Abstract
Parenting and family environment have significant impact on child development, including development of executive function, attention, and self-regulation, and may affect the risk of developmental disorders including attention-deficit/hyperactivity disorder (ADHD). This paper examines the relationship of parenting and family environment factors with ADHD. A systematic review of the literature was conducted in 2014 and identified 52 longitudinal studies. A follow-up search in 2021 identified 7 additional articles, for a total of 59 studies that examined the association of parenting factors with ADHD outcomes: ADHD overall (diagnosis or symptoms), ADHD diagnosis specifically, or presence of the specific ADHD symptoms of inattention and hyperactivity/impulsivity. For parenting factors that were present in three or more studies, pooled effect sizes were calculated separately for dichotomous or continuous ADHD outcomes, accounting for each study’s conditional variance. Factors with sufficient information for analysis were parenting interaction quality (sensitivity/warmth, intrusiveness/reactivity, and negativity/harsh discipline), maltreatment (general maltreatment and physical abuse), parental relationship status (divorce, single parenting), parental incarceration, and child media exposure. All factors showed a significant direct association with ADHD outcomes, except sensitivity/warmth which had an inverse association. Parenting factors predicted diagnosis and overall symptoms as well as inattentive and hyperactive symptoms when measured, but multiple factors showed significant heterogeneity across studies. These findings support the possibility that parenting and family environment influences ADHD symptoms and may affect a child’s likelihood of being diagnosed with ADHD. Prevention strategies that support parents, such as decreasing parenting challenges and increasing access to parent training in behavior management, may improve children’s long-term developmental health.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11121-022-01358-4.
Keywords: ADHD, Attention-deficit/hyperactivity disorder, Parenting, Family environment
Parents, and other primary caregivers (hereinafter referred to as parents), have a strong influence on children’s development starting in infancy (National Academies of Sciences, Engineering, and Medicine (NASEM), 2016b). Parents affect their child’s development directly through daily interaction and communication, parents shape the child’s environment and protect them from risks, and parents are the child’s first role models for interactions with the larger social world (Kiff et al., 2011). Extensive evidence has shown the importance of early environment on social, emotional, and behavioral development (NASEM, 2019b), and the key role that parents play (NASEM, 2016b). However, the relationship is influenced by both the parent and child, including by the child’s communicative and interactive characteristics and by the parent’s responses to the child’s signals (Kiff et al., 2011).
Attention-deficit/hyperactivity disorder (ADHD) is a neurobehavioral condition, characterized by challenges with regulation of attention, emotion, and behavior (American Psychiatric Association, 2013), with multiple risk factors and possible causes (Faraone et al., 2021). Heritability of ADHD has been well documented, but environmental influences, either directly or through gene-environment interactions, are likely to play a significant role in whether symptoms become severe and impairing, thus warranting diagnosis and treatment (Faraone & Larsson, 2019; Faraone & Mick, 2010; Faraone et al., 2021; Freitag & Retz, 2010; Humphreys & Zeanah, 2015). Given that the development of behavior and emotions is strongly affected by childhood experiences, parenting behaviors and family context may affect the development and expression of behavioral symptoms of ADHD (Humphreys & Zeanah, 2015; Sonuga-Barke & Halperin, 2010). The present paper explores factors related to parenting and the likelihood of developing ADHD.
Parenting can influence the child’s development of self-regulation and behavior through multiple pathways. One important influence is through daily interactions with the child (Haltigan et al., 2013; NASEM, 2016). Quality of attachment, which indicates the degree of feeling safe and protected by the parent, has long-term impact on emotional development, including the likelihood of developing mental disorders (Fearon et al., 2010). Parental sensitivity to the child’s signals and supportive responsiveness during interactions are necessary components of a secure parent–child relationship (Claussen & Crittenden, 2000). Positive and supportive parenting behaviors include being sensitive and warm in response to emotional needs, being engaged and involved, and having low levels of intrusive or emotionally reactive behavior. By responding sensitively, secure attachment figures can support children in regulating their emotion and behavior and in developing executive function skills (Menon et al., 2020; Pallini et al., 2019). Conversely, a parent’s persistent lack of sensitivity and failure to respond supportively can result in a lack of predictability which impacts the development of the child’s regulatory processes (Auersperg et al., 2019; Murray & Murray, 2010; Pallini et al., 2019). Negative or hostile responses and harsh discipline have been associated with increased hyperactivity (Romano et al., 2006). At the extremes, parents may neglect basic needs or respond in harmful and abusive ways, and maltreated children may become hypervigilant and attend to their own safety rather than learn and explore, impairing the development of typical attentional processes (Humphreys & Zeanah, 2015; Pallini et al., 2019; Strathearn et al., 2020).
Extended separation from a parent, for example from parental incarceration, or from the instability of care and loss of a key attachment figure that can follow a divorce in some families, has a significant impact on children (D'Onofrio & Emery, 2019; NASEM, 2019b). Such loss affects children even when the child experienced maltreatment (Goldsmith et al., 2004). Like maltreatment, trauma from separation and loss may impair children’s ability to develop executive function, self-regulation, and attention skills (Humphreys & Zeanah, 2015; van der Bij et al., 2020). Another type of family structure, single parenting, has also been identified as a factor that may influence child development, due to associated factors such as increased role demand and decreased economic resources that are often present (Hilton et al., 2001).
In addition to the direct impact through interactions, parents can also shape children’s experiences and daily lives, such as by determining the amount and content of screen media such as television and video games to which a child is exposed (Maniccia et al., 2011). Excessive screen media exposure in early childhood has been examined as a possible risk factor for attention and self-regulation issues (Beyens et al., 2018; Christakis et al., 2004; Radesky et al., 2014). Healthy habits such as limiting young children’s access to screen media and monitoring the content are strongly influenced by parents’ choices (Coyne et al., 2017). The amount and content of screen time may indicate parents’ choices regarding their child’s leisure time; excessive use of screen time may also indicate less time spent playing and interacting with parents and others (Mendelsohn et al., 2011).
Understanding broad patterns of potential risk factors can help identify those that are potentially modifiable and might be addressed through prevention and intervention (Bitsko et al., this issue). The focus of the present paper is to summarize the risks for ADHD associated with parenting behaviors and the parent–child relationship as potentially modifiable factors. Family-centered interventions have been well documented to support parents and improve their ability to provide sensitive, stable, and nurturing care for their child (NASEM, 2016b). Parenting thus represents a potentially modifiable risk factor through which the likelihood of developing ADHD, or more severe ADHD symptoms, may be changed. Given prior evidence, it was expected that characteristics of parenting would emerge as associated with ADHD symptoms and diagnosis. The present paper leverages a large set of meta-analyses to examine the associations between parenting in early childhood and increased likelihood of later ADHD symptoms and diagnosis.
Methods
Procedure
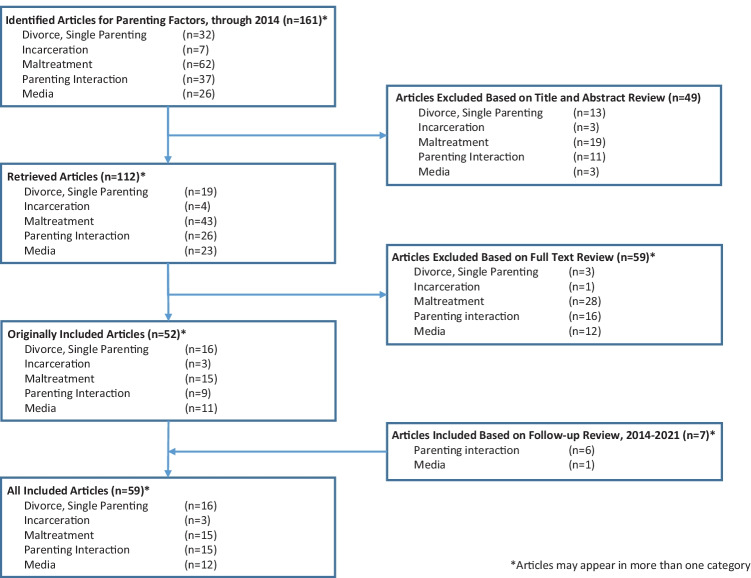
This paper is part of a series of systematic reviews and meta-analyses of potentially modifiable broad risk factors for ADHD. See Bitsko et al. (this issue) for details. Studies for the meta-analysis were identified using a comprehensive literature search of PubMed, Web of Science (WOS), and EMBASE in 2014 using both a top-down and a bottom-up approach to identify articles that captured ADHD or symptoms of ADHD and studies indicating risk factors. See the 17 for search terms. The initial review for inclusion was based on abstracts; for articles that received a full review, cited references also were checked for potential inclusion (iterative reference mining). The studies were examined for suitability using the abstract, reviewed based on methods, and clustered into conceptually related factors. Of the studies, 161 included parenting-related factors. Within these factors, clusters emerged around parental relationship status (divorce or single parenting), parental incarceration, maltreatment, parenting interaction quality, and child media exposure. Figure 1 describes the flow chart for the review and inclusion process.
Fig. 1.
Flow chart of triage process for inclusion/exclusion of articles identified for meta-analyses of parenting risk factors for attention-deficit/hyperactivity disorder (ADHD)
The final selection of articles was limited to those that involved human subjects, were published in English, and described research not duplicated in other included studies. Studies were included if they were longitudinal or retrospective; the parenting factor of note was identified prior to the assessment of ADHD. For example, studies that measured child media exposure or parenting interaction quality were only included if the measurement of ADHD symptoms or diagnosis was conducted at a later time. Reports of factors could be retrospective, for example for maltreatment or marital status. The studies also needed to have sufficient statistical details to calculate effect sizes for the specific factor in question (see Bitsko et al., this issue, for details). Statistical reporting of ADHD associations included dichotomous and continuous measurement, (e.g., dichotomous = odds ratios or categorical analyses; continuous = correlation coefficients or beta weights) which were analyzed separately. Forest plots and overall effect sizes were calculated for any ADHD outcomes, including diagnosis or symptoms (referred to as “ADHD overall”), as well as for studies assessing ADHD diagnosis, inattention, or hyperactivity/impulsivity separately, when available.
Of the general parenting factor categories, parental relationship status, maltreatment, and parenting interaction quality were further separated into individual clustered factors when sufficient data were available, i.e., a minimum of three effect sizes. Parental relationship status factors were divorce and single parenthood. Parental incarceration was a single factor that included arrest. Maltreatment-related factors were general maltreatment (not differentiated by type, could include physical and emotional abuse and neglect, sexual abuse, exposure to violence, or unspecified maltreatment) and physical abuse. Parenting interaction quality included sensitivity/warmth, intrusiveness/reactivity, and negativity/harsh discipline. Childhood media exposure was a single factor that included TV, video, and gaming. Several factors were initially targeted for analysis but not included in the final set of analyses due to fewer than three studies that met inclusion criteria, i.e., sexual abuse, neglect, foster care, parental permissiveness/inconsistent parenting, and parental involvement.
Search Strategy
The search used terms related to ADHD diagnoses, or ADHD symptoms such as inattention, hyperactivity, and impulsivity including terms more commonly used in previous decades such as attention-deficit disorder, hyperkinetic disorder, or minimal brain dysfunction (see Bitsko et al., this issue, for details). The search strings relevant to parenting were foster care, single parent, institution, advers*, maltreatment, deprivation, trauma, rejection, discipline, attachment, electronic, television, TV, video game, or screen time. See the 17 for search terms. There were 50 studies that met inclusion criteria. Because the initial search strings did not include all of the key terms that emerged as potential factors (i.e., “abuse,” “neglect,” “involvement,” “intrusive,” “permissive,” and “sensitive”), a follow-up literature search using these terms was conducted to ensure that no relevant articles were omitted, which identified two further articles that had been included in the larger systematic search but not previously identified as assessing abuse. No additional articles on the other factors emerged for inclusion. The original set of 52 papers was used to establish the parenting factors of interest that are addressed in the present study.
The search focused on selected words describing the social environment (see the 17) rather than all aspects of parenting; therefore, the included clusters are not an exhaustive representation of all possible parent–child-related factors. Parental factors that are characteristics of the parent, such as mental health and stress, or substance abuse, are reviewed elsewhere (Maher et al., under review this issue; Robinson et al., this issue).
Follow-up Literature Search
After the parenting factors of interest were established in the initial systematic review, an additional review of all literature published from 2014 until January 2021 was conducted using the same search terms (see the 17) to ensure that all relevant studies were included in the final manuscript. We identified 7 additional studies that met methodological and statistical criteria for inclusion in the final set of articles for the analyses.
