Abstract
Background
Neutrophil gelatinase-associated lipocalin (NGAL) is not only a bone-derived factor involved in metabolism, but also a biomarker of kidney disease and cardiovascular pathophysiology. We conducted this cross-sectional observational study to explore relationships between plasma NGAL and thoracic aorta calcification (TAC) in maintenance hemodialysis (MHD) patients with and without diabetes.
Methods
Plasma NGAL was measured by ELISA, TAC was evaluated via computed tomography scan using a 3D quantification method or chest radiography aortic arch calcification score. Spearman correlation, Logistic regression and Partial correlation analysis were used to describe the correlations between NGAL and TAC.
Results
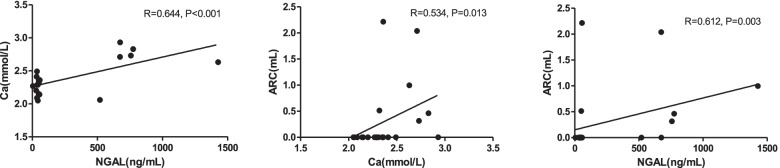
Plasma NGAL levels were lower in MHD patients with diabetes compared to those without diabetes (49.33(42.37, 55.48) vs 56.78(44.37, 674.13) ng/mL, P = 0.026). In MHD patients without diabetes, lg (NGAL) was positively correlated with ARC value(R = 0.612, P = 0.003) analyzed by Spearman correlation; for partial correlation analysis, lg (NGAL) was positively correlated with ARC value, after adjusting for age and sex (R = 0.550, P = 0.015), adjusting for age, sex and CHD (R = 0.565, P = 0.015), adjusting for age, sex, CHD and Alb (R = 0.536, P = 0.027), or adjusting for age, sex, CHD, Alb, and dialyzer membrane (polysulfone) (R = 0.590, P = 0.016); however, when adjusting for age, sex, CHD, Alb and Ca, the correlation between lg (NGAL) and ARC value disappeared. Positive correlation were found between NGAL and Ca (R = 0.644, P < 0.001), Ca and ACR (R = 0.534, P = 0.013) in Spearman coefficient analysis.
Conclusion
There were positive correlations among plasma NGAL, serum Ca and ARC in MHD patients without diabetes; which suggests that NGAL is possibly a participant in cardiovascular calcification, in non-diabetic MHD.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12882-022-02773-z.
Keywords: Neutrophil gelatinase-associated lipocalin, Thoracic aorta calcification, Maintenance hemodialysis, Diabetes
Background
NGAL, also known as 24p3 or lipocalin2, is a 25-kDa secretory protein, which has been found to be involved in numerous functions such as bacteriostasis, iron trafficking, metabolic regulation, chemotaxis, differentiation, proliferation and so on [1–4]. Under basal conditions, NGAL is mainly expressed by osteoblasts and has been identified as a bone-derived hormone involved in appetite control and metabolism [5]. In pathological states, the expression of NGAL can be induced in many other cells and tissues [6, 7], including neutrophil granules [8], macrophages [9], dendritic cells [10], adipocytes [6, 11], cardiomyocytes [12], smooth muscle cells [7], neurons [13], liver [14] and so on. Evidence from both mouse and human studies demonstrates that NGAL is highly expressed in damaged kidney tubule cells, and it is widely accepted as one of the optimal biomarkers for kidney injury [15–17]. Moreover, NGAL is also a biomarker for cardiovascular disease [18], such as heart failure, coronary artery disease (CAD), abdominal aortic aneurysm (AAA). Our previous study [19] has demonstrated that “plasma NGAL is positively associated with parameters of CKD-MBD such as calcium (Ca), alkaline phosphatase (ALP) in maintenance hemodialysis patients (MHD)”. However, few data are available on the possible relationship between NGAL and vascular calcification, which is a common and intractable character of CKD-MBD; so we conducted this study to explore the association between plasma NGAL and thoracic aorta calcification in MHD patients. Considering that lots of studies have suggested that NGAL is closely related to diabetes and insulin resistance [18], patients were divided to 2 groups according to with or without diabetes for subgroup analysis.
Methods
Study population and data source
Stable adult MHD patients with available plasma samples and chest radiography or computed tomography (CT) in our center from July 2019 to December 2020 were included in the cross-sectional observational study. Inclusion criteria were age ≥ 18 years and underwent MHD for at least 3 months; exclusion criteria were Kt/V < 1.2, hospitalization within 3 months before enrollment, cancer, active inflammation, or high serum C-reactive protein. This study was approved by the Ethics Committee of the First Affiliated Hospital of Shandong First Medical University, and all subjects gave their informed consent.
Demographic and clinical characteristics were collected from medical records as we have described before [19]. In detail, demographic factors (age, sex, vintage); smoking, residual urine volume, blood pressure, comorbid coronary heart disease (CHD) or not,comorbid diabetes or not; serum Ca, phosphate (P), iPTH, ALP, potassium(K), carbonate ion (HCO3-), urea nitrogen (BUN), creatinine (Cr), albumin (Alb), low density lipoprotein (LDL), triglyceride (TG) and ferritin (SF); blood hemoglobin (Hb), white blood cells (WBC) and platelet (PLT). Prescription drugs for CKD-MBD and arteriosclerosis were also collected, including calcium free phosphorus binders (sevelamer or lanthanum carbonate), calciums, active vitamin D, paricalcitol and statins.
Detection of plasma NGAL and klotho
Blood samples were collected and detected as previously described [19]. Blood samples were drawn from the dialysis pipeline immediately after initiation of single hemodialysis treatment. The plasma were multiple aliquoted after centrifugation and stored at − 80 °C until use. The concentrations of NGAL and Klotho were measured by ELISA Kit (Sandwich-ELISA Systems, Elabscience, China) with intra-assay and inter-assay CVs of less than 5 and 8%, respectively.
Assessment of thoracic aorta calcification
Thoracic aorta calcification (TAC) was evaluated via chest computed tomography (CT) or routine chest radiography [20–22]. Thoracic aorta calcium was estimated by CT in mediastinal window with slice is 1.25 mm: calcification volume was quantified by extracting the aorta calcium with density ≥ 130 HU from the volume-rendered image under the assistance of semi-automatic software; thoracic aorta was divided into 4 sites, aortic root calcium (ARC), ascending aorta calcium (ATAC), aortic arch calcium (AAC), descending thoracic aorta calcium (DTAC) and total calcium (TC) were all calculated. AAC by routine chest radiography: the circumferences of aortic arch was divided into 16 sites, the number of sectors with calcification was counted and divided by 100 to express the results as a percentage.
