Abstract
Simple Summary
For the growing number of cancer survivors worldwide, fatigue presents a major hurdle to function and quality of life. Treatment options for cancer-related fatigue are still emerging, and our current understanding of its etiology is limited. In this paper, we describe a new application of a comprehensive model for cancer-related fatigue: the predisposing, precipitating, and perpetuating (3P) factors model. We propose that the 3P model may be leveraged—particularly using metabolomics, the microbiome, and inflammation in conjunction with behavioral science—to better understand the pathophysiology of cancer-related fatigue.
Abstract
A major gap impeding development of new treatments for cancer-related fatigue is an inadequate understanding of the complex biological, clinical, demographic, and lifestyle mechanisms underlying fatigue. In this paper, we describe a new application of a comprehensive model for cancer-related fatigue: the predisposing, precipitating, and perpetuating (3P) factors model. This model framework outlined herein, which incorporates the emerging field of metabolomics, may help to frame a more in-depth analysis of the etiology of cancer-related fatigue as well as a broader and more personalized set of approaches to the clinical treatment of fatigue in oncology care. Included within this review paper is an in-depth description of the proposed biological mechanisms of cancer-related fatigue, as well as a presentation of the 3P model’s application to this phenomenon. We conclude that a clinical focus on organization risk stratification and treatment around the 3P model may be warranted, and future research may benefit from expanding the 3P model to understand fatigue not only in oncology, but also across a variety of chronic conditions.
Keywords: fatigue, metabolomics, survivorship
1. Introduction
Cancer-related fatigue is defined by the National Comprehensive Cancer Network (NCCN) as a distressing, persistent sense of physical, emotional, and/or cognitive exhaustion related to cancer that is not proportional to activity and interferes with functioning [1]. Moderate to severe fatigue affects up to 90% of patients during chemotherapy and approximately 30–40% years after treatment completion [1,2]. Unlike typical fatigue, cancer-related fatigue tends to be more severe, distressing, and unlikely to be relieved by rest [3]. Patients describe it as “devastating”, “never-ending” and “totally consuming” [4,5]. Fatigue is associated with worse quality of life and lower likelihood of returning to normal daily activities, including work [2,6,7,8,9].
Treatment options for cancer patients with fatigue are limited. Behavioral and psychosocial interventions demonstrate benefit [10,11,12,13,14] but tend to be time intensive, limiting uptake, compliance, and maintenance. Medications to treat sleep problems such as paroxetine, sertraline, modafinil, and armodafinil have shown limited benefit for cancer-related fatigue in randomized trials [15,16,17,18,19,20]. Evidence is mixed for methylphenidate, which may be poorly tolerated [21,22,23,24]. Because of the limited benefit of pharmacotherapy and since patients often prefer to avoid additional medications, behavioral treatment options for cancer-related fatigue are urgently needed [25,26]. A major gap impeding development of new treatments is an inadequate understanding of the complex biological, clinical, demographic, and lifestyle mechanisms underlying fatigue [6]. In this paper, we describe a new application of a comprehensive model for a better understanding of cancer-related fatigue: the predisposing, precipitating, and perpetuating (3P) factors model. This model framework outlined herein, which incorporates the emerging field of metabolomics, may help to frame a more in-depth analysis of the etiology of cancer-related fatigue as well as a broader and more personalized set of approaches to the clinical treatment of fatigue in oncology care.
2. Proposed Biological Mechanisms of Cancer-Related Fatigue
The pathophysiology of cancer-related fatigue is thought to be multifactorial [27,28]. Despite this complexity, the large majority of studies on the biological mechanisms of cancer-related fatigue have focused on immune and inflammatory variables, which are hypothesized to induce fatigue via the effect of inflammatory mediators on brain systems involved in “sickness behaviors.” Specific variants include genes regulating inflammation (e.g., IL6, TNFA, and IL1) [29], inflammatory gene expression profiles (e.g., increased NF-kB) [30,31,32], and circulating markers of inflammation (e.g., IL-1, TNFA, CRP, and IL-6) [32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53]. Inflammation is linked with the dysregulation of biochemical and physiological systems including peripheral (muscles and tissues) and central mechanisms (central nervous system) [54] and may cause fatigue through cytokine dysregulation, hypothalamic–pituitary–adrenal (HPA) axis dysfunction, 5-hydroxy-tryptophan (5-HT) neurotransmitter dysregulation, circadian rhythm disruption, alterations in adenosine triphosphate (ATP), muscle metabolism, and vagal afferent activation [28,54,55]. Recent research has suggested that agents with anti-inflammatory properties (i.e., non-steroidal anti-inflammatory drugs or NSAIDs, bupropion) could offer a safe, inexpensive, and widely-available means to revolutionize the treatment of cancer-related fatigue [56,57,58,59]. These findings suggest that pathophysiologic pathways and genetic mechanisms hold promise for the identification of new causal mechanisms and potential treatment targets; however, these mechanisms are poorly understood. In addition, current models of pathophysiology do not take into account the complex psychosocial and behavioral factors that may also play a major role in cancer-related fatigue.
3. An Alternative Model of Cancer-Related Fatigue: The 3P Factors Model
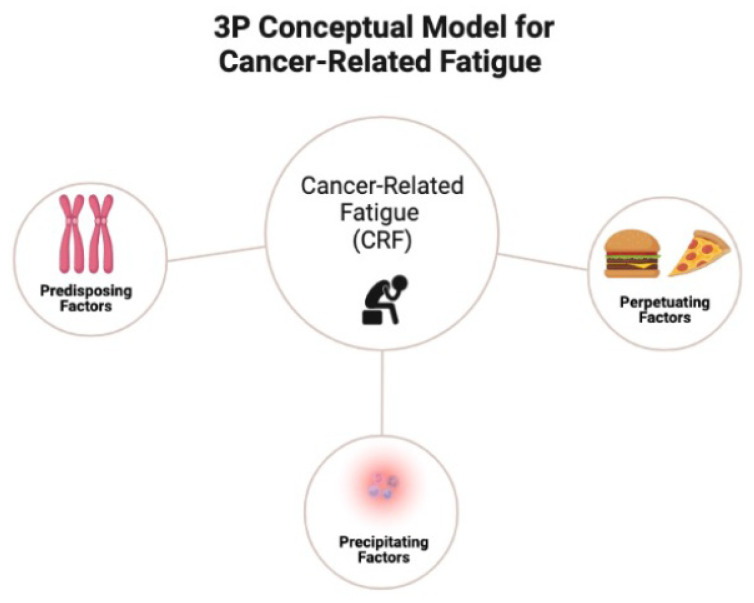
The most notable framework previously proposed to describe complex disease processes is the biopsychosocial model, an inter-disciplinary model that looks at the interconnection between biology, psychology, and socioenvironmental factors [60]. While the biopsychosocial model has played a crucial role in counteracting biological reductionism and progressing towards a more holistic philosophy of human health, it lacks the granularity necessary to understand how various factors contribute to disease [61]. In contrast, as shown in Table 1, the 3P model can be utilized to describe the complex biological and psychological processes underlying cancer-related fatigue. The 3P model postulates that predisposing factors place patients at risk of developing baseline fatigue (e.g., 1. biobehavioral: age, biological sex, genetic variants, metabolomics, inflammation, body composition, nutritional quality, circadian disruption, and co-morbidities; 2. psychosocial: depressed mood, anxiety, insomnia, and perceived stress); precipitating factors spur the onset of fatigue (e.g., changes in metabolism and inflammation due to cancer and/or chemotherapy and treatment-related factors: systemic therapy and radiotherapy); and perpetuating factors worsen fatigue or cause it to become chronic (e.g., poor sleep, physical inactivity, and poor diet). The 3P model (Figure 1) has been suggested for better understanding fatigue [62] and successfully applied to other chronic conditions including sleep and pain [24,25].
Table 1.
3P definitions, examples, and recommended clinical actions.
| 3P Component | Definition | Examples | Recommended Clinical Actions |
|
|---|---|---|---|---|
| Predisposing Factors | Relatively stable patient characteristics that increase risk of developing cancer-related fatigue | Sex; age; genetics; circadian disruption; SNPS in circadian regulation; body composition; genetic variants altering metabolome and inflammasome | Genetic pathway analysis; risk stratification; tailored prehabilitation interventions |
 Patient education about the 3P model; standardized self-health-management techniques for mitigating cancer-related fatigue. 
|
| Precipitating Factors | States and traits that bring about or hasten the onset of cancer-related fatigue | Metabolic dysregulation; inflammation; biobehavioral: metabolic dysregulation, inflammation; treatment-related factors: systemic therapy, radiotherapy | Monitoring for inflammation; preventive health behaviors | |
| Perpetuating Factors | Characteristics and behaviors that worsen or prolong fatigue | Metabolic endotoxemia caused by changes in the microbiome; physical inactivity; sleep disturbance; biobehavioral: metabolic endotoxemia caused by changes in the microbiome, physical inactivity, circadian disruption, sleep disturbance. Treatment-related factors: maintenance therapy (e.g., aromatase inhibitors) Psychosocial: social isolation |
Intensive, personalized health self-management training; web-based behavioral counseling | |
Figure 1.
The 3P conceptual model for cancer-related fatigue.
3.1. Predisposing Factors
Patient characteristics conceptualized as predisposing factors in cancer-related fatigue include biological sex [63], genetics [34], body composition (e.g., body fat and low muscle mass) [64,65,66], and viral exposures [67,68]. Additionally, circadian rhythms could play a significant role in the etiology of fatigue through the modulation of arousal and sleep [54].
Predisposing risk factors for cancer-related fatigue include poor performance status, chemoradiotherapy, female sex, insomnia, neuroticism, pain, and depression [69]. In cancer-related fatigue, the role of genetic variation remains unclear. Twin studies have shown the heritability of fatigue to be between 6% and 50%, with a higher concordance in monozygotic twins than dizygotic twins. Some preliminary studies have identified sets of inflammation-related genetic polymorphisms that are associated with increased fatigue in cancer patients [34], but the generality of these effects remains to be determined. Genome-wide association studies (GWAS) in fatigue-related diseases have identified variants in genes involved in cognition and circadian rhythms [70,71,72]. We propose that genetic variants altering metabolic including inflammatory traits may also be associated with cancer-related fatigue through inflammation pathways. Publicly available lists of high-scoring genetic–metabolomic associations known as “genetically influenced metabotypes” include several variants located in or near genes encoding enzymes central to human lipid metabolism, including polyunsaturated fatty acid biosynthesis (e.g., FADS1, ELOVL2) and biosynthesis of phospholipids (e.g., SPT16A) [73], which have not been explored in cancer-related fatigue. Similarly, “genetically influenced inflammotypes” [74] can be identified by inflammatory-based genome-wide association studies (iWAS), but also have not yet been explored among cancer patients with fatigue.