Analyses
For each factor that reached or exceeded the minimum number of effect sizes (k ≥ 3), pooled analyses were conducted to calculate an overall pooled effect size for the association between the risk factor and any ADHD outcomes. Effect sizes were calculated separately for ADHD outcomes depending on whether study findings were reported as dichotomous versus continuous. More detailed analyses calculated separate pooled effect sizes for ADHD diagnosis, inattentive symptoms, or hyperactive/impulsive symptoms, whenever three or more eligible effect sizes were available. For studies that reported on male and female children separately, effect sizes were averaged, and for studies that assessed mothers and fathers on the same predictive factor, scores were averaged across both parents. When multiple levels, dosages, or severities of exposures had possible effect sizes, the most severe exposure that met other inclusion criteria (e.g., measured at least 6 months prior to the measurement of ADHD) was included, to increase the sensitivity for detecting an association if present. See Bitsko et al. (this issue), for details on the meta-analytic methods.
For each dichotomous analysis, odds ratios (OR) with 95% confidence intervals (CI) were calculated, and for continuous factors, correlation coefficients (CC) with 95% CI were calculated. To examine heterogeneity of effects, Cochran’s Q test was used to describe the variation across study estimates (DerSimonian & Laird, 1986). As in other studies in this issue, the analyses used random-effects models, using weights to account for the variation in effect size between studies (Sutton et al., 2000). Compared to a fixed-effect model, this provides a more conservative estimate of effect size (Berlin et al., 1989).
Results
The first literature search conducted in 2014 resulted in 17,734 studies and the follow-up search resulted in 11,506 additional studies. Among these studies, 161 were identified as relevant for parenting-related factors and a full review was conducted. Of the 161 studies fully reviewed, 59 studies addressed parenting-related factors and met all criteria, and thus were included in this meta-analysis. General parenting factor categories were parental relationship status (n = 16), parental incarceration (n = 3), maltreatment (n = 15), parenting interaction quality (n = 16), and child media exposure (n = 12). See Fig. 1 for the selection flow chart and Table 1 for studies included in the analyses.
Table 1.
Characteristics of studies included in meta-analyses of the association of parenting factors to child attention-deficit/hyperactivity disorder (ADHD)
| Article | Risk factorsa | Forest plot Nb | Age at outcome (years)c | Male (%) | ADHD measurement (method of assessment) | Country | Study design | Parenting factor measurement |
|---|---|---|---|---|---|---|---|---|
| Becker-Blease and Freyd (2008) | Maltreatment | 28 | 9.27 | 38–60 | ADHD symptoms (ADHDT; SNAP-IV) | USA | Community sample, recruitment through flyers in public spaces | Retroactive parent report on maltreatment (including physical abuse, sexual abuse, emotional abuse or neglect) |
| Bonde et al. (2004) | Divorce and single parenthood | 1,345 | 3.5 | 69 | Hyperactivity (Behar Scale Questionnaire) | Denmark | Birth cohort (Aarhus) | Retroactive report of family structure at outcome (divorce) |
| Breaux and Harvey (2019) | Parenting | 167 | 6 | 55.8 | ADHD symptoms (DISC) | USA | Longitudinal study of community sample of children at risk for ADHD or ODD | Observer rating of sensitive/warm parenting (play and cleanup interaction); parent self-report of intrusiveness/reactivity (overreactivity using the Parenting Scale) |
| Briscoe-Smith and Hinshaw (2006) | Maltreatment | 228 | 6–12 | 0 | Diagnosis (included CBCL, SNAP, and DISC-IV; DSM-IV) | USA | Community sample, 3 cohorts of summer camp participants, recruitment through educational and healthcare settings | Maltreatment determined from records (including physical abuse, sexual abuse, neglect, witnessing domestic violence, or combination) |
| Cheng et al. (2010) | Media | 241 | 2.5 | 50.7 | ADHD symptoms (SDQ) | Japan | Birth cohort (Japan Children’s Study), 3 study sites | Maternal report of TV exposure (≥ 4 h daily at 18 and 30 months vs < 4 h at both times)d |
| Choenni et al. (2019) | Parenting | 547 | 8 | 51.7 | ADHD symptoms (CPRS-R:S) | Netherlands | Prospective population-based cohort study (Generation R Study) | Observer rating of sensitive/warm parenting and negativity/harsh parenting (do not touch videotaped procedure, supportive presence, negative discipline) |
| Cohen et al. (2002) | Divorce and single parenthood; maltreatment | 62–80 | 15 | 35–63.6 | Diagnosis (K-SADS-E; DSM-III-R) | USA | Cohort of cases from the New York State Central Register for child abuse, randomly selected community control sample |
Parent report of family structure (marital disruption, defined as divorce or separation)e Maltreatment determined from records (physical abuse)f |
| de Paul and Arruabarrena (1995) | Maltreatment | 42 | 5–11 | n/a | Inattention (TRF) | Spain | Sample randomly selected from cases reported to child protective services, matched comparison from a stratified community sample | Maltreatment determined from records (physical abuse)g |
| Famularo et al. (1992) | Maltreatment | 96 | 5–10 | 43–44 | Diagnosis (DICA-6-R; DSM-III-R) | USA | Cases selected from court cases and hospital, comparison from hospital sample | Maltreatment determined from records (abuse or neglect) |
| Fitzpatrick et al. (2012) | Media; parenting | 1,786 | 8.08 | n/a | Inattention (teacher SBQ) | Canada | Birth cohort (Quebec Longitudinal Study of Child Development) |
Parent report of any exposure to violent film/TV content Observer rating of maternal negativity/harsh parenting (hostility using the HOME) |
| Foster and Watkins (2010) | Media | 1,033 | 7 | n/a | Inattention (BPI) | USA | Cohort from the National Longitudinal Survey of Youth | Parent report of TV exposure (> 7 h vs 0 h daily)h |
| Gabel and Shindledecker (1993) | Parental incarceration | 31 | 5.5–12.5 | 70.3 | Inattention (TRF) | USA | Cohort of clinical clients of a day hospital | Parent or caregiver report of prior incarceration of either parent |
| Geller et al. (2012) | Parental incarceration | 2,695 | 5 | 52.1 | Inattention (CBCL) | USA | Birth cohort (Fragile Families) | Father self-report, mother report, and disposition data of parent incarceration |
| Giannotta and Rydell (2017) | Parenting | 596 | 15 | 50 | ADHD symptoms (ADHD-RS) | Sweden | Population-based, regional longitudinal cohort study | Parental self-report of sensitivity/warmth and negativity/harsh discipline (Parental Environment Questionnaire) |
| Graziano et al. (2011) | Parenting | 357 | 2–4.5 | 53.4 | Sustained attention (lab video) | USA | Longitudinal sample selected at risk for behavior problems, 3 cohorts of 2-year-old children from community samples screened for risk | Observer rating of Intrusive/reactive and sensitive/warm parenting (warmth, overcontrol/intrusiveness using the Early Parenting Coding System) |
| Haj-Yahia and Abdo-Kaloti (2008) | Maltreatment | 1,185 | 16.58 | 49.8 | Inattention (YSR) | Palestine | Convenience sample, 3 classes randomly selected from 13 high schools | Maltreatment based on child self-report using Conflict Tactics Scale (aggregate of physical violence by father and mother) |
| Hjern et al. (2010) | Divorce and single parenthood | 1,162,524 | 6–19 | 51.3 | ADHD medication purchase | Sweden | Birth cohort from National Register 1987–2000, excluding foreign-born parents | Family structure based on register information (lone parenting) |
| Hurtig et al. (2005) | Divorce and single parenthood | 4,634 | 15 | 47.9 | ADHD symptoms (SWAN) | Finland | Birth cohort from two provinces | Parent self-report of family structure (divorced or widowed) (always single parent)i |
| Jacobvitz and Sroufe (1987) | Parenting | 68 | 6 | 70.6 | Hyperactivity (CBCL) | USA | Case/control sample of hyperactive with matched comparison selected from a prospective longitudinal sample of primiparous mothers attending prenatal clinics | Observer rating of intrusive/reactive parenting (overstimulation during structured play interaction) |
| Johnson et al. (2007) | Media | 678 | 14–22 | 50 | Inattention (DISC) | USA | Community-based prospective longitudinal sample of adolescents (Children in the Community Study) | Parent report of TV exposure (> 1 h daily)j |
| Kashala et al. (2005) | Divorce and single parenthood | 185 | 8.4 | 45 | ADHD symptoms (SDQ) | Democratic Republic of Congo | School-based sample, Teacher SDQ plus DBD high screened hyperactive/inattentive and matched control (nested case/control) | Parent report of family structure (divorced) (single parent) |
| Kelly et al. (2001) | Divorce and single parenthood | 5,181 | 4–15 | 50 | Hyperactivity (SDQ) | England | Representative survey, Health Survey for England | Parent reported family structure (lone parenting) |
| Keown (2012) | Parenting | 81 | 7 | 100 | ADHD symptoms (ADHD-RS) | New Zealand | Prospective longitudinal community sample, case/control on hyperactivity using PACS |
Observer rating of intrusive/reactive, sensitive/warm parenting by both parents Intrusiveness and sensitivity using Early Head Start 3-bag coding scheme |
| Kerr and Michalski (2007) | Divorce and single parenthood | 1,920 | 4–11 | n/a | ADHD symptoms (interview) | Canada | Cohort of children age 4–5 in 1994 (Canadian National Longitudinal Survey of Children and Youth) | Parent report of family structure (separation or divorce)k |
| Kim et al. (2009) | Divorce and single parenthood | 2,419 | 10 | 48.6 | Diagnosis (DISC-IV) | Korea | School-based sample (Seoul Child and Adolescent Mental Health Survey) | Parent report of family structure (separation or divorce) |
| King et al. (2011) | Maltreatment | 600 | 10–18 | 63.1 | Diagnosis (DISC-III-R/DISC-IV) | USA | Random sample from juvenile temporary detention center | Self-report and record review of maltreatment (presence/absence of combined severe physical and sexual abuse)l |
| Kočovská et al. (2012) | Maltreatment | 66 | 9 | 43.1–51.5 | Diagnosis (clinician, DAWBA) | UK | Sample recruited from adoption charity selected for indiscriminately friendly behavior and history of maltreatment, and matched controls | Maltreatment recorded from adoption records (includes physical abuse, sexual abuse, physical neglect, emotional neglect) |
| Landhuis et al. (2007) | Media | 980 | 3–15 | 52 | Inattention (Quay-Peterson RBPC/Rutter Scale/Child DISC) | New Zealand | Birth cohort (Dunedin Multidisciplinary Health and Development Study) | Parent of TV exposure (hours of daily exposure) |
| Larsson et al. (2011) | Divorce and single parenthood | 2,160 | 8–20 | 49 | Hyperactivity and Inattention Symptoms Checklistm | Sweden | Birth cohort (Twin study of Child and Adolescent Development) | Parent report of family structure (divorce; comparison included single parent, married, widowed) |
| Lifford et al. (2008) | Parenting | 194 | 11–13 | 45.8 | ADHD symptoms (CBCL) | UK | Longitudinal community study | Child report of sensitive/warm parenting (acceptance/rejection using the Child’s Report of Parental Behavior Inventory) |
| Lifford et al. (2009) | Parenting | 282 | 11–14 | 49.6 | ADHD symptoms (CBCL) | UK | Longitudinal community study | Child report of negativity/harsh parenting (hostility using the Iowa Youth Family Project Hostility scale) |
| Liu et al. (2000) | Divorce and single parenthood | 174 | 10.3 | 51.7 | Inattention (CBCL, TRF) | China | Cases and controls (divorced and not divorced) selected from a representative community sample | Parent report of family structure (divorce) |
| Meysamie et al. (2011) | Divorce and single parenthood | 1,403 | 3–6 | 51.8 | ADHD symptoms (parent and teacher BRPC) | Iran | School-based sample from randomly selected kindergartens | Parent report of family structure (single parenting) |
| Miller et al. (2019) | Parenting | 241 | 9 | 46 | ADHD symptoms (SNAP-IV) | USA | Longitudinal study on temperament, oversampled on infant reactivity | Observer rating of sensitivity/warmth (Ainsworth’s Maternal Care Behavior rating scales) |
| Mimouni-Bloch et al. (2013) | Divorce and single parenthood | 107 | 6–12 | 52.9–73.2 | Diagnosis (medical records) | Israel | Retrospective matched study, medical center, case and control (ADHD) | Parent report of family structure (divorce) |
| Mistry et al. (2007) | Media | 2,306 | 5.5 | 49 | Inattention (CBCL) | USA | Prospective longitudinal study (Healthy Steps for Young Children) | Parent report of TV exposure (> 2 vs ≤ 2 h daily) |
| Morrell and Murray (2003) | Parenting | 59 | 5–8 | 52.5 | Hyperactivity (RS) | UK | Case control study (depression) from representative sample, birth cohort | Observer rating of maternal negativity/harsh and sensitive/warm parenting (hostility and positive composite using the HOME) |
