Abstract
Posttraumatic stress disorder (PTSD) is a debilitating psychiatric disorder that affects 6% of U.S. adults, yet is treated in only 30% of affected individuals and even fewer low-income individuals. One third of the nation’s low-income individuals are treated in Federally Qualified Health Centers (FQHCs). Most of these facilities lack capacity to provide their patients with first-line, evidence-based treatments for PTSD such as Prolonged Exposure (PE). To address this problem, PE has been adapted for use in a primary care setting and demonstrated efficacy in a brief model for military service members (PE in Primary Care: PE-PC). The effectiveness of this treatment in civilian, low-resource settings such as FQHCs is unknown. This pilot study tested the feasibility and acceptability of PE-PC in 30 Michigan FQHC patients. High rates of therapy participation suggest that the intervention was feasible and acceptable. Semi-structured interview data from 10 patients and 5 FQHC providers indicated that the intervention was helpful and filled a critical need for effective PTSD treatment in the FQHC setting. Interviews also elucidated barriers such as transportation, provider training, and time commitment for patients and providers. These findings set the stage for a full-scale randomized controlled trial to test the effectiveness of PE-PC on PTSD symptoms in this low-resource, high-need setting.
Trial registry ClinicalTrials.gov Identifier: NCT03711266. October 18, 2018.
Keywords: Posttraumatic stress disorder, PTSD, Federally Qualified Health Center, Trauma-focused treatment, Prolonged exposure, Stepped care
Posttraumatic stress disorder (PTSD) is a debilitating psychiatric disorder that affects 14.3 million U.S. adults (Goldstein et al., 2016; Hale et al., 2018) and is likely to increase due to the COVID-19 pandemic (Liu et al., 2020). PTSD is associated with myriad problems including decreased quality of life (Schnurr et al., 2009), increased risk of later-life physical disability (Byers et al., 2014), lost productivity (Adler et al., 2011), and increased risk of suicide (Nock et al., 2014). Unfortunately, only 30% of individuals with PTSD receive treatment in a given year (Hale et al., 2018), and low-income individuals are 30% less likely to receive treatment (Sripada et al., 2015). Critically, previous research demonstrates that low-income individuals experience disproportional mental health burden following national disasters (Bonanno et al., 2007), making it likely that they will experience heightened rates of PTSD in response to the COVID-19 pandemic (McGinty et al., 2020). Thus, there is a pressing need to improve PTSD treatment delivery for these individuals and develop feasible models for implementation (Rauch et al., 2020).
One third of the nation’s low-income individuals are treated in Federally Qualified Health Centers (FQHCs), which receive federal funds to provide primary care services in underserved areas. Highlighting health disparities in access to services, 91% of FQHC patients are low-income, 63% are racial/ethnic minorities, and 20% of them screen positive for PTSD (Meredith et al., 2016). Despite this elevated prevalence, treatment for PTSD is severely limited at FQHCs (Meredith et al., 2009). Furthermore, community mental health providers rarely have training in efficacious PTSD treatments, and community dissemination and implementation efforts have had mixed success (Ruzek & Rosen, 2009). FQHCs do not have the capacity to provide first-line, evidence-based treatments for PTSD such as Prolonged Exposure (PE), which requires specialized training and 90-min sessions. Although one non-trauma-focused PTSD treatment has recently been piloted in the primary care setting (Jain et al., 2020; Smith et al., 2020), no first-line PTSD treatment other than PE-PC (Cigrang et al., 2017) has been tested in the primary care or FQHC setting. Therefore, there is significant need for an adapted first-line, trauma-focused treatment to be delivered in FQHCs.
Prolonged Exposure is a first-line trauma-focused treatment for PTSD that has three core components: in vivo exposure, imaginal exposure, and emotional processing. In vivo exposure is the repeated and systematic approach to objectively safe people, places, objects, and situations that are avoided because they remind individuals of their trauma. Imaginal exposure is the repeated and systematic approach to the trauma memory and related thoughts and feelings. Emotional processing is the confrontation with and expression of trauma-related thoughts and feelings in order to incorporate corrective information into trauma-related fear structures (Foa et al., 2007). PE has substantial evidence supporting its efficacy (Cusack et al., 2016; Foa et al., 2005). It is recommended as a first-line treatment by the American Psychological Association, International Society for Traumatic Stress Studies, Veterans Health Administration, and Department of Defense (APA, 2017; ISTSS, 2020; VA/DoD, 2017) and has high strength of evidence according to a recent systematic review by the Agency for Healthcare Research and Quality (Forman-Hoffman et al., 2018). PE has been demonstrated efficacious in veterans (Rauch et al., 2019) and civilians (Foa et al., 2005) and via telehealth (Morland et al., 2020), with an effect size of 1.37 (Foa et al., 2005). However, PE is only delivered by specialized providers and is not available to the vast majority of individuals with PTSD (Finley et al., 2018). Consequently, strategies are needed to improve the scalability of PE by adapting it to fit the delivery setting.
Standard PE requires 90-min sessions and cannot be delivered in faster-paced primary care settings. Because PTSD is most often detected in primary care (Greene et al., 2016), an on-site adaptation is needed to extend its reach. Moreover, since standard PE requires specialized training, supervision, and consultation, few community-based clinics offer it (Finley et al., 2018; Wolitzky-Taylor et al., 2015). Thus, most individuals with PTSD do not have access to efficacious psychotherapeutic treatment options. PE in Primary Care (PE-PC) is an adapted version of PE that includes all its effective components (Cigrang et al., 2017). This intervention represents a psychotherapeutic advancement in PTSD treatment specifically designed for primary care that can be seamlessly integrated and delivered in the FQHC setting. PE-PC comprises four to eight, 30-min sessions consisting of in-vivo and narrative exposure. PE-PC is efficacious among military service members: a randomized controlled trial with minimal exclusion criteria demonstrated that PE-PC significantly reduces PTSD and other mental health symptoms, as compared to treatment as usual (i.e., between group effect of Cohen’s d = 0.55) (Cigrang et al., 2017). Attrition from PE-PC was only 12%, compared to the typical 20–40% attrition in Standard PE. Ninety-four percent of patients received at least one session and 82% completed all four weekly sessions (Cigrang et al., 2017). Nonetheless, further effectiveness data specific to the FQHC setting are critically needed.
The purpose of the current study was to determine the feasibility and acceptability of PE-PC in the FQHC setting. The rationale is that adapted brief evidence-based interventions for PTSD can improve treatment access and efficiency for low-resource settings. This approach has the potential to improve the scalability of PTSD treatment by minimizing required resources while maximizing effectiveness. We also assessed the impact of PE-PC on PTSD and depression symptoms. We hypothesized that PE-PC would be feasible and acceptable to patients and FQHC providers. We followed the Transparent Reporting of Evaluations with Non-randomized Designs (TREND) statement (Des Jarlais et al., 2004) in reporting methods and results of this study.