Previous viral exposure—for example, to Epstein–Barr virus, human herpesvirus, Lyme disease, or COVID-19—may predispose individuals to fatigue through cell alterations, hyperinflammation, mitochondrial modulation, and autoimmunity, although research in this area is lacking [75,76]. Additionally, anthropometry measurements (e.g., obesity) have been associated with links in apnea, sleep quality, and inflammatory biomarkers.
3.2. Precipitating Factors
Factors that may initially precipitate the development of cancer-related fatigue remain unclear, though likely include metabolic dysregulation (alterations in metabolic genes and regulatory pathways), as well as inflammation (overproduction of pro-inflammatory cytokines) and accelerated cellular aging (e.g., the premature shortening of telomeres and altered DNA methylation) due to cancer treatment. For example, chemotherapy is known to accelerate aging [77,78]. Chemotherapy may also damage mitochondria in muscle and deconditioning of muscle that may contribute to perceptions of fatigue [79,80,81,82].
Multiplicative interactions between precipitating factors may also exist. Studies investigating muscle fatigue in cancer patients show metabolic dysregulation, including energy, lipid, and amino acid metabolism [83,84,85,86]. Furthermore, evidence supports that chemotherapy may damage mitochondria in muscle that in turn increases fatigue, and the deconditioning of muscle further contributes to perceptions of fatigue. In particular, studies have focused on tryptophan catabolism [87,88,89]. An essential amino acid, tryptophan drives de novo synthesis of serotonin and niacin. Serotonin modulates behavioral and neuropsychological processes and niacin produces NAD, a co-factor crucial for energy homeostasis that is linked with aging and circadian regulation (SIRT1). Trials modifying tryptophan have demonstrated reductions in physical and mental fatigue following endurance exercise [90]. Furthermore, metabolic disturbances related to chronic fatigue syndrome have included alterations in 20 metabolic pathways including sphingolipids, phospholipids, purine, cholesterol, microbial metabolites, pyroline-5-carboxylate, riboflavin, amino acids, peroxisomal and mitochondrial metabolism [91]. All are directly regulated by redox or the availability of NADPH, highlighting the importance of the mitochondria, cellular organelles that produce energy [91]. Sphingolipids and phospholipids accounted for almost 70% of the variation in metabolic phenotype in a study of 84 patients with chronic fatigue syndrome, and differences among males and females were observed. Area under the receiver operator characteristic curve analysis showed accuracies in predicting fatigue of 94% (95% CI = 84–100%) for males and 96% (95% CI = 86–100%) for females. Three other metabolomics studies of fatigue-associated diseases support the key role of sphingolipids and phospholipids in addition to irregularities in energy, amino acid, and nucleotide metabolism [92,93,94]. The alterations in sphingolipids may be related to impaired lipid metabolism and mitochondria energetics, with evidence suggesting that PPAR suppression in the muscle of cancer patients could mediate this [81,95,96]. Furthermore, in vitro studies have demonstrated that ceramides induce oxidant production in the mitochondria, have specific effects in certain tissues (e.g., adipocyte ceramides and inflammation) and increase oxidant activity [97], depressing muscle fiber force and exacerbating muscle fatigue [98]. While a number of pathological pathways have been identified as playing a role in cancer-related fatigue, it is possible that different mechanisms are responsible for different dimensions of fatigue (e.g., mental fatigue vs. physical fatigue). Further delineation of unique dimensions of fatigue associated with each pathway will assist in the identification of new intervention targets for the specific type of fatigue experienced.
3.3. Perpetuating Factors
Perpetuating factors are conceptualized as characteristics and behaviors that may worsen or prolong fatigue including poor dietary pattern, irregular meal timing [99,100], physical inactivity [101], and poor sleep [102,103,104,105,106,107]. Previous research suggests that anti-inflammatory dietary patterns, such as prudent and Mediterranean diets, offer a plausible mechanism to mitigate cancer-related fatigue through reducing inflammation and improving body composition [108,109,110]. The key components of the Mediterranean dietary pattern include high intake of vegetables, fruits, whole grains, legumes, and nuts; moderate intake of seafood and red wine; and olive oil as the main fat source [111,112]. Anti-inflammatory dietary patterns are associated with improvements in the gastrointestinal (GI) microbiota and lessening of metabolic endotoxemia, defined as a 2- to 3-fold increase in circulating levels of bacterial endotoxin [113]. In comparison, pro-inflammatory dietary patterns, such as the Western dietary pattern, widely consumed in the United States, is characterized by high consumption of red and processed meats; high consumption of sugar-sweetened beverages and refined grains; and low consumption of fresh fruits, vegetables, and legumes [114,115,116]. Western diets contribute to metabolic endotoxemia through changes in the GI microbiome and bacterial fermentation end products, intestinal physiology and barrier function, and enterohepatic circulation of bile acids [113]. Additionally, the Western dietary pattern has been correlated with pro-inflammatory markers associated with cancer-related fatigue, including tumor necrosis factor (TNF)-α, C-reactive protein, interleukin (IL)-6, and IL-8 [117]. Dietary patterns promoting hyperinsulinemia and chronic inflammation, including the empirical dietary index for hyperinsulinemia (EDIH) and empirical dietary inflammatory pattern (EDIP), strongly influence risk of weight gain, type 2 diabetes, cardiovascular disease, and cancer [118]. The EDIH and EDIP have predicted concentrations of known insulinemic and inflammatory biomarkers, and the EDIH further predicted risk of future cancer [119].
In addition to evaluating dietary patterns based on self-reported questionnaires, the role of diet in cancer-related fatigue can be investigated through nutritional metabolomics, the study of food-related metabolites in a biofluid that can provide an objective measure of recent or habitual dietary intake [120]. Moreover, untargeted metabolomics offers a discovery tool to identify small molecules both influenced by dietary behavior and associated with disease, thus characterizing endogenous response to diet, and metabolic targets for dietary intervention for disease prevention. To our knowledge, nutritional metabolomics studies of cancer-related fatigue are yet to be implemented. The microbiota has been recognized to play a role in human disease [121], and the mechanisms by which these microorganisms contribute to host health have been extensively investigated over the past decade. The microbiome, specifically bacterial metabolites, has been linked with inflammation and oxidation. Two studies in mice have suggested that the gut microbiota produces metabolites from dietary tryptophan that regulate inflammation in the gut and central nervous system [122].
In terms of general lifestyle, prior research in fatigue-associated diseases highlights the role of lipid mediators including sphingolipids, phospholipids, and oxygenated polyunsaturated fatty acids (PUFAs) (oxylipins). Sphingolipid metabolites play key roles in the regulation of both trafficking and function of immune cells, and there are indications that sphingolipid metabolism might be altered by inflammation [123]. Ceramides, key sphingolipids, promote numerous inflammatory processes, including induction of macrophages and B cells [124]. Prior studies indicate alteration of ceramide metabolism among patients with chronic fatigue syndrome [92]. Intervention trials show that diet can lower ceramide levels [125]. In the PREDIMED study, a Mediterranean dietary intervention mitigated potential deleterious effects of elevated plasma ceramide concentrations on cardiovascular disease [126]. Similarly, omega-3 polyunsaturated fatty acid (n3-PUFA) is a common phospholipid, which plays an important role in immunomodulatory activities. Ceramides and its metabolites have been proposed as an intermediate link between over-nutrition and certain underlying abnormalities driving disease risk, insulin resistance and low-grade inflammation [127,128,129]. Data suggest beneficial effects of n3-PUFA in reducing fatigue in cancer patients [33,130,131,132,133]. N-3 PUFA therapy upregulates the muscle transcriptome, including several pathways that control mitochondrial function in both human [134], and animal studies [135,136,137], emphasizing the role of energy metabolism. Other metabolic pathways related to diet that might also contribute to fatigue include dysregulated tryptophan catabolism. Tryptophan is an amino acid metabolized into several molecules involved in energy production [87,88,89]. Potential interventions might target modulation of tryptophan-related molecules via administration of branched chain amino acids. In addition to endogenous metabolites, untargeted approaches may identify unexpected or novel exposures that might play an important role in cancer-related fatigue by implicating exogenously derived chemicals. Adherence to specific dietary patterns (e.g., time-restricted eating) may offer a novel, cost-effective strategy to reduce cancer-related fatigue while quantification of targeted metabolites may allow for a robust evaluation of metabolite changes in people with cancer-related fatigue over time [138].
There is an interaction of diet, physical activity, and sleep on many levels (e.g., behavioral, circadian, obesity, metabolic). Particularly, intermittent fasting regimens have been hypothesized to influence metabolic regulation via effects on (a) circadian biology, (b) the gut microbiome, and (c) modifiable lifestyle behaviors, such as sleep [100]. Evidence suggests that irregular meal timing may impact metabolic health. Specifically, eating more frequently, reducing evening energy intake, and fasting for longer nightly intervals may lower systemic inflammation and subsequently reduce breast cancer risk [99]. In another study examining associations between fasting duration, timing of first and last meals, and cardiometabolic endpoints using data from the National Health and Nutrition Examination Survey (NHANES), evidence suggested that there were beneficial effects on cardiometabolic health of starting energy consumption earlier in the day [139].
In addition to diet, physical inactivity and sleep disturbance represent key modifiable perpetuating factors associated with cancer-related fatigue [101]. In a systematic review and meta-analysis of randomized controlled trials, physical activity has been identified as effective for mitigating cancer-related fatigue in colorectal cancer [140]. Moderate-intensity aerobic exercise training and a combination of moderate-intensity aerobic and resistance training have reduced fatigue in patients with breast and prostate cancer, both during and following cancer therapy [141,142]. Reductions in fatigue from exercise training appear to result from both independent and supervised interventions [143], highlighting its potential applicability to a wide range of cancer patients and survivors. Similarly, sleep disturbance confers risk of cancer-related fatigue across various cancer diagnoses. A recent meta-analysis studying risk factors for cancer-related fatigue in 84 studies with 144,813 participants found that patients with insomnia had significantly higher odds of cancer-related fatigue [69]. Notably, the odds ratio for insomnia was higher than the odds ratio for treatment of chemoradiotherapy, although the magnitude of these effects was not formally compared. In patients with chronic myeloid leukemia receiving cognitive behavioral therapy for targeted-therapy-related fatigue, improvements in sleep and physical activity were associated with declines in fatigue [101]. Sleep disturbance and physical inactivity both contribute to known pathways for cancer-related fatigue (e.g., inflammation, circadian disruption) [144,145]. Emerging evidence suggests that sleep disturbance and physical inactivity may also implicate additional pathways, such as accelerated aging and gene expression through DNA methylation. For example, one study of 2078 women found that those with insomnia showed advanced biological age relative to chronological age [146]. In another study, individuals with insufficient sleep showed hypomethylation of DNA in regions associated with neuroplasticity and neurodegeneration [147]. Further research is necessary to elucidate the nuanced role of sleep and physical activity in cancer-related fatigue. Please see Table 1.
