoxemia. Furthermore, hypoxia aggravates the contraction of pulmonary capillary ECs which thicken and narrow the capillaries, ultimately causing pulmonary hypertension. The plasma and some erythrocytes in the pulmonary capillaries are pushed into the alveolar space, further aggravating respiratory dysfunction and ARDS. As the disease progresses, injury to circulating blood cells and vascular endothelium can activate cytokines release, resulting in extensive capillary ECs damage, increasing the transport channel diameter and vessels permeability, and albumin leakage in the blood vessels.