Statistical analyses
Categorical data are presented as frequencies and percentages. Continuous variables are expressed as mean ± standard deviation (SD) for normally distributed variables and as median (interquartile range [IQR]) for variables with skewed distribution. Patients were subsequently divided into 2 groups according to comorbid diabetes or not for subgroup analysis. Differences between patients with and without diabetes were assessed using the t test, Mann–Whitney U test or Chi-square analysis, as appropriate. Spearman correlation coefficients, Logistic regression analyses and Partial correlation analysis were used to describe the correlations between NGAL and TAC. All statistical tests were two-sided, a P-value of less than 0.05 was considered as statistically significant. All statistical analyses were performed using SPSS 20.0 (SPSS, Chicago, IL).
Results
Demographic, clinical characteristics, NGAL and TAC in all MHD patients
A total of 62 stable adult MHD patients were finally included in the cross-sectional observational study (in Table 1). All patients received the same dialysis modality, that is three sessions per week, for 4 h per session. The dialysate calcium concentration = 1.25 mmol/L for patients with adjusted serum calcium> 2.5 mmol/L or confirmed ectopic calcification, and dialysate calcium concentration = 1.5 mmol/L for other patients. The average age was 58.10 ± 15.98 years; male to female ratio was 1:0.94; median vintage was 29.27(8.65, 78.02) months; 43.55% of patients comorbid diabetes, 30.6% comorbid CHD. The median concentration of NGAL was 52.02(43.11, 422.30) ng/mL. As shown in the Table 2, there were 43 patients with chest CT, the TAC incidences were: TC 81.4%, ARC 30.2%, ATAC 34.9%, AAC 81.4%, DTAC 74.4%; 24 patients with routine chest radiography, the AAC incidence was 75%; 49 cases with AAC estimated by CT or routine chest radiography, the AAC incidence was 79%. Table 3 shows the values of TAC of 43 patients with chest CT: TC 9.55(0.70, 23.65) mL, ARC 0(0, 0.46) mL, ATAC 0(0, 0.58) mL, AAC 3.65(0.49, 8.08) mL, DTAC5.38(0, 11.71) mL; AAC values of 24 patients with routine chest radiography was 21.88(1.56, 35.94)%.
Table 1.
Characteristics of total MHD patients, MHD patients with and without diabetes
| Characteristic | Total(N = 62) | With diabetes(N = 27) | Without diabetes(N = 35) | P |
|---|---|---|---|---|
| Male(0)/female(1) | 30/32 | 14/13 | 16/19 | 0.798 |
| Age (year) | 58.10 ± 15.98 | 65.33 ± 13.17 | 52.51 ± 15.87 | 0.001 |
| Smoking, (%) | 21.0 | 25.9 | 17.1 | 0.297 |
| Vintage (months) | 29.27(8.65, 78.02) | 19.28(3.78, 52.50) | 40.27(16.16, 98.00) | 0.007 |
| Residual urine volume (ml/24 h) | 0(0, 200) | 100(0, 400) | 0(0, 150) | 0.123 |
| SBP (mmHg) | 155.05 ± 21.53 | 163.37 ± 17.68 | 148.63 ± 22.24 | 0.005 |
| DBP (mmHg) | 79.03 ± 16.13 | 68.48 ± 11.92 | 87.17 ± 14.32 | < 0.001 |
| Comorbid CHD, (%) | 30.6 | 40.7 | 22.9 | 0.108 |
| NGAL (ng/mL) | 52.02(43.11, 422.30) | 49.33(42.37,55.48) | 56.78(44.37,674.13) | 0.026 |
| Klotho (pg/mL) | 308.49(76.94, 877.32) | 265.22(11.70, 1391.19) | 319.96(138.46,608.23) | 0.836 |
| Ca (mmol/L) | 2.29(2.17, 2.41) | 2.21(2.12, 2.32) | 2.35(2.27, 2.51) | 0.001 |
| P (mmol/L) | 1.82(1.52, 2.26) | 1.67(1.49, 1.91) | 1.97(1.53, 2.53) | 0.039 |
| iPTH (pg/mL) | 245.4 0(122.35, 864.75) | 165.00(79.53, 274.80) | 745.60(162.30, 1775.00) | < 0.001 |
| ALP(U/L) | 75.00(60.00, 146.25) | 73.00(59.00, 91.00) | 110.00(60.00, 353.00) | 0.019 |
| K (mmol/L) | 5.02(4.44, 5.51) | 4.86(4.45, 5.73) | 5.10(4.40, 5.45) | 0.943 |
| HCO3−(mmol/L) | 20.04 ± 3.25 | 20.21 ± 2.90 | 19.91 ± 3.53 | 0.716 |
| BUN (mmol/L) | 24.66 ± 6.09 | 23.50 ± 5.79 | 25.55 ± 6.24 | 0.191 |
| Cr (μmol/L) | 786.50(680.60, 922.00) | 707.00(535.00, 752.00) | 884.00(754.00, 1038.00) | < 0.001 |
| Alb(g/L) | 41.1(39.0, 43.75) | 39.30(35.30, 42.10) | 42.1(39.8, 44.60) | 0.005 |
| LDL (mmol/L) | 2.04 ± 0.59 | 2.02 ± 0.67 | 2.06 ± 0.52 | 0.800 |
| TG (mmol/L) | 1.22(0.88,1.77) | 1.12(0.88,1.75) | 1.29(0.88,2.17) | 0.247 |
| SF (ng/mL) | 155.10(80.13, 317.25) | 135.87(83.65, 249.71) | 197.64(78.19, 405.49) | 0.089 |
| Hb(g/L) | 112.00(100.00, 121.25) | 117.00(100.00, 124.00) | 111.00(100.00, 119.00) | 0.259 |
| WBC(910^9/L) | 6.06(4.55,7.37) | 6.62(5.47, 7.98) | 5.11(4.23, 7.29) | 0.025 |
| PLT(510^9/L) | 189.50(160.00, 22D1.75) | 203.00(145.00, 247.00) | 184.00(164.00, 199.00) | 0.338 |
| Dialyzer membrane | ||||
| CTA, (%) | 35.5 | 22.2 | 45.7 | 0.048 |
| PS, (%) | 54.8 | 63.0 | 48.6 | 0.192 |
| PMMA, (%) | 9.7 | 14.8 | 5.7 | 0.221 |
| Calciums, (%) | 79.0 | 66.7 | 88.6 | 0.037 |
| Calcium free phosphorus binders carbonate) | ||||
| Sevelamer, (%) | 25.8 | 3.7 | 42.9 | < 0.001 |
| Lanthanum carbonate, (%) | 16.1 | 18.5 | 14.3 | 0.735 |
| Active vitamin D, (%) | 29.0 | 7.4 | 45.7 | 0.001 |
| Paricalcitol, (%) | 8.1 | 3.7 | 11.4 | 0.376 |
| Statins, (%) | 16.1 | 33.3 | 2.9 | 0.002 |
Continuous variables are expressed as mean ± standard deviation for normally distributed variables and as median (interquartile range) for variables with skewed distribution. Differences between patients with and without diabetes were assessed using the t test, Mann–Whitney U test or Chi-square analysis, as appropriate. Values with p < 0.05 were considered statistically significant and are indicated in bold
MHD maintenance hemodialysis, SBP systolic blood pressure, DBP diastolic blood pressure, CHD Coronary heart disease, NGAL neutrophil gelatinase-associated lipocalin, Ca calcium, P phosphate, iPTH intact parathyroid hormone, ALP alkaline phosphatase, K potassium, HCO3- carbonate ion, BUN blood urea nitrogen, Cr creatinine, Alb albumin, LDL low density lipoprotein, TG triglyceride, SF serum ferritin, Hb hemoglobin, WBC white blood cells, PLT platelet, HD hemodialysis, HFD high-flux hemodialysis, HDF hemodiafiltration, CTA cellulose triacetate, PS polysulfone, PMMA polymethylmethacrylate
Table 2.