4. Clinical Implications
Use of the 3P model can benefit clinical oncology practice by offering pathways to prevention and mitigation strategies for cancer-related fatigue. First, screening for predisposing factors of cancer-related fatigue may facilitate risk stratification of cancer patients at the time of diagnosis. Risk stratification has been endorsed by experts in oncology healthcare delivery science as a personalized approach to care in which survivors are triaged to distinct care pathways based on their individual needs [148]. For example, patients who display a genetic predisposition to cancer-related fatigue and fit a predetermined risk profile of sociodemographic factors can be appropriately routed to prehabilitation and behavioral counseling to prevent fatigue such as by intervening upon the modifiable predisposing (e.g., obesity) or precipitating factors.
Additionally, if routed to appropriate care early in the onset of fatigue, these patients may learn mitigating physical and cognitive-behavioral strategies [149,150,151]. Prehabilitation, a multidisciplinary clinical process on the continuum of care that occurs between diagnosis and treatment, involves targeted interventions to reduce the incidence and severity of future impairments [152]. For patients deemed at high risk for cancer-related fatigue, prehabilitation may beneficially include prescribed physical activity regimens, energy conservation techniques, and dietary consultations to prevent fatigue onset during and after treatment. Targeting pre-treatment windows for multimodal prehabilitation can help patients increase their physiologic reserve or functional capacity as early as possible, mitigating the effects of fatigue-inducing circumstances such as physical inactivity, inflammation, anorexia, and skeletal muscle loss. A recent, single-group study involving individualized, home-based aerobic and resistance training prior to breast cancer surgery demonstrated reduced fatigue over the intervention period [153]. More evidence, including randomized controlled trials of prehabilitation, is needed to confirm longer-term, post-treatment impact on fatigue. Multimodal prehabilitation interventions can also be delivered concurrently with cancer therapies, such as exercise during neoadjuvant chemotherapy or radiation therapy [154]. Prehabilitation may also profitably include cognitive behavioral therapy to reduce dysfunctional fatigue-related beliefs. If routed to appropriate care early in the onset of fatigue, patients can learn cognitive-behavioral strategies for optimizing sleep, emotion, and daily activity patterns in order to mitigate fatigue [149,150,151,155]. In fact, a recent study found that reduced fatigue in cancer patients was attributable to changes in cognition (specifically self-efficacy) stemming from cognitive behavioral therapy rather than to changes in physical activity [156]. Interventions targeting self-efficacy may therefore be particularly beneficial for patients with higher risk of fatigue.
After stratifying patients by risk based on predisposing (e.g., genetic) and perpetuating (e.g., diet, physical activity) factors, healthcare practitioners can leverage the 3P model by conducting ongoing screening for precipitating factors of cancer-related fatigue. These factors—such as metabolic dysregulation and inflammation—may arise at any point during cancer treatment, and can be watched closely using biomarker testing. Through monitoring for precipitating factors, providers can identify at-risk individuals who are not initially flagged for prehabilitation due to predisposing factors. These individuals would then receive prehabilitation appropriate for their specific needs, including specific exercise interventions optimally timed for each patient’s unique constellation of ability, challenges, and needs [157,158,159].
While being monitored for the emergence of new precipitating factors, cancer patients can concurrently receive education and training in health self-management techniques to mitigate symptoms of cancer-related fatigue. Health self-management is defined as “the individual’s ability to manage the symptoms, treatment, physical and psychosocial consequences and lifestyle changes inherent in living with a chronic condition” [160]. Crucially, self-management training can teach cancer survivors the tools they need to sustainably maintain physical activity, adhere to dietary recommendations, and exercise energy conservation and sleep hygiene techniques. These health behaviors reduce the risk of long-lasting fatigue after the conclusion of the treatment phase. Furthermore, research has demonstrated that symptoms may appear in a cascade pattern, and treating symptoms higher in the cascade may prevent downstream symptoms. For example, sleep disturbance contributes to fatigue, which in turn contributes to depressed mood. Interventions for cancer-related fatigue therefore may be specifically targeted to mitigate symptoms early in the cascade, such as sleep disturbance [161].
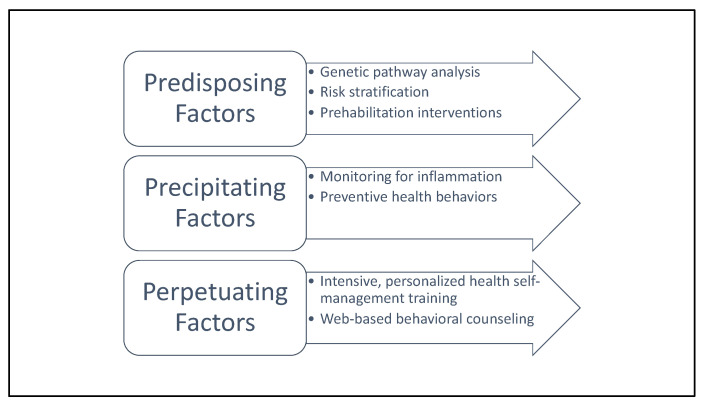
Indeed, while clinicians may benefit from education about the 3P model in order to leverage its content for clinical practice, patients may also benefit from comprehensive education about the predisposing, precipitating, and perpetuating factors involved in cancer-related fatigue to promote sustainable, independent management of symptoms. Future health self-management training endeavors for cancer survivors may be enhanced by support from web-based health self-management training tools. This emerging area of practice provides patients with hyper-tailored health self-management plans, sometimes enhanced by machine-learning to be granularly responsive to the unique strengths and challenges of each person [162,163]. Please see Figure 2 for an overview of recommended clinical actions organized using the 3P model. Further research is needed to establish web-based tools powered by artificial intelligence specifically for the self-management of cancer-related fatigue.
Figure 2.
Recommended clinical actions to address each 3P factor.
5. Future Directions for Research
While clinical care can leverage the 3P model to prevent or mitigate symptoms of cancer-related fatigue, future research is also warranted to further investigate its pathophysiology and efficacy/effectiveness of adopting a 3P model in cancer care. One potentially fruitful target area for study may be the metabolome. The metabolome directly reflects the underlying biochemical activity and state of cells and tissues, including energy production. Because the metabolome is downstream of genomics, transcriptomics, and proteomics, it may be the closest molecular phenotype to the patient-reported phenotype of cancer-related fatigue. The metabolic state of an individual at the time of illness is produced by current environmental and host biological conditions, host susceptibility, and the aggregate history, time, and magnitude of exposures recorded as metabolic memory [164]. Moreover, preclinical research has recently identified inflammation-independent “metabolic reprogramming” as a mediator of cancer-induced fatigue in animal models [165,166]. Thus, the metabolome could provide a comprehensive snapshot of cellular processes at a single point in time that is also representative of cumulative exposures, ideal for discovery of new mechanisms of cancer-related fatigue.
The 3P framework proposed here to conceptualize cancer-related fatigue may also be applicable to fatigue related to other conditions such as chronic fatigue syndrome, post-COVID syndrome, rheumatoid arthritis, and multiple sclerosis. Through applying the 3P framework, researchers and clinicians studying fatigue across a wide variety of illnesses and chronic diseases may be able to more readily understand the pathophysiology of fatigue as it presents across various diagnoses, as well as systematically identify and mitigate predisposing, precipitating, and perpetuating factors relevant to unique populations experiencing fatigue.
6. Conclusions
For the growing number of cancer survivors worldwide, fatigue presents a major hurdle to a return to function and quality of life after cancer treatment. Treatment options for cancer-related fatigue are still emerging, and our current understanding of its etiology is limited. The presented 3P model may be leveraged—particularly using metabolomics, the microbiome, and inflammation in conjunction with behavioral science—to better understand the pathophysiology of cancer-related fatigue. While application of the 3P model alone will not be enough to solve the complex problem of cancer-related fatigue, it may represent a key step towards ameliorating this pervasive issue for patients. A clinical focus on organizing risk stratification and treatment around the 3P model would be warranted. Future research may benefit from expanding the 3P model to understand fatigue not only in oncology, but also in the wider context of a variety of chronic conditions.
Funding
This study was funded by the National Cancer Institute NR018762 [principal investigators Jane C. Figueiredo and Heather S. L. Jim] and T32CA090314 [multiple principal investigators, Thomas Brandon and Susan Vadaparampil].