| Nolin and Ethier (2007) | Maltreatment | 109 | 6–12 | 55.7 | Inattention (Visual Attention Test – NEPSY) | Canada | Case control study (maltreated vs matched control) | Record review (neglect with physical abuse, comparison)n |
| Obel et al. (2004) | Media | 244 | 3.5–12 | n/a | Probable diagnosis (Rutter Scale, CBCL, SDQ) | Denmark | Longitudinal study of birth cohort from hospital | Parent report of TV exposure (> 2 vs < ½ h daily)o |
| Parkes et al. (2013) | Media | 10,500 | 5–7 | 48.9 | ADHD symptoms (SDQ) | UK | Prospective birth cohort study (UK millennium) | Parent report of TV/video/DVD and electronic games exposure (> 3 vs < 1 h daily)p |
| Pauli-Pott et al. (2018) | Parenting | 120 | 5 | 57 | ADHD symptoms (FBB-ADHS-V and PrePacs composite) | Germany | Longitudinal study of preschooler, oversampled on ADHD risk | Observer rating of sensitivity/warmth (responsiveness scale on the Mannheim Rating Scale for the Assessment of Mother–Child Interaction) |
| Pinto et al. (2006) | Parenting | 104 | 6–8 | n/a | ADHD symptoms (ADHD-RS, mother and teacher) | UK | Community-based case control (stillbirth and matched control) | Observer rating of sensitive/warm parenting (disorganization of attachment scale based on strange situation behavior) |
| Poulain et al. (2018) | Media | 527 | 3–7 | 52 | ADHD symptoms (SDQ) | Germany | Longitudinal childhood cohort study (LIFE Child study) | Parent and child report of TV, videogame, and mobile phone exposure (hours of daily exposure) |
| Robinson et al. (2012) | Maltreatment | 102 | 7.14 | 44.3–53.1 | Inattention (CBCL) | USA | Cohort of maltreated children taken into state custody and matched controls | Record review of maltreatment status (includes physical abuse, sexual abuse, and neglect) |
| Rodriguez et al. (2011) | Divorce and single parenthood | 805 | 7–9 | 51.7 | Hyperactivity (SDQ) | Brazil | Birth cohort, stratified random sampling based on birth weight | Parental report of family structure (single parenting)q |
| Rogosch et al. (2011) | Maltreatment | 247 | 9.42 | 52.2 | Inattention (TRF) | USA | Community-based case control (maltreated and SES matched comparison) | Maltreatment status coded from records (includes neglect, emotional maltreatment, physical abuse, and sexual abuse) |
| Rydell (2010) | Divorce and single parenthood | 1,124 | 10.2 | 52 | ADHD symptoms (ADHD-RS) | Sweden | Population-based random sample of age cohort | Parental report of family structure (single parenting)r |
| Schachar and Wachsmuth (1991) | Divorce and single parenthood | 63 | 7–11 | 100 | Diagnosis (Teacher Rutter Scale, CATRSB, SNAP; parent and child interview) | Canada | Clinic referred case–control study behavior problems and community comparison (boys) | Parental report of family structure (divorce)s |
| Sesar et al. (2008) | Maltreatment | 458 | 15–20 | 39 | ADHD symptoms (YSR) | Bosnia and Herzegovina | Population-based sample of high school students from a specific canton | Self-report of maltreatment based on Child Maltreatment Questionnaire (includes emotional abuse, physical abuse, sexual abuse, neglect, and witnessing family violence) |
| Simmel et al. (2001) | Maltreatment | 808 | 10 (5–18) | 50.7 | ADHD symptoms (BPI, IOWA Connors) | USA | Population-based cohort of adoptive families (California Long-Range Adoption Study) | Parent report of maltreatment based on information by birth parent or social worker (includes physical/sexual abuse and neglect) |
| Stadelmann et al. (2010) | Divorce and single parenthood | 187 | 5.27–6.23 | 59.4 | Hyperactivity (SDQ) | Switzerland | Community sample of Kindergarten students plus participants of longitudinal sample recruited prenatally plus sample of children referred for behavior problems | Parent report of family structure (separation) |
| Stevens and Muslow (2006) | Media | 2,500 | Kindergarten | n/a | ADHD symptoms (SRS) | USA | Random sample from the Early Childhood Longitudinal Study, Kindergarten Class 1998–1999 | Parent report of TV or video exposure (hours daily) |
| Stright and Neitzel (2003) | Parenting | 52 | 8.6 | 55.8–92.3 | Inattention (TRF; behavior observation) | USA | Community sample | Observer rating of negativity/hostile parenting (maternal and paternal rejection using the System for Coding Interaction and Family Functioning) |
| Swing et al. (2010) | Media | 1,323 | 6–12 | 47 | Inattention/impulsivity (ASRS; BSCS, BIS-11) | USA | Sample from obesity prevention study | Parent and child report of TV and videogame exposure (combined average weekly exposure) |
| Thompson and Tabone (2010) | Maltreatment | 242 | 4 | 44.3–48.7 | Inattention (CBCL) | USA | Longitudinal multisite study of high-risk infants | Maltreatment based on case record review (includes physical abuse, sexual abuse, and neglect) |
| Umemura et al. (2015) | Parenting | 85 | 7 | n/a | ADHD symptoms (CBCL and TRF composite) | USA | Longitudinal pregnancy follow-up study | Observer rating of and negativity/harsh discipline (Parental Coping with Children’s Negative Emotions Questionnaire) |
| Wolfe and Mosk (1983) | Maltreatment | 70 | 6–16 | 45.7–51.4 | Hyperactivity (CBP) | Canada | Case control study of abused agency cases, non-abused agency cases, and community groups | Maltreatment based on case record review or on observation (includes physical aggression and coercion) |
| Zimmerman and Christakis (2007) | Media | 391 | 5–10 | n/a | Inattention (BPI) | USA | Longitudinal survey, nationally representative, Panel Survey of Income Dynamics | Parent report (time diary) of violent media exposure (average hours daily) |
| Ziv et al. (2010) | Parental incarceration | 1,347 | n/a | 50–51.1 | Hyperactivity (BPI) | USA | Nationally representative survey (Head Start Family and Child Experiences Survey) | Parent incarceration based on parent report of arrest or charges against household member including parent |
ADHDT Attention Deficit Hyperactivity Disorder Test, ADHD-RS ADHD Rating Scale–IV, ASRS Adult ADHD Self Report, BSCS Brief Self-Control Scale, BRPC Behavior Rating for the Preschool Child, BIS-11 Barratt Self-Control Scale, BPI Behavior Problems Inventory, CATRSB Conners Abbreviated Teacher Rating Scale, CBCL Child Behavior Checklist, CBP Child Behavior Profile, CPRS-R:S Conners’ Parent Rating Scale Revised, DAWBA Development and Well-Being Assessment, DBD Disruptive Behavior Disorder Rating Scale, DICA Diagnostic Interview for Children and Adolescents, DISC Diagnostic Interview Schedule for Children, DSM-III-R Diagnostic and Statistical Manual of Mental Disorders, 3rd edition, Text Revision, DSM-IV Diagnostic and Statistical Manual of Mental Disorders, 4th edition, FBB-ADHS-V preschool version of the ADHD rating scale, HOME Home Observation for Measurement of the Environment, K-SADS-E Kiddie Schedule for Affective Disorders and Schizophrenia for School-Age Children, epidemiological version, NEPSY developmental neuropsychological assessment, PACS, Parental Account of Children’s Symptoms, PrePACS Parental Account of Children’s Symptoms, preschool version, RBPC Revised Behavior Problem Checklist, SBQ Social Behavior Questionnaire, SDQ Strengths and Difficulties Questionnaire, SNAP Swanson, Nolan, and Pelham, SRS Social Rating Scale, SWAN Strengths and Weaknesses of ADHD Symptoms and Normal Behaviors Questionnaire, TRF Teacher Report Form, YSR Youth Self Report
aEffect size information was extracted whenever possible, regardless of whether the risk factor was the main variable of interest in a study or was simply included as a covariate or statistical control
b N may differ across forest plots for studies with multiple effect sizes
cMean ages are reported if available; otherwise, the range is reported
dChildren who watched ≥ 4 h at one time and < 4 h at the other were not included in the analyses
eDivorce analyses excluded all cases with maltreatment
fMaltreatment analyses excluded all cases with marital disruption
gCases of neglect were not included in the analyses
hChildren with between > 0 and < 7 h were not included in the analyses
iThe sample also included formerly divorced/widowed and now reconstructed families who were not included in the analyses
jChildren with 1–3 h and > 3 h were combined
kThis study also addressed single parenting (lone parenting) but there were insufficient numbers of studies for continuous outcomes, so lone parenting and step families were not included in the analyses
lCases with moderate or severe physical abuse without sexual abuse were not included in the analyses
mJoint trajectory across ages 8–9, 13–14, and 16–17 years, DSM-IV-based symptom scale
nNeglect only cases were not included in the analyses
oChildren who watched between ½ and 2 h were not included in the analyses
pChildren who watched between 1 and 3 h were not included in the analyses
qThe sample also included cohabiting couples who were not included in the analysis. Comparisons were between single and married
rThe sample also included parent and stepparent families who were not included in the analyses. Comparisons were between single and married/two biological parents
sThe sample also included children with learning disability, emotional disability, and conduct disorder who were not included in the analyses. Comparisons were between children with ADHD, alone and combined with conduct disorder, and those without diagnoses
Relation of Risk Factors to ADHD Outcomes
Across all analyses, these parenting factors were significantly associated with ADHD outcomes, including all factors related to parental relationship status, parental incarceration, maltreatment, parenting interaction, and child media exposure. See Table 2 for the results of analyses. Forest plots are included in the Supplemental material.
Table 2.
Results of the systematic review and meta-analysis of studies examining attention-deficit/hyperactivity disorder (ADHD) outcomes for selected parenting risk factors
| Risk factor | Outcome measure | ADHD overall | ADHD diagnosis only | Inattention | Hyperactivity/impulsivity | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Sample size (kxx) | Pooled effect sizexxi (95% CI) | Sample size (k) | Pooled effect size2 (95% CI) | Sample size (k) | Pooled effect size2 (95% CI) | Sample size (k) | Pooled effect size2 (95% CI) | |||
| Parental relationship status | Divorce | Dichotomous | 11,929 (9) |
2.93 (1.54, 5.55) + |
2,651 (4) |
4.84 (2.22, 10.56) |
||||
| Continuous | 3,405 (4) |
0.11 (0.04, 0.18) + |
||||||||
| Single parenting | Dichotomous | 1,174,547 (5) |
1.61 (1.17, 2.22) |
|||||||
| Parental incarceration | Incarceration | Continuous | 4,073 (3) |
0.10 (0.06, 0.14) |
||||||
| Maltreatment | General maltreatmentxxii | Dichotomous | 1,878 (6) |
7.27 (4.23, 12.49) |
1,070 (5) |
7.63 (3.95; 14.75) |
||||
| Continuous | 2,483 (9) |
0.30 (0.18, 0.42) + |
1,955 (7) |
0.26 (0.12, 0.40) + |
||||||
| Physical abuse | Continuous | 1,406 (4) |
0.39 (0.31, 0.47) |
|||||||
| Parenting interaction quality | Sensitivity/warmth | Continuous | 2,475 (10) |
− 0.16 (− 0.20; − 0.12) |
1,379 (5) |
− 0.17 (− 0.24; − 0.10) |
1,054 (5) |
− 0.14 (− 0.21; − 0.07) |
||
| Intrusive/reactive | Continuous | 682 (4) |
0.17 (0.08; 0.26) |
|||||||
| Negativity/harsh discipline | Continuous | 3,407 (7) |
0.19 (0.06; 0.32) + |
|||||||
| Child media exposure | Media exposure | Dichotomous | 3,853 (6) |
1.94 (1.57; 2.30) |
2,049 (3) |
1.45 (0.84, 2.50) |
||||
| Continuous | 22,235 (9) |
0.07 (0.02; 0.12) + |
6,395 (4) |
0.12 (0.04, 0.20) + |
||||||
xxK = number of studies included
xxiPooled effect size is calculated as odds ratio for dichotomous analyses and as a correlation coefficient for continuous analyses. All effect sizes were considered statistically significant at p < .05. + indicates tests of heterogeneity statistically significant at p < 0.05
xxiiIncluded physical and emotional abuse, neglect, sexual abuse, or unspecified maltreatment
Parental Relationship Status
Divorce was significantly associated with risk for ADHD overall for both dichotomous (OR = 2.93; 95% CI: 1.54, 5.55; k = 9) and continuous (CC = 0.11; 95% CI: 0.04, 0.18; k = 4) effect sizes. These effect sizes showed significant heterogeneity for dichotomous (Q(8) = 14.32, p = 0.07) as well as continuous ADHD overall (Q(3) = 9.48, p = 0.02). There were also sufficient studies with dichotomous effect sizes (k = 4) for an analysis of divorce and ADHD diagnosis. Children of divorced parents had a significantly increased risk of having an ADHD diagnosis later (OR = 4.84; 95% CI: 2.22, 10.56), and this test was not significantly heterogeneous. For single parenting, only dichotomous effect sizes on ADHD overall had enough studies for analysis (k = 5). The test of heterogeneity was not significant. Single parenting was significantly associated with increased risk of later ADHD in children (OR = 1.61; 95% CI: 1.17, 2.22), and heterogeneity was not significant. There were insufficient studies to separately examine any effects on inattention or hyperactivity.