Materials and Methods
Participants
The sample was designed with minimal exclusion criteria to be representative of FQHC patients with PTSD. Inclusion criteria for PTSD symptoms was a score of 33 or above on the PTSD checklist for DSM-5 (PCL-5; see Measures), when anchored to an index trauma meeting A1 criteria (Weathers et al., 2013). Patients were also required to be 18 years or older, receive care at one of the participating FQHCs, and have psychotropic medication stability for at least four weeks. Patients were excluded if they were: (1) substantially cognitively impaired (according to the study investigator), (2) unable to agree to study procedures for any reason, (3) at high risk of suicide, (4) currently engaged in a different trauma-focused behavioral treatment (such as Prolonged Exposure or Cognitive Processing Therapy), or (5) had a comorbid disorder that required a higher level of care (e.g., severe substance use disorder or psychotic disorder). We also decided partway through the study to exclude patients with unstable housing, because these patients were having difficulty engaging in trauma-focused treatment while focusing on obtaining stable housing.
Recruitment
FQHC staff screened patients for PTSD using a brief, six-item screener (PTSD Checklist 6-item; Lang & Stein, 2005). Patients who screened positive received a warm handoff (via phone call or page) to a study research assistant, who described the study and completed the remaining screening items with the patient over the phone. Patients were also able to self-refer by contacting the research assistant via phone or through the email listed on fliers placed in clinic waiting rooms. The research assistant determined patient eligibility, reviewed with the patient a comprehensive information sheet about the project, and conducted baseline assessment of demographic information, PTSD symptoms, and secondary outcomes (see Measures).
Setting
Patients were recruited from the following FQHCs: Family Medical Center of Michigan, Hamilton Community Health Network, and Family Health Care. The Family Medical Center of MI, Inc. is a not-for-profit FQHC that provides medical and dental services to adults and children in Monroe, Lenawee, and southwestern Wayne counties in southeastern Michigan. Hamilton Community Health Network is a non-profit organization that provides comprehensive, community-oriented health care to underserved, primarily urban-residing individuals in Genesee County. Family Health Care provides integrated and comprehensive healthcare services to patients at health centers and outreach centers in Lake, Newaygo, Wexford and Missaukee counties. All clinic locations had dedicated telehealth rooms for video visits between the patient and the University of Michigan telepsychologists.
Procedure
PE-PC was delivered by experienced University of Michigan telepsychologists via telehealth (BlueJeans). Interactive video technology is widely available in FQHCs (Fortney et al., 2020) and randomized clinical trials have demonstrated equivalency of standard PE (Acierno et al., 2017; Morland et al., 2020) and other trauma-focused treatments (Morland et al., 2014, 2015) when delivered by telehealth versus in-person. Initially, telehealth sessions were delivered only to the FQHC. However, at the onset of the COVID-19 pandemic in March 2020, we began offering telehealth sessions to patients’ homes, depending on patient preference and FQHC availability. This strategy is sustainable because telehealth-delivered psychotherapy interventions are now fully reimbursable in the state of Michigan (MDHHS, 2020).
Qualitative Data Collection
In this explanatory sequential design (Fetters et al., 2013), qualitative data was used to explore the concept of patient engagement. We conducted semi-structured 30-min interviews with 10 patients and five FQHC providers. Patient interviews focused on the experience of treatment, treatment satisfaction, barriers to treatment engagement (e.g., scheduling, time, finances, transportation, or childcare), and suggestions for overcoming barriers. Provider interviews were guided by the Consolidated Framework for Implementation Research (CFIR), a meta-theoretical framework that serves as a practical guide for assessing barriers and facilitators to prepare for implementation (Damschroder et al., 2009). We designed provider interview guides to encompass the key constructs of Patient Needs and Resources, Implementation Climate (Tension for Change and Compatibility), and Available Resources. We conducted interviews with a purposively selected sample of patients who engaged (n = 7) and did not engage (n = 3) in the intervention, where engagement was defined as attending at least one PE-PC session. The aim was to achieve maximum variation in the patient sample so that we had the broadest understanding of patient experiences. Non-engagers were not asked about their experience of treatment or treatment satisfaction. To achieve maximum variation in provider interviews, we interviewed 1–2 providers from each FQHC (n = 5). Interview guides were refined after the initial patient and provider interviews.
All patients were recruited by email and interviewed via telehealth or telephone. Interviews were conducted by the PI, the project coordinator, and a research assistant. All interviewers received standardized training in conducting qualitative interviews.
Qualitative Data Analysis
Qualitative data collection, coding, analysis, and interpretation were integrated activities, ensuring that the interpretation of findings was well grounded in the data. Interview audio recordings were summarized using structured templates. All interviews were coded by two qualitative analysts and discrepancies were resolved through consensus. To facilitate interview coding, we created a summary template that contained the following columns: CFIR construct (or patient interview domain), sample interview question targeting the construct, key points, and exemplar quotations. Summaries were subsequently consolidated into matrices by participant type in order to identify commonly occurring themes and allow comparison across groups (Gale et al., 2019). The analytic team collaboratively and iteratively reviewed, discussed, and sorted the data to refine the list of themes and highlight the most salient quotes.
Intervention
Treatment content for PE-PC is drawn from the Standard PE model and condensed so as to deliver the most efficacious components of PE in a brief format (Cigrang et al., 2017). PE-PC consisted of four to six weekly 30-min sessions that occurred over a maximum of eight weeks. Study treatment followed the standardized PE-PC manual and workbook, which was provided to the patient by the FQHC or emailed/mailed directly to the patient’s home. In vivo and narrative exposure were introduced at the first session and reviewed at sessions 2–6. To conduct in vivo exposure, patients repeatedly and systematically approached objectively safe people, places, objects, and situations that they previously avoided because these stimuli reminded them of their trauma. To conduct narrative exposure (a modification of imaginal exposure), patients repeatedly and systematically approached their trauma memory and related thoughts and feelings.
In an optional “Session 0,” the therapist reviewed the patient’s PCL-5 responses, provided psychoeducation about PTSD, and provided an overview of the treatment model. During the first PE-PC session, the therapist reviewed the “Confronting Uncomfortable Memories” activity workbook, which was to be completed at home and brought back for use in subsequent sessions. The workbook asked the patient to write a detailed first-person narrative of the event associated with the greatest level of current distress. Emotional processing questions were also included. In addition, the therapist and patient collaboratively planned for in vivo exposure activities between sessions. The patient was instructed to complete the memory exposure for 30 min each day between sessions. At the second PE-PC session, the therapist and patient collaboratively reviewed the patient’s homework. The patient then read the narrative and his or her answers to the emotional processing questions out loud and they processed the exercise with the therapist. Practice continued between sessions. This session format and content were repeated at the third through sixth sessions. At the conclusion of PE-PC, patients who desired additional treatment for co-occurring mental health concerns received referrals to local mental health resources.
Therapist Training and Fidelity
Study therapists received manualized training by the treatment developer and six months of weekly consultation in PE-PC prior to the initiation of the study. During the training phase, they completed at least two training cases and demonstrated fidelity to the therapy model. Consultation calls occurred bi-weekly throughout the study period. Fidelity was assessed by review of progress notes. For each PE-PC session, four dichotomous items for therapist adherence were generated from session outlines and materials to include critical session-specific topics. This yielded Session-Specific Adherence Rating Scales.
