Abstract
Background:
Compared to whites, African-Americans have lower prevalence of ideal cardiovascular health (CVH) based on the American Heart Association Life’s Simple 7 (LS7). These CVH inequities have worsened during the COVID-19 pandemic. Ideal LS7 health-promoting behaviors and biological risk factors (e.g., diet, blood pressure) are associated with improved CVH outcomes. The FAITH! (Fostering African-American Improvement in Total Health) App, a community-informed, mobile health (mHealth) intervention, previously demonstrated significant improvements in LS7 components among African-Americans, suggesting mHealth interventions may be effective in improving CVH. This paper presents the FAITH! Trial design, baseline findings and pandemic-related lessons learned.
Methods:
Utilizing a community-based participatory research approach, this study assessed the feasibility/preliminary efficacy of a refined FAITH! App for promoting LS7 among African-Americans in faith communities using a cluster, randomized controlled trial. Participants received the FAITH! App (immediate intervention) or were assigned to a delayed intervention comparator group. Baseline data were collected via electronic surveys and health assessments. Primary outcomes are change in LS7 score from baseline to 6-months post-intervention and app engagement/usability.
Results:
Of 85 enrolled individuals, 76 completed baseline surveys/health assessments, for a participation rate of 89% (N=34 randomized to immediate intervention, N=42 to delayed intervention). At baseline, participants were predominantly female (54/76, 71%), employed (56/76, 78%) and of high cardiometabolic risk (72/76, 95% with hypertension and/or overweight/obesity) with mean LS7 scores in the poor range (6.8, SD=1.9).
Conclusions:
The FAITH! Trial recruitment was feasible, and its results may inform the use of mHealth tools to increase ideal CVH among African-Americans.
Introduction
Cardiovascular health (CVH) disparities in African-Americans (AAs) persist. Recent epidemiologic studies find that compared to whites, AAs have significantly fewer ideal CVH components that comprise the American Heart Association Life’s Simple 7 (AHA LS7).1–5 Data from the Jackson Heart Study, the largest observational cohort of AAs examining their cardiovascular disease (CVD) risk, showed that only 3.2% of AAs met ≥5 ideal levels of the LS7 components and none met ideal levels for all components.6 Established as the foundation of the AHA 2020 Strategic Impact Goal to improve CVH and CVD outcomes population-wide, the LS7 is an evidence-based metric of seven health-promoting behaviors and biological risk factors: physical activity (PA), diet, smoking, body mass index (BMI), blood pressure (BP), cholesterol, and glucose.7 Thus, strides towards improving CVH in AAs could lead to substantial reductions in CVD burden and premature death in this group. In recent years, numerous culturally tailored, community-based, health interventions have shown effectiveness in improving general health knowledge and health behaviors among AAs.8 These interventions have largely targeted single CV risk factors (e.g., PA, obesity) and have less potential to significantly reduce CVH disparities than those targeting multiple risk factors.9 Further, many of these interventions have been unsustainable and inadequately disseminated in AA communities.8,10–13 AAs face multi-level psychosocial and structural barriers or adverse social determinants of health (SDOH) including systemic racism, poor access to quality healthcare/health information and trusted providers, and financial/environmental constraints that limit their abilities to focus on their own CVH and wellness.14–16 Unfortunately, the COVID-19 pandemic undoubtedly unveiled and exacerbated many of these pre-existing negative SDOH and CVH inequities, which disproportionately impacted socioeconomically disadvantaged populations, particularly AAs.17–20 This additional heavy burden of pandemic-related obstacles and stressors may portend worse CVH and health outcomes of AAs.
Novel methods for overcoming barriers to ideal CVH in AAs are warranted. Even prior to the COVID-19 pandemic, mobile health (mHealth) technology swiftly gained recognition for its ability to deliver effective health information to under-resourced populations.21 According to contemporary observational data, AAs have identical patterns of mobile technology and smartphone-use as their white counterparts.22 Further, AAs are more likely to rely on smartphones as their primary Internet access source23 and express willingness to engage with these devices for mHealth research and lifestyle interventions.24–26 mHealth technologies, digital communication and devices are adaptable, engaging, cost-effective, scalable, and effective in improving CV risk factors (e.g., hypertension, diabetes).27–29 However, there are few effective, culturally relevant, evidence-based interventions for this population. No community-based mHealth lifestyle intervention has assessed the impact of risk-based prevention by targeting multiple CV risk factors among a high CVD risk, racial/ethnic minority group as recommended by the AHA.7,29,30 Our study fills this gap by enhancing our existing general CVH and wellness digital application to more effectively address the LS7 through a community-based participatory research (CBPR) approach.31,32 CBPR strategies have cultivated trust between researchers and underserved communities and increased enrollment/retention rates among AAs which has become especially important during the COVID-19 crisis.33,34 AA faith communities offer promising avenues to deliver mHealth interventions as technology integration into church health promotion activities may facilitate their implementation, dissemination, and sustainability.35,36
The FAITH! Trial
The FAITH! (Fostering African-American Improvement in Total Health) Trial builds upon over a decade of collaboration within a rich, dynamic CBPR academic-community partnership with AA churches in Rochester and Minneapolis-St. Paul (MSP), MN.37,38 To better address CVD health disparities within the AA community in MN, the academic-community partners and stakeholders (through the FAITH! Community Steering Committee-CSC) mutually formulated a mission to focus on CVH promotion through the LS7 framework and actionable, community-based interventions. In partnership with community members, we co-designed a general CVH and wellness digital application for AAs (FAITH! App) which had high acceptability and resulted in significant improvements in multiple LS7 components among our pilot study participants.39,40 Feedback from participants indicated a need for individually-tailored messaging and interpersonal features.41 Thus, we refined the FAITH! App and evaluated its feasibility and preliminary efficacy among AA adults within faith communities using a pilot randomized controlled trial (RCT). We hypothesize that our FAITH! App intervention will be feasible and improve CVH among AAs in faith communities from baseline to six-months post-intervention. Herein, we present the design and baseline findings of the FAITH! Trial and offer lessons learned on the recruitment process during the COVID-19 pandemic.