Thoracic aorta calcification incidences of total MHD patients, MHD patients with and without diabetes
| Characteristic | Total (N = 62) | With diabetes (N = 27) | Without diabetes (N = 35) | P |
|---|---|---|---|---|
| CT | N = 43 | N = 22 | N = 21 | |
| TC | 35, 81.4% | 19, 86.4% | 16, 76.2% | 0.457 |
| ARC | 13, 30.2% | 7, 31.8% | 6, 28.6% | 1.000 |
| ATAC | 15, 34.9% | 8, 36.8% | 7, 33.3% | 1.000 |
| AAC | 35, 81.4% | 19, 86.4% | 16, 76.2% | 0.457 |
| DTAC | 32, 74.4% | 18, 81.8% | 14, 66.7% | 0.310 |
| Routine chest radiography | N = 24 | N = 6 | N = 18 | |
| AAC | 18, 75% | 6, 100% | 12, 66.7% | 0.277 |
| AAC by CT or chest radiography | N = 62 | N = 27 | N = 35 | |
| 49, 79.0% | 24, 88.9% | 25, 71.4% | 0.122 |
Thoracic aorta calcium estimated by computed tomography (CT): calcification volume quantified by extracting the aorta calcium with density ≥ 130 HU from the volume-rendered image under the assistance of semi-automatic software; thoracic aorta was divided into 4 sites, aortic root calcium (ARC), ascending aorta calcium (ATAC), AAC (aortic arch calcium), DTAC(descending thoracic aorta calcium) and TC (total calcium) were all calculated
AAC by routine chest radiography: the circumferences of aortic arch was divided into 16 sites, the number of sectors with calcification was calculated and multiplied by 100 to express the results as a percentage
Table 3.
Thoracic aorta calcification parameter values of total MHD patients, MHD patients with and without diabetes
| Characteristic | Total (N = 62) | With diabetes (N = 27) | Without diabetes (N = 35) | P |
|---|---|---|---|---|
| CT | N = 43 | N = 22 | N = 21 | |
| TC (mL) | 9.55(0.70, 23.65) | 11.86(4.74, 32.09) | 5.27(0.14, 18.13) | 0.176 |
| ARC (mL) | 0(0, 0.46) | 0(0, 0.65) | 0(0, 0.39) | 0.709 |
| ATAC (mL) | 0(0, 0.58) | 0(0, 0.69) | 0(0, 0.64) | 0.819 |
| AAC (mL) | 3.65(0.49, 8.08) | 4.32(0.61, 8.28) | 1.70(0.14, 9.21) | 0.670 |
| DTAC (mL) | 5.38(0, 11.71) | 7.05(2.24, 20.29) | 3.31(0, 8.85) | 0.070 |
| Routine chest radiography | N = 24 | N = 6 | N = 18 | |
| AAC(%) | 21.88(1.56, 35.94) | 31.25(25.00, 53.12) | 18.75(0, 28.13) | 0.090 |
Thoracic aorta calcium estimated by computed tomography (CT): calcification volume quantified by extracting the aorta calcium with density ≥ 130 HU from the volume-rendered image under the assistance of semi-automatic software; thoracic aorta was divided into 4 sites, aortic root calcium (ARC), ascending aorta calcium (ATAC), AAC(aortic arch calcium), DTAC(descending thoracic aorta calcium) and TC (total calcium) were all calculated
AAC by routine chest radiography: the circumferences of aortic arch was divided into 16 sites, the number of sectors with calcification was calculated and multiplied by 100 to express the results as a percentage
Differences of demographic, clinical characteristics, NGAL and TAC between patients with and without diabetes
Characteristics of study participants are shown in Table 1. Compared with patients without diabetes, patients with diabetes were significantly older (65.33±13.17 vs 52.51±15.87 years, P = 0.001); and with shorter vintage (19.28(3.78, 52.50) vs 40.27(16.16, 98.00) months, P = 0.007), higher systolic blood pressure (SBP) (163.37 ± 17.68 vs 148.63 ± 22.24 mmHg, P = 0.005), lower diastolic blood pressure (DBP) (68.48 ± 11.92 vs 87.17 ± 14.32 mmHg, P < 0.001), lower plasma NGAL(49.33(42.37,55.48) vs 56.78(44.37,674.13) ng/mL, P = 0.026), lower Ca(2.21(2.12, 2.32) vs 2.35 (2.27, 2.51) mmol/L, P = 0.001), lower P (1.67(1.49, 1.91) vs 1.97(1.53, 2.53) mmol/L, P = 0.039), lower iPTH (165.00(79.53, 274.80) vs 745.60(162.30, 1775.00)pg/mL, P < 0.001), lower ALP(73.00(59.00, 91.00) vs 110.00(60.00, 353.00)U/L, P = 0.019), lower Cr(707.00(535.00, 752.00) vs 884.00(754.00, 1038.00) 38.00) P < 0.001), lower Alb(39.30(35.30, 42.10) vs 42.1(39.8, 44.60) g/L, P = 0.005), higher WBC(6.62(5.47, 7.98) vs5.11(4.23, 7.29) × 10^9/L, P = 0.025). In terms of the application of medicine, lesser proportion of patients with diabetes taking calcium (66.7% vs 88.6%, P = 0.037), sevelamer(3.7% vs 42.9%), active vitamin D(7.4% vs 45.7%, P = 0.001), while larger proportion of them taking statins(33.3% vs 2.9%, P = 0.002). All estimated TAC parameters incidences (Table 2) or values (Table 3) were higher in MHD patients with diabetes than those without diabetes; however, the differences were not statistically significant.