Objectives
The objective was to determine the feasibility and acceptability of PE-PC. We hypothesized that patients and FQHC staff would view the intervention as helpful and sustainable in practice.
Outcomes
Consistent with the purpose of a pilot study, the primary outcomes were feasibility and acceptability (Arain et al., 2010). Specific feasibility outcomes included the number of patients screened, number meeting inclusion criteria, identified barriers to participation, adherence of patients to the proposed treatment (measured via number of sessions attended), standard deviation of the proposed outcome measure, response rates to questionnaires, and loss to follow-up (Arain et al., 2010). Although this was a feasibility study and not an effectiveness study, scores on PTSD and depression symptom measures were also assessed. Such assessment allows confidence interval estimation to guide future randomized controlled trials (Lancaster et al., 2004).
Measures
All measures were administered at baseline, 2-month follow-up, and 4-month follow-up, through Qualtrics. Patients had the option to complete the measures online or to report responses over the phone to the study research assistant, who entered answers into Qualtrics. Participants were compensated $30 for completing each of the three assessment batteries and another $30 if they participated in a semi-structured interview.
The PCL-5 (Weathers et al., 2013) is a 20-item self-report measure of PTSD symptoms as defined by the DSM-5. Each item of the PCL-5 is scored on a five-point scale ranging from 0 (“not at all”) to 4 (“extremely”). The PCL-5 has strong internal consistency, test–retest reliability, and convergent and discriminant validity (Blevins et al., 2015; Bovin et al., 2016). Patients were prompted to respond to PCL-5 items in reference to their index trauma. To be included in the study, patients were required to score ≥ 33, which indicates a probable diagnosis of PTSD (Bovin et al., 2016). The PHQ-9 is a 9-item measure of depression with excellent internal and test–retest reliability as well as construct and criterion validity (Kroenke et al., 2001) that effectively detects treatment changes in depression in primary care settings (Lowe et al., 2004; Richards et al., 2008). Alcohol use was measured by the Alcohol Use Disorders Identification Test (AUDIT; Saunders et al., 1993). Change in functional status was measured by the Short Form 12 (SF-12; Jenkinson et al., 1997), which assesses (1) physical functioning; (2) role-physical; (3) bodily pain; (4) general health; (5) vitality; (6) social functioning; (7) role-emotional; and (8) mental health. We computed the Physical and Mental Health Composite Scores from the 12 questions. Patient Satisfaction (at 2- and 4-month follow-up) was measured via two questions from the CAHPS-ECHO (AHRQ, 2003). Specifically, patients were asked, “Using any number from 0 to 10, where 0 is the worst mental health care possible and 10 is the best mental health care possible, what number would you use to rate the mental health care you received?” and “How much were you helped by the mental health care you received? Would you say not at all, a little, somewhat, or a lot?” We also collected baseline demographic information including age, gender, race, ethnicity, marital status, income, education, occupational status, and health insurance coverage.
Sample Size
We aimed to recruit 40–50 patients. However, due to FQHC constraints during the COVID-19 pandemic, we were only able to recruit 30 patients. Of note, N = 30 was the median sample size per arm for trials with continuous outcome measures in a review of 79 feasibility trials (Billingham et al., 2013).
Quantitative Methods
Descriptive statistics and unadjusted PCL-5 scores were used for primary outcomes of feasibility and acceptability.
Regulatory Approval
We received an IRB exempt determination from the University of Michigan, per the University of Michigan “flexibility initiative” Exemption 5 for State of Michigan projects, which extends federal exemption category 5 at 45 CFR 46.104(d) to cover public benefit and service programs sponsored by the State of Michigan. This exemption covers research and demonstration projects that are conducted or supported by a State of Michigan department or agency and that are designed to study, evaluate, improve, or otherwise examine public benefit or service programs. Although an exemption determination eliminated the need for ongoing IRB review and approval, this exemption still obligated the study team to abide by generally accepted principles of responsible and ethical conduct of research, as specified in the Belmont Report.
Results
Participant Flow
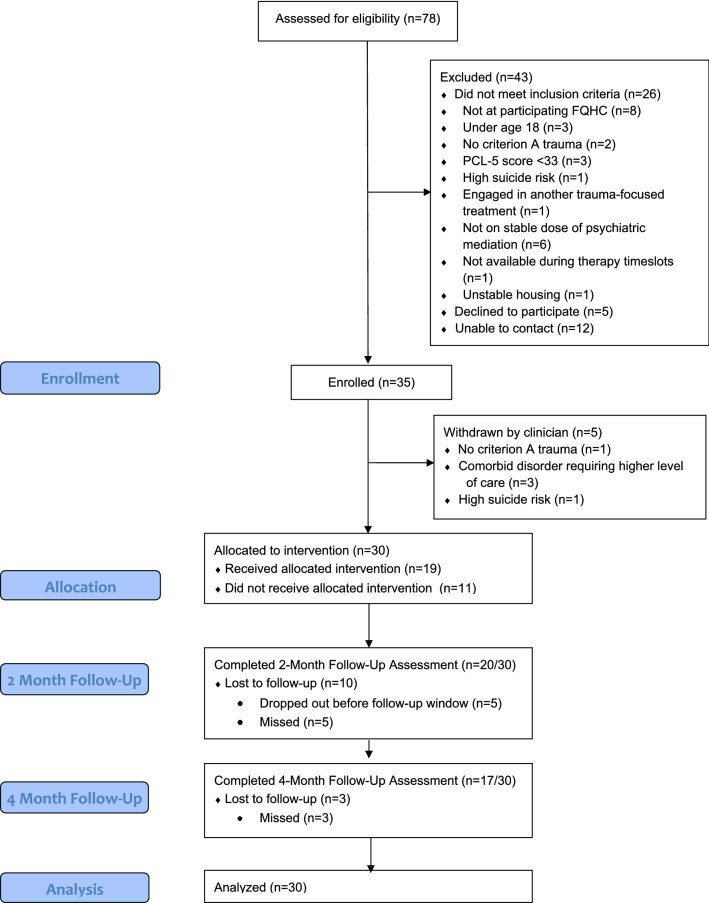
Participant flow is displayed in a CONSORT diagram (see Fig. 1). Seventy-eight patients were referred to the study and assessed for eligibility. Of those, 26 did not meet inclusion criteria, five declined to participate, and 12 could not be contacted for follow-up. Reasons for exclusion are listed in Fig. 1. Thirty-five patients were enrolled; however, five were removed by the study therapist prior to intervention initiation and were not included in the final analysis. Of these five patients, one did not have a Criterion A trauma, three had a comorbid condition requiring a higher level of care (active psychotic symptoms; severe emotion dysregulation), and one was deemed to be at high risk for suicide. Of the 30 patients allocated to the intervention, 19 initiated PE-PC and 11 dropped out prior to engaging in treatment. Twenty patients (67%) completed follow-up assessment at 2-months and 17 patients (57%) completed follow-up assessment at 4-months.