Conflicts of Interest
Brian Gonzalez is an advisory board member for Elly Health, Inc., a former paid consultant for KemPharm, and a former paid consultant for SureMed Compliance, none of which is relevant to this manuscript. Heather Jim is a consultant for Janssen Scientific Affairs and Merck and has grant funding from Kite Pharma. All other others declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Cella D., Davis K., Breitbart W., Curt G. Cancer-related fatigue: Prevalence of proposed diagnostic criteria in a United States sample of cancer survivors. J. Clin. Oncol. 2001;19:3385–3391. doi: 10.1200/JCO.2001.19.14.3385. [DOI] [PubMed] [Google Scholar]
- 2.Bower J.E. Cancer-related fatigue-mechanisms, risk factors, and treatments. Nat. Rev. Clin. Oncol. 2014;11:597–609. doi: 10.1038/nrclinonc.2014.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Berger A.M., Mooney K., Alvarez-Perez A., Breitbart W.S., Carpenter K.M., Cella D., Cleeland C., Dotan E., Eisenberger M.A., Escalante C.P., et al. Cancer-Related Fatigue, Version 2.2015. J. Natl. Compr. Canc. Netw. 2015;13:1012–1039. doi: 10.6004/jnccn.2015.0122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Borneman T., Piper B.F., Koczywas M., Munevar C.M., Sun V., Unman G.C., Ferrell B.R. A qualitative analysis of cancer-related fatigue in ambulatory oncology. Clin. J. Oncol. Nurs. 2012;16:E26–E32. doi: 10.1188/12.CJON.E26-E32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Poulson M.J. Not just tired. J. Clin. Oncol. 2001;19:4180–4181. doi: 10.1200/JCO.2001.19.21.4180. [DOI] [PubMed] [Google Scholar]
- 6.Barsevick A.M., Irwin M.R., Hinds P., Miller A., Berger A., Jacobsen P., Ancoli-Israel S., Reeve B.B., Mustian K., O’Mara A., et al. Recommendations for high-priority research on cancer-related fatigue in children and adults. J. Natl. Cancer Inst. 2013;105:1432–1440. doi: 10.1093/jnci/djt242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen M.L., Liu L.N., Miaskowski C., Chen S.C., Lin Y.C., Wang J.S. Presurgical symptom profiles predict quality of life 2 years after surgery in women with breast cancer. Support Care Cancer. 2016;24:243–251. doi: 10.1007/s00520-015-2784-8. [DOI] [PubMed] [Google Scholar]
- 8.Byar K.L., Berger A.M., Bakken S.L., Cetak M.A. Impact of adjuvant breast cancer chemotherapy on fatigue, other symptoms, and quality of life. Oncol. Nurs. Forum. 2006;33:E18–E26. doi: 10.1188/06.ONF.E18-E26. [DOI] [PubMed] [Google Scholar]
- 9.Lindbohm M.L., Kuosma E., Taskila T., Hietanen P., Carlsen K., Gudbergsson S., Gunnarsdottir H. Early retirement and non-employment after breast cancer. Psychooncology. 2014;23:634–641. doi: 10.1002/pon.3459. [DOI] [PubMed] [Google Scholar]
- 10.Duijts S.F., Faber M.M., Oldenburg H.S., van Beurden M., Aaronson N.K. Effectiveness of behavioral techniques and physical exercise on psychosocial functioning and health-related quality of life in breast cancer patients and survivors—A meta-analysis. Psychooncology. 2011;20:115–126. doi: 10.1002/pon.1728. [DOI] [PubMed] [Google Scholar]
- 11.Goedendorp M.M., Gielissen M.F., Verhagen C.A., Bleijenberg G. Psychosocial interventions for reducing fatigue during cancer treatment in adults. Cochrane Database Syst. Rev. 2009;2009:CD006953. doi: 10.1002/14651858.CD006953.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jacobsen P.B., Donovan K.A., Vadaparampil S.T., Small B.J. Systematic review and meta-analysis of psychological and activity-based interventions for cancer-related fatigue. Health Psychol. 2007;26:660–667. doi: 10.1037/0278-6133.26.6.660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kangas M., Bovbjerg D.H., Montgomery G.H. Cancer-related fatigue: A systematic and meta-analytic review of non-pharmacological therapies for cancer patients. Psychol. Bull. 2008;134:700–741. doi: 10.1037/a0012825. [DOI] [PubMed] [Google Scholar]
- 14.Mustian K.M., Alfano C.M., Heckler C., Kleckner A.S., Kleckner I.R., Leach C.R., Mohr D., Palesh O.G., Peppone L.J., Piper B.F., et al. Comparison of Pharmaceutical, Psychological, and Exercise Treatments for Cancer-Related Fatigue: A Meta-analysis. JAMA Oncol. 2017;3:961–968. doi: 10.1001/jamaoncol.2016.6914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Berenson J.R., Yellin O., Shamasunder H.K., Chen C.S., Charu V., Woliver T.B., Sanani S., Schlutz M., Nassir Y., Swift R.A., et al. A phase 3 trial of armodafinil for the treatment of cancer-related fatigue for patients with multiple myeloma. Support Care Cancer. 2015;23:1503–1512. doi: 10.1007/s00520-014-2486-7. [DOI] [PubMed] [Google Scholar]
- 16.Jean-Pierre P., Morrow G.R., Roscoe J.A., Heckler C., Mohile S., Janelsins M., Peppone L., Hemstad A., Esparaz B.T., Hopkins J.O. A phase 3 randomized, placebo-controlled, double-blind, clinical trial of the effect of modafinil on cancer-related fatigue among 631 patients receiving chemotherapy: A University of Rochester Cancer Center Community Clinical Oncology Program Research base study. Cancer. 2010;116:3513–3520. doi: 10.1002/cncr.25083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Morrow G.R., Hickok J.T., Roscoe J.A., Raubertas R.F., Andrews P.L., Flynn P.J., Hynes H.E., Banerjee T.K., Kirshner J.J., King D.K. Differential effects of paroxetine on fatigue and depression: A randomized, double-blind trial from the University of Rochester Cancer Center Community Clinical Oncology Program. J. Clin. Oncol. 2003;21:4635–4641. doi: 10.1200/JCO.2003.04.070. [DOI] [PubMed] [Google Scholar]
- 18.Roscoe J.A., Morrow G.R., Hickok J.T., Mustian K.M., Griggs J.J., Matteson S.E., Bushunow P., Qazi R., Smith B. Effect of paroxetine hydrochloride (Paxil) on fatigue and depression in breast cancer patients receiving chemotherapy. Breast Cancer Res. Treat. 2005;89:243–249. doi: 10.1007/s10549-004-2175-1. [DOI] [PubMed] [Google Scholar]
- 19.Spathis A., Fife K., Blackhall F., Dutton S., Bahadori R., Wharton R., O’Brien M., Stone P., Benepal T., Bates N., et al. Modafinil for the treatment of fatigue in lung cancer: Results of a placebo-controlled, double-blind, randomized trial. J. Clin. Oncol. 2014;32:1882–1888. doi: 10.1200/JCO.2013.54.4346. [DOI] [PubMed] [Google Scholar]
- 20.Stockler M.R., O’Connell R., Nowak A.K., Goldstein D., Turner J., Wilcken N.R., Wyld D., Abdi E.A., Glasgow A., Beale P.J., et al. Effect of sertraline on symptoms and survival in patients with advanced cancer, but without major depression: A placebo-controlled double-blind randomised trial. Lancet Oncol. 2007;8:603–612. doi: 10.1016/S1470-2045(07)70148-1. [DOI] [PubMed] [Google Scholar]
- 21.Qu D., Zhang Z., Yu X., Zhao J., Qiu F., Huang J. Psychotropic drugs for the management of cancer-related fatigue: A systematic review and meta-analysis. Eur. J. Cancer Care. 2015;25:970–979. doi: 10.1111/ecc.12397. [DOI] [PubMed] [Google Scholar]
- 22.Gong S., Sheng P., Jin H., He H., Qi E., Chen W., Dong Y., Hou L. Effect of methylphenidate in patients with cancer-related fatigue: A systematic review and meta-analysis. PLoS ONE. 2014;9:e84391. doi: 10.1371/journal.pone.0084391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bruera E., Yennurajalingam S., Palmer J.L., Perez-Cruz P.E., Frisbee-Hume S., Allo J.A., Williams J.L., Cohen M.Z. Methylphenidate and/or a nursing telephone intervention for fatigue in patients with advanced cancer: A randomized, placebo-controlled, phase II trial. J. Clin. Oncol. 2013;31:2421–2427. doi: 10.1200/JCO.2012.45.3696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Moraska A.R., Sood A., Dakhil S.R., Sloan J.A., Barton D., Atherton P.J., Suh J.J., Griffin P.C., Johnson D.B., Ali A., et al. Phase III, randomized, double-blind, placebo-controlled study of long-acting methylphenidate for cancer-related fatigue: North Central Cancer Treatment Group NCCTG-N05C7 trial. J. Clin. Oncol. 2010;28:3673–3679. doi: 10.1200/JCO.2010.28.1444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ho R.T., Fong T.C., Cheung I.K. Cancer-related fatigue in breast cancer patients: Factor mixture models with continuous non-normal distributions. Qual. Life Res. 2014;23:2909–2916. doi: 10.1007/s11136-014-0731-7. [DOI] [PubMed] [Google Scholar]
- 26.Minton O., Stone P.C. A comparison of cognitive function, sleep and activity levels in disease-free breast cancer patients with or without cancer-related fatigue syndrome. BMJ Support Palliat. Care. 2012;2:231–238. doi: 10.1136/bmjspcare-2011-000172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Saligan L.N., Olson K., Filler K., Larkin D., Cramp F., Sriram Y., Escalante C.P., Del Giglio A., Kober K.M., Kamath J., et al. The biology of cancer-related fatigue: A review of the literature. Support Care Cancer. 2015;23:2461–2478. doi: 10.1007/s00520-015-2763-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ryan J.L., Carroll J.K., Ryan E.P., Mustian K.M., Fiscella K., Morrow G.R. Mechanisms of cancer-related fatigue. Oncologist. 2007;12((Suppl. S1)):22–34. doi: 10.1634/theoncologist.12-S1-22. [DOI] [PubMed] [Google Scholar]