Correlation analysis between plasma NGAL and TAC
Univariable logistic regression analyses showed positive correlations between lg (NGAL) and ARC (Table 4, OR = 5.581, P = 0.028), no correlations were found between lg (NGAL) and other TAC parameters. Age, sex and positive factors calculated by univariable logistic regression analyses (supplemental Table 1) between ARC and all characters were used for multivariable models (Table 5); lg (NGAL) was positively correlated with ARC after adjusting for age and sex (OR = 13.335, P = 0.012), adjusting for CHD (OR = 18.675, P = 0.014), or adjusting for active vitamin D (OR = 4.988, P = 0.043); however, when adjusting for Ca or vintage, the correlation between lg (NGAL) and ARC disappeared.
Table 4.
Univariable logistic regression analyses of lg (NGAL (ng/mL)) and thoracic aorta calcification in MHD patients (n = 62)
| Characteristic | OR (95% CI) | P |
|---|---|---|
| CT | N = 43 | |
| TC | 1.124(0.213-5.946) | 0.890 |
| ARC | 5.581(1.204-25.871) | 0.028 |
| ATAC | 1.586(0.431-5.834) | 0.488 |
| AAC | 1.124(0.213-5.946) | 0.890 |
| DTAC | 1.539(0.317-7.468) | 0.593 |
| Routine chest radiography | N = 24 | |
| AAC | 0.499(0.101-2.470) | 0.394 |
| AAC by CT or chest radiography | N = 62 | |
| 0.561(0.195-1.611) | 0.283 |
Thoracic aorta calcium estimated by computed tomography (CT): calcification volume quantified by extracting the aorta calcium with density ≥ 130 HU from the volume-rendered image under the assistance of semi-automatic software; thoracic aorta was divided into 4 sites, aortic root calcium (ARC), ascending aorta calcium (ATAC), AAC(aortic arch calcium), DTAC(descending thoracic aorta calcium) and TC (total calcium) were all calculated
AAC by routine chest radiography: the circumferences of aortic arch was divided into 16 sites, the number of sectors with calcification was calculated and multiplied by 100 to express the results as a percentage
Table 5.
Logistic regression analyses of lg (NGAL (ng/mL)) and aortic root calcium (ARC) in MHD patients (n = 43)
| Models | OR (95% CI) | P |
|---|---|---|
| Univariable analysis | 5.581(1.204-25.871) | 0.028 |
| Multivariable-adjusted analysis | ||
| Age and sex | 13.335(1.781-99.829) | 0.012 |
| Comorbid CHD | 18.675(1.791-194.711) | 0.014 |
| Ca | 2.561(0.342-19.172) | 0.360 |
| Vintage (months) | 3.410(0.497-23.393) | 0.212 |
| Active vitamin D | 4.988(1.053-23.641) | 0.043 |
NGAL neutrophil gelatinase-associated lipocalin, CHD Coronary heart disease, Ca calcium
Spearman correlation analysis between lg (NGAL) and TAC parameter values are depicted in Table 6. In MHD patients without diabetes (n = 21), lg (NGAL) were positively correlated with ARC value (R = 0.612, P = 0.003); no other correlations were found in total group or subgroups. Spearman correlation analysis between ARC value and all demographic, clinical characters were further performed in without diabetes group (supplemental Table 2); and 4 potential confounders were found as follows, comorbid CHD (R = 0.481, P = 0.027), Ca (mmol/L)(R = 0.534, P = 0.013), Alb(g/L)(R = -0.539, P = 0.012), dalyzer membrane (polysulfone)(R = -0.458, P = 0.037). Age, sex and all confounders were employed in partial correlation analysis in patients without diabetes (Table 7). Lg (NGAL) was positively correlated with ARC value, after adjusting for age and sex(R = 0.550, P = 0.015), adjusting for age, sex and CHD(R = 0.565, P = 0.015), adjusting for age, sex, CHD and Alb(R = 0.536, P = 0.027), or adjusting for age, sex, CHD, Alb, and dialyzer membrane (polysulfone)(R = 0.590, P = 0.016); however, when adjusting for age, sex, CHD, Alb, and Ca, the correlation between lg (NGAL) and ARC value disappeared. Scatter diagrams and Spearman coefficient are shown in Fig. 1, positive correlation were found between NGAL and Ca(R = 0.644, P < 0.001), Ca and ARC(R = 0.534, P = 0.013), NGAL and ACR(R = 0.612, P = 0.003).
Table 6.