Fig. 1.
CONSORT diagram
Recruitment
Patients were recruited from December 2018 to July 2020 and follow-up was completed in November 2020.
Baseline Data
The sample was representative of the FQHC population (see Table 1): 70% were not employed, 67% reported an income below the federal poverty guideline, 77% received Medicaid and 13% were covered by Medicare. Patients were 83% female, 40% African-American, and 13% Hispanic. Mean age was 41. The majority of participants identified a childhood traumatic event as the index trauma (nine experienced childhood sexual abuse, three experienced another form of child abuse, and eight experienced the sudden accidental or violent death of a family member). Mean time since index trauma was 13.8 years (SD = 18.0). Mean baseline scores were 59.4 (SD = 9.0) on the PCL-5, 18.5 (SD = 4.9) on the PHQ-9, 6.0 (SD = 8.5) on the AUDIT, 44.2 (SD = 15.1) on the SF-12 Physical Composite and 27.2 (SD = 13.2) on the SF-12 Mental Health Composite. We compared baseline characteristics of those lost to follow-up versus those retained. Patients lost to follow-up at 2-months were more likely to be unemployed (p < 0.02, Fisher's exact test) and those lost to follow-up at 4-months were more likely to be receiving Medicare (p < 0.03, Fisher's exact test). There were no other differences in baseline characteristics.
Table 1.
Sample demographics (N = 30)
| Characteristic | n | % |
|---|---|---|
| Sex | ||
| Female | 25 | 83.3 |
| Male | 4 | 13.3 |
| Other | 1 | 3.3 |
| Age (mean ± SD) | 40.5 ± 15.0 | |
| Race | ||
| African-American | 12 | 40.0 |
| Caucasian | 14 | 46.7 |
| Multi-racial | 4 | 13.3 |
| Ethnicity | ||
| Hispanic or Latino | 4 | 13.3 |
| Non-Hispanic or Latino | 26 | 86.7 |
| Marital status | ||
| Single | 11 | 36.7 |
| Divorced/separated/widowed | 11 | 36.7 |
| Married/cohabiting | 8 | 26.7 |
| Education | ||
| No high school degree | 9 | 30.0 |
| Completed high school | 8 | 26.7 |
| Attended some college or higher | 13 | 43.3 |
| Employment status | ||
| Employed | 9 | 30.0 |
| Unemployed | 19 | 63.3 |
| Retired/student | 2 | 6.7 |
| Income | ||
| Below federal poverty guideline | 20 | 66.7 |
| Above federal poverty guideline | 7 | 23.3 |
| Don’t know | 3 | 10.0 |
| Insurance status | ||
| Medicaid | 23 | 76.7 |
| Medicare | 4 | 13.3 |
| Private health insurance | 5 | 16.7 |
Quantitative Outcomes and Estimation
The primary outcomes were feasibility and acceptability (Arain et al., 2010). Seventy-eight patients were screened and 35 (45%) met initial inclusion criteria. Only five patients (14%) declined participation; the most frequently identified barrier to participation was time constraints. Adherence of patients to the proposed treatment was measured via number of sessions attended. The overall average among the 30 enrolled patients was 2.6 sessions. For the 19 patients who attended at least 1 session, the average was 4.1 sessions. Loss to follow-up was 33% at 2 months and 43% at 4 months. Among those who attended at least one session, loss to follow-up was 26% at 2 months and 37% at 4 months. Patients who attended at least one session were asked to rate the care they received and indicate how much they were helped by the care, via two items from the CAHPS ECHO. On a scale of 0–10, care was rated at 8.8 (SD = 1.4) at 2-month follow up and 8.9 (SD = 1.6) at 4-month follow-up. Eighty-one percent of patients at 2-month follow-up said they were helped “a lot” by the care they received, as did 62% at 4-month follow-up.
We assessed PTSD symptoms via PCL-5 score at 2-month and 4-month follow-up among patients who engaged in at least 1 PE-PC session, unadjusted (raw) PCL-5 score was 60.9 (SD = 9.7) at baseline, 33 (SD = 19.8) at 2-month follow-up (Cohen’s d = 1.8), and 25.6 (SD = 22.8) at 4-month follow-up (Cohen’s d = 2.0). Among patients who did not engage in any PE-PC sessions, unadjusted (raw) PCL-5 score was 57.0 (SD = 7.5) at baseline, 40.5 (SD = 18.7) at 2-month follow-up (Cohen’s d = 1.2), and 46.0 (SD = 30.3) at 4-month follow-up (Cohen’s d = 0.50).
Fidelity Ratings
Therapist fidelity was rated via review of progress notes using Session-Specific Adherence Rating Scales. Each session was rated using four dichotomous items. The average adherence rating was 94%.
Adverse Events
No significant adverse events (e.g., suicide attempt, psychiatric hospitalization) were reported over the course of the study.
Qualitative Results
Patient Interviews: Experience of Treatment and Satisfaction with Treatment
All seven treatment engagers said that treatment was helpful and they would recommend it to others. Patients said that after treatment they felt less angry, fearful, and edgy; experienced fewer nightmares; felt calmer and more relaxed; felt more assertive; and were less avoidant. One patient stated, “you basically get your life back when you’re done.” Patients said that it was challenging, but beneficial. For example, one patient said, “It was harder than I thought it would be mentally, but in the end it seemed to help out more than I expected it to. So I was pretty glad I went through it despite how uncomfortable it made me at times.” Another said, “I felt like I was … I was kind of made to do it, even when I didn’t want to she would push me. So like even if I didn’t answer the question fully … she would push me to delve deeper into what I was trying to get across and in other therapies they really, they don’t seem to do that.” Three patients noted that the treatment compared favorably to other treatments they had received. For example, one said,
“I have been in other treatments and seen other therapists for PTSD and trauma and I usually quit going, it didn’t really seem it was serving much help or purpose but the way she kind of attacked it head on, it kind of really didn’t give me much chance to run, so I think the more aggressive helped out a little bit in this regard.”
Another said, “it seemed to help more than other treatments I’ve had because it was more focused and targeted. It was intense and short but it got to the point.” One patient specifically noted the benefit of practice: “the more you address it, the easier it is to say. The more it comes out the more weight is lifted... I’m able to talk about it without crying so much or getting so edgy – because I still read over it, and it’s still becoming easier and easier to read.” However, some noted that they did not complete homework on a regular basis. A couple of patients said they would have liked treatment to be longer or to have addressed more than one traumatic event. On the whole, patients were very satisfied with treatment.
Patient Interviews: Barriers to Treatment Engagement and Suggestions for Overcoming Barriers
Patient Non-engagers
Three interviewees were non-engagers, meaning they did not attend any PE-PC sessions after enrolling in the study. One patient reported that she was not able to participate due to other commitments, including school and preexisting psychotherapy appointments: “I had a little bit of stuff on my plate, and I couldn’t do everything at one time.” Two patients reported that they did not own vehicles. One patient stated she did not like discussing her traumatic experiences. One patient recommended having therapists come to the patient’s home to provide treatment. Of note, this recommendation was given prior to the onset of the COVID-19 pandemic.
