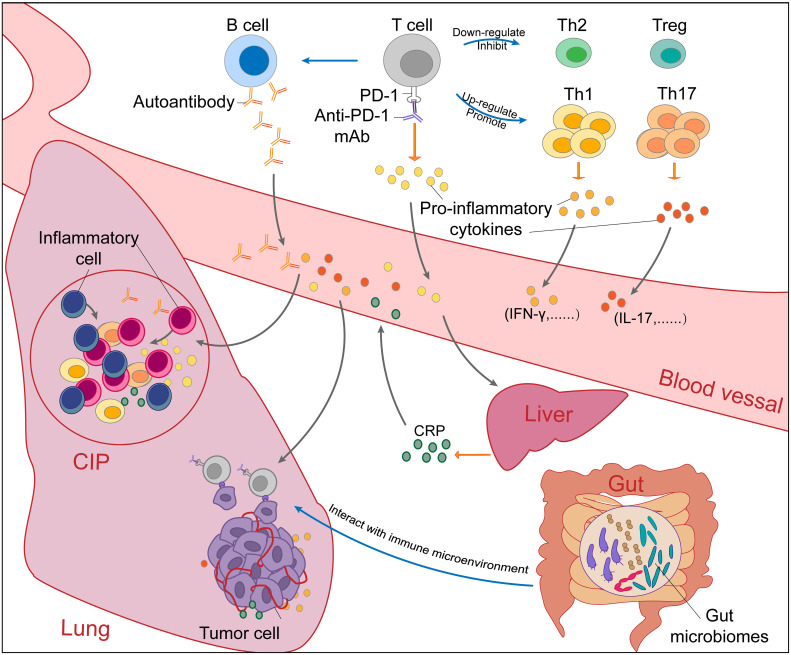
Figure 2.
The potential mechanisms of checkpoint inhibitor pneumonitis (CIP) in NSCLC patients receiving PD-1/PD-L1 inhibitor monotherapy. The occurrence of checkpoint inhibitor pneumonitis (CIP) in NSCLC is the result of a combination of many factors. Blockade of the PD-1-PD-L1 pathway by PD-1/PD-L1 mAbs (PD-1 mAb in the figure, for example) will upregulate and promote Th1 and Th17 cells and downregulate and inhibit Th2 cells and Tregs. Without immunosuppression of Th2 cells and Tregs, excessive immune responses and cytokine secretion of Th1 and Th17 cells will cause autoimmune damage in normal tissues such as the lung. In addition, autoantibodies increased after PD-1/PD-L1 blockade can also cause normal tissue lesions. Proinflammatory cytokines secreted by activated T cells promote the infiltration of inflammatory cells. Under the stimulation of IL-6, CRP produced by the liver will promote inflammation and strengthen autoimmunity. Through the “gut-lung axis”, gut microbiomes can regulate the immune microenvironment in the lung. Overall, the immune dysregulation caused by PD-1/PD-L1 blockade leads to the occurrence and development of CIP. NSCLC, non-small cell cancer; CIP, checkpoint inhibitor pneumonitis; PD-1, programmed cell death protein 1; PD-L1, programmed cell death protein ligand-1; mAbs, monoclonal antibody; Th, helper T cell; IL, Interleukin; CRP, C-reactive protein.