Spearman coefficients between lg (NGAL (ng/mL)) and thoracic aorta calcification parameter values of total MHD patients, MHD patients with and without diabetes
| Characteristic | Total | With diabetes | Without diabetes | ||||||
|---|---|---|---|---|---|---|---|---|---|
| CT | N = 43 | R | P | N = 22 | R | P | N = 21 | R | P |
| TC (mL) | 0.081 | 0.607 | −0.025 | 0.911 | 0.149 | 0.519 | |||
| ARC (mL) | 0.271 | 0.079 | −0.076 | 0.737 | 0.612 | 0.003 | |||
| ATAC (mL) | 0.092 | 0.555 | −0.127 | 0.573 | 0.273 | 0.231 | |||
| AAC (mL) | 0.107 | 0.495 | 0.143 | 0.525 | 0.068 | 0.770 | |||
| DTAC (mL) | 0.060 | 0.702 | −0.113 | 0.618 | 0.169 | 0.465 | |||
| Routine chest radiography | |||||||||
| AAC(%) | N = 24 | −0.199 | 0.351 | N = 6 | 0.213 | 0.686 | N = 18 | −0.053 | 0.835 |
Thoracic aorta calcium estimated by computed tomography (CT): calcification volume quantified by extracting the aorta calcium with density and without diabetesiplied by 100 to express the results as a percentage.matic software; thoracic aorta was divided into 4 sites, aortic root calcium (ARC), ascending aorta calcium (ATAC), AAC(aortic arch calcium), DTAC(descending thoracic aorta calcium) and TC (total calcium) were all calculated
AAC by routine chest radiography: the circumferences of aortic arch was divided into 16 sites, the number of sectors with calcification was calculated and multiplied by 100 to express the results as a percentage
Table 7.
Partial coefficients between lg (NGAL (ng/mL)) and aortic root calcium (ARC) parameter values of MHD patients without diabetes (n = 21)
| Adjusted characters | R | P |
|---|---|---|
| Age and sex | 0.550 | 0.015 |
| Age, sex and comorbid CHD | 0.565 | 0.015 |
| Age, sex, comorbid CHD and Alb | 0.536 | 0.027 |
| Age, sex, comorbid CHD, Alb, and Ca | 0.175 | 0.518 |
| Age, sex, comorbid CHD, Alb, and Dialyzer membrane(PS) | 0.590 | 0.016 |
NGAL neutrophil gelatinase-associated lipocalin, CHD Coronary heart disease, Alb albumin, Ca calcium, PS polysulfone
Fig. 1.
Scatter diagrams and Spearman coefficient between NGAL, Ca and ARC of MHD patients without diabetes (n = 21)
Discussion
Cardiovascular calcification is a common and refractory complication of MHD patients, and is closely related to the high cardiovascular morbidity and mortality [18, 23]. In addition to conventional risk factors such as diabetes, hypertension and lipid metabolism disorder; disturbance of mineral metabolism is also associated with cardiovascular calcification [24–26]. To assess thoracic aorta calcification through chest CT, we employed a 3D visualization and quantification method to divided thoracic aorta into 4 sites, ARC, ATAC, AAC, DTAC [22]. The final results showed that NGAL, a bone-derived factor involved in metabolism and a biomarker of kidney injury and cardiovascular pathophysiology, were positively correlated with serum Ca and ARC in MHD patients without diabetes. Previous studies have confirmed that ARC is associated with total coronary artery calcification and the number of coronary stenotic vessels in patients with an intermediate pretest probability of ischemic heart disease [27]. NGAL is also an independent factor for predicting major adverse cardiac events in familial hypercholesterolemia [28]. To our knowledge, this is the first study to find an association between NGAL and ARC in MHD patients; the result suggests that NGAL is an important link in the cross-talk between bone and vascular. Former observational studies have demonstrated that increased circulating NGAL levels are associated with the severity of coronary artery disease [29] and increased risk of future cardiovascular disease events [23, 30, 31]. Results from basic researches reveal the detrimental roles of NGAL in the development of cardiovascular pathophysiological process, such as atherosclerosis [18], abdominal aortic aneurysm [32] and endothelial dysfunction [33, 34].
In physiological condition, NGAL was once thought to be secreted mainly by adipose tissue; however recent study showed that it is “expressed by osteoblasts, at levels that are at least tenfold higher in osteoblasts than in white adipose tissue or other organs” [5]. In pathological conditions, NGAL is expressed by various injured cells and tissues. It is an excellent biomarker in acute kidney injure secreted by tubular epithelial cell. In MHD population, there is no difference in plasma NGAL in patients with or without kidneys, which suggest that kidney is not the main source of increased circulating NGAL [35]. In our former study [19], positive correlations between circulating NGAL and CKD-MBD parameters (serum ALP and Ca) were found in MHD patients; while a downward trend in plasma NGAL was observed after PTX + AT in MHD patients with severe SHPT. These results suggested that “bone maybe one of the main sources of increased NGAL in MHD patients”. In the present study, MHD patients with diabetes showed lower plasma NGAL level, the absent correlation between NGAL and ARC may due to impaired osteoblast function in diabetes [36–38]. It is confirmed that CKD patients with diabetes are more prone to present with low bone turnover states [39], the potential mechanisms probably lie in the suppression of parathyroid hormone secretion, osteoblast activity and bone turnover by hyperglycemia and insulin deficiency [40, 41].
Above all, the major finding of our study is that there were positive correlations among plasma NGAL, serum Ca and ARC in MHD patients without diabetes; which suggests that NGAL is possibly a participant in cardiovascular calcification under MHD condition. However, this is a cross-sectional observational study. Small sample size and no follow-up observations of cardiovascular event or mortality are limitations of this study and also the direction of future research.
Conclusion
There were positive correlations among plasma NGAL, serum Ca and ARC in MHD patients without diabetes; which suggests that NGAL is possibly a participant in cardiovascular calcification, in non-diabetic MHD.
Supplementary Information
Additional file 1 Supplemental Table 1. Univariable logistic regression analyses between aortic root calcium (ARC) and characters of all MHD patients (n = 43) MHD maintenance hemodialysis, SBP systolic blood pressure, DBP diastolic blood pressure, CHD Coronary heart disease, NGAL neutrophil gelatinase-associated lipocalin, Ca calcium, P phosphate, iPTH intact parathyroid hormone, ALP alkaline phosphatase, K potassium, HCO3- carbonate ion, BUN blood urea nitrogen, Cr creatinine, Alb albumin, LDL low density lipoprotein, TG triglyceride, SF serum ferritin; Hb hemoglobin, WBC white blood cells, PLT platelet, HD hemodialysis, HFD high-flux hemodialysis, HDF hemodiafiltration, CTA cellulose triacetate, PS polysulfone, PMMA polymethylmethacrylate. Supplemental Table 2. Spearman coefficients between aortic root calcium (ARC) and characters of MHD patients without diabetes (n = 21) MHD maintenance hemodialysis, SBP systolic blood pressure, DBP diastolic blood pressure, CHD Coronary heart disease, NGAL neutrophil gelatinase-associated lipocalin, Ca calcium, P phosphate, iPTH intact parathyroid hormone, ALP alkaline phosphatase, K potassium, HCO3- carbonate ion, BUN blood urea nitrogen, Cr creatinine, Alb albumin, LDL low density lipoprotein, TG triglyceride, SF serum ferritin; Hb hemoglobin, WBC white blood cells, PLT platelet, HD hemodialysis, HFD high-flux hemodialysis, HDF hemodiafiltration, CTA cellulose triacetate, PS polysulfone, PMMA polymethylmethacrylate.