Patient Engagers
Six patients noted lack of time was a barrier to treatment. These patients cited competing demands of work, school, and childcare. Lack of time was cited as a barrier to scheduling visits, as well as to completing homework associated with treatment: “I would usually do it [the homework] on my lunch break in my car. But then that was difficult because then I have to go back to work after rehashing all these memories.” For this patient, the barrier was lack of time to decompress after completing the therapy homework. One patient who was unemployed stated that having a job while doing PE-PC would have added stress that would have caused her to discontinue treatment: “I would have had to give up on one of the two—the job or the PTSD study would have had to go.” Three individuals described their PTSD itself (specifically avoidance symptoms) as a barrier. One patient noted that she was afraid to go to her appointments by herself. Patients reported that paying for treatment was not a barrier, in part because PE-PC was provided to them free of charge and Medicaid covered other treatment for many patients. However, half of patients shared that paying for treatment had been an issue in the past. For some individuals, when insurance ran out or they did not have money for copayments in the past, they stopped going to treatment. One patient shared that she had a previous experience of receiving a surprise bill from an insurance company that caused her to avoid therapy for several years for fear this would happen again. Three patients cited childcare as a barrier while four stated it was not a barrier. One individual reported that if the treatment were not offered as telehealth to home, she would not have been able to attend due to childcare needs. Three patients stated that transportation was a barrier, while four stated it was not. However, several patients reported relying on public transportation or others for rides. One patient suggested home pick up for treatment, especially in the winter, as a way to get patients to start and stay in PTSD treatment. Several patients described technology or logistics challenges: “it was like they would forget about me—wouldn’t call me back to the room. So several times I had to call the therapist from my phone and do it over the phone rather than on the tablet.” Patients recommended more preparation ahead of the appointment time (e.g., making sure that technology worked, timing worked, and ensuring there was a comfortable room for the session). Overall, despite these challenges, patients appreciated the flexibility of being able to attend sessions from home or from their clinic.
Provider Interviews: Patient Needs and Resources
Providers noted that trauma and PTSD were highly prevalent in their patient population: “[PE-PC] meets the needs very well, especially because most of my patients have some form of trauma.” Several indicated a need for targeted PTSD treatment. One provider observed, “We see a lot of PTSD—every behavioral health provider here has a good number of PTSD patients on their caseload. Even in our school-based clinics. More trauma than we ever expected to see.” Another noted that “trauma treatment is definitely needed, especially in community mental health.” Several providers mentioned that transportation was a major barrier for their patients, echoing the concern of some patients. Providers described their patient population as low-income and underserved. One provider noted, “people here are living in extreme, extreme poverty. Lots of socioeconomic issues.” Because of this, two providers noted that patients sometimes had difficulty attending their appointments. As one provider stated, “you know, Maslow’s hierarchy of needs—they have no food; they have no shelter; no safety. So you’re prioritizing—okay, do I eat today, or do I go to see < my PE-PC therapist > ?” When basic needs were unmet, they needed to be prioritized over psychotherapy. Despite this caveat, all providers acknowledged a need for PTSD treatment in their clinics.
Provider Interviews: Tension for Change
Most providers indicated a need for additional PTSD treatment options. One provider described this as a “desperate need” for PTSD treatment at his clinic. Another stated, “any form of trauma therapy I think needs to be implemented—it’s needed.” One provider observed, “I definitely need more tools to deal with trauma.” Several providers shared that there was no set standard for PTSD treatment. One provider said her clinic had completed training in another trauma-focused treatment, but not a brief treatment. She said, “there’s definitely an understanding of treatment and trauma. But there’s always room to expand skills—learn new techniques and skills.” The majority of providers said that they would like to receive training in PE-PC and believed their colleagues would as well.
Provider Interviews: Compatibility
Providers reported that PE-PC was overall compatible with their sites, but noted several ways in which it could be adapted to fit better. For example, providers had varying perspectives on having therapy delivered by telehealth (either to their clinic or directly to the patient’s home). One noted that having telehealth to the home would be tremendously helpful for patients without means of reliable transportation. However, two providers believed in-person care was best. Generally, providers agreed that either telehealth or in-person care would be a good resource for their patients. Two providers mentioned that PE-PC asks patients to focus on one specific trauma, but many of their patients had complex/numerous traumas. PE-PC, as a brief treatment, may not be sufficient for some patients with multiple traumas that they wish to address. A stepped-care model might be beneficial for these patients. Providers also raised the issue of PE-PC session length. Since PE-PC was explicitly designed for the primary care setting, sessions are designed to be 30 min long. A couple of providers noted that 30-min sessions were advantageous, but one noted that patients expected longer sessions: “With some of our appointments, we have gone down from 45 to 30 min, so on some level a little bit of resistance from patients and providers who are used to longer appointments. [It would be useful to have] a level of education on how this could be effective even though it’s brief.” For settings that are able to offer longer sessions, a version of PE-PC with sessions formatted to 45 min might be beneficial.
Provider Interviews: Available Resources
Providers mentioned several constraints to PTSD treatment delivery, including busy schedules and the opportunity cost of therapy training and consultation. When asked about their interest in learning to provide PE-PC to their patients, two providers cited their busy schedules as a barrier. One provider mentioned that social workers are “three months out” for accepting patients for therapy, and that his clinic often has to refer behavioral healthcare out to other agencies. He observed that even when patients are able schedule an appointment, they frequently cannot attend due to transportation problems, which leads to a high cancellation rate and reduced efficiency. Another provider noted that she was “scheduled out for two months,” so trying to take new cases would be very difficult. Although the majority of providers expressed interest in receiving training in PE-PC, some mentioned that the time (and potential cost) required for training would be burdensome for their clinics. One provider stated he would love to have additional training, but did not believe his supervisor would support it because it would pull him away from his caseload and normal routine. Another noted that she would like to learn another trauma-focused treatment, but that these trainings are too expensive. One supervisor reported that her behavioral health providers have expressed interest in trauma-focused treatment and that her site has enough resources for some of the trainings, but not all. “I had three requests in the past week for continued certification in those areas. Some of the briefer ones we could accommodate, but there are some that are a little more expensive and lengthy—we’d have to look at that further to see how we would do that.” She stated that participating in trainings during the summer would be easier to accommodate because school is not in session and therapist caseloads are not as full. In summary, providers were interested in PE-PC training, but would require protected time for training and scheduling new patients.
Discussion
This study tested the feasibility and acceptability of PE-PC as delivered to 30 low-income patients in Michigan FQHCs. We interviewed 10 patients and five providers about their perceptions of the intervention and assessed PTSD symptoms at two- and four- months post-enrollment. We found that PE-PC was feasible according to primary outcome measures. Among eligible patients, 87.5% agreed to participate in the study and 63% of participants allocated to intervention initiated PE-PC. Therapy attendance was high among patients who attended at least one session. Loss to follow-up was moderate, but better among those who attended at least one session. Overall, patients reported they found treatment very helpful. Feedback from interviews indicated that the intervention was beneficial and filled a critical gap in PTSD services at FQHCs. A fully-powered randomized controlled trial is now needed to test the effectiveness of PE-PC in the FQHC setting.