- 29.Jim H.S., Park J.Y., Permuth-Wey J., Rincon M.A., Phillips K.M., Small B.J., Jacobsen P.B. Genetic predictors of fatigue in prostate cancer patients treated with androgen deprivation therapy: Preliminary findings. Brain Behav. Immun. 2012;26:1030–1036. doi: 10.1016/j.bbi.2012.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Black D.S., Cole S.W., Christodoulou G., Figueiredo J.C. Genomic mechanisms of fatigue in survivors of colorectal cancer. Cancer. 2018;124:2637–2644. doi: 10.1002/cncr.31356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bower J.E., Ganz P.A., Irwin M.R., Arevalo J.M., Cole S.W. Fatigue and gene expression in human leukocytes: Increased NF-kappaB and decreased glucocorticoid signaling in breast cancer survivors with persistent fatigue. Brain Behav. Immun. 2011;25:147–150. doi: 10.1016/j.bbi.2010.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Felger J.C., Cole S.W., Pace T.W., Hu F., Woolwine B.J., Doho G.H., Raison C.L., Miller A.H. Molecular signatures of peripheral blood mononuclear cells during chronic interferon-alpha treatment: Relationship with depression and fatigue. Psychol. Med. 2012;42:1591–1603. doi: 10.1017/S0033291711002868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Alfano C.M., Imayama I., Neuhouser M.L., Kiecolt-Glaser J.K., Smith A.W., Meeske K., McTiernan A., Bernstein L., Baumgartner K.B., Ulrich C.M., et al. Fatigue, inflammation, and omega-3 and omega-6 fatty acid intake among breast cancer survivors. J. Clin. Oncol. 2012;30:1280–1287. doi: 10.1200/JCO.2011.36.4109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bower J.E., Ganz P.A., Irwin M.R., Castellon S., Arevalo J., Cole S.W. Cytokine genetic variations and fatigue among patients with breast cancer. J. Clin. Oncol. 2013;31:1656–1661. doi: 10.1200/JCO.2012.46.2143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bower J.E., Ganz P.A., Irwin M.R., Kwan L., Breen E.C., Cole S.W. Inflammation and behavioral symptoms after breast cancer treatment: Do fatigue, depression, and sleep disturbance share a common underlying mechanism? J. Clin. Oncol. 2011;29:3517–3522. doi: 10.1200/JCO.2011.36.1154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bower J.E., Ganz P.A., Tao M.L., Hu W., Belin T.R., Sepah S., Cole S., Aziz N. Inflammatory biomarkers and fatigue during radiation therapy for breast and prostate cancer. Clin. Cancer Res. 2009;15:5534–5540. doi: 10.1158/1078-0432.CCR-08-2584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Clevenger L., Schrepf A., Christensen D., DeGeest K., Bender D., Ahmed A., Goodheart M.J., Penedo F., Lubaroff D.M., Sood A.K., et al. Sleep disturbance, cytokines, and fatigue in women with ovarian cancer. Brain Behav. Immun. 2012;26:1037–1044. doi: 10.1016/j.bbi.2012.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Collado-Hidalgo A., Bower J.E., Ganz P.A., Cole S.W., Irwin M.R. Inflammatory biomarkers for persistent fatigue in breast cancer survivors. Clin. Cancer Res. 2006;12:2759–2766. doi: 10.1158/1078-0432.CCR-05-2398. [DOI] [PubMed] [Google Scholar]
- 39.Collado-Hidalgo A., Bower J.E., Ganz P.A., Irwin M.R., Cole S.W. Cytokine gene polymorphisms and fatigue in breast cancer survivors: Early findings. Brain Behav. Immun. 2008;22:1197–1200. doi: 10.1016/j.bbi.2008.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cuneo M.G., Schrepf A., Slavich G.M., Thaker P.H., Goodheart M., Bender D., Cole S.W., Sood A.K., Lutgendorf S.K. Diurnal cortisol rhythms, fatigue and psychosocial factors in five-year survivors of ovarian cancer. Psychoneuroendocrinology. 2017;84:139–142. doi: 10.1016/j.psyneuen.2017.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.de Raaf P.J., Sleijfer S., Lamers C.H., Jager A., Gratama J.W., van der Rijt C.C. Inflammation and fatigue dimensions in advanced cancer patients and cancer survivors: An explorative study. Cancer. 2012;118:6005–6011. doi: 10.1002/cncr.27613. [DOI] [PubMed] [Google Scholar]
- 42.Gelinas C., Fillion L. Factors related to persistent fatigue following completion of breast cancer treatment. Oncol. Nurs. Forum. 2004;31:269–278. doi: 10.1188/04.ONF.269-278. [DOI] [PubMed] [Google Scholar]
- 43.Gerber L.H., Stout N., McGarvey C., Soballe P., Shieh C.Y., Diao G., Springer B.A., Pfalzer L.A. Factors predicting clinically significant fatigue in women following treatment for primary breast cancer. Support Care Cancer. 2011;19:1581–1591. doi: 10.1007/s00520-010-0986-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hamre H., Zeller B., Kanellopoulos A., Ruud E., Fosså S.D., Loge J.H., Aukrust P., Halvorsen B., Mollnes T.E., Kiserud C.E. Serum cytokines and chronic fatigue in adults surviving after childhood leukemia and lymphoma. Brain Behav. Immun. 2013;30:80–87. doi: 10.1016/j.bbi.2013.01.006. [DOI] [PubMed] [Google Scholar]
- 45.Laird B.J., McMillan D.C., Fayers P., Fearon K., Kaasa S., Fallon M.T., Klepstad P. The systemic inflammatory response and its relationship to pain and other symptoms in advanced cancer. Oncologist. 2013;18:1050–1055. doi: 10.1634/theoncologist.2013-0120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Liu L., Mills P.J., Rissling M., Fiorentino L., Natarajan L., Dimsdale J.E., Sadler G.R., Parker B.A., Ancoli-Israel S. Fatigue and sleep quality are associated with changes in inflammatory markers in breast cancer patients undergoing chemotherapy. Brain Behav. Immun. 2012;26:706–713. doi: 10.1016/j.bbi.2012.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Meyers C.A., Albitar M., Estey E. Cognitive impairment, fatigue, and cytokine levels in patients with acute myelogenous leukemia or myelodysplastic syndrome. Cancer. 2005;104:788–793. doi: 10.1002/cncr.21234. [DOI] [PubMed] [Google Scholar]
- 48.Orre I.J., Murison R., Dahl A.A., Ueland T., Aukrust P., Fossa S.D. Levels of circulating interleukin-1 receptor antagonist and C-reactive protein in long-term survivors of testicular cancer with chronic cancer-related fatigue. Brain Behav. Immun. 2009;23:868–874. doi: 10.1016/j.bbi.2009.04.003. [DOI] [PubMed] [Google Scholar]
- 49.Orre I.J., Reinertsen K.V., Aukrust P., Dahl A.A., Fosså S.D., Ueland T., Murison R. Higher levels of fatigue are associated with higher CRP levels in disease-free breast cancer survivors. J. Psychosom. Res. 2011;71:136–141. doi: 10.1016/j.jpsychores.2011.04.003. [DOI] [PubMed] [Google Scholar]
- 50.Pertl M.M., Hevey D., Boyle N.T., Hughes M.M., Collier S., O’Dwyer A.M., Harkin A., Kennedy M.J., Connor T.J. C-reactive protein predicts fatigue independently of depression in breast cancer patients prior to chemotherapy. Brain Behav. Immun. 2013;34:108–119. doi: 10.1016/j.bbi.2013.07.177. [DOI] [PubMed] [Google Scholar]
- 51.Pusztai L., Mendoza T.R., Reuben J.M., Martinez M.M., Willey J.S., Lara J., Syed A., Fritsche H.A., Bruera E., Booser D., et al. Changes in plasma levels of inflammatory cytokines in response to paclitaxel chemotherapy. Cytokine. 2004;25:94–102. doi: 10.1016/j.cyto.2003.10.004. [DOI] [PubMed] [Google Scholar]
- 52.Schrepf A., Clevenger L., Christensen D., DeGeest K., Bender D., Ahmed A., Goodheart M.J., Dahmoush L., Penedo F., Lucci I.I.I.J.A., et al. Cortisol and inflammatory processes in ovarian cancer patients following primary treatment: Relationships with depression, fatigue, and disability. Brain Behav. Immun. 2013;30:S126–S134. doi: 10.1016/j.bbi.2012.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wang X.S., Shi Q., Williams L.A., Mao L., Cleeland C.S., Komaki R.R., Mobley G.M., Liao Z. Inflammatory cytokines are associated with the development of symptom burden in patients with NSCLC undergoing concurrent chemoradiation therapy. Brain Behav. Immun. 2010;24:968–974. doi: 10.1016/j.bbi.2010.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Barsevick A., Frost M., Zwinderman A., Hall P., Halyard M., Consortium G. I’m so tired: Biological and genetic mechanisms of cancer-related fatigue. Qual. Life Res. 2010;19:1419–1427. doi: 10.1007/s11136-010-9757-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Morrow G.R., Andrews P.L., Hickok J.T., Roscoe J.A., Matteson S. Fatigue associated with cancer and its treatment. Support Care Cancer. 2002;10:389–398. doi: 10.1007/s005200100293. [DOI] [PubMed] [Google Scholar]
- 56.Jim H.S., Hoogland A.I., Han H.S., Culakova E., Heckler C., Janelsins M., Williams G.C., Bower J., Cole S., Desta Z., et al. A randomized placebo-controlled trial of bupropion for Cancer-related fatigue: Study design and procedures. Contemp. Clin. Trials. 2020;91:105976. doi: 10.1016/j.cct.2020.105976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ashrafi F., Mousavi S., Karimi M. Potential Role of Bupropion Sustained Release for Cancer-Related Fatigue: A Double-Blind, Placebo-Controlled Study. Asian Pac. J. Cancer Prev. 2018;19:1547–1551. doi: 10.22034/APJCP.2018.19.6.1547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Salehifar E., Azimi S., Janbabai G., Zaboli E., Hendouei N., Saghafi F., Borhani S. Efficacy and safety of bupropion in cancer-related fatigue, a randomized double blind placebo controlled clinical trial. BMC Cancer. 2020;20:158. doi: 10.1186/s12885-020-6618-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Burks T.F. New agents for the treatment of cancer-related fatigue. Cancer. 2001;92:1714–1718. doi: 10.1002/1097-0142(20010915)92:6+<1714::AID-CNCR1502>3.0.CO;2-N. [DOI] [PubMed] [Google Scholar]
- 60.Wade D.T., Halligan P.W. The biopsychosocial model of illness: A model whose time has come. Clin. Rehabil. 2017;31:995–1004. doi: 10.1177/0269215517709890. [DOI] [PubMed] [Google Scholar]
- 61.Wright C.D., Tiani A.G., Billingsley A.L., Steinman S.A., Larkin K.T., McNeil D.W. A Framework for Understanding the Role of Psychological Processes in Disease Development, Maintenance, and Treatment: The 3P-Disease Model. Front. Psychol. 2019;10:2498. doi: 10.3389/fpsyg.2019.02498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Bower J.E. The role of neuro-immune interactions in cancer-related fatigue: Biobehavioral risk factors and mechanisms. Cancer. 2019;125:353–364. doi: 10.1002/cncr.31790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kilgour R.D., Vigano A., Trutschnigg B., Hornby L., Lucar E., Bacon S.L., Morais J.A. Cancer-related fatigue: The impact of skeletal muscle mass and strength in patients with advanced cancer. J. Cachexia Sarcopenia Muscle. 2010;1:177–185. doi: 10.1007/s13539-010-0016-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.van Baar H., Bours M.J., Beijer S., van Zutphen M., van Duijnhoven F.J., Kok D.E., Wesselink E., de Wilt J.H., Kampman E., Winkels R.M. Body composition and its association with fatigue in the first 2 years after colorectal cancer diagnosis. J. Cancer Surviv. 2021;15:597–606. doi: 10.1007/s11764-020-00953-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Neefjes E.C., Van Den Hurk R.M., Blauwhoff-Buskermolen S., van der Vorst M.J., Becker-Commissaris A., de van der Schueren M.A., Buffart L.M., Verheul H.M. Muscle mass as a target to reduce fatigue in patients with advanced cancer. J. Cachexia Sarcopenia Muscle. 2017;8:623–629. doi: 10.1002/jcsm.12199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Bye A., Sjøblom B., Wentzel-Larsen T., Grønberg B.H., Baracos V.E., Hjermstad M.J., Aass N., Bremnes R.M., Fløtten Ø., Jordhøy M. Muscle mass and association to quality of life in non-small cell lung cancer patients. J. Cachexia Sarcopenia Muscle. 2017;8:759–767. doi: 10.1002/jcsm.12206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Schur E., Afari N., Goldberg J., Buchwald D., Sullivan P.F. Twin analyses of fatigue. Twin Res. Hum. Genet. 2007;10:729–733. doi: 10.1375/twin.10.5.729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Sullivan P.F., Evengard B., Jacks A., Pedersen N.L. Twin analyses of chronic fatigue in a Swedish national sample. Psychol. Med. 2005;35:1327–1336. doi: 10.1017/S0033291705005222. [DOI] [PubMed] [Google Scholar]