Acknowledgments
We would like to thank Dr. Fang Tang, at center for data science in health and medicine, the First Affiliated Hospital of Shandong First Medical University, Jinan, China, for their valuable inputs in data analysis.
Abbreviations
- NGAL
Neutrophil gelatinase-associated lipocalin
- TAC
Thoracic aorta calcification
- MHD
Maintenance hemodialysis
- CAD
Coronary artery disease
- AAA
Abdominal aortic aneurysm
- Ca
Calcium
- P
Phosphate
- ALP
Alkaline phosphatase
- CT
Computed tomography
- CHD
Coronary heart disease
- K
Potassium
- HCO3-
Carbonate ion
- BUN
Urea nitrogen
- Cr
Creatinine
- Alb
Albumin
- LDL
Low density lipoprotein
- TG
Triglyceride
- SF
Territin
- Hb
Hemoglobin
- WBC
White blood cells
- PLT
Platelet
- ARC
Aortic root calcium
- ATAC
Ascending aorta calcium
- AAC
Aortic arch calcium
- DTAC
Descending thoracic aorta calcium
- TC
Total calcium
- SD
Standard deviation
- IQR
Interquartile range
- SBP
Systolic blood pressure
- DBP
Diastolic blood pressure
- iPTH
Intact Parathyroid hormone
Authors’ contributions
XJ, KW and DX designed research; XJ, KW, JC, GS, YW, CS, PC, YL and LW conducted research; XJ, XK and YL analyzed data; XJ, DX, KW, LX and YW wrote the paper; XJ had primary responsibility for final content. All authors read and approved the final manuscript.
Funding
National Natural Science Foundation of China (81970615 to Dongmei Xu) was responsible for the collection, management, and interpretation of data; National Natural Science Foundation of China (82004088 to Kai Wei) was responsible for analysis of data and manuscript writing; National Natural Science Foundation of China (82000728 to Xianglei Kong) contributed to data interpretation, preparation and review.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
This study was approved by the Ethics Committee of the First Affiliated Hospital of Shandong First Medical University and carried out in accordance with the declaration of Helsinki. Written informed consent was obtained from each participant prior to study procedures.
Consent for publication
Not applicable.
Competing interests
All of the authors declare that they have no conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Kai Wei and Gesheng Song contributed equally to this work.
References
- 1.Asimakopoulou A, Borkham-Kamphorst E, Tacke F, Weiskirchen R. Lipocalin-2 (NGAL/LCN2), a "help-me" signal in organ inflammation. Hepatology. 2016;63(2):669–671. doi: 10.1002/hep.27930. [DOI] [PubMed] [Google Scholar]
- 2.Buonafine M, Martinez-Martinez E, Jaisser F. More than a simple biomarker: the role of NGAL in cardiovascular and renal diseases. Clin Sci (Lond) 2018;132(9):909–923. doi: 10.1042/CS20171592. [DOI] [PubMed] [Google Scholar]
- 3.Abella V, Scotece M, Conde J, Gómez R, Lois A, Pino J, Gómez-Reino JJ, Lago F, Mobasheri A, Gualillo O. The potential of lipocalin-2/NGAL as biomarker for inflammatory and metabolic diseases. Biomarkers. 2015;20(8):565–571. doi: 10.3109/1354750X.2015.1123354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gouweleeuw L, Naudé PJ, Rots M, DeJongste MJ, Eisel UL, Schoemaker RG. The role of neutrophil gelatinase associated lipocalin (NGAL) as biological constituent linking depression and cardiovascular disease. Brain Behav Immun. 2015;46:23–32. doi: 10.1016/j.bbi.2014.12.026. [DOI] [PubMed] [Google Scholar]
- 5.Mosialou I, Shikhel S, Liu JM, Maurizi A, Luo N, He Z, Huang Y, Zong H, Friedman RA, Barasch J, Lanzano P, Deng L, Leibel RL, Rubin M, Nickolas T, Chung W, Zeltser LM, Williams KW, Pessin JE, Kousteni S. MC4R-dependent suppression of appetite by bone-derived lipocalin 2. Nature. 2017;543(7645):385–390. doi: 10.1038/nature21697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Luo Y, Ma X, Pan X, Xu Y, Xiong Q, Xiao Y, Bao Y, Jia W. Serum lipocalin-2 levels are positively associated with not only total body fat but also visceral fat area in Chinese men. Medicine (Baltimore) 2016;95(30):e4039. doi: 10.1097/MD.0000000000004039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jaberi SA, Cohen A, D'Souza C, Abdulrazzaq YM, Ojha S, Bastaki S, Adeghate EA. Lipocalin-2: structure, function, distribution and role in metabolic disorders. Biomed Pharmacother. 2021;142:112002. doi: 10.1016/j.biopha.2021.112002. [DOI] [PubMed] [Google Scholar]
- 8.Bedouhène S, Dang PM, Hurtado-Nedelec M, El-Benna J. Neutrophil degranulation of Azurophil and specific granules. Methods Mol Biol. 2020;2087:215–222. doi: 10.1007/978-1-0716-0154-9_16. [DOI] [PubMed] [Google Scholar]
- 9.Lekva T, Gullestad L, Broch K, Aukrust P, Andreassen AK, Ueland T. Distinct patterns of soluble leukocyte activation markers are associated with etiology and outcomes in precapillary pulmonary hypertension. Sci Rep. 2020;10(1):18540. doi: 10.1038/s41598-020-75654-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Araos P, Prado C, Lozano M, Figueroa S, Espinoza A, Berger T, Mak TW, Jaisser F, Pacheco R, Michea L, Amador CA. Dendritic cells are crucial for cardiovascular remodeling and modulate neutrophil gelatinase-associated lipocalin expression upon mineralocorticoid receptor activation. J Hypertens. 2019;37(7):1482–1492. doi: 10.1097/HJH.0000000000002067. [DOI] [PubMed] [Google Scholar]