Parental Incarceration
For research on parental incarceration, only overall continuous effect sizes had enough studies for analysis (k = 3). Parental incarceration significantly predicted later ADHD overall (CC = 0.10; 95% CI: 0.06, 0.14). The test for heterogeneity was not significant.
Maltreatment
For general maltreatment, the association with ADHD overall was positive for both dichotomous (OR = 7.27; 95% CI: 4.23, 12.49; k = 6) and continuous (CC = 0.30; 95% CI: 0.18, 0.42; k = 9) effect sizes. Tests of heterogeneity for general maltreatment were significant for continuous ADHD overall outcomes (Q(8) = 52.82, p < 0.001) but not for dichotomous outcomes. General maltreatment was also significantly associated with ADHD diagnosis specifically, using dichotomous effect sizes (OR = 7.63; 95% CI: 3.95, 14.75; k = 5). There were sufficient studies (k = 7) to investigate the association of general maltreatment and inattentive symptoms using continuous effect sizes; children who experienced general maltreatment were significantly more likely to show inattentive symptoms (CC = 0.26; 95% CI: 0.12, 0.40), which had significant heterogeneity (Q(6) = 36.54, p < 0.001). When investigating specific types of maltreatment, the only type that had sufficient studies for analysis was physical abuse using continuous ADHD outcomes overall (k = 4). Experiencing physical abuse was significantly associated with continuous ADHD outcomes overall (CC = 0.39; 95% CI: 0.31, 0.47). The test for heterogeneity was not significant.
Parenting Interaction Quality
Among possible factors describing quality of parent–child interaction, three emerged as having sufficient studies to estimate pooled effect sizes for continuous ADHD overall. Pooled data from a cluster of 10 studies measuring sensitivity/warmth showed a negative correlation with continuous ADHD outcomes overall (CC = − 0.16; 95% CI: − 0.20, − 0.12) and data from 4 studies investigating intrusive/reactive interaction behavior showed a positive correlation with continuous ADHD outcomes overall (CC = 0.17; 95% CI: 0.08, 0.26). Neither of the tests for heterogeneity was significant. Data from the 7 studies investigating negativity/harsh discipline showed a positive association with continuous ADHD outcomes overall (CC = 0.19; 95% CI: 0.06, 0.32). For this factor, the test of heterogeneity showed significant heterogeneity (Q(6) = 57.21, p < 0.001). As seen in the forest plot (Supplemental Fig. S15), a single study (Morrell & Murray, 2003) showed a correlation that was negative in direction while other effect sizes were all positive. Upon inspection, this correlation coefficient (− 0.232) was with a factor described as hostility, which was identical to the coefficient listed for positivity, coded at the same time from the same observation. No reverse coding was mentioned so the possibility of a reporting error could not be excluded. We re-calculated the effect size and heterogeneity for the factor with the correlation coefficient from Morrell and Murray (2003) excluded, and still found significant heterogeneity among the remaining effect sizes.
Of these three parenting interaction factors, only sensitivity/warmth had sufficient studies to examine specific symptoms using continuous outcome scales (inattention and hyperactivity k = 5); sensitivity/warmth was inversely correlated with inattention symptoms (CC = − 0.17; 95% CI: − 0.24, − 0.10) as well as hyperactivity (CC = − 0.14, 95% CI: − 0.21, − 0.07). Neither set of pooled correlation coefficients was significantly heterogeneous.
Child Media Exposure
For child media exposure, there was a positive association with overall ADHD for both dichotomous outcomes (OR = 1.94; 95% CI: 1.57, 2.30; k = 6) and continuous outcomes (CC = 0.07; 95% CI: 0.02, 0.12; k = 9); children with more media exposure were more likely to have ADHD. Pooled effect sizes were significantly heterogeneous for the continuous overall ADHD outcomes (Q(8) = 83.25, p < 0.001) but not for the dichotomous overall ADHD outcomes. There were also sufficient studies to examine the association of child media exposure and inattention using dichotomous (k = 3) and continuous effect sizes (k = 4), and each association was positive and statistically significant (OR = 1.45; 95% CI: 0.84, 2.50; and CC = 0.12; 95% CI: 0.04, 0.20; respectively). For inattention, pooled estimates for continuous (Q(3) = 27.74, p < 0.001) but not dichotomous effect sizes showed significant heterogeneity.
Discussion
The results of the meta-analysis showed a pattern of statistically significant associations between multiple factors related to parenting and later ADHD symptoms and diagnosis. Poorer quality of interaction, maltreatment, divorce and single parenting, and higher child media exposure were statistically significantly associated with an increased likelihood of later ADHD symptoms and diagnosis, and thus emerged as potential risk factors. These findings suggest opportunities for potential prevention of ADHD symptoms through addressing parental risk factors. This study adds to the literature by suggesting that the focus of public health efforts that address outcomes such as maltreatment and positive parenting can be expanded to address these factors as prevention for clinical disorders such as ADHD. However, the results also point to gaps in knowledge, with limited numbers of high-quality studies available to examine the associations more thoroughly.
Overall, maltreatment was most strongly associated with ADHD diagnosis and symptoms; based on the odds ratios, children who experienced maltreatment were about 7 times as likely to have ADHD symptoms or diagnoses than the comparison groups. Based on Cohen’s method to estimate variance explained, general maltreatment explained about 9% and physical abuse explained about 15% of the variance in continuous ADHD measures, thus indicating a sizeable association of each type of maltreatment on children’s likelihood of developing ADHD symptoms (Chen et al., 2010; Cohen, 1988). Children whose parents experienced separation or divorce were about 3 times as likely to have ADHD overall, including diagnosis or symptoms, based on the odds ratio, showing moderate pooled effects (Chen et al., 2010). Other factors showed smaller pooled effect sizes, indicating that these factors, while statistically significantly associated with the ADHD outcome, may have a smaller impact, or may impact a subset of children who are particularly vulnerable to the risks.
The review indicates that despite decades of research, there are still significant gaps, due to limited high-quality studies that contained the necessary data for inclusion in this meta-analysis. Most factors included in these analyses could only be examined for overall ADHD outcomes; few factors had enough studies that met inclusion criteria to examine associations with inattention or hyperactivity/impulsivity separately. For inattention, general maltreatment, higher child media exposure, and lower sensitivity/warmth during interactions emerged being statistically significantly associated. For hyperactivity, only sensitivity/warmth could be evaluated and was inversely associated. The analyses of specific outcomes showed similar magnitude for pooled effects as for the overall ADHD analyses, thus not pointing to differential associations of these factors on specific symptoms.
The data support associations between these parenting and family environment factors and child ADHD. There are multiple possible pathways by which they are related, such as directly through the parent–child relationship, indirectly through factors that parents may influence, or through common risk factors that affect both the child and the parent, including genetic factors. These possible pathways are likely to each play a role and thus present multiple opportunities for prevention and intervention (Faraone et al., 2021).
As established in previous research, parenting can have a strong influence on child development (NASEM, 2016b). The quality of the parent–child relationship and the cumulative effect of parent–child interactions has a measurable influence not just on observable behavior but also on underlying cognitive and emotional processes, including those that underly ADHD (Pallini et al., 2019). Adverse parenting such as insensitivity, lack of responsiveness, or maltreatment can have a negative effect on brain development, whereas sensitivity and supportive parenting particularly in early childhood is significantly related to more optimal structural brain development (Belsky & de Haan, 2011; Kok et al., 2015). Such impact on brain development in turn can influence the development of ADHD symptoms (Humphreys & Zeanah, 2015; Jimenez et al., 2017; Strathearn et al., 2020) and also of executive function skills, which play a major role in ADHD (Hughes & Devine, 2017; Pallini et al., 2019).
Parents and children also may have shared risk for ADHD, adding to the intergenerational transmission of ADHD, and thus pointing to the family needing support as a unit, rather than the child with a diagnosis alone. Heritability of ADHD has been well documented, showing that genes can contribute to the probability of developing ADHD (Faraone & Larsson, 2019; Faraone & Mick, 2010; Freitag & Retz, 2010). Parents who share the genetic vulnerability and themselves have ADHD symptoms such as inattention or impulsivity may make different reproductive choices such as having children at a younger age or having more children (Ni et al., 2019), may have more difficulty providing resources for their children (Rowland et al., 2018), and may struggle more than other parents with creating a predictable and consistently supportive environment for their child (Storebø et al., 2013). Some parents with a history of ADHD symptoms may have experienced adversity in their own childhood, and may have lacked positive role models, which increases the risk of ADHD symptoms in their offspring (McDonald et al., 2019; Park et al., 2017; Radesky et al., 2014; Roberts et al., 2018). Parents of children with ADHD may be at a higher risk of mental disorders, which further contributes to the likelihood of children developing ADHD (Robinson et al., this issue). Thus, the genetic vulnerability towards ADHD that parents may share with their child is also associated with the parenting factors that may contribute to the child’s symptoms of ADHD. Moreover, animal and emerging human research suggests parents’ own trauma history can result in epigenetic changes associated with stress reactivity and regulation which then can be transmitted to their offspring (Hays-Grudo & Morris, 2020) pointing to additional possible pathways of influence and of opportunities for intervention.
The present analysis included parenting factors that preceded the assessment of ADHD symptoms or the diagnosis of ADHD, but possible causal pathways by which parents contribute to ADHD symptoms are likely to be one part of a much larger, complex pattern of possible influences (Faraone et al., 2021). Early signs of ADHD may have already been present in the child before ADHD outcomes were measured. As parenting can influence child development, children can also influence parenting (Darling Rasmussen et al., 2019; Johnston et al., 2012). Children who are predisposed to develop ADHD may show early neuro-atypical characteristics such as lacking attention to social cues, acting impulsively, and not attending to consequences of actions that may present challenges for parents (Deault, 2010; Johnston et al., 2012) and affect the quality of the parent–child relationship (Darling Rasmussen et al., 2019). ADHD may impact how children perceive and react differently to their parents’ behavior and thus influence parenting styles (Molina & Musich, 2016), particularly given the increased likelihood of co-occurring behavior disorders (Deault, 2010).
Moreover, ADHD is associated with several child physical health risks (Bitsko et al., this issue; So et al., under review this issue). Combined with an elevated likelihood for environmental risks (Dimitrov et al., under review this issue) and parental risks such as poor mental health and substance abuse (Maher et al., under review this issue; Robinson et al., this issue), these risk factors may place additional demands on the subset of parents who experience risks themselves (Deault, 2010). Thus, by the time the child is diagnosed with ADHD (typically early school age), a range of parental and child factors related to ADHD may have jointly impacted the child’s developmental trajectory.
In addition, it is also likely that both the parenting factors and ADHD are affected by other factors and potentially functioning as flags for underlying risks. For example, divorced and single parents can fully support their child’s healthy development, but among groups of children, those whose parents are divorced may have higher odds of experiencing family conflict, and single parenting has higher odds of economic disadvantage (Aizer, 2017; Bramlett & Mosher, 2002). Similarly, parental incarceration is more prevalent in households with lower income and lack of resources (Geller et al., 2009). Adverse experiences may compound risk, such as socioeconomic risks coupled with increased difficulties with relationships and decreased ability to cope with adversity, as well as increased chance of exposing the child to violence along with poor parenting and mental health issues, pointing to a cluster of disadvantages across the factors measured in this paper (Fredland et al., 2018; Roberts et al., 2018; Schickedanz et al., 2018). Nationally, early indicators of self-regulation are associated with social determinants of health such as living in financially and socially disadvantaged families and communities, and experiencing family adversity (Claussen et al., 2021). Such lack of resources and support, in turn, may make life more challenging, increase the likelihood of depression and anxiety, and decrease the parents’ ability to help their child manage their behavior (Deault, 2010; Johnston et al., 2012; Robinson et al., this issue). Lack of resources may serve as a marker for communities that are unable to provide necessary supports, which may compound parenting challenges (Midouhas et al., 2014).
It may also be possible that parenting factors influence other conditions that are commonly co-occurring with ADHD and that the presence of these conditions can make ADHD symptoms worse. For example, there is stronger evidence for media exposure as a risk for obesity and depression than for ADHD symptoms (Stiglic & Viner, 2019). Given co-occurrence of obesity and depression with ADHD (Danielson et al., 2018; Li et al., 2020), it is unclear whether the association of media exposure and ADHD would remain if controlling for these co-occurring outcomes, but presence of multiple conditions may warrant additional need for support.
Strengths and Limitations
The meta-analysis had multiple strengths. It specifically focused on studies where the exposure preceded the ADHD outcome. We also included ADHD symptoms, rather than relying only on existing diagnosis (see Table 1). Finally, the studies included large datasets as well as smaller samples, included males and females, and drew on data from multiple countries, broadening the scope of inquiry.