- 69.Ma Y., He B., Jiang M., Yang Y., Wang C., Huang C., Han L. Prevalence and risk factors of cancer-related fatigue: A systematic review and meta-analysis. Int. J. Nurs. Stud. 2020;111:103707. doi: 10.1016/j.ijnurstu.2020.103707. [DOI] [PubMed] [Google Scholar]
- 70.Schlauch K.A., Khaiboullina S.F., De Meirleir K.L., Rawat S., Petereit J., Rizvanov A.A., Blatt N., Mijatovic T., Kulick D., Palotas A., et al. Genome-wide association analysis identifies genetic variations in subjects with myalgic encephalomyelitis/chronic fatigue syndrome. Transl. Psychiatry. 2016;6:e730. doi: 10.1038/tp.2015.208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Smith A.K., Fang H., Whistler T., Unger E.R., Rajeevan M.S. Convergent genomic studies identify association of GRIK2 and NPAS2 with chronic fatigue syndrome. Neuropsychobiology. 2011;64:183–194. doi: 10.1159/000326692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Deary V., Hagenaars S.P., Harris S.E., Hill W.D., Davies G., Liewald D.C., McIntosh A.M., Gale C.R., Deary I.J. Genetic contributions to self-reported tiredness. Mol. Psychiatry. 2018;23:609–620. doi: 10.1038/mp.2017.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Illig T., Gieger C., Zhai G., Römisch-Margl W., Wang-Sattler R., Prehn C., Altmaier E., Kastenmüller G., Kato B.S., Mewes H.W., et al. A genome-wide perspective of genetic variation in human metabolism. Nat. Genet. 2010;42:137–141. doi: 10.1038/ng.507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Wang T., Yin J., Miller A.H., Xiao C. A systematic review of the association between fatigue and genetic polymorphisms. Brain Behav. Immun. 2017;62:230–244. doi: 10.1016/j.bbi.2017.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Rasa S., Nora-Krukle Z., Henning N., Eliassen E., Shikova E., Harrer T., Scheibenbogen C., Murovska M., Prusty B.K. Chronic viral infections in myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) J. Transl. Med. 2018;16:268. doi: 10.1186/s12967-018-1644-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Wilson C. Concern coronavirus may trigger post-viral fatigue syndromes. New Sci. 2020;246:10–11. doi: 10.1016/S0262-4079(20)30746-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Sanoff H.K., Deal A.M., Krishnamurthy J., Torrice C., Dillon P., Sorrentino J., Ibrahim J.G., Jolly T.A., Williams G., Carey L.A., et al. Effect of cytotoxic chemotherapy on markers of molecular age in patients with breast cancer. J. Natl. Cancer Inst. 2014;106:dju057. doi: 10.1093/jnci/dju057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Smitherman A.B., Wood W.A., Mitin N., Ayer Miller V.L., Deal A.M., Davis I.J., Blatt J., Gold S.H., Muss H.B. Accelerated aging among childhood, adolescent, and young adult cancer survivors is evidenced by increased expression of p16(INK4a) and frailty. Cancer. 2020;126:4975–4983. doi: 10.1002/cncr.33112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Guigni B.A., Callahan D.M., Tourville T.W., Miller M.S., Fiske B., Voigt T., Korwin-Mihavics B., Anathy V., Dittus K., Toth M.J. Skeletal muscle atrophy and dysfunction in breast cancer patients: Role for chemotherapy-derived oxidant stress. Am. J. Physiol. Cell Physiol. 2018;315:C744–C756. doi: 10.1152/ajpcell.00002.2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Beaudry R.I., Kirkham A.A., Thompson R.B., Grenier J.G., Mackey J.R., Haykowsky M.J. Exercise Intolerance in Anthracycline-Treated Breast Cancer Survivors: The Role of Skeletal Muscle Bioenergetics, Oxygenation, and Composition. Oncologist. 2020;25:e852–e860. doi: 10.1634/theoncologist.2019-0777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Mallard J., Hucteau E., Hureau T.J., Pagano A.F. Skeletal Muscle Deconditioning in Breast Cancer Patients Undergoing Chemotherapy: Current Knowledge and Insights from Other Cancers. Front. Cell Dev. Biol. 2021;9:719643. doi: 10.3389/fcell.2021.719643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Kunz H.E., Port J.D., Kaufman K.R., Jatoi A., Hart C.R., Gries K.J., Lanza I.R., Kumar R. Skeletal muscle mitochondrial dysfunction and muscle and whole body functional deficits in cancer patients with weight loss. J. Appl. Physiol. 2022;132:388–401. doi: 10.1152/japplphysiol.00746.2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Forsyth L.M., Preuss H.G., MacDowell A.L., Chiazze L., Jr Birkmayer G.D., Bellanti J.A. Therapeutic effects of oral NADH on the symptoms of patients with chronic fatigue syndrome. Ann. Allergy Asthma Immunol. 1999;82:185–191. doi: 10.1016/S1081-1206(10)62595-1. [DOI] [PubMed] [Google Scholar]
- 84.Lane R.J., Barrett M.C., Taylor D.J., Kemp G.J., Lodi R. Heterogeneity in chronic fatigue syndrome: Evidence from magnetic resonance spectroscopy of muscle. Neuromuscul. Disord. 1998;8:204–209. doi: 10.1016/S0960-8966(98)00021-2. [DOI] [PubMed] [Google Scholar]
- 85.McCully K.K., Natelson B.H., Iotti S., Sisto S., Leigh J.S., Jr. Reduced oxidative muscle metabolism in chronic fatigue syndrome. Muscle Nerve. 1996;19:621–625. doi: 10.1002/(SICI)1097-4598(199605)19:5<621::AID-MUS10>3.0.CO;2-Q. [DOI] [PubMed] [Google Scholar]
- 86.Pastoris O., Aquilani R., Foppa P., Bovio G., Segagni S., Baiardi P., Catapano M., Maccario M., Salvadeo A., Dossena M. Altered muscle energy metabolism in post-absorptive patients with chronic renal failure. Scand. J. Urol. Nephrol. 1997;31:281–287. doi: 10.3109/00365599709070349. [DOI] [PubMed] [Google Scholar]
- 87.Kurz K., Fiegl M., Holzner B., Giesinger J., Pircher M., Weiss G., Denz H.A., Fuchs D. Fatigue in patients with lung cancer is related with accelerated tryptophan breakdown. PLoS ONE. 2012;7:e36956. doi: 10.1371/journal.pone.0036956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Newsholme E.A., Blomstrand E. Tryptophan, 5-hydroxytryptamine and a possible explanation for central fatigue. Adv. Exp. Med. Biol. 1995;384:315–320. doi: 10.1007/978-1-4899-1016-5_25. [DOI] [PubMed] [Google Scholar]
- 89.Yamashita M., Yamamoto T. Tryptophan circuit in fatigue: From blood to brain and cognition. Brain Res. 2017;1675:116–126. doi: 10.1016/j.brainres.2017.09.002. [DOI] [PubMed] [Google Scholar]
- 90.Newsholme E.A., Blomstrand E. Branched-chain amino acids and central fatigue. J. Nutr. 2006;136:274S–276S. doi: 10.1093/jn/136.1.274S. [DOI] [PubMed] [Google Scholar]
- 91.Naviaux R.K., Naviaux J.C., Li K., Bright A.T., Alaynick W.A., Wang L., Baxter A., Nathan N., Anderson W., Gordon E. Metabolic features of chronic fatigue syndrome. Proc. Natl. Acad. Sci. USA. 2016;113:E5472–E5480. doi: 10.1073/pnas.1607571113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Nagy-Szakal D., Barupal D.K., Lee B., Che X., Williams B.L., Kahn E.J., Ukaigwe J.E., Bateman L., Klimas N.G., Komaroff A.L., et al. Insights into myalgic encephalomyelitis/chronic fatigue syndrome phenotypes through comprehensive metabolomics. Sci. Rep. 2018;8:10056. doi: 10.1038/s41598-018-28477-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Freidin M.B., Wells H.R.R., Potter T., Livshits G., Menni C., Williams F.M.K. Metabolomic markers of fatigue: Association between circulating metabolome and fatigue in women with chronic widespread pain. Biochim. Biophys. Acta Mol. Basis Dis. 2018;1864:601–606. doi: 10.1016/j.bbadis.2017.11.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Surowiec I., Gjesdal C.G., Jonsson G., Norheim K.B., Lundstedt T., Trygg J., Omdal R. Metabolomics study of fatigue in patients with rheumatoid arthritis naive to biological treatment. Rheumatol. Int. 2016;36:703–711. doi: 10.1007/s00296-016-3426-2. [DOI] [PubMed] [Google Scholar]
- 95.Wilson H.E., Rhodes K.K., Rodriguez D., Chahal I., Stanton D.A., Bohlen J., Davis M., Infante A.M., Hazard-Jenkins H., Klinke D.J., et al. Human Breast Cancer Xenograft Model Implicates Peroxisome Proliferator-activated Receptor Signaling as Driver of Cancer-induced Muscle Fatigue. Clin. Cancer Res. 2019;25:2336–2347. doi: 10.1158/1078-0432.CCR-18-1565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Wilson H.E., Stanton D.A., Rellick S., Geldenhuys W., Pistilli E.E. Breast cancer-associated skeletal muscle mitochondrial dysfunction and lipid accumulation is reversed by PPARG. Am. J. Physiol. Cell Physiol. 2021;320:C577–C590. doi: 10.1152/ajpcell.00264.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Chaurasia B., Talbot C.L., Summers S.A. Adipocyte Ceramides—The Nexus of Inflammation and Metabolic Disease. Front. Immunol. 2020;11:576347. doi: 10.3389/fimmu.2020.576347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Ferreira L.F., Moylan J.S., Gilliam L.A., Smith J.D., Nikolova-Karakashian M., Reid M.B. Sphingomyelinase stimulates oxidant signaling to weaken skeletal muscle and promote fatigue. Am. J. Physiol. Cell Physiol. 2010;299:C552–C560. doi: 10.1152/ajpcell.00065.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Marinac C.R., Sears D.D., Natarajan L., Gallo L.C., Breen C.I., Patterson R.E. Frequency and Circadian Timing of Eating May Influence Biomarkers of Inflammation and Insulin Resistance Associated with Breast Cancer Risk. PLoS ONE. 2015;10:e0136240. doi: 10.1371/journal.pone.0136240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Patterson R.E., Sears D.D. Metabolic Effects of Intermittent Fasting. Annu. Rev. Nutr. 2017;37:371–393. doi: 10.1146/annurev-nutr-071816-064634. [DOI] [PubMed] [Google Scholar]