- 11.Meyers K, López M, Ho J, Wills S, Rayalam S, Taval S. Lipocalin-2 deficiency may predispose to the progression of spontaneous age-related adiposity in mice. Sci Rep. 2020;10(1):14589. doi: 10.1038/s41598-020-71249-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Marques FZ, Prestes PR, Byars SG, Ritchie SC, Würtz P, Patel SK, Booth SA, Rana I, Minoda Y, Berzins SP, Curl CL, Bell JR, Wai B, Srivastava PM, Kangas AJ, Soininen P, Ruohonen S, Kähönen M, Lehtimäki T, Raitoharju E, Havulinna A, Perola M, Raitakari O, Salomaa V, Ala-Korpela M, Kettunen J, McGlynn M, Kelly J, Wlodek ME, Lewandowski PA, Delbridge LM, Burrell LM, Inouye M, Harrap SB, Charchar FJ. Experimental and human evidence for Lipocalin-2 (neutrophil gelatinase-associated Lipocalin [NGAL]) in the development of cardiac hypertrophy and heart failure. J Am Heart Assoc. 2017;6(6):e005971. doi: 10.1161/JAHA.117.005971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Olson B, Zhu X, Norgard MA, Diba P, Levasseur PR, Buenafe AC, Huisman C, Burfeind KG, Michaelis KA, Kong G, Braun T, Marks DL. Chronic cerebral lipocalin 2 exposure elicits hippocampal neuronal dysfunction and cognitive impairment. Brain Behav Immun. 2021;S0889-1591(21):00266–0026X. doi: 10.1016/j.bbi.2021.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Krizanac M, Mass Sanchez PB, Weiskirchen R, Asimakopoulos A. A scoping review on Lipocalin-2 and its role in non-alcoholic steatohepatitis and hepatocellular carcinoma. Int J Mol Sci. 2021;22(6):2865. doi: 10.3390/ijms22062865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Malyszko J, Malyszko JS, Koc-Zorawska E, Kozminski P, Mysliwiec M. Neutrophil gelatinase-associated lipocalin in dialyzed patients is related to residual renal function, type of renal replacement therapy and inflammation. Kidney Blood Press Res. 2009;32(6):464–469. doi: 10.1159/000274048. [DOI] [PubMed] [Google Scholar]
- 16.Song X, Cai D, Zhang B. Clinical values of serum NGAL combined with NT-proBNP in the early prognosis of type 1 cardiorenal syndrome. Am J Transl Res. 2021;13(4):3363–3368. [PMC free article] [PubMed] [Google Scholar]
- 17.Shang W, Wang Z. The update of NGAL in acute kidney injury. Curr Protein Pept Sci. 2017;18(12):1211–1217. doi: 10.2174/1389203717666160909125004. [DOI] [PubMed] [Google Scholar]
- 18.Lin X, Onda DA, Yang CH, Lewis JR, Levinger I, Loh K. Roles of bone-derived hormones in type 2 diabetes and cardiovascular pathophysiology. Mol Metab. 2020;40:101040. doi: 10.1016/j.molmet.2020.101040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jia XY, Wei K, Chen J, Xi LH, Kong XL, Wei Y, et al. Association of plasma neutrophil gelatinase-associated lipocalin with parameters of CKD-MBD in maintenance hemodialysis patients. J Bone Miner Metab. 2021. 10.1007/s00774-021-01248-9. [DOI] [PubMed]
- 20.Rogers MA, Aikawa E. Cardiovascular calcification: artificial intelligence and big data accelerate mechanistic discovery. Nat Rev Cardiol. 2019;16(5):261–274. doi: 10.1038/s41569-018-0123-8. [DOI] [PubMed] [Google Scholar]
- 21.Pedrosa JF, Barreto SM, Bittencourt MS, Ribeiro ALP. Anatomical references to evaluate thoracic aorta calcium by computed tomography. Curr Atheroscler Rep. 2019;21(12):51. doi: 10.1007/s11883-019-0811-9. [DOI] [PubMed] [Google Scholar]
- 22.Fujii H, Kono K, Watanabe K, Goto S, Nishii T, Kono A, Nishi S. Evaluation of aortic calcification using a three-dimensional volume-rendering method in patients with end-stage kidney disease. J Bone Miner Metab. 2021;39(3):439–445. doi: 10.1007/s00774-020-01172-4. [DOI] [PubMed] [Google Scholar]
- 23.Chong JJH, Prince RL, Thompson PL, Thavapalachandran S, Ooi E, Devine A, Lim EEM, Byrnes E, Wong G, Lim WH, Lewis JR. Association between plasma neutrophil gelatinase-associated Lipocalin and cardiac disease hospitalizations and deaths in older women. J Am Heart Assoc. 2019;8(1):e011028. doi: 10.1161/JAHA.118.011028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hénaut L, Chillon JM, Kamel S, Massy ZA. Updates on the mechanisms and the Care of Cardiovascular Calcification in chronic kidney disease. Semin Nephrol. 2018;38(3):233–250. doi: 10.1016/j.semnephrol.2018.02.004. [DOI] [PubMed] [Google Scholar]
- 25.Massy ZA, Drüeke TB. Vascular calcification. Curr Opin Nephrol Hypertens. 2013;22(4):405–412. doi: 10.1097/MNH.0b013e328362155b. [DOI] [PubMed] [Google Scholar]
- 26.Himmelsbach A, Ciliox C, Goettsch C. Cardiovascular calcification in chronic kidney disease-therapeutic opportunities. Toxins (Basel) 2020;12(3):181. doi: 10.3390/toxins12030181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nafakhi H, Al-Nafakh HA, Al-Mosawi AA, Al GF. Correlations between aortic root calcification and coronary artery atherosclerotic markers assessed using multidetector computed tomography. Acad Radiol. 2015;22(3):357–362. doi: 10.1016/j.acra.2014.09.017. [DOI] [PubMed] [Google Scholar]
- 28.Okada H, Tada H, Hayashi K, Kawashima H, Takata T, Sakata K, Nohara A, Mabuchi H, Yamagishi M, Kawashiri MA. Aortic root calcification score as an independent factor for predicting major adverse cardiac events in familial hypercholesterolemia. J Atheroscler Thromb. 2018;25(7):634–642. doi: 10.5551/jat.42705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zografos T, Haliassos A, Korovesis S, Giazitzoglou E, Voridis E, Katritsis D. Association of neutrophil gelatinase-associated lipocalin with the severity of coronary artery disease. Am J Cardiol. 2009;104(7):917–920. doi: 10.1016/j.amjcard.2009.05.023. [DOI] [PubMed] [Google Scholar]
