Abstract
Ectopic spleen is a rare clinical entity characterized by splenic hypermobility which may be congenital or acquired. The spleen may be migrated to different positions in the peritoneum. The main complication is pedicular torsion with splenic volvulus, presenting as an emergency abdominal surgery. We present and discuss a case of ectopic and twisted spleen resulting in complete splenic infarction, diagnosed by ultrasound, confirmed by CT scan and treated by splenectomy.
Keywords: Wandering spleen, Splenic volvulus, Imaging
Introduction
Wandering spleen or Ectopic spleen results from a congenital or acquired defect in the means of attachment of the spleen, which makes it wander. Attached to a long pedicle, the spleen is located outside the left upper quadrant of the abdomen. It can therefore be palpated in all quadrants of the abdomen depending on the length of its pedicle.
Torsion of its pedicle is a serious complication, which should be diagnosed early; thus, avoiding splenectomy in case of irreversible splenic infarction, especially in young patients.
The aim of this paper is to report the case of a walking spleen revealed by an acute surgical abdomen secondary to pedicular torsion and a review of the literature.
Case presentation
We report the case of a 26-year-old woman, without any particular pathological history, who regularly presented with paroxysmal abdominal pain that resolved spontaneously. She was admitted to the emergency department for intense and persistent abdominal pain of the left hypochondrium and periumbilical.
The pain was preceded by a sensation of heaviness of sudden onset with bilious vomiting, without transit disorder or externalized digestive hemorrhage. All this in a context of apyrexia and conservation of the general state.
On examination: the patient was hemodynamically and respiratorily stable: T 37°, BP 12/06, HR 80 bpm and RR 16 cpm.
The abdomen was slightly distended with periumbilical and hypogastric tenderness. On palpation there was a mass straddling the umbilical and hypogastric region measuring 15 cm, firm and mobile.
The rectal examination was unremarkable.
Abdominal ultrasound was hampered by gastrointestinal gases, but showed a periumbilical mass and a vacuity of the splenic compartment.
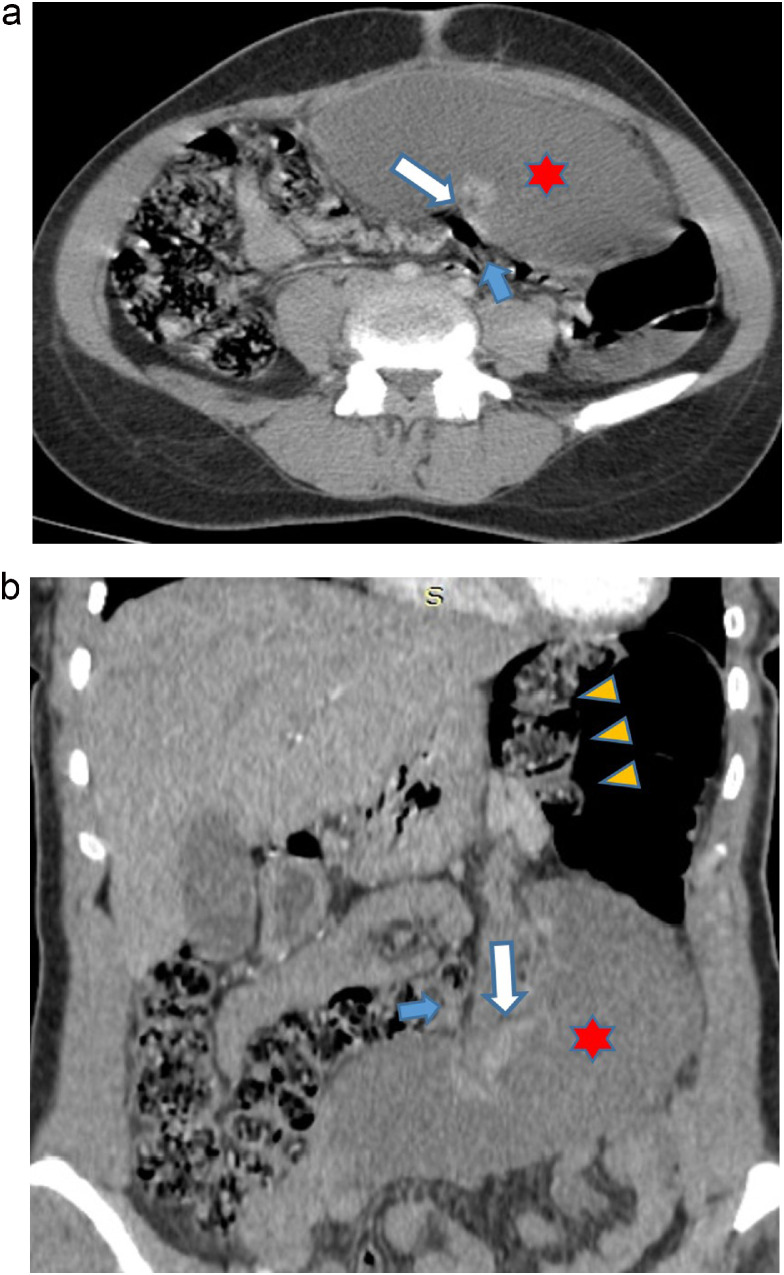
Abdominal and pelvic CT scan showed a large spleen measuring 15 cm in long axis, in an anterolateral left ectopic position at the level of the umbilicus. It was hypodense with regular contours and not enhanced after injection of contrast.