- 101.Hyland K.A., Nelson A.M., Eisel S.L., Hoogland A.I., Ibarz-Pinilla J., Sweet K., Jacobsen P.B., Knoop H., Jim H.S. Fatigue Perpetuating Factors as Mediators of Change in a Cognitive Behavioral Intervention for Targeted Therapy-Related Fatigue in Chronic Myeloid Leukemia: A Pilot Study. Ann. Behav. Med. 2022;56:137–145. doi: 10.1093/abm/kaab035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Cormie P., Zopf E.M., Zhang X., Schmitz K.H. The Impact of Exercise on Cancer Mortality, Recurrence, and Treatment-Related Adverse Effects. Epidemiol. Rev. 2017;39:71–92. doi: 10.1093/epirev/mxx007. [DOI] [PubMed] [Google Scholar]
- 103.Ariza-Garcia A., Galiano-Castillo N., Cantarero-Villanueva I., Fernandez-Lao C., Diaz-Rodriguez L., Arroyo-Morales M. Influence of physical inactivity in psychophysiological state of breast cancer survivors. Eur. J. Cancer Care. 2013;22:738–745. doi: 10.1111/ecc.12101. [DOI] [PubMed] [Google Scholar]
- 104.van Zutphen M., Kampman E., Giovannucci E.L., van Duijnhoven F.J.B. Lifestyle after Colorectal Cancer Diagnosis in Relation to Survival and Recurrence: A Review of the Literature. Curr. Colorectal. Cancer Rep. 2017;13:370–401. doi: 10.1007/s11888-017-0386-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Naqash A.R., Kihn-Alarcón A.J., Stavraka C., Kerrigan K., Vareki S.M., Pinato D.J., Puri S. The role of gut microbiome in modulating response to immune checkpoint inhibitor therapy in cancer. Ann. Transl. Med. 2021;9:1034. doi: 10.21037/atm-20-6427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Carroll J.E., Small B.J., Tometich D.B., Zhai W., Zhou X., Luta G., Ahles T.A., Saykin A.J., Nudelman K.N., Clapp J.D., et al. Sleep disturbance and neurocognitive outcomes in older patients with breast cancer: Interaction with genotype. Cancer. 2019;125:4516–4524. doi: 10.1002/cncr.32489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Liu L., Fiorentino L., Rissling M., Natarajan L., Parker B.A., Dimsdale J.E., Mills P.J., Sadler G.R., Ancoli-Israel S. Decreased health-related quality of life in women with breast cancer is associated with poor sleep. Behav. Sleep Med. 2013;11:189–206. doi: 10.1080/15402002.2012.660589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Alfano C.M., Day J.M., Katz M.L., Herndon J.E., Bittoni M.A., Oliveri J.M., Donohue K., Paskett E.D. Exercise and dietary change after diagnosis and cancer-related symptoms in long-term survivors of breast cancer: CALGB 79804. Psychooncology. 2009;18:128–133. doi: 10.1002/pon.1378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Zick S.M., Sen A., Han-Markey T.L., Harris R.E. Examination of the association of diet and persistent cancer-related fatigue: A pilot study. Oncol. Nurs. Forum. 2013;40:E41–E49. doi: 10.1188/13.ONF.E41-E49. [DOI] [PubMed] [Google Scholar]
- 110.Schwingshackl L., Hoffmann G. Mediterranean dietary pattern, inflammation and endothelial function: A systematic review and meta-analysis of intervention trials. Nutr. Metab. Cardiovasc Dis. 2014;24:929–939. doi: 10.1016/j.numecd.2014.03.003. [DOI] [PubMed] [Google Scholar]
- 111.Sofi F., Abbate R., Gensini G.F., Casini A. Accruing evidence on benefits of adherence to the Mediterranean diet on health: An updated systematic review and meta-analysis. Am. J. Clin. Nutr. 2010;92:1189–1196. doi: 10.3945/ajcn.2010.29673. [DOI] [PubMed] [Google Scholar]
- 112.Mentella M.C., Scaldaferri F., Ricci C., Gasbarrini A., Miggiano G.A.D. Cancer and Mediterranean Diet: A Review. Nutrients. 2019;11:2059. doi: 10.3390/nu11092059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Bailey M.A., Holscher H.D. Microbiome-Mediated Effects of the Mediterranean Diet on Inflammation. Adv. Nutr. 2018;9:193–206. doi: 10.1093/advances/nmy013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Christ A., Lauterbach M., Latz E. Western Diet and the Immune System: An Inflammatory Connection. Immunity. 2019;51:794–811. doi: 10.1016/j.immuni.2019.09.020. [DOI] [PubMed] [Google Scholar]
- 115.Crowder S.L., Sarma K.P., Mondul A.M., Chen Y.T., Li Z., Pepino M.Y., Zarins K.R., Wolf G.T., Rozek L.S., Arthur A.E. Pretreatment Dietary Patterns Are Associated with the Presence of Nutrition Impact Symptoms 1 Year after Diagnosis in Patients with Head and Neck Cancer. Cancer Epidemiol. Biomarkers Prev. 2019;28:1652–1659. doi: 10.1158/1055-9965.EPI-19-0128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Argirion I., Arthur A.E., Zarins K.R., Bellile E., Crowder S.L., Amlani L., Taylor J.M., Wolf G.T., McHugh J., Nguyen A., et al. Pretreatment Dietary Patterns, Serum Carotenoids and Tocopherols Influence Tumor Immune Response in Head and Neck Squamous Cell Carcinoma. Nutr. Cancer. 2021;73:2614–2626. doi: 10.1080/01635581.2020.1842895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Baguley B.J., Skinner T.L., Jenkins D.G., Wright O.R.L. Mediterranean-style dietary pattern improves cancer-related fatigue and quality of life in men with prostate cancer treated with androgen deprivation therapy: A pilot randomised control trial. Clin. Nutr. 2021;40:245–254. doi: 10.1016/j.clnu.2020.05.016. [DOI] [PubMed] [Google Scholar]
- 118.Shi N., Aroke D., Jin Q., Lee D.H., Hussan H., Zhang X., Manson J.E., LeBlanc E.S., Barac A., Arcan C., et al. Proinflammatory and Hyperinsulinemic Dietary Patterns Are Associated with Specific Profiles of Biomarkers Predictive of Chronic Inflammation, Glucose-Insulin Dysregulation, and Dyslipidemia in Postmenopausal Women. Front. Nutr. 2021;8:690428. doi: 10.3389/fnut.2021.690428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Aroke D., Folefac E., Shi N., Jin Q., Clinton S.K., Tabung F.K. Inflammatory and Insulinemic Dietary Patterns: Influence on Circulating Biomarkers and Prostate Cancer Risk. Cancer Prev. Res. 2020;13:841–852. doi: 10.1158/1940-6207.CAPR-20-0236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Maruvada P., Lampe J.W., Wishart D.S., Barupal D., Chester D.N., Dodd D., Djoumbou-Feunang Y., Dorrestein P.C., Dragsted L.O., Draper J., et al. Perspective: Dietary Biomarkers of Intake and Exposure-Exploration with Omics Approaches. Adv. Nutr. 2020;11:200–215. doi: 10.1093/advances/nmz075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Descamps H.C., Herrmann B., Wiredu D., Thaiss C.A. The path toward using microbial metabolites as therapies. EBioMedicine. 2019;44:747–754. doi: 10.1016/j.ebiom.2019.05.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Marsland B.J. Regulating inflammation with microbial metabolites. Nat. Med. 2016;22:581–583. doi: 10.1038/nm.4117. [DOI] [PubMed] [Google Scholar]
- 123.Maceyka M., Spiegel S. Sphingolipid metabolites in inflammatory disease. Nature. 2014;510:58–67. doi: 10.1038/nature13475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Chiurchiu V., Leuti A., Maccarrone M. Bioactive Lipids and Chronic Inflammation: Managing the Fire Within. Front. Immunol. 2018;9:38. doi: 10.3389/fimmu.2018.00038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Mathews A.T., Famodu O.A., Olfert M.D., Murray P.J., Cuff C.F., Downes M.T., Haughey N.J., Colby S.E., Chantler P.D., Olfert I.M., et al. Efficacy of nutritional interventions to lower circulating ceramides in young adults: FRUVEDomic pilot study. Physiol. Rep. 2017;5:e13329. doi: 10.14814/phy2.13329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Wang D.D., Toledo E., Hruby A., Rosner B.A., Willett W.C., Sun Q., Razquin C., Zheng Y., Ruiz-Canela M., Guasch-Ferré M., et al. Plasma Ceramides, Mediterranean Diet, and Incident Cardiovascular Disease in the PREDIMED Trial (Prevencion con Dieta Mediterranea) Circulation. 2017;135:2028–2040. doi: 10.1161/CIRCULATIONAHA.116.024261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Summers S.A. Ceramides in insulin resistance and lipotoxicity. Prog. Lipid. Res. 2006;45:42–72. doi: 10.1016/j.plipres.2005.11.002. [DOI] [PubMed] [Google Scholar]
- 128.Holland W.L., Summers S.A. Sphingolipids, insulin resistance, and metabolic disease: New insights from in vivo manipulation of sphingolipid metabolism. Endocr. Rev. 2008;29:381–402. doi: 10.1210/er.2007-0025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Summers S.A. The ART of Lowering Ceramides. Cell Metab. 2015;22:195–196. doi: 10.1016/j.cmet.2015.07.019. [DOI] [PubMed] [Google Scholar]
- 130.George S.M., Alfano C.M., Neuhouser M.L., Smith A.W., Baumgartner R.N., Baumgartner K.B., Bernstein L., Ballard-Barbash R. Better postdiagnosis diet quality is associated with less cancer-related fatigue in breast cancer survivors. J. Cancer Surviv. 2014;8:680–687. doi: 10.1007/s11764-014-0381-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.George S.M., Neuhouser M.L., Mayne S.T., Irwin M.L., Albanes D., Gail M.H., Alfano C.M., Bernstein L., McTiernan A., Reedy J., et al. Postdiagnosis diet quality is inversely related to a biomarker of inflammation among breast cancer survivors. Cancer Epidemiol. Biomarkers Prev. 2010;19:2220–2228. doi: 10.1158/1055-9965.EPI-10-0464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Huang X., Zhang Q., Kang X., Song Y., Zhao W. Factors associated with cancer-related fatigue in breast cancer patients undergoing endocrine therapy in an urban setting: A cross-sectional study. BMC Cancer. 2010;10:453. doi: 10.1186/1471-2407-10-453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Zick S.M., Colacino J., Cornellier M., Khabir T., Surnow K., Djuric Z. Fatigue reduction diet in breast cancer survivors: A pilot randomized clinical trial. Breast Cancer Res. Treat. 