- 30.Wu G, Li H, Fang Q, Jiang S, Zhang L, Zhang J, Hou X, Lu J, Bao Y, Xu A, Jia W. Elevated circulating lipocalin-2 levels independently predict incident cardiovascular events in men in a population-based cohort. Arterioscler Thromb Vasc Biol. 2014;34(11):2457–2464. doi: 10.1161/ATVBAHA.114.303718. [DOI] [PubMed] [Google Scholar]
- 31.Lindberg S, Jensen JS, Mogelvang R, Pedersen SH, Galatius S, Flyvbjerg A, Magnusson NE. Plasma neutrophil gelatinase-associated lipocalinin in the general population: association with inflammation and prognosis. Arterioscler Thromb Vasc Biol. 2014;34(9):2135–2142. doi: 10.1161/ATVBAHA.114.303950. [DOI] [PubMed] [Google Scholar]
- 32.Tarín C, Fernandez-Garcia CE, Burillo E, Pastor-Vargas C, Llamas-Granda P, Castejón B, Ramos-Mozo P, Torres-Fonseca MM, Berger T, Mak TW, Egido J, Blanco-Colio LM, Martín-Ventura JL. Lipocalin-2 deficiency or blockade protects against aortic abdominal aneurysm development in mice. Cardiovasc Res. 2016;111(3):262–273. doi: 10.1093/cvr/cvw112. [DOI] [PubMed] [Google Scholar]
- 33.Song E, Fan P, Huang B, Deng HB, Cheung BM, Félétou M, Vilaine JP, Villeneuve N, Xu A, Vanhoutte PM, Wang Y. Deamidated lipocalin-2 induces endothelial dysfunction and hypertension in dietary obese mice. J Am Heart Assoc. 2014;3(2):e000837. doi: 10.1161/JAHA.114.000837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Liu JT, Song E, Xu A, Berger T, Mak TW, Tse HF, Law IK, Huang B, Liang Y, Vanhoutte PM, Wang Y. Lipocalin-2 deficiency prevents endothelial dysfunction associated with dietary obesity: role of cytochrome P450 2C inhibition. Br J Pharmacol. 2012;165(2):520–531. doi: 10.1111/j.1476-5381.2011.01587.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rau S, Habicht A, Kauke T, Hillmer A, Wessely M, Stangl M, Guba M, Fischereder M, Schönermarck U. Neutrophil gelatinase-associated lipocalin and end-stage renal disease: it is not all about the kidneys! Eur J Clin Investig. 2013;43(8):816–820. doi: 10.1111/eci.12110. [DOI] [PubMed] [Google Scholar]
- 36.Dixit M, Liu Z, Poudel SB, Yildirim G, Zhang YZ, Mehta S, Murik O, Altarescu G, Kobayashi Y, Shimizu E, Schaffler MB, Yakar S. Skeletal response to insulin in the naturally occurring type 1 diabetes mellitus mouse model. JBMR Plus. 2021;5(5):e10483. doi: 10.1002/jbm4.10483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Donat A, Knapstein PR, Jiang S, Baranowsky A, Ballhause TM, Frosch KH, Keller J. Glucose metabolism in osteoblasts in healthy and pathophysiological conditions. Int J Mol Sci. 2021;22(8):4120. doi: 10.3390/ijms22084120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cipriani C, Colangelo L, Santori R, Renella M, Mastrantonio M, Minisola S, Pepe J. The interplay between bone and glucose metabolism. Front Endocrinol (Lausanne) 2020;11:122. doi: 10.3389/fendo.2020.00122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Moreira CA, Barreto FC, Dempster DW. New insights on diabetes and bone metabolism. J Bras Nefrol. 2015;37(4):490–495. doi: 10.5935/0101-2800.20150077. [DOI] [PubMed] [Google Scholar]
- 40.Sugimoto T, Ritter C, Morrissey J, Hayes C, Slatopolsky E. Effects of high concentrations of glucose on PTH secretion in parathyroid cells. Kidney Int. 1990;37(6):1522–1527. doi: 10.1038/ki.1990.144. [DOI] [PubMed] [Google Scholar]
- 41.Bover J, Ureña P, Brandenburg V, Goldsmith D, Ruiz C, DaSilva I, Bosch RJ. Adynamic bone disease: from bone to vessels in chronic kidney disease. Semin Nephrol. 2014;34(6):626–640. doi: 10.1016/j.semnephrol.2014.09.008. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1 Supplemental Table 1. Univariable logistic regression analyses between aortic root calcium (ARC) and characters of all MHD patients (n = 43) MHD maintenance hemodialysis, SBP systolic blood pressure, DBP diastolic blood pressure, CHD Coronary heart disease, NGAL neutrophil gelatinase-associated lipocalin, Ca calcium, P phosphate, iPTH intact parathyroid hormone, ALP alkaline phosphatase, K potassium, HCO3- carbonate ion, BUN blood urea nitrogen, Cr creatinine, Alb albumin, LDL low density lipoprotein, TG triglyceride, SF serum ferritin; Hb hemoglobin, WBC white blood cells, PLT platelet, HD hemodialysis, HFD high-flux hemodialysis, HDF hemodiafiltration, CTA cellulose triacetate, PS polysulfone, PMMA polymethylmethacrylate. Supplemental Table 2. Spearman coefficients between aortic root calcium (ARC) and characters of MHD patients without diabetes (n = 21) MHD maintenance hemodialysis, SBP systolic blood pressure, DBP diastolic blood pressure, CHD Coronary heart disease, NGAL neutrophil gelatinase-associated lipocalin, Ca calcium, P phosphate, iPTH intact parathyroid hormone, ALP alkaline phosphatase, K potassium, HCO3- carbonate ion, BUN blood urea nitrogen, Cr creatinine, Alb albumin, LDL low density lipoprotein, TG triglyceride, SF serum ferritin; Hb hemoglobin, WBC white blood cells, PLT platelet, HD hemodialysis, HFD high-flux hemodialysis, HDF hemodiafiltration, CTA cellulose triacetate, PS polysulfone, PMMA polymethylmethacrylate.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.