The arterial and venous splenic pedicle showed a swirl sign with significant infiltration of the peritoneal fat of the splenic hilum and a spontaneously hyperdense splenic artery in relation to a recent thrombus. This was suggestive of an ectopic spleen complicated by torsion of the pedicle with splenic infarction. (Fig. 1).
Fig. 1.
Axial (A) and coronal (B) CT scan images: Vacuity of the splenic lodge (yellow arrowheads). Spleen in an ectopic position at the umbilical level, hypodense and not enhanced after contrast injection (red star). Vascular pedicle torsion (swirl sign: white arrow). Infiltration of the peritoneal fat of the splenic hilum and around (blue arrow).
The indication for surgery was given after the patient had received pneumococcal and Hemophilus vaccinations as a preventive measure in patients with asplenia against encapsulated bacteria in combination with prophylactic antibiotic therapy (Amoxicillin and clavulanic acid).
The surgical procedure consisted of a median laparotomy straddling the umbilicus. Exploration revealed a large, free spleen with complete absence of the gastrosplenic and pancreatico-splenic omentum and splenocolic ligament; located medially. It was purplish with areas of infarction and necrosis and 2 turns of spiral around its pedicle (Fig. 2). The splenic compartment was empty, occupied by the intestinal loops. Splenectomy was performed with ligation section of the splenic artery and vein with subphrenic drainage by Redon drain. The postoperative course was straightforward. The total duration of hospitalization was 5 days. Pathological examination of the surgical specimen revealed a pale, soft spleen in relation to the ischemia surrounded by a red congestive border (inflammatory granulation tissue), diffuse foci of ischemic necrosis and the beginning of replacement of the necrotic tissue by a fleshy bud.
Fig. 2.
Surgical exploration revealed a large, voluminous free spleen with complete absence of the gastrosplenic and pancreatico-splenic omentum and splenocolic ligament, located medially in the umbilical region. Note the torsion of the splenic pedicle (white arrow). Areas of infarction and necrosis (yellow star).
Discussion
Ectopic spleen is a rare condition. It is most often seen in children [1]. The predominance of females is reported in the adult population [2], due to a congenital or acquired anomaly of its means of fixation by a defect or abnormal development of the gastrosplenic, phrenosplenic, splenorenal, splenocolic, splenopancreatic and colophrenic ligaments that normally maintain the organ in its compartment, resulting in the formation of a long splenic meso. It can migrate to any region of the peritoneal cavity [3].
As for the acquired form, several factors have been incriminated; such as gastric distension; splenomegaly; abdominal hyperlaxity; abdominal trauma and pregnancy.
In our case, the total absence of omentum confirms the congenital origin of this ectopic spleen [4].
A mobile spleen may be asymptomatic and discovered incidentally on clinical examination, abdominal imaging or preoperatively [5].
It may also manifest as an abdominal or pelvic mass, chronic intermittent abdominal pain with spontaneous torsion and untwisting [6] or an acute surgical abdomen in which abdominal pain is the main feature; sometimes associated with nausea, vomiting and fever indicating torsion of the ectopic spleen favored by its mobility, weight and length of its pedicle, which may be irreversible, as was the case in our observation.
The spleen may be healthy [7] or may be the site of an infarct [8], a pseudocyst [6] or splenomegaly [9]. As in our patient who presented with splenomegaly with diffuse necrosis.
These complications are the consequence of acute (infarction) or chronic (splenic pseudocyst, splenomegaly) torsion phenomena following venous congestion and inflammatory phenomena secondary to repeated torsion and detorsion [10].
The association of this acute abdominal picture with a mobile abdominal mass should raise the diagnosis of ectopic torsion of the spleen as well as other pathologies, which will lead us to perform an imaging workup to confirm the diagnosis.
Abdominal and pelvic ultrasound can confirm the diagnosis of ectopic torsion of the spleen in view of the vacuity of the splenic cavity and the demonstration of an abdominal mass reminiscent of the splenic echostructure but heterogeneous because it is the site of areas of necrosis.
The absence of splenic vascularity on Doppler and the reduction or absence of flow in the splenic vein and artery is an argument in favor of torsion [11].
Abdominal-pelvic CT is the imaging modality of choice, confirming the diagnosis of ectopic splenic torsion by showing an empty splenic compartment with an abdominal or abdominal-pelvic mass reminiscent of the hypodense appearance of the spleen and not taking contrast after intravenous injection [12,13].
The twisted pedicle can be seen on CT as a swirl sign representing the coils [13].