2017;161:299–310. doi: 10.1007/s10549-016-4070-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Yoshino J., Smith G.I., Kelly S.C., Julliand S., Reeds D.N., Mittendorfer B. Effect of dietary n-3 PUFA supplementation on the muscle transcriptome in older adults. Physiol. Rep. 2016;4:e12785. doi: 10.14814/phy2.12785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Johnson M.L., Lalia A.Z., Dasari S., Pallauf M., Fitch M., Hellerstein M.K., Lanza I.R. Eicosapentaenoic acid but not docosahexaenoic acid restores skeletal muscle mitochondrial oxidative capacity in old mice. Aging Cell. 2015;14:734–743. doi: 10.1111/acel.12352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Mizunoya W., Iwamoto Y., Shirouchi B., Sato M., Komiya Y., Razin F.R., Tatsumi R., Sato Y., Nakamura M., Ikeuchi Y. Dietary fat influences the expression of contractile and metabolic genes in rat skeletal muscle. PLoS ONE. 2013;8:e80152. doi: 10.1371/journal.pone.0080152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Philp L.K., Heilbronn L.K., Janovska A., Wittert G.A. Dietary enrichment with fish oil prevents high fat-induced metabolic dysfunction in skeletal muscle in mice. PLoS ONE. 2015;10:e0117494. doi: 10.1371/journal.pone.0117494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.St-Onge M.P., Ard J., Baskin M.L., Chiuve S.E., Johnson H.M., Kris-Etherton P., Varady K. Meal Timing and Frequency: Implications for Cardiovascular Disease Prevention: A Scientific Statement from the American Heart Association. Circulation. 2017;135:e96–e121. doi: 10.1161/CIR.0000000000000476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Wirth M.D., Zhao L., Turner-McGrievy G.M., Ortaglia A. Associations between Fasting Duration, Timing of First and Last Meal, and Cardiometabolic Endpoints in the National Health and Nutrition Examination Survey. Nutrients. 2021;13:2686. doi: 10.3390/nu13082686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Dun L., Xian-Yi W., Xiao-Ying J. Effects of Moderate-To-Vigorous Physical Activity on Cancer-Related Fatigue in Patients with Colorectal Cancer: A Systematic Review and Meta-Analysis. Arch. Med. Res. 2020;51:173–179. doi: 10.1016/j.arcmed.2019.12.015. [DOI] [PubMed] [Google Scholar]
- 141.Cramp F., Byron-Daniel J. Exercise for the management of cancer-related fatigue in adults. Cochrane Database Syst. Rev. 2012;11:CD006145. doi: 10.1002/14651858.CD006145.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Juvet L.K., Thune I., Elvsaas I.Ø., Fors E.A., Lundgren S., Bertheussen G., Leivseth G., Oldervoll L.M. The effect of exercise on fatigue and physical functioning in breast cancer patients during and after treatment and at 6 months follow-up: A meta-analysis. Breast. 2017;33:166–177. doi: 10.1016/j.breast.2017.04.003. [DOI] [PubMed] [Google Scholar]
- 143.Campbell K.L., Winters-Stone K., Wiskemann J., May A.M., Schwartz A.L., Courneya K.S., Zucker D., Matthews C., Ligibel J., Gerber L., et al. Exercise Guidelines for Cancer Survivors: Consensus Statement from International Multidisciplinary Roundtable. Med. Sci. Sports Exerc. 2019;51:2375–2390. doi: 10.1249/MSS.0000000000002116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Depner C.M., Cogswell D.T., Bisesi P.J., Markwald R.R., Cruickshank-Quinn C., Quinn K., Melanson E.L., Reisdorph N., Wright K.P., Jr. Developing preliminary blood metabolomics-based biomarkers of insufficient sleep in humans. Sleep. 2020;43:zsz321. doi: 10.1093/sleep/zsz321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Xiao Q., Moore S.C., Keadle S.K., Xiang Y.B., Zheng W., Peters T.M., Leitzmann M.F., Ji B.T., Sampson J.N., Shu X.O., et al. Objectively measured physical activity and plasma metabolomics in the Shanghai Physical Activity Study. Int. J. Epidemiol. 2016;45:1433–1444. doi: 10.1093/ije/dyw033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Carroll J.E., Irwin M.R., Levine M., Seeman T.E., Absher D., Assimes T., Horvath S. Epigenetic Aging and Immune Senescence in Women with Insomnia Symptoms: Findings From the Women’s Health Initiative Study. Biol. Psychiatry. 2017;81:136–144. doi: 10.1016/j.biopsych.2016.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Lahtinen A., Puttonen S., Vanttola P., Viitasalo K., Sulkava S., Pervjakova N., Joensuu A., Salo P., Toivola A., Härmä M., et al. A distinctive DNA methylation pattern in insufficient sleep. Sci. Rep. 2019;9:1193. doi: 10.1038/s41598-018-38009-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Mayer D.K., Alfano C.M. Personalized Risk-Stratified Cancer Follow-Up Care: Its Potential for Healthier Survivors, Happier Clinicians, and Lower Costs. J. Natl. Cancer Inst. 2019;111:442–448. doi: 10.1093/jnci/djy232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Jim H.S., Hyland K.A., Nelson A.M., Pinilla-Ibarz J., Sweet K., Gielissen M., Bulls H., Hoogland A.I., Jacobsen P.B., Knoop H. Internet-assisted cognitive behavioral intervention for targeted therapy-related fatigue in chronic myeloid leukemia: Results from a pilot randomized trial. Cancer. 2020;126:174–180. doi: 10.1002/cncr.32521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Abrahams H.J., Gielissen M.F., Donders R.R., Goedendorp M.M., van der Wouw A.J., Verhagen C.A., Knoop H. The efficacy of Internet-based cognitive behavioral therapy for severely fatigued survivors of breast cancer compared with care as usual: A randomized controlled trial. Cancer. 2017;123:3825–3834. doi: 10.1002/cncr.30815. [DOI] [PubMed] [Google Scholar]
- 151.Van Gessel L.D., Abrahams H.J., Prinsen H., Bleijenberg G., Heins M., Twisk J., Van Laarhoven H.W., Verhagen S.C., Gielissen M.F., Knoop H. Are the effects of cognitive behavior therapy for severe fatigue in cancer survivors sustained up to 14 years after therapy? J. Cancer Surviv. 2018;12:519–527. doi: 10.1007/s11764-018-0690-z. [DOI] [PubMed] [Google Scholar]
- 152.Silver J.K. Cancer prehabilitation and its role in improving health outcomes and reducing health care costs. Semin. Oncol. Nurs. 2015;31:13–30. doi: 10.1016/j.soncn.2014.11.003. [DOI] [PubMed] [Google Scholar]
- 153.Brahmbhatt P., Sabiston C.M., Lopez C., Chang E., Goodman J., Jones J., McCready D., Randall I., Rotstein S., Santa Mina D. Feasibility of Prehabilitation Prior to Breast Cancer Surgery: A Mixed-Methods Study. Front Oncol. 2020;10:571091. doi: 10.3389/fonc.2020.571091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Loughney L., West M.A., Kemp G.J., Grocott M.P., Jack S. Exercise intervention in people with cancer undergoing neoadjuvant cancer treatment and surgery: A systematic review. Eur. J. Surg. Oncol. 2016;42:28–38. doi: 10.1016/j.ejso.2015.09.027. [DOI] [PubMed] [Google Scholar]
- 155.Abrahams H.J., Knoop H., Schreurs M., Aaronson N.K., Jacobsen P.B., Newton R.U., Courneya K.S., Aitken J.F., Arving C., Brandberg Y., et al. Moderators of the effect of psychosocial interventions on fatigue in women with breast cancer and men with prostate cancer: Individual patient data meta-analyses. Psychooncology. 2020;29:1772–1785. doi: 10.1002/pon.5522. [DOI] [PubMed] [Google Scholar]
- 156.Poort H., Müller F., Bleijenberg G., Verhagen S.A., Verdam M.G., Nieuwkerk P.T., Knoop H. Condition or cognition? Mechanism of change in fatigue in a randomized controlled trial of graded exercise therapy or cognitive behavior therapy for severe fatigue in patients with advanced cancer. J. Consult. Clin. Psychol. 2021;89:731–741. doi: 10.1037/ccp0000670. [DOI] [PubMed] [Google Scholar]
- 157.Van Vulpen J.K., Sweegers M.G., Peeters P.H., Courneya K.S., Newton R.U., Aaronson N.K., Jacobsen P.B., Galvão D.A., Chinapaw M.J., Steindorf K., et al. Moderators of Exercise Effects on Cancer-related Fatigue: A Meta-analysis of Individual Patient Data. Med. Sci. Sports Exerc. 2020;52:303–314. doi: 10.1249/MSS.0000000000002154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Gielissen M.F., Wiborg J.F., Verhagen C.A., Knoop H., Bleijenberg G. Examining the role of physical activity in reducing postcancer fatigue. Support Care Cancer. 2012;20:1441–1447. doi: 10.1007/s00520-011-1227-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Buffart L.M., Sweegers M.G., May A.M., Chinapaw M.J., van Vulpen J.K., Newton R.U., Galvão D.A., Aaronson N.K., Stuiver M.M., Jacobsen P.B., et al. Targeting Exercise Interventions to Patients with Cancer in Need: An Individual Patient Data Meta-Analysis. J. Natl. Cancer Inst. 2018;110:1190–1200. doi: 10.1093/jnci/djy161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Howell D., Mayer D.K., Fielding R., Eicher M., Verdonck-de Leeuw I.M., Johansen C., Soto-Perez-de-Celis E., Foster C., Chan R., Alfano C.M., et al. Management of Cancer and Health After the Clinic Visit: A Call to Action for Self-Management in Cancer Care. J. Natl. Cancer Inst. 2021;113:523–531. doi: 10.1093/jnci/djaa083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Jim H.S., Jacobsen P.B., Phillips K.M., Wenham R.M., Roberts W., Small B.J. Lagged relationships among sleep disturbance, fatigue, and depressed mood during chemotherapy. Health Psychol. 2013;32:768–774. doi: 10.1037/a0031322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.van der Hout A., van Uden-Kraan C.F., Holtmaat K., Jansen F., Lissenberg-Witte B.I., Nieuwenhuijzen G.A., Hardillo J.A., de Jong R.B., Tiren-Verbeet N.L., Sommeijer D.W., et al. Reasons for not reaching or using web-based self-management applications, and the use and evaluation of Oncokompas among cancer survivors, in the context of a randomised controlled trial. Internet Interv. 2021;25:100429. doi: 10.1016/j.invent.2021.100429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Haase K.R., Avery J., Bryant-Lukosius D., Kryzanowska M., Kukretti V., Liu G., Mayo S.J., Jones J., Howell D. Patient and clinician perspectives of desired features for a web-based self-management program (icanmanage.ca): Exposing patients “hard work” of managing acute cancer. Support Care Cancer. 2021;29:1989–1998. doi: 10.1007/s00520-020-05683-8. [DOI] [PubMed] [Google Scholar]
- 164.Naviaux R.K. Metabolic features of the cell danger response. Mitochondrion. 2014;16:7–17. doi: 10.1016/j.mito.2013.08.006. [DOI] [PubMed] [Google Scholar]
- 165.Grossberg A.J., Vichaya E.G., Christian D.L., Molkentine J.M., Vermeer D.W., Gross P.S., Vermeer P.D., Lee J.H., Dantzer R. Tumor-Associated Fatigue in Cancer Patients Develops Independently of IL1 Signaling. Cancer Res. 2018;78:695–705. doi: 10.1158/0008-5472.CAN-17-2168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Grossberg A.J., Vichaya E.G., Gross P.S., Ford B.G., Scott K.A., Estrada D., Vermeer D.W., Vermeer P., Dantzer R. Interleukin 6-independent metabolic reprogramming as a driver of cancer-related fatigue. Brain Behav. Immun. 2020;88:230–241. doi: 10.1016/j.bbi.2020.05.043. [DOI] [PMC free article] [PubMed] [Google Scholar]