There were also several limitations. As discussed, causal pathways cannot be determined from any of the included studies in our meta-analysis. We observed significant heterogeneity for multiple potential risk factors examined, suggesting variability in the magnitude or direction of estimates from individual studies. This finding may not be surprising, as the studies were from different countries, employed different study designs, and used different measurement approaches for risk factors and ADHD outcomes. Therefore, factors had a common conceptual definition but were assessed in different ways. For example, media exposure included studies that examined exposure to TV (Cheng et al., 2010; Landhuis et al., 2007; Mistry et al., 2007) and TV and gaming (Poulain et al., 2018; Stevens & Mulsow, 2006; Swing et al., 2010), as well as exposure to violent TV content (Fitzpatrick et al., 2012) or violent TV and gaming (Parkes et al., 2013). Given that content, pacing, and duration of media exposure may well have differential effects on symptoms (Beyens et al., 2018), such variability may have contributed to heterogeneity. Bias in assessment may also affect heterogeneity; while qualitative constructs such as sensitivity and responsiveness apply across cultures (Claussen & Crittenden, 2000), the behaviors used to measure sensitivity or responsiveness may be impacted by racial, ethnic, and cultural bias (Guerrero et al., 2021). Furthermore, studies used different types of data sources, for example, maltreatment included case records and assessed reported maltreatment, but also utilized parent report (Becker-Blease & Freyd, 2008; Simmel et al., 2001), child self-report (Haj-Yahia & Abdo-Kaloti, 2008; King et al., 2011; Sesar et al., 2008), or observation (Wolfe & Mosk, 1983). The studies of maltreatment varied in whether they focused on physical abuse, neglect, sexual abuse, psychological maltreatment, or combinations thereof, even though these may have different effects on children’s development (Strathearn et al., 2020) thus impacting heterogeneity.
Variability in the measured ADHD outcomes may also impact the heterogeneity. Studies included parent, teachers, case record review, clinical diagnosis, and direct child observation. Generally, ADHD symptoms vary among children and present differently across context, different observers may witness dissimilar behaviors, and single assessments may not capture all facets. For case records, the validity of the original diagnosis often cannot easily be ascertained, and parents with poor parenting skills may not be reliable observers of behavior concerns (Bennett et al., 2006; Lau et al., 2006), thus adding a potential source of error or bias. Thus, while the overall analyses showed statistically significant associations that were generally consistent in direction (positive or negative), such heterogeneity limits the ability to interpret the accuracy of the magnitude of the pooled estimates. For multiple factors such as divorce, maltreatment, negativity/harsh punishment, and media exposure, several of the presented pooled effect sizes need to be interpreted with caution.
Co-occurring disorders were not assessed systematically or in detail across studies. Thus, it is unclear whether symptoms of ADHD may have been caused by other conditions with similar symptoms, such as difficulties with attention and regulation due to learning disorders or sleep disorders (Wolraich et al., 2019). Trauma in specific may be likely to occur with maltreatment and unsupportive parenting, and careful clinical diagnosis beyond use of rating scales may be needed to differentiate symptoms of trauma from ADHD (Wolraich et al., 2019; American Psychiatric Association, 2013). Moreover, factors such as parental mental disorders were also not consistently taken into considerations in these studies.
The diversity of studies drawing from samples from different countries and using different study design also represents a limitation. With samples ranging from population samples, community samples, convenience samples, to clinic samples, it is not possible to adjust for selection bias and other confounding variables.
We were also not able to assess several parenting factors of interest due to fewer than three effect sizes from studies that met inclusion criteria. For example, physical neglect or sexual abuse may have a different impact on children than physical abuse, but insufficient data were present to examine those factors. The available literature also did not allow a thorough examination of ADHD diagnosis, hyperactivity, or impulsivity as separate from the overall outcome for many parenting factors of interest. Other factors relevant to parenting may have also been missed by the search strategy given that it was focused on a broad range of factors rather than focused on all possible relevant search terms related to parenting (Bitsko et al., this issue).
Gaps and Future Directions
In addition to the reported findings, this meta-analysis revealed gaps in the literature on parenting factors and ADHD. Between 2014 and early 2021, only 7 studies had sufficient details to meet the criteria for inclusion in this paper. Important factors such as the interaction of child sex, socioeconomic, and parenting factors on ADHD outcomes could not be examined. Future studies can examine which factors predict hyperactive/impulsive versus inattentive symptoms and the impact of different measures of ADHD (e.g., clinical, observational, parent or teacher report). More thorough research could contribute to understanding which among the possible causal pathways may play stronger roles, and for which subsets of parents and children these risk factors play a role.
Implications for Public Health and Prevention
The parenting factors associated with ADHD identified in this analysis point to potential targets for lowering the odds of children having clinically significant ADHD symptoms and receiving an ADHD diagnosis. Given heritability and multiple causal pathways of influence, interventions are unlikely to prevent overall occurrence of ADHD symptoms, but may lessen the severity and impact on functioning, thus lessening the odds of meeting diagnostic criteria. The focus of well-established public health efforts to improve healthy child development, such as preventing maltreatment CDC, 2016; Fortson et al., 2016), can be expanded to address clinically diagnosed disorders such as ADHD. Even when specific parenting factors contribute only modestly to individual risk, supporting parents may have a notable impact on population health given the considerable challenges that parents face (NASEM, 2016b). Strategies to support parents by enhancing their parenting skills and by promoting their own health and well-being can promote positive outcomes in children (NASEM, 2019a).
Expanding access to parenting intervention may improve outcomes. Significant evidence exists that behavioral parenting interventions have a positive effect on ADHD symptoms (Epstein et al., 2015; Evans et al., 2018). In fact, for young children with ADHD, parent behavior training is the recommended first-line treatment because it has the best evidence to benefit children and parents (Barbaresi et al., 2020; Rimestad et al., 2016; Wolraich et al., 2019). Many of the evidence-based parenting interventions for ADHD were also used to prevent maltreatment (Altafim & Linhares, 2016), demonstrated effectiveness for children who have ADHD and other conditions such as anxiety (Lebowitz et al., 2020), and can be used if a diagnosis of ADHD may not be easily ascertained (Barbaresi et al., 2020). By decreasing behavior problems in at-risk populations, parenting interventions can be used as prevention (van Aar et al., 2017). For parents who themselves struggle with ADHD symptoms while raising children at risk for ADHD, interventions may benefit from adaptation to individual families’ needs and to address factors in the home and community so parents can change their own behaviors and cognition to support their child’s development more effectively (Johnston et al., 2012).
Interventions that are centered on the whole family may benefit parents and children with ADHD. Strategies that support parenting, promote parental mental health, and address stress may prevent or reduce the impact of childhood mental disorders including ADHD (NASEM, 2019a). For example, given the possible connection between family conflict, divorce, and maltreatment, supporting families during the process of divorce with mediation and mental health support may positively impact children’s development (D'Onofrio & Emery, 2019). However, many families face substantial barriers when trying to access treatment and support for children’s behavioral health; therefore, public health strategies may benefit from including efforts to identify barriers to access to behavioral health interventions and to reduce such barriers, including by addressing funding and payment challenges (Brundage & Shearer, 2019; So et al., 2019). From a public health perspective, supporting parents may also include public health education on specific parenting topics, for example, by working with healthcare providers to inform parents about appropriate limits on screen media (American Academy of Pediatrics, 2016) or by directly providing parents with tools and resources to learn behavioral strategies to support their children and cope with parenting challenges (NASEM, 2021).
For public health, supporting parents can include addressing the social determinants of risk and adversity (CDC, 2019), family conflict and violence (CDC, 2016; Fortson et al., 2016), and the root cause of structural inequalities of parental incarceration and trauma (Bailey et al., 2021). Support for parents may also be provided by directly reducing factors that negatively impact parenting such as lack of resources, health disparities, and systemic disadvantages (NASEM, 2016). Given that ADHD is associated with increased socioeconomic risk, which can be transmitted intergenerationally (Aizer, 2017), interventions that support parents and decrease poverty-associated challenges (CDC Foundation, 2020; Hamad & Rehkopf, 2016) may also improve outcomes for children with ADHD, potentially decreasing the number of children who will be diagnosed with ADHD. For example, the Earned Income Tax Credits which may benefit children’s mental health overall (CDC Foundation, 2020) could potentially improve ADHD outcomes as well. Systemic approaches that address adverse childhood experiences (ACEs) such as child maltreatment, separation, and parental incarceration, may prevent long-term negative consequences for health and development that compound the impact of ADHD (CDC, 2019; Fortson et al., 2016; Jimenez et al., 2017). In addition to broadening access to evidence-based parenting programs and high-quality early childhood programs, prevention of adverse childhood experiences can include strengthening household financial security, supporting family friendly work policies, and enhancing norms that protect against violence (CDC, 2019). A broad approach to supporting parents may result in decreasing risk for ADHD symptoms and in strengthening factors that allow children with ADHD to live healthy and supported lives.
Appendix. Search terms
| Component | Search terms |
|---|---|
| Attention-deficit/hyperactivity disorder (ADHD)–related terms | (((“attention deficit”) OR (“hyperactivity disorder*”) OR (“deficit hyperactiv*”) OR (“ADHD”) OR (“deficit disorder*”) OR (“minimal brain dysfunction”) OR (“minimal brain damage”) OR (“MBD”) OR (“brain injured child syndrome*”) OR (“hyperactive child syndrome*”) OR (“hyperactive syndrome*”) OR (“impulse disorder*”) OR (“hyperkinetic disease”) OR (“hyperkinetic syndrome*”) OR (“hyperkinetic reaction of childhood”)) OR ((“ADD” AND (disorder OR attention OR hyperactiv*))) OR ((“attention problem*”) OR (“inattenti*”) OR (“hyperactiv*”) OR (“hyperkines*”))) |
| Child health terms | AND ((“nutrition*”) OR (“deficienc*”) OR (“iron”) OR (“ferritin”) OR (“transferrin”) OR (“anemia”) OR (“copper”) OR (“zinc”) OR (“magnesium”) OR (“polyunsaturated fatty acids”) OR (“fatty acid*”) OR (“folate”) OR (“nutritional surplus*”) OR (“fat”) OR (“sugar*”) OR (“sodium”) OR (“food additive*”) OR (“food color additive*”) OR (“food color*”) OR (“FD&C Yellow”) OR (“FD&C Red”) OR (“preservatives”) OR (“sodium benzoate”) OR (“diet”) OR (“IgG”) OR (“western diet”) OR (“malnutrition”) OR (“electronic*”) OR (“television”) OR (“TV”) OR (“video game*”) OR (“screen time”) OR (“sleep”) OR (“built environment”) OR (“nature”) OR (“green space”) OR (“physical activity”) OR (“exercise”)) |
| Social environment terms | AND ((“socioeconomic”) OR (“SES”) OR (“income”) OR (“social class”) OR (“urban*”) OR (“rural*”) OR (“conflict”) OR (“discord”) OR (“stress”) OR (“foster care”) OR (“single parent*”) OR (“institution*”) OR (“advers*”) OR (“maltreatment”) OR (“deprivation”) OR (“trauma”) OR (“rejection”) OR (“discipline”) OR (“attachment”)) |
| Follow-up search terms | AND ((“abuse”) OR (“neglect”) OR (“involvement”) OR (“intrusive”) OR (“permissive”) OR (“sensitive”)) |
Supplementary Information
Below is the link to the electronic supplementary material.
Funding
The work presented here was completed through an interagency agreement between the Centers for Disease Control and Prevention and the General Service Administration (13-FED-1303304), under GSA Order Number ID04130157 to Gryphon Scientific, LLC, titled “Identifying Public Health Strategies with Potential for Reducing Risk for Attention-Deficit/Hyperactivity Disorder.”
Declarations
Ethical Approval
Not applicable. This study includes analyses of data previously published in the literature.
Informed Consent
Not applicable. This study includes analyses of data previously published in the literature.
Disclaimer
The findings and conclusions in this manuscript are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Conflict of Interest
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Aizer A. The role of children’s health in the intergenerational transmission of economic status. Child Development Perspectives. 2017;11:167–172. doi: 10.1111/cdep.12231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Altafim ERP, Linhares MBM. Universal violence and child maltreatment prevention programs for parents: A systematic review. Psychosocial Intervention. 2016;25:27–38. doi: 10.1016/j.psi.2015.10.003. [DOI] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders, 5th edition. American Psychiatric Association.