It confirms the diagnosis and allows treatment to be adapted. Indeed, in the absence of splenic necrosis, detorsion can be performed with splenoplexy to fix the spleen in its normal anatomical position. In case of splenic necrosis, splenectomy is indicated [14]. In our patient, a splenectomy was performed, due to the infarction of the spleen.
Once the diagnosis of this complication is made, surgical exploration is necessary. If the spleen is healthy with no splenic necrosis, treatment is conservative, detorsion can be performed with splenopexy to fix the spleen in its normal anatomical position. In case of irreversible complications such as splenomegaly, pseudocysts but especially splenic infarction as in our patient's case, splenectomy is indicated by conventional or laparoscopic approach [14].
Vaccinations against Hemophilus influenzae and pneumococcus should be considered in order to prevent fulminant infections due to encapsulated germs [14].
Conclusion
Wandering spleen syndrome is a rare condition in which congenital or acquired hyperlaxity of the splenic suspensory ligaments results in splenic migration into an unusual anatomical position. It is mostly described in children and young women. Early diagnosis is essential for conservative treatment in young patients. Torsion of the spleen pedicle is a serious complication that can lead to splenic infarction. Its diagnosis should be made in the presence of acute abdominal pain associated with a mobile abdominal mass. Imaging, particularly Doppler ultrasound and CT scans, can confirm the diagnosis. The radical treatment is splenectomy.
Patient consent
Written and informed consent for publication of the case was obtained from the patient.
Footnotes
Competing interests: The authors have declared that no competing interests exist.
References
- 1.Horwitz JR, Black CT. Traumatic rupture of a wandering spleen in a child: case report and literature review. J Trauma. 1996;41(2):348–350. doi: 10.1097/00005373-199608000-00027. [Abstract] [Google Scholar] [DOI] [PubMed] [Google Scholar]
- 2.Sodhi KS, Saggar K, Sood BP, Sandhu P. Torsion of a wandering spleen: acute abdominal présentation. J Emerg Med. 2003;25(2):133–137. doi: 10.1016/s0736-4679(03)00160-4. [DOI] [PubMed] [Google Scholar]
- 3.Kapan M, Gümüs M, Onder A, Gümüs H, Aldemir M. A wandering spleen presenting as an acute abdomen: case report. J Emerg Med. 2010 doi: 10.1016/j.jemermed.2010.06.029. Sep 18; [Abstract] [Google Scholar] [DOI] [PubMed] [Google Scholar]
- 4.Singh Sodhi K, Saggar K, Bimal PS, Sandhu P. Torsion of a wandering spleen: acute abdominal presentation. J Emerg Med. 2003;25(2):133–137. doi: 10.1016/s0736-4679(03)00160-4. [DOI] [PubMed] [Google Scholar]
- 5.ibault L, Vergos M, Ribault A. Deux cas de rate ectopique. Med Afr Noire. 1990;37:43–44. [Google Scholar]
- 6.Traori K, Sanyal R, Deshmukh A, Saini T. Pseudo cyst formation: a rare complication of wandering spleen. British J Radiol. 2005;78:1050–1052. doi: 10.1259/bjr/33073529. [DOI] [PubMed] [Google Scholar]
- 7.Armstrong CA, Clarke ED, Tsang TM, Stewart RT. The wandering spleen. Arch Dis Cild. 1996;74:247–248. doi: 10.1136/adc.74.3.247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Alawi MH, Khalifa A. Wandering spleen: a challenging diagnosis. Pak J Med Sci. 2005;21:482–484. [Google Scholar]
- 9.Navarro RDC, Gomez AT, Paz PS, et al. Wandering spleen causing acute abdomen. Case Rep Clin Pract Rev. 2003;4:173–175. [Google Scholar]
- 10.Sharon N, Schachter J, Talnir R, et al. Weird activity and the wandering spleen. IMAJ. 2005;7:744–745. [PubMed] [Google Scholar]
- 11.Befikadu S, Gudu W, Abseno N. Torsion of a pelvic wandering spleen as a cause of acute abdomen in a woman: a case report and review of the literature. Ethiop Med J. 2004;42(1):53–61. [PubMed] [Google Scholar]
- 12.Rasheed B, Ahmed F, Iqbal Z, Babar S, Ahmed N. Wandering spleen with tortion leading to infarction. Europ J Radiol Extra. 2011;77(1):5–7. [Google Scholar]
- 13.Puglisi F, Potenza A, Melchionda M, Capuano P, De Fazio M, Lobascio P, et al. Wandering spleen as a cause of acute abdomen: a case report. Chir Ital. 2005;57(3):373–375. [PubMed] [Google Scholar]
- 14.Misawa T, Yoshida K, Shiba H, Kobayashi S, Yanaga K. Wandering spleen with chronic torsion. Am J Surg. 2008;195(4):504–505. doi: 10.1016/j.amjsurg.2006.08.083. [DOI] [PubMed] [Google Scholar]