One of the primary goals of this study was to determine patient and provider perspectives on feasibility and acceptability of PE-PC in the FQHC setting. To that end, we conducted semi-structured interviews with 10 patients (seven treatment engagers and three non-engagers) and five providers. These interviews support the acceptability of treatment and provide additional data on barriers and facilitators to implementation for low-income individuals served in FQHCs. Identified facilitators included the perceived effectiveness of the intervention from the patient and provider perspective and the flexibility of receiving the intervention in the FQHC or in the patient’s home, by telehealth. In terms of barriers, patients noted that time constraints, transportation, paying for treatment, and technological difficulties made it more difficult to engage in PE-PC or other PTSD treatment. Providers echoed that transportation and technological difficulties were barriers for patients. They also stated that time constraints made it difficult for them to take on new patients and/or devote time to PE-PC training and consultation. Offering both in-person and telehealth options for PE-PC may be one way to alleviate transportation difficulties for patients, although internet-related constraints among this primarily rural and low-income population require careful consideration. Many providers wished to receive training in PE-PC, which would expand availability of care. Low-burden ways to provide training and consultation would be beneficial. Although these efforts would require upfront investment of resources, treating PTSD more efficiently would be advantageous in the long run.
Although PE-PC has demonstrated preliminary evidence of effectiveness, there will certainly be patients that require additional or more intensive PTSD treatment. Future directions for this work include testing PE-PC as part of a stepped-care treatment sequence in which those who do not fully respond to PE-PC are stepped up to Standard PE or another first-line PTSD treatment. Our data also demonstrate the feasibility of delivering PE-PC directly to the patient’s home. Since telehealth-delivered psychotherapy interventions were made fully reimbursable in the state of Michigan shortly before the COVID-19 pandemic, this practice could potentially be continued past the end of the pandemic. Although PE-PC was delivered by University of Michigan telepsychologists in this pilot, FQHC providers could be trained to deliver PE-PC using the established training model designed for the primary care setting. Training requires a four-hour initial workshop and eight hours of subsequent consultation (delivered in weekly, 30-min consultation sessions over the course of 4–6 months). The authors have successfully trained generalist community providers in PE-PC.
Findings from this study should be interpreted in the context of several limitations. First, we lacked a control condition. However, these data were collected as part of a quality improvement project funded by the Michigan Department of Health and Human Services, and as such, randomization was not permitted. Another limitation was the small sample size, which was caused in part by the onset of the COVID-19 pandemic. Many of the participating clinics shut down during the initial months of the pandemic, and those that did not, redirected all resources to essential services. Consequently, referrals to PE-PC declined tremendously during the last eight months of the study. However, previously enrolled patients were able to continue with treatment via telehealth visits to their clinic (if it was still open) or to their home (with clinic approval). Given the challenges that we encountered with recruitment, we plan to refine our processes in order to reach more patients in the future. We intend to establish a referral process that allows for the exchange of identifiable data with the clinics so that we can reach out directly to patients when they express interest in treatment. We will attempt to reduce the time burden imposed on clinic staff and therapists for coordinating visits, rooming patients, and setting up video visits. We will offer treatment both in-person and through telehealth, depending on patient preference. Continuing to provide a telehealth option will help address the logistical barriers and time constraints cited by patients. Most importantly, we will work to train FQHC therapists to provide treatment themselves so that PE-PC can become integrated into regular clinical practice. To improve retention in follow-up assessments, we will now reach out to participants through multiple modalities (e.g., phone, text, email, or social media) and maintain engagement with participants throughout the follow-up period.
In conclusion, these data support the feasibility of delivering PE-PC to FQHC patients via telehealth. We found high rates of therapy attendance and treatment satisfaction, and moderate rates of follow-up. A planned full-scale randomized trial will be used to determine the effectiveness of PE-PC in reducing PTSD symptoms in this setting. Adapted brief evidence-based interventions for PTSD are scalable and require fewer resources than standard treatments, allowing for improved treatment access and efficiency. This innovative approach has the potential to improve the efficiency of PTSD treatment while maximizing effectiveness.
Acknowledgements
The authors wish to thank Ms. Courtney Miller, Ms. Cassuandra Peterson, and Ms. Murphy Van Sparrentak for their assistance with this study.
Author Contributions
Drs. RKS, KMA, JAC, and SAMR contributed to the study conception and design. Data collection, data curation, and data analysis were performed by Ms. HMW and Ms. DG. The first draft of the manuscript was written by Dr. RKS and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Funding
This work was supported by the Center of Medicare and Medicaid Services through the Michigan Department of Health and Human Services and by the Frances and Kenneth Eisenberg Collaborative Innovation Award, University of Michigan Depression Center, to Dr. Sripada (Project Number MA No. 20200032-00/PN E20202413-00). Dr. Sripada is supported by CDA 15-251, IK2 HX-002095-01 from the United States (U.S.) Department of Veterans Affairs Health Services R&D (HSRD) Service. These funding sources had no involvement in the analysis, interpretation of data, or writing of this report.
Declarations
Conflicts of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical Approval
The study received an IRB exempt determination from the University of Michigan. The study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Clinical Trial Registration
ClinicalTrials.gov Identifier: NCT03711266. October 18, 2018.
Consent to Participate
Verbal informed consent was obtained prior to participation. We followed the Transparent Reporting of Evaluations with Non-randomized Designs (TREND) statement (Des Jarlais, Lyles, Crepaz, & Group, 2004) in reporting methods and results of this study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Acierno R, Knapp R, Tuerk P, Gilmore AK, Lejuez C, Ruggiero K, Muzzy W, Egede L, Hernandez-Tejada MA, Foa EB. A non-inferiority trial of Prolonged Exposure for posttraumatic stress disorder: In person versus home-based telehealth. Behaviour Research and Therapy. 2017;89:57–65. doi: 10.1016/j.brat.2016.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adler DA, Possemato K, Mavandadi S, Lerner D, Chang H, Klaus J, Tew JD, Barrett D, Ingram E, Oslin DW. Psychiatric status and work performance of veterans of Operations Enduring Freedom and Iraqi Freedom. Psychiatric Services (washington, D. C.) 2011;62(1):39–46. doi: 10.1176/ps.62.1.pss6201_0039. [DOI] [PubMed] [Google Scholar]
- AHRQ. (2003). CAHPS Mental Health Care Surveys. Content last reviewed February 2019. Rockville, MD: Agency for Healthcare Research and Quality. Retrieved from https://www.ahrq.gov/cahps/surveys-guidance/echo/index.html.
- APA. (2017). Clinical practice guideline for the treatment of posttraumatic stress disorder (PTSD) in adults. American Psychological Association Guideline Development Panel for the Treatment of PTSD in Adults.