- American Academy of Pediatrics. (2016). Media and young minds. Pediatrics 138(5), e20162591. [DOI] [PubMed]
- Auersperg F, Vlasak T, Ponocny I, Barth A. Long-term effects of parental divorce on mental health – A meta-analysis. Journal of Psychiatric Research. 2019;119:107–115. doi: 10.1016/j.jpsychires.2019.09.011. [DOI] [PubMed] [Google Scholar]
- Bailey ZD, Feldman JM, Bassett MT. How structural racism works — Racist policies as a root cause of U.S. racial health inequities. New England Journal of Medicine. 2021;384:768–773. doi: 10.1056/NEJMms2025396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barbaresi WJ, Campbell L, Diekroger EA, Froehlich TE, Liu YH, O'Malley E, Pelham WE, Power TJ, Zinner SH, Chan E. Society for Developmental and Behavioral Pediatrics clinical practice guideline for the assessment and treatment of children and adolescents with complex attention-deficit/hyperactivity disorder. Journal of Developmental & Behavioral Pediatrics. 2020;41:S35–S57. doi: 10.1097/DBP.0000000000000770. [DOI] [PubMed] [Google Scholar]
- Becker-Blease KA, Freyd JJ. A preliminary study of ADHD symptoms and correlates: Do abused children differ from nonabused children? Journal of Aggression, Maltreatment and Trauma. 2008;17:133–140. doi: 10.1080/10926770802250736. [DOI] [Google Scholar]
- Belsky J, de Haan M. Annual research review: Parenting and children’s brain development: The end of the beginning. Journal of Child Psychology and Psychiatry. 2011;52:409–428. doi: 10.1111/j.1469-7610.2010.02281.x. [DOI] [PubMed] [Google Scholar]
- Bennett DS, Sullivan MW, Lewis M. Relations of parental report and observation of parenting to maltreatment history. Child Maltreatment. 2006;11:63–75. doi: 10.1177/1077559505283589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berlin JA, Laird NM, Sacks HS, Chalmers TC. A comparison of statistical methods for combining event rates from clinical trials. Statistics and Medicine. 1989;8:141–151. doi: 10.1002/sim.4780080202. [DOI] [PubMed] [Google Scholar]
- Beyens I, Valkenburg PM, Piotrowski JT. Screen media use and ADHD-related behaviors: Four decades of research. PNAS. 2018;115:9875–9881. doi: 10.1073/pnas.1611611114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bitsko, R. H., Holbrook, J. R., O’Masta, B., Maher, B., Cerles, A., Saadeh, K., Mahmooth, Z., MacMillan, L. M., Rush, M., Kaminski, J. W. (this issue). A systematic review and meta-analysis of prenatal, birth, and postnatal factors associated with attention-deficit/hyperactivity disorder. Prevention Science. [DOI] [PMC free article] [PubMed]
- Bonde, E., Obel, C., Nedergård, N. J., & Thomsen, P. H. (2004). Social risk factors as predictors for parental report of deviant behaviour in 3-year-old children. Nordic Journal of Psychiatry, 58(1), 17–23. [DOI] [PubMed]
- Bramlett MD, Mosher WD. Cohabitation, marriage, divorce, and remarriage in the United States. Vital Health Statistics. 2002;23:1–93. [PubMed] [Google Scholar]
- Breaux, R. P., & Harvey, E. A. (2019). A longitudinal study of the relation between family functioning and preschool ADHD symptoms. Journal of Clinical Child and Adolescent Psychology, 48(5), 749–764. [DOI] [PubMed]
- Briscoe-Smith, A. M., & Hinshaw, S. P. (2006). Linkages between child abuse and attention-deficit/hyperactivity disorder in girls: behavioral and social correlates. Child Abuse & Neglect, 30, 1239–1255. [DOI] [PMC free article] [PubMed]
- Brundage, S. C., & Shearer, C. (2019). Plan and provider opportunities to move toward integrated family health care. United Hospital Fund. https://uhfnyc.org/media/filer_public/c1/0b/c10bfb65-dbf9-4d2c-9f97-ecd2a3928a9e/plan_and_provider_opportunities_uhf.pdf
- CDC Foundation. (2020). Public health action guide: Earned income tax credit. https://www.cdcfoundation.org/sites/default/files/files/EITC_PublicHealthActionGuide.pdf. Accessed 8 Jan 2021.
- Centers for Disease Control and Prevention (CDC). (2016). Preventing multiple forms of violence: A strategic vision for connecting the dots. https://www.cdc.gov/violenceprevention/pdf/strategic_vision.pdf. Accessed 5 Mar 2021.
- Centers for Disease Control and Prevention (CDC). (2019). Preventing adverse childhood experiences: Leveraging the best available evidence. https://www.cdc.gov/violenceprevention/pdf/preventingACES.pdf. Accessed 1 Nov 2021.
- Chen H, Cohen P, Chen S. How big is a big odds ratio? Interpreting the magnitudes of odds ratios in epidemiological studies. Communications in Statistics - Simulation and Computation. 2010;39:860–864. doi: 10.1080/03610911003650383. [DOI] [Google Scholar]
- Choenni, V., Lambregtse-van den Berg, M. P., Verhulst, F. C., Tiemeier, H., & Kok, R. (2019). The longitudinal relation between observed maternal parenting in the preschool period and the occurrence of child ADHD symptoms in middle childhood. Journal of Abnormal Child Psychology, 47(5), 755–764. [DOI] [PMC free article] [PubMed]
- Cheng, S., Maeda, T., Yoichi, S., Yamagata, Z., Tomiwa, K., Group, J. C. s. S Early television exposure and children’s behavioral and social outcomes at age 30 months. Journal of Epidemiology. 2010;20:S482–489. doi: 10.2188/jea.JE20090179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christakis DA, Zimmerman FJ, DiGiuseppe DL, McCarty CA. Early television exposure and subsequent attentional problems in children. Pediatrics. 2004;113:708–713. doi: 10.1542/peds.113.4.708. [DOI] [PubMed] [Google Scholar]
- Claussen AH, Crittenden PM. Maternal sensitivity. In: Crittenden PM, Claussen AH, editors. The organization of attachment relationships: Maturation, culture, and context. Cambridge University Press; 2000. pp. 115–122. [Google Scholar]
- Claussen AH, Robinson LR, Kaminski JW, Charania S, Holbrook JR, So M, Ghandour R, Smith C, Satterfield-Nash A, Peacock G, Boyle C. Factors associated with self-regulation in a nationally representative sample of children ages 3–5 years: United States, 2016. Maternal and Child Health Journal. 2021;25:27–37. doi: 10.1007/s10995-020-03039-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen JR. Statistical power analysis for the behavioral sciences. 2. Routledge; 1988. [Google Scholar]
- Cohen, A. J., Adler, N., Kaplan, S. J., Pelcovitz, D., & Mandel, F. S. (2002). Interactional effects of marital status and physical abuse on adolescent psychopathology. Child Abuse & Neglect, 26(3), 277–288. [DOI] [PubMed]
- Coyne SM, Radesky J, Collier KM, Gentile DA, Linder JR, Nathanson AI, Rasmussen RR, Reich SM, Rogers J. Parenting and digital media. Pediatrics. 2017;140:S112–S116. doi: 10.1542/peds.2016-1758N. [DOI] [PubMed] [Google Scholar]
- D'Onofrio B, Emery R. Parental divorce or separation and children’s mental health. World Psychiatry : Official Journal of the World Psychiatric Association (WPA) 2019;18:100–101. doi: 10.1002/wps.20590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danielson, M. L., Bitsko, R. H., Ghandour, R. M., Holbrook, J. R., Kogan, M. D., & Blumberg, S. J. (2018). Prevalence of parent-reported ADHD diagnosis and associated treatment among U.S. children and adolescents, 2016. Journal of Clinical Child & Adolescent Psychology, 47(2), 199–212. [DOI] [PMC free article] [PubMed]
- Darling Rasmussen P, Bilenberg N, Shmueli-Goetz Y, Simonsen E, Bojesen AB, Storebø OJ. Attachment representations in mothers and their children diagnosed with ADHD: Distribution, transmission and impact on treatment outcome. Journal of Child and Family Studies. 2019;28:1018–1028. doi: 10.1007/s10826-019-01344-5. [DOI] [Google Scholar]
- de Paul, J., & Arruabarrena, M. I. (1995). Behavior problems in school-aged physically abused and neglected children in Spain. Child Abuse & Neglect, 19(4), 409–418. [DOI] [PubMed]
- Deault LC. A systematic review of parenting in relation to the development of comorbidities and functional impairments in children with attention-deficit/hyperactivity disorder (ADHD) Child Psychiatry & Human Development. 2010;41:168–192. doi: 10.1007/s10578-009-0159-4. [DOI] [PubMed] [Google Scholar]
- DerSimonian R, Laird N. Meta-analysis in clinical trials. Controlled Clinical Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- Dimitrov, L. V., Kaminski, J. W., Holbrook, J. R., Bitsko, R. H., Yeh, M., O’Masta, B., Cerles, A., Rush, M., & Maher, B. (under review this issue). A systematic review and meta-analysis of chemical and environmental exposures and attention deficit/hyperactivity disorder. Prevention Science. [DOI] [PMC free article] [PubMed]
- Epstein, R. A., Fonnesbeck, C., Williamson, E., Kuhn, T., Lindegren, M. L., Rizzone, K., Krishnaswami, S., Sathe, N., Ficzeree, C. H, Ness, G. L., Wright, G. W., Raj, M., Potter, S. & McPheeters, M. R. (2015). Psychosocial and pharmacologic interventions for disruptive behavior in children and adolescents. Agency for Healthcare Research and Quality. https://effectivehealthcare.ahrq.gov/products/disruptive-behavior-disorder/research. Accessed 15 Oct 2019. [PubMed]
- Evans SW, Owens JS, Wymbs BT, Ray AR. Evidence-based psychosocial treatments for children and adolescents with attention deficit/hyperactivity disorder. Journal of Clinical Child & Adolescent Psychology. 2018;47:157–198. doi: 10.1080/15374416.2017.1390757. [DOI] [PubMed] [Google Scholar]
- Famularo, R., Kinscherff, R., & Fenton, T. (1992). Psychiatric diagnoses of maltreated children: preliminary findings. Journal of the American Academy of Child and Adolescent Psychiatry, 31, 863–867. [DOI] [PubMed]
- Faraone SV, Banaschewski T, Coghill D, Zheng Y, Biederman J, Bellgrove MA, Newcorn JF, Gignac M, Al Saud NM, Manor I, Rohde LA, Yang L, Cortese S, Almagor D, Stein MA, Albatti TH, Aljoudi HF, Alqahtani M, Wang Y. The World Federation of ADHD International Consensus Statement: 208 evidence-based conclusions about the disorder. Neuroscience & Biobehavioral Reviews. 2021;128:789–818. doi: 10.1016/j.neubiorev.2021.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faraone SV, Larsson H. Genetics of attention deficit hyperactivity disorder. Molecular Psychiatry. 2019;24:562–575. doi: 10.1038/s41380-018-0070-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faraone SV, Mick E. Molecular genetics of attention deficit hyperactivity disorder. Psychiatric Clinics. 2010;33:159–180. doi: 10.1016/j.psc.2009.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fearon RP, Bakermans-Kranenburg MJ, van IJzendoorn, M. H., Lapsley, A.-M., & Roisman, G. I. The significance of insecure attachment and disorganization in the development of children’s externalizing behavior: A meta-analytic study. Child Development. 2010;81:435–456. doi: 10.1111/j.1467-8624.2009.01405.x. [DOI] [PubMed] [Google Scholar]
- Fitzpatrick C, Barnett T, Pagani LS. Early exposure to media violence and later child adjustment. Journal of Developmental and Behavioral Pediatrics. 2012;33:291–297. doi: 10.1097/DBP.0b013e31824eaab3. [DOI] [PubMed] [Google Scholar]
- Fortson, B. L., Klevens, J., Merrick, M. T., Gilbert, L. K., & Alexander, S. P. (2016). Preventing child abuse and neglect: A technical package for policy, norm, and programmatic activities. https://www.cdc.gov/violenceprevention/pdf/CAN-Prevention-Technical-Package.pdf. Accessed 5/3/2021
- Foster, E. M., & Watkins, S. (2010). The value of reanalysis: TV viewing and attention problems. Child development, 81(1), 368–375. [DOI] [PubMed]
- Fredland N, McFarlane J, Symes L, Maddoux J. Exploring the association of maternal adverse childhood experiences with maternal health and child behavior following intimate partner violence. Journal of Women's Health. 2018;27:64–71. doi: 10.1089/jwh.2016.5969. [DOI] [PubMed] [Google Scholar]
- Freitag, C. M., & Retz, W. (2010). Family and twin studies in attention-deficit hyperactivity disorder. In W. Retz & R. G. Klein (Eds.), Attention-deficit hyperactivity disorder (ADHD) in adults. Key Issues in Mental Health. Basel: Karger.
- Gabel, S., & Shindledecker, R. (1993). Characteristics of children whose parents have been incarcerated. Hospital & Community Psychiatry, 44(7), 656–660. [DOI] [PubMed]
- Geller, A., Cooper, C. E., Garfinkel, I., Schwartz-Soicher, O., & Mincy, R. B. (2012). Beyond absenteeism: father incarceration and child development. Demography, 49, 49–76. [DOI] [PMC free article] [PubMed]
- Geller A, Garfinkel I, Cooper CE, Mincy RB. Parental incarceration and child well-being: Implications for urban families*. Social Science Quarterly. 2009;90:1186–1202. doi: 10.1111/j.1540-6237.2009.00653.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giannotta, F., & Rydell, A. M. (2017). The role of the mother-child relationship in the route from child ADHD to adolescent symptoms of depressed mood. Journal of Adolescence, 61, 40–49. [DOI] [PubMed]
- Goldsmith DF, Oppenheim D, Wanlass J. Separation and reunification: Using attachment theory and research to inform decisions affecting the placements of children in foster care. Juvenile and Family Court Journal. 2004;55:1–13. doi: 10.1111/j.1755-6988.2004.tb00156.x. [DOI] [Google Scholar]
- Graziano, P. A., Calkins, S. D., & Keane, S. P. (2011). Sustained attention development during the toddlerhood to preschool period: associations with toddlers' emotion regulation strategies and maternal behaviour. Infant and Child, 20(6), 389–408. [DOI] [PMC free article] [PubMed]
- Guerrero AD, Biely C, Dudovitz R, Coker T, Iyer S, Barnert E, Szilagyi P, Szilagyi M, Chung PJ. Measurement and identification of parenting behaviors associated with social-emotional outcomes in children: The racial and cultural appropriateness of a commonly used parenting measure. Journal of Developmental & Behavioral Pediatrics. 2021;42:524–531. doi: 10.1097/DBP.0000000000000933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haj-Yahia MM, Abdo-Kaloti R. Mental health consequences of Palestinian adolescents’ exposure to family violence. Journal of Loss & Trauma. 2008;13:1–41. doi: 10.1080/15325020701429130. [DOI] [Google Scholar]
- Haltigan, J. D., Roisman, G. I., & Fraley, R. C. (2013). The predictive significance of early caregiving experiences for symptoms of psychopathology through midadolescence: Enduring or transient effects? Development and Psychopathology, 25(Special Issue 01), 209–221. [DOI] [PubMed]
- Hamad R, Rehkopf DH. Poverty and child development: A longitudinal study of the impact of the Earned Income Tax Credit. American Journal of Epidemiology. 2016;183:775–784. doi: 10.1093/aje/kwv317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hays-Grudo, J., & Morris, A. S. (2020). The intergenerational transmission of ACEs and PACEs. In Adverse and protective childhood experiences: A developmental perspective (pp. 69–84). American Psychological Association.
- Hilton JM, Desrochers S, Devall EL. Comparison of role demands, relationships, and child functioning in single-mother, single father, and intact families. Journal of Divorce & Remarriage. 2001;35:29–56. doi: 10.1300/J087v35n01_02. [DOI] [Google Scholar]
- Hjern, A., Weitoft, G. R., & Lindblad, F. (2010). Social adversity predicts ADHD-medication in school children--a national cohort study. Acta Paediatrica, 99(6), 920–924. [DOI] [PubMed]
- Hughes C, Devine RT. For better or for worse? Positive and negative parental influences on young children’s executive function. Child Development. 2017;90:593–609. doi: 10.1111/cdev.12915. [DOI] [PubMed] [Google Scholar]
- Humphreys KL, Zeanah CH. Deviations from the expectable environment in early childhood and emerging psychopathology. Neuropsychopharmacology. 2015;40:154–170. doi: 10.1038/npp.2014.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hurtig, T., Taanila, A., Ebeling, H., Miettunen, J., & Moilanen, I. (2005). Attention and behavioural problems of Finnish adolescents may be related to the family environment. European Child & Adolescent Psychiatry, 14(8), 471–478. [DOI] [PubMed]
- Jacobvitz, D., & Sroufe, L. A. (1987). The early caregiver-child relationship and attention-deficit disorder with hyperactivity in kindergarten: a prospective study. Child Development, 58(6), 1496–1504. [DOI] [PubMed]
- Jimenez ME, Wade R, Jr, Schwartz-Soicher O, Lin Y, Reichman NE. Adverse childhood experiences and ADHD diagnosis at age 9 years in a national urban sample. Academic Pediatrics. 2017;17:356–361. doi: 10.1016/j.acap.2016.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson, J. G., Cohen, P., Kasen, S., & Brook, J. S. (2007). Extensive television viewing and the development of attention and learning difficulties during adolescence. Archives of Pediatrics & Adolescent Medicine, 161, 480–486. [DOI] [PubMed]
- Johnston C, Mash EJ, Miller N, Ninowski JE. Parenting in adults with attention-deficit/hyperactivity disorder (ADHD) Clinical Psychology Review. 2012;32:215–228. doi: 10.1016/j.cpr.2012.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kashala, E., Tylleskar, T., Elgen, I., Kayembe, K. T., & Sommerfelt, K. (2005). Attention deficit and hyperactivity disorder among school children in Kinshasa, Democratic Republic of Congo. African Health Sciences, 5, 172–181. [DOI] [PMC free article] [PubMed]
- Kelly, Y. J., Nazroo, J. Y., McMunn, A., Boreham, R., & Marmot, M. (2001). Birthweight and behavioural problems in children: a modifiable effect? International Journal of Epidemiology, 30, 88–94. [DOI] [PubMed]
- Keown, L. J. (2012). Predictors of boys' ADHD symptoms from early to middle childhood: the role of father-child and mother-child interactions. Journal of Abnormal Child Psychology, 40(4), 569–581. [DOI] [PubMed]
- Kerr, D., & Michalski, J. H. (2007). Family structure and children's hyperactivity problems: A longitudinal analysis. Canadian Journal of Sociology-Cahiers Canadiens De Sociologie, 32, 85–112.
- Kiff CJ, Lengua LJ, Zalewski M. Nature and nurturing: Parenting in the context of child temperament. Clinical Child and Family Psychology Review. 2011;14:251. doi: 10.1007/s10567-011-0093-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim, H. W., Cho, S. C., Kim, B. N., Kim, J. W., Shin, M. S., & Kim, Y. (2009). Perinatal and familial risk factors are associated with full syndrome and subthreshold attention-deficit hyperactivity disorder in a Korean community sample. Psychiatry Investigation, 6(4), 278–285. [DOI] [PMC free article] [PubMed]
- King DC, Abram KM, Romero EG, Washburn JJ, Welty LJ, Teplin LA. Childhood maltreatment and psychiatric disorders among detained youths. Psychiatric Services. 2011;62:1430–1438. doi: 10.1176/appi.ps.004412010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kočovská, E., Puckering, C., Follan, M., Smillie, M., Gorski, C., Barnes, J., Wilson, P., Young, D., Lidstone, E., Pritchett, R., Hockaday, H., & Minnis, H. (2012). Neurodevelopmental problems in maltreated children referred with indiscriminate friendliness. Research in Developmental Disabilities, 33, 1560–1565. [DOI] [PubMed]
- Kok R, Thijssen S, Bakermans-Kranenburg MJ, Jaddoe VWV, Verhulst FC, White T, van IJzendoorn, M. H., & Tiemeier, H. Normal variation in early parental sensitivity predicts child structural brain development. Journal of the American Academy of Child & Adolescent Psychiatry. 2015;54:824–831.e821. doi: 10.1016/j.jaac.2015.07.009. [DOI] [PubMed] [Google Scholar]
- Landhuis CE, Poulton R, Welch D, Hancox RJ. Does childhood television viewing lead to attention problems in adolescence? Results from a prospective longitudinal study. Pediatrics. 2007;120:532–537. doi: 10.1542/peds.2007-0978. [DOI] [PubMed] [Google Scholar]
- Larsson, H., Dilshad, R., Lichtenstein, P., & Barker, E. D. (2011). Developmental trajectories of DSM-IV symptoms of attention-deficit/hyperactivity disorder: genetic effects, family risk and associated psychopathology. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 52, 954–963. [DOI] [PubMed]
- Lau AS, Valeri SM, McCarty CA, Weisz JR. Abusive parents’ reports of child behavior problems: Relationship to observed parent-child interactions. Child Abuse & Neglect. 2006;30:639–655. doi: 10.1016/j.chiabu.2005.11.009. [DOI] [PubMed] [Google Scholar]
- Lebowitz ER, Marin C, Martino A, Shimshoni Y, Silverman WK. Parent-based treatment as efficacious as cognitive-behavioral therapy for childhood anxiety: A randomized noninferiority study of supportive parenting for anxious childhood emotions. Journal of the American Academy of Child & Adolescent Psychiatry. 2020;59:362–372. doi: 10.1016/j.jaac.2019.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, Y.-J., Xie, X.-N., Lei, X., Li, Y.-M., & Lei, X. (2020). Global prevalence of obesity, overweight and underweight in children, adolescents and adults with autism spectrum disorder, attention-deficit hyperactivity disorder: A systematic review and meta-analysis. Obesity Reviews, 21(12), e13123. [DOI] [PubMed]
- Lifford, K. J., Harold, G. T., & Thapar, A. (2008). Parent-child relationships and ADHD symptoms: a longitudinal analysis. Journal of Abnormal Child Psychology, 36, 285–296. [DOI] [PubMed]
- Lifford, K. J., Harold, G. T., & Thapar, A. (2009). Parent-child hostility and child ADHD symptoms: a genetically sensitive and longitudinal analysis. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 50, 1468–1476. [DOI] [PubMed]
- Liu, X., Guo, C., Okawa, M., Zhai, J., Li, Y., Uchiyama, M., Neiderhiser, J. M., & Kurita, H. (2000). Behavioral and emotional problems in Chinese children of divorced parents. Journal of the American Academy of Child and Adolescent Psychiatry, 39(7), 896–903. [DOI] [PubMed]
- Maher, B., Kaminski, J. W., O'Masta, B., Cerles, A., Holbrook, J. R., Mahmooth, Z., & Bitsko, R. H. (under review this issue). A systematic meta-analysis of the relationship between exposure to parental substance use and attention-deficit/hyperactivity disorder. Prevention Science. [DOI] [PMC free article] [PubMed]
- Maniccia DM, Davison KK, Marshall SJ, Manganello JA, Dennison BA. A meta-analysis of interventions that target children’s screen time for reduction. Pediatrics. 2011;128:e193–e210. doi: 10.1542/peds.2010-2353. [DOI] [PubMed] [Google Scholar]
- McDonald SW, Madigan S, Racine N, Benzies K, Tomfohr L, Tough S. Maternal adverse childhood experiences, mental health, and child behaviour at age 3: The all our families community cohort study. Preventive Medicine. 2019;118:286–294. doi: 10.1016/j.ypmed.2018.11.013. [DOI] [PubMed] [Google Scholar]
- Mendelsohn AL, Dreyer BP, Brockmeyer CA, Berkule-Silberman SB, Huberman HS, Tomopoulos S. Randomized controlled trial of primary care pediatric parenting programs: Effect on reduced media exposure in infants, mediated through enhanced parent-child interaction. Archives of Pediatrics & Adolescent Medicine. 2011;165:42–48. doi: 10.1001/archpediatrics.2010.266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menon M, Katz RC, Easterbrooks MA. Linking attachment and executive function systems: Exploring associations in a sample of children of young mothers. Journal of Child and Family Studies. 2020;29:2314–2329. doi: 10.1007/s10826-020-01759-5. [DOI] [Google Scholar]
- Meysamie, A., Fard, M. D., & Mohammadi, M. R. (2011). Prevalence of attention-deficit/hyperactivity disorder symptoms in preschool-aged Iranian children. Iranian Journal of Pediatrics, 21, 467–472. [PMC free article] [PubMed]
- Midouhas E, Kuang Y, Flouri E. Neighbourhood human capital and the development of children׳s emotional and behavioural problems: The mediating role of parenting and schools. Health & Place. 2014;27:155–161. doi: 10.1016/j.healthplace.2014.02.004. [DOI] [PubMed] [Google Scholar]
- Miller, N. V., Degnan, K. A., Hane, A. A., Fox, N. A., & Chronis-Tuscano, A. (2019). Infant temperament reactivity and early maternal caregiving: independent and interactive links to later childhood attention-deficit/hyperactivity disorder symptoms. Journal of Child Psychology and Psychiatry, 60(1), 43–53. [DOI] [PMC free article] [PubMed]
- Mimouni-Bloch, A., Kachevanskaya, A., Mimouni, F. B., Shuper, A., Raveh, E., & Linder, N. (2013). Breastfeeding may protect from developing attention-deficit/hyperactivity disorder. Breastfeeding Medicine, 8(4), 363–367. [DOI] [PubMed]
- Mistry, K. B., Minkovitz, C. S., Strobino, D. M., & Borzekowski, D. L. (2007). Children’s television exposure and behavioral and social outcomes at 5.5 years: Does timing of exposure matter? Pediatrics, 120(4), 762–769. [DOI] [PubMed]
- Molina MF, Musich FM. Perception of parenting style by children with ADHD and its relation with inattention, hyperactivity/impulsivity and externalizing symptoms. Journal of Child and Family Studies. 2016;25:1656–1671. doi: 10.1007/s10826-015-0316-2. [DOI] [Google Scholar]
- Morrell J, Murray L. Parenting and the development of conduct disorder and hyperactive symptoms in childhood: A prospective longitudinal study from 2 months to 8 years. Journal of Child Psychology and Psychiatry. 2003;44:489–508. doi: 10.1111/1469-7610.t01-1-00139. [DOI] [PubMed] [Google Scholar]
- Murray J, Murray L. Parental incarceration, attachment and child psychopathology. Attachment & Human Development. 2010;12:289–309. doi: 10.1080/14751790903416889. [DOI] [PubMed] [Google Scholar]
- National Academies of Sciences, Engineering, and Medicine. (2016). Parenting matters: Supporting parents of children ages 0–8. https://www.nap.edu/read/21868/chapter/1. Accessed 3 Dec 2019. [PubMed]
- National Academies of Sciences, Engineering, and Medicine. (2019a). Fostering healthy mental, emotional, and behavioral development in children and youth: A national agenda. https://www.nap.edu/resource/25201/MEB.pdf. Accessed 31 Jan 2020. [PubMed]
- National Academies of Sciences, Engineering, and Medicine. (2019b). Vibrant and healthy kids: Aligning science, practice, and policy to advance health equity. https://www.nap.edu/catalog/25466/vibrant-and-healthy-kids-aligning-science-practice-and-policy-to. Accessed 3 Dec 2019. [PubMed]
- National Academies of Sciences, Engineering, and Medicine. (2021). Promoting emotional well-being and resilience. https://www.nationalacademies.org/our-work/promoting-emotional-well-being-and-resilience. 1 May 2021.