- Arain M, Campbell MJ, Cooper CL, Lancaster GA. What is a pilot or feasibility study? A review of current practice and editorial policy. BMC Medical Research Methodology. 2010;10:67. doi: 10.1186/1471-2288-10-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Billingham SA, Whitehead AL, Julious SA. An audit of sample sizes for pilot and feasibility trials being undertaken in the United Kingdom registered in the United Kingdom Clinical Research Network database. BMC Medical Research Methodology. 2013;13:104. doi: 10.1186/1471-2288-13-104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blevins CA, Weathers FW, Davis MT, Witte TK, Domino JL. The posttraumatic stress disorder checklist for DSM-5 (PCL-5): Development and initial psychometric evaluation. Journal of Traumatic Stress. 2015;28(6):489–498. doi: 10.1002/jts.22059. [DOI] [PubMed] [Google Scholar]
- Bonanno GA, Galea S, Bucciarelli A, Vlahov D. What predicts psychological resilience after disaster? The role of demographics, resources, and life stress. Journal of Consulting and Clinical Psychology. 2007;75(5):671. doi: 10.1037/0022-006X.75.5.671. [DOI] [PubMed] [Google Scholar]
- Bovin MJ, Marx BP, Weathers FW, Gallagher MW, Rodriguez P, Schnurr PP, Keane TM. Psychometric properties of the PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders-Fifth Edition (PCL-5) in veterans. Psychological Assessment. 2016;28(11):1379. doi: 10.1037/pas0000254. [DOI] [PubMed] [Google Scholar]
- Byers AL, Covinsky KE, Neylan TC, Yaffe K. Chronicity of posttraumatic stress disorder and risk of disability in older persons. JAMA Psychiatry. 2014 doi: 10.1001/jamapsychiatry.2014.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cigrang JA, Rauch SA, Mintz J, Brundige AR, Mitchell JA, Najera E, Litz BT, Young-McCaughan S, Roache JD, Hembree EA, Goodie JL. Moving effective treatment for posttraumatic stress disorder to primary care: A randomized controlled trial with active duty military. Families, Systems & Health. 2017;35(4):450–462. doi: 10.1037/fsh0000315. [DOI] [PubMed] [Google Scholar]
- Cusack K, Jonas DE, Forneris CA, Wines C, Sonis J, Middleton JC, Feltner C, Brownley KA, Olmsted KR, Greenblatt A, Weil A. Psychological treatments for adults with posttraumatic stress disorder: A systematic review and meta-analysis. Clinical Psychology Reviews. 2016;43:128–141. doi: 10.1016/j.cpr.2015.10.003. [DOI] [PubMed] [Google Scholar]
- Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: A consolidated framework for advancing implementation science. Implementation Science. 2009;4:50. doi: 10.1186/1748-5908-4-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Des Jarlais DC, Lyles C, Crepaz N, Group T. Improving the reporting quality of nonrandomized evaluations of behavioral and public health interventions: The TREND statement. American Journal of Public Health. 2004;94(3):361–366. doi: 10.2105/ajph.94.3.361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finley EP, Noël PH, Lee S, Haro E, Garcia H, Rosen C, Bernardy N, Pugh MJ, Pugh JA. Psychotherapy practices for veterans with PTSD among community-based providers in Texas. Psychological Services. 2018;15(4):442–452. doi: 10.1037/ser0000143. [DOI] [PubMed] [Google Scholar]
- Foa EB, Hembree EA, Cahill SP, Rauch SAM, Riggs DS, Feeny NC, Yadin E. Randomized trial of prolonged exposure for posttraumatic stress disorder with and without cognitive restructuring: Outcome at academic and community clinics. Journal of Consulting and Clinical Psychology. 2005;73(5):953–964. doi: 10.1037/0022-006X.73.5.953. [DOI] [PubMed] [Google Scholar]
- Foa EB, Hembree EA, Rothbaum BO. Prolonged exposure therapy for PTSD: Therapist guide. Oxford University Press; 2007. [Google Scholar]
- Forman-Hoffman V, Middleton JC, Feltner C, Gaynes BN, Weber RP, Bann C, Viswanathan M, Lohr KN, Baker C, Green J. Psychological and pharmacological treatments for adults with posttraumatic stress disorder: A systematic review update. Agency for Healthcare Research and Quality; 2018. [PubMed] [Google Scholar]
- Fortney JC, Heagerty PJ, Bauer AM, Cerimele JM, Kaysen D, Pfeiffer PN, Zielinski MJ, Pyne JM, Bowen D, Russo J, Ferro L. Study to promote innovation in rural integrated telepsychiatry (SPIRIT): Rationale and design of a randomized comparative effectiveness trial of managing complex psychiatric disorders in rural primary care clinics. Contemporary Clinical Trials. 2020;90:105873. doi: 10.1016/j.cct.2019.105873. [DOI] [PubMed] [Google Scholar]
- Gale RC, Wu J, Erhardt T, Bounthavong M, Reardon CM, Damschroder LJ, Midboe AM. Comparison of rapid vs in-depth qualitative analytic methods from a process evaluation of academic detailing in the Veterans Health Administration. Implementation Science. 2019;14(1):11. doi: 10.1186/s13012-019-0853-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein RB, Smith SM, Chou SP, Saha TD, Jung J, Zhang H, Pickering RP, Ruan W, Huang B, Grant BF. The epidemiology of DSM-5 posttraumatic stress disorder in the United States: Results from the National Epidemiologic Survey on Alcohol and Related Conditions-III. Social Psychiatry and Psychiatric Epidemiology. 2016;51(8):1137–1148. doi: 10.1007/s00127-016-1208-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greene T, Neria Y, Gross R. Prevalence, detection and correlates of PTSD in the primary care setting: A systematic review. Journal of Clinical Psychology in Medical Settings. 2016;23(2):160–180. doi: 10.1007/s10880-016-9449-8. [DOI] [PubMed] [Google Scholar]
- Hale AC, Sripada RK, Bohnert KM. Past-year treatment utilization among individuals meeting dsm-5 ptsd criteria: Results from a nationally representative sample. Psychiatric Services (washington, D. C.) 2018;69(3):341–344. doi: 10.1176/appi.ps.201700021. [DOI] [PubMed] [Google Scholar]
- ISTSS. (2020). Effective treatments for PTSD: practice guidelines from the International Society for Traumatic Stress Studies (D. Forbes, J. I. Bisson, C. M. Monson, & L. Berliner Eds. 3rd ed.): Guilford Press.
- Jain S, Ortigo K, Gimeno J, Baldor DA, Weiss BJ, Cloitre M. A Randomized Controlled Trial of Brief Skills Training in Affective and Interpersonal Regulation (STAIR) for Veterans in Primary Care. Journal of Traumatic Stress. 2020;33(4):401–409. doi: 10.1002/jts.22523. [DOI] [PubMed] [Google Scholar]
- Jenkinson C, Layte R, Jenkinson D, Lawrence K, Petersen S, Paice C, Stradling J. A shorter form health survey: Can the SF-12 replicate results from the SF-36 in longitudinal studies? Journal of Public Health. 1997;19(2):179–186. doi: 10.1093/oxfordjournals.pubmed.a024606. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lancaster GA, Dodd S, Williamson PR. Design and analysis of pilot studies: Recommendations for good practice. Journal of Evaluation in Clinical Practice. 2004;10(2):307–312. doi: 10.1111/j.2002.384.doc.x. [DOI] [PubMed] [Google Scholar]
- Lang AJ, Stein MB. An abbreviated PTSD checklist for use as a screening instrument in primary care. Behaviour Research and Therapy. 2005;43(5):585–594. doi: 10.1016/j.brat.2004.04.005. [DOI] [PubMed] [Google Scholar]
- Liu N, Zhang F, Wei C, Jia Y, Shang Z, Sun L, Wu L, Sun Z, Zhou Y, Wang Y, Liu W. Prevalence and predictors of PTSS during COVID-19 Outbreak in China Hardest-hit Areas: Gender differences matter. Psychiatry Research. 2020;287:112921. doi: 10.1016/j.psychres.2020.112921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowe B, Unutzer J, Callahan CM, Perkins AJ, Kroenke K. Monitoring depression treatment outcomes with the patient health questionnaire-9. Medical Care. 2004;42(12):1194–1201. doi: 10.1097/00005650-200412000-00006. [DOI] [PubMed] [Google Scholar]
- McGinty EE, Presskreischer R, Anderson KE, Han H, Barry CL. Psychological distress and COVID-19-related stressors reported in a longitudinal cohort of US adults in April and July 2020. JAMA. 2020;324(24):2555–2557. doi: 10.1001/jama.2020.21231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MDHHS. (2020). MDHHS Bulletin MSA 20-09; General Telemedicine Policy Changes; Updates to Existing Policy; Federally Qualified Health Center and Rural Health Clinic Policy Changes.
- Meredith LS, Eisenman DP, Green BL, Basurto-Davila R, Cassells A, Tobin J. System factors affect the recognition and management of posttraumatic stress disorder by primary care clinicians. Medical Care. 2009;47(6):686–694. doi: 10.1097/MLR.0b013e318190db5d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meredith LS, Eisenman DP, Han B, Green BL, Kaltman S, Wong EC, Sorbero M, Vaughan C, Cassells A, Zatzick D, Diaz C. Impact of collaborative care for underserved patients with PTSD in primary care: A randomized controlled trial. Journal of General Internal Medicine. 2016;31(5):509–517. doi: 10.1007/s11606-016-3588-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morland LA, Mackintosh MA, Glassman LH, Wells SY, Thorp SR, Rauch SA, Cunningham PB, Tuerk PW, Grubbs KM, Golshan S, Sohn MJ. Home-based delivery of variable length prolonged exposure therapy: A comparison of clinical efficacy between service modalities. Depression and Anxiety. 2020;37(4):346–355. doi: 10.1002/da.22979. [DOI] [PubMed] [Google Scholar]
- Morland LA, Mackintosh MA, Greene CJ, Rosen CS, Chard KM, Resick P, Frueh BC. Cognitive processing therapy for posttraumatic stress disorder delivered to rural veterans via telemental health: A randomized noninferiority clinical trial. Journal of Clinical Psychiatry. 2014;75(5):470–476. doi: 10.4088/JCP.13m08842. [DOI] [PubMed] [Google Scholar]
- Morland LA, Mackintosh MA, Rosen CS, Willis E, Resick P, Chard K, Frueh BC. Telemedicine versus in-person delivery of cognitive processing therapy for women with posttraumatic stress disorder: A randomized noninferiority trial. Depression and Anxiety. 2015;32(11):811–820. doi: 10.1002/da.22397. [DOI] [PubMed] [Google Scholar]
- Nock MK, Stein MB, Heeringa SG, Ursano RJ, Colpe LJ, Fullerton CS, Hwang I, Naifeh JA, Sampson NA, Schoenbaum M, Zaslavsky AM. Prevalence and correlates of suicidal behavior among soldiers: Results from the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS) JAMA Psychiatry. 2014;71(5):514–522. doi: 10.1001/jamapsychiatry.2014.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rauch SA, Kim HM, Powell C, Tuerk PW, Simon NM, Acierno R, Allard CB, Norman SB, Venners MR, Rothbaum BO, Stein MB. Efficacy of prolonged exposure therapy, sertraline hydrochloride, and their combination among combat veterans with posttraumatic stress disorder: A randomized clinical trial. JAMA Psychiatry. 2019;76(2):117–126. doi: 10.1001/jamapsychiatry.2018.3412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rauch SAM, Simon NM, Rothbaum BO. Rising tide: Responding to the mental health impact of the COVID-19 pandemic. Depression and Anxiety. 2020;37(6):505–509. doi: 10.1002/da.23058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richards DA, Lovell K, Gilbody S, Gask L, Torgerson D, Barkham M, Bland M, Bower P, Lankshear AJ, Simpson A, Fletcher J. Collaborative care for depression in UK primary care: A randomized controlled trial. Psychological Medicine. 2008;38(2):279–287. doi: 10.1017/S0033291707001365. [DOI] [PubMed] [Google Scholar]
- Ruzek JI, Rosen RC. Disseminating evidence-based treatments for PTSD in organizational settings: A high priority focus area. Behaviour Research and Therapy. 2009;47(11):980–989. doi: 10.1016/j.brat.2009.07.008. [DOI] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, De la Fuente JR, Grant M. Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption-II. Addiction. 1993;88(6):791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Schnurr PP, Lunney CA, Bovin MJ, Marx BP. Posttraumatic stress disorder and quality of life: Extension of findings to veterans of the wars in Iraq and Afghanistan. Clinical Psychology Review. 2009;29(8):727–735. doi: 10.1016/j.cpr.2009.08.006. [DOI] [PubMed] [Google Scholar]
- Smith AM, Stewart K, Baul T, Valentine SE. Peer delivery of a brief cognitive-behavioral treatment for posttraumatic stress disorder: A hybrid effectiveness-implementation pilot study. Journal of Clinical Psychology. 2020;76(12):2133–2154. doi: 10.1002/jclp.23020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sripada RK, Pfeiffer PN, Rauch SAM, Bohnert KM. Social support and mental health treatment among persons with PTSD: Results of a Nationally Representative Survey. Psychiatric Services (washington, D. C.) 2015;66(1):65–71. doi: 10.1176/appi.ps.201400029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- VA, DoD . US Department of Veterans Affairs & Department of Defense. VA/DoD clinical practice guideline for the management of posttraumatic stress disorder and acute stress disorder. VA/DoD; 2017. [Google Scholar]
- Weathers, F. W., Litz, B. T., Keane, T. M., Palmieri, P. A., Marx, B. P., & Schnurr, P. P. (2013). The PTSD Checklist for DSM-5 (PCL-5). Scale available from the National Center for PTSD.
- Wolitzky-Taylor K, Zimmermann M, Arch JJ, De Guzman E, Lagomasino I. Has evidence-based psychosocial treatment for anxiety disorders permeated usual care in community mental health settings? Behaviour Research and Therapy. 2015;72:9–17. doi: 10.1016/j.brat.2015.06.010. [DOI] [PubMed] [Google Scholar]