- Ni G, Amare AT, Zhou X, Mills N, Gratten J, Lee SH. The genetic relationship between female reproductive traits and six psychiatric disorders. Scientific Reports. 2019;9:12041. doi: 10.1038/s41598-019-48403-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nolin, P., & Ethier, L. (2007). Using neuropsychological profiles to classify neglected children with or without physical abuse. Child Abuse & Neglect, 31(6), 631–643. [DOI] [PubMed]
- Obel, C., Henriksen, T. B., Dalsgaard, S., Linnet, K. M., Skajaa, E., Thomsen, P. H., & Olsen, J. (2004). Does children's watching of television cause attention problems? Retesting the hypothesis in a Danish cohort. Pediatrics, 114, 1373–1374. [DOI] [PubMed]
- Pallini, S., Morelli, M., Chirumbolo, A., Baiocco, R., Laghi, F., & Eisenberg, N. (2019). Attachment and attention problems: A meta-analysis. Clinical Psychology Review, 74, 101772. [DOI] [PubMed]
- Park JL, Hudec KL, Johnston C. Parental ADHD symptoms and parenting behaviors: A meta-analytic review. Clinical Psychology Review. 2017;56:25–39. doi: 10.1016/j.cpr.2017.05.003. [DOI] [PubMed] [Google Scholar]
- Parkes A, Sweeting H, Wight D, Henderson M. Do television and electronic games predict children’s psychosocial adjustment? Longitudinal research using the UK Millennium Cohort Study. Archives of Disease in Childhood. 2013;98:341–348. doi: 10.1136/archdischild-2011-301508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pauli-Pott, U., Schloß, S., & Becker, K. (2018). Maternal responsiveness as a predictor of self-regulation development and attention-deficit/hyperactivity symptoms across preschool ages. Child Psychiatry and Human Development, 49(1), 42–52. [DOI] [PubMed]
- Pinto, C., Turton, P., Hughes, P., White, S., & Gillberg, C. (2006). ADHD and infant disorganized attachment: a prospective study of children next-born after stillbirth. Journal of Attention Disorders, 10(1), 83–91. [DOI] [PubMed]
- Poulain T, Vogel M, Neef M, Abicht F, Hilbert A, Genuneit J, Körner A, Kiess W. Reciprocal associations between electronic media use and behavioral difficulties in preschoolers. International Journal of Environmental Research and Public Health. 2018;15:814. doi: 10.3390/ijerph15040814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radesky JS, Silverstein M, Zuckerman B, Christakis DA. Infant self-regulation and early childhood media exposure. Pediatrics. 2014;133:e1172–e1178. doi: 10.1542/peds.2013-2367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rimestad ML, Lambek R, Zacher Christiansen H, Hougaard E. Short- and long-term effects of parent training for preschool children with or at risk of ADHD: A systematic review and meta-analysis. Journal of Attention Disorders. 2016;23:423–434. doi: 10.1177/1087054716648775. [DOI] [PubMed] [Google Scholar]
- Roberts AL, Liew Z, Lyall K, Ascherio A, Weisskopf MG. Association of maternal exposure to childhood abuse with elevated risk for attention deficit hyperactivity disorder in offspring. American Journal of Epidemiology. 2018;187:1896–1906. doi: 10.1093/aje/kwy098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson, L. R., Bitsko, R. H., O’Masta, B., Holbrook, J. R., Ko, J., Barry, C. M., Maher, B., Cerles, A., Saadeh, K., MacMillan, L. M., Mahmooth, Z., Bloomfield, J., Rush, M., & Kaminski, J. W. (this issue). A systematic review and meta-analysis of parental depression, antidepressant usage, antisocial personality disorder, and stress and anxiety as risk factors for attention-deficit/hyperactivity disorder (ADHD) in children. Prevention Science. [DOI] [PMC free article] [PubMed]
- Robinson, L. R., Boris, N. W., Heller, S. S., Rice, J., Zeanah, C. H., Clark, C., & Hawkins, S. (2012). The good enough home? Home environment and outcomes of young maltreated children. Child & Youth Care Forum, 41, 73–88.
- Rodriguez, J. D. M., da Silva, A. A. M., Bettiol, H., Barbieri, M. A., & Rona, R. J. (2011). The impact of perinatal and socioeconomic factors on mental health problems of children from a poor Brazilian city: a longitudinal study. Social Psychiatry and Psychiatric Epidemiology, 46(5), 381–391. [DOI] [PubMed]
- Rogosch, F. A., Dackis, M. N., & Cicchetti, D. (2011). Child maltreatment and allostatic load: consequences for physical and mental health in children from low-income families. Development and Psychopathology, 23, 1107–1124. [DOI] [PMC free article] [PubMed]
- Romano E, Tremblay RE, Farhat A, Cote S. Development and prediction of hyperactive symptoms from 2 to 7 years in a population-based sample. Pediatrics. 2006;117:2101–2110. doi: 10.1542/peds.2005-0651. [DOI] [PubMed] [Google Scholar]
- Rowland AS, Skipper BJ, Rabiner DL, Qeadan F, Campbell RA, Naftel AJ, Umbach DM. Attention-deficit/hyperactivity disorder (ADHD): Interaction between socioeconomic status and parental history of ADHD determines prevalence. Journal of Child Psychology and Psychiatry. 2018;59:213–222. doi: 10.1111/jcpp.12775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rydell, A.-M. (2010). Family factors and children's disruptive behaviour: an investigation of links between demographic characteristics, negative life events and symptoms of ODD and ADHD. Social Psychiatry and Psychiatric Epidemiology, 45(2), 233–244. [DOI] [PubMed]
- Schachar, R. J., & Wachsmuth, R. (1991). Family dysfunction and psychosocial adversity: Comparison of attention deficit disorder, conduct disorder, normal and clinical controls. Canadian Journal of Behavioural Science, 23(3), 332–348.
- Schickedanz, A., Halfon, N., Sastry, N., & Chung, P. J. (2018). Parents’ adverse childhood experiences and their children’s behavioral health problems. Pediatrics, 142(2). [DOI] [PMC free article] [PubMed]
- Sesar K, Zivcić-Bećirević I, Sesar D. Multi-type maltreatment in childhood and psychological adjustment in adolescence: Questionnaire study among adolescents in Western Herzegovina Canton. Croatian Medical Journal. 2008;49:243–256. doi: 10.3325/cmj.2008.2.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simmel C, Brooks D, Barth RP, Hinshaw SP. Externalizing symptomatology among adoptive youth: Prevalence and preadoption risk factors. Journal of Abnormal Child Psychology. 2001;29:57–69. doi: 10.1023/A:1005251513130. [DOI] [PubMed] [Google Scholar]
- So, M., Dziuban, E. J., Pedati, C., Holbrook, J. R., Claussen, A. H., O'Masta, B., Maher, B., Cerles, A., Mamooth, Z. McMillan, L., Kaminski, J. W., & Rush, M. (under review this issue). Childhood physical health and attention deficit/hyperactivity disorder: A systematic review and meta-analysis of modifiable factors. Prevention Science. [DOI] [PMC free article] [PubMed]
- So M, McCord RF, Kaminski JW. Policy levers to promote access to and utilization of children’s mental health services: A systematic review. Administration and Policy in Mental Health and Mental Health Services Research. 2019;46:334–351. doi: 10.1007/s10488-018-00916-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sonuga-Barke EJS, Halperin JM. Developmental phenotypes and causal pathways in attention deficit/hyperactivity disorder: Potential targets for early intervention? Journal of Child Psychology and Psychiatry. 2010;51:368–389. doi: 10.1111/j.1469-7610.2009.02195.x. [DOI] [PubMed] [Google Scholar]
- Stadelmann, S., Perren, S., Groeben, M., & von Klitzing, K. (2010). Parental separation and children's behavioral/emotional problems: the impact of parental representations and family conflict. Family process, 49(1), 92–108. [DOI] [PubMed]
- Stevens T, Mulsow M. There is no meaningful relationship between television exposure and symptoms of attention-deficit/hyperactivity disorder. Pediatrics. 2006;117:665–672. doi: 10.1542/peds.2005-0863. [DOI] [PubMed] [Google Scholar]
- Stiglic, N., & Viner, R. M. (2019). Effects of screentime on the health and well-being of children and adolescents: A systematic review of reviews. BMJ Open, 9(1), e023191. [DOI] [PMC free article] [PubMed]
- Storebø OJ, Darling Rasmussen P, Simonsen E. Association between insecure attachment and ADHD: Environmental mediating factors. Journal of Attention Disorders. 2013;20:187–196. doi: 10.1177/1087054713501079. [DOI] [PubMed] [Google Scholar]
- Strathearn, L., Giannotti, M., Mills, R., Kisely, S., Najman, J., & Abajobir, A. (2020). Long-term cognitive, psychological, and health outcomes associated with child abuse and neglect. Pediatrics, 146(4), e20200438. [DOI] [PMC free article] [PubMed]
- Stright, A. D., & Neitzel, C. (2003). Beyond parenting: Coparenting and children's classroom adjustment. International Journal of Behavioral Development, 27, 31–40.
- Sutton, A. J., Abrams, K. R., Jones, D. R., Sheldon, T. A., & Song, F. (2000). Methods for meta-analysis in medical research. J. Wiley.
- Swing EL, Gentile DA, Anderson CA, Walsh DA. Television and video game exposure and the development of attention problems. Pediatrics. 2010;126:214–221. doi: 10.1542/peds.2009-1508. [DOI] [PubMed] [Google Scholar]
- Thompson, R., & Tabone, J. K. (2010). The impact of early alleged maltreatment on behavioral trajectories. Child Abuse & Neglect, 34, 907–916. [DOI] [PubMed]
- Umemura, T., Christopher, C., Mann, T., Jacobvitz, D., & Hazen, N. (2015). Coparenting problems with toddlers predict children's symptoms of psychological problems at age 7. Child Psychiatry and Human Development, 46(6), 981–996. [DOI] [PubMed]
- van Aar J, Leijten P, Orobio de Castro B, Overbeek G. Sustained, fade-out or sleeper effects? A systematic review and meta-analysis of parenting interventions for disruptive child behavior. Clinical Psychology Review. 2017;51:153–163. doi: 10.1016/j.cpr.2016.11.006. [DOI] [PubMed] [Google Scholar]
- van der Bij J, den Kelder RO, Montagne B, Hagenaars MA. Inhibitory control in trauma-exposed youth: A systematic review. Neuroscience & Biobehavioral Reviews. 2020;118:451–462. doi: 10.1016/j.neubiorev.2020.06.001. [DOI] [PubMed] [Google Scholar]
- Wolfe DA, Mosk MD. Behavioral comparisons of children from abusive and distressed families. Journal of Consulting and Clinical Psychology. 1983;51:702–708. doi: 10.1037/0022-006X.51.5.702. [DOI] [PubMed] [Google Scholar]
- Wolraich, M. L., Hagan, J. F., Allan, C., Chan, E., Davison, D., Earls, M., Evans, S. W., Flinn, S. K., Froehlich, T., Frost, J., Holbrook, J. R., Lehmann, C. U., Lessin, H. R., Okechukwu, K., Pierce, K. L., Winner, J. D., & Zurhellen, W. (2019). Clinical practice guideline for the diagnosis, evaluation, and treatment of attention-deficit/hyperactivity disorder in children and adolescents. Pediatrics, 144(4), e20192528. [DOI] [PMC free article] [PubMed]
- Zimmerman, F. J., & Christakis, D. A. (2007). Associations between content types of early media exposure and subsequent attentional problems. Pediatrics, 120(5), 986–992. [DOI] [PubMed]
- Ziv, Y., Alva, S., & Zill, N. (2010). Understanding Head Start children's problem behaviors in the context of arrest or incarceration of household members. Early Childhood Research Quarterly, 25, 396–408.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.