Methods/Design
Study design
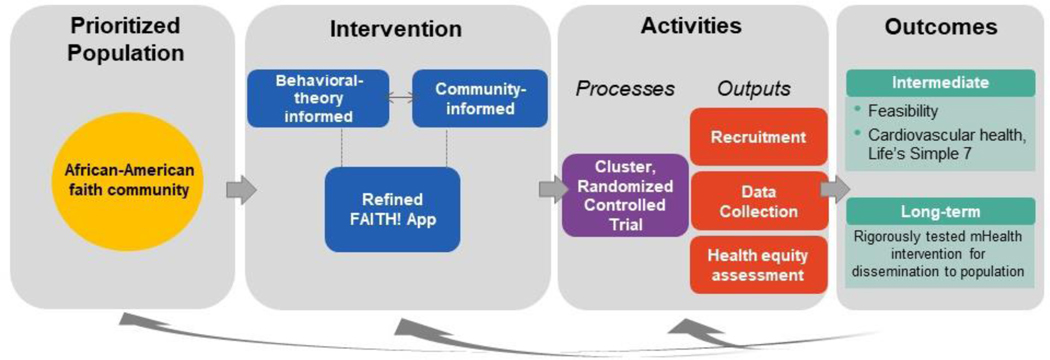
The overall study design is depicted in Figure 1 according to a modified CBPR conceptual logic model.42–44
Figure 1.
Study design by modified community-based participatory research conceptual logic model Adapted from Wallerstein et al, 200840 and Wallerstein and Duran, 201041
We employed a pilot cluster, RCT with delayed intervention control group which is consistent with the overarching CBPR process. The study was reviewed and approved by the Mayo Clinic Institutional Review Board and registered (clinicaltrials.gov NCT03777709). Written informed consent was obtained from all individuals prior to participation. This study was directly funded by the National Institutes of Health (NIH)/National Institute on Minority Health and Health Disparities (NIMHD) (Grant No. 1 R21 MD013490–01), the American Heart Association-Amos Medical Faculty Development Program (Grant No. 19AMFDP35040005), the Clinical and Translational Science Awards (CTSA) (Grant No. UL1 TR000135) from the National Center for Advancing Translational Sciences (NCATS) and the Mayo Clinic Center for Health Equity and Community Engagement in Research. The authors are solely responsible for the design and conduct of this study, all study analyses, the drafting and editing of the paper and its final contents.
Recruitment
Recruitment of participants occurred from May 2020 through October 2020. To enhance recruitment in this underserved and traditionally underrepresented population in research, the study leadership hired compassionate and culturally sensitive staff of diverse backgrounds and experiences. The study team also included members reflective of the prioritized study population (study principal investigator and community health workers of AA heritage). Further, all study staff completed diversity, equity and inclusion and CBPR training as a part of the hiring process.
Church screening and eligibility
We recruited churches in Rochester and MSP to participate primarily through existing contacts (FAITH! CSC members) and by city-wide congregational and business listings. Details of the church recruitment process will be discussed in a separate report. In brief, in-person church recruitment events were initially held at health centers in Rochester and MSP but as a result of the COVID-19 pandemic, a subsequent recruitment event was shifted to a virtual platform (Zoom) to prioritize safety and convenience. Each church was assessed for readiness to engage by adaptation of the PREACH (Predicting Readiness to Engage AA Churches in Health) model (i.e., infrastructure, prior health programming)45,46 by an electronic and follow-up telephone screening survey. Defined church inclusion criteria were the following: 1) predominantly AA parishioners, 2) commitment from church pastor/senior leadership to promote the study at church, and 3) willingness of church member to serve as church liaison (FAITH! Partner). Church pastors electronically signed a letter of mutual intent as a commitment to participate in the study and received a $250 incentive.
Participant screening and eligibility
Participants were recruited by telephone, email, and direct referral from the church-designated FAITH! Partners from the enrolled churches. The study team organized joint congregation community recruitment kickoff events which included a project overview and open discussion (transitioned from in-person to virtual due to the COVID-19 pandemic). To adapt to pandemic-related restrictions (e.g., social/physical distancing, church closures) and limited in-person events, a promotional video was developed to provide a study overview with most frequently asked questions from interested participants. To enhance our recruitment outreach during the pandemic, all hard-copy recruitment materials were distributed by multiple modalities including postal mail and electronically via email and social media platforms. Interested individuals completed an eligibility “Program Interest/Eligibility Form” and forwarded it to the study team by email. The study coordinator contacted interested individuals by telephone to reiterate study details and to complete confirmatory eligibility screening. Study inclusion criteria were: AA person, age ≥18 years, smartphone ownership (iOS or Android systems), basic Internet skills, at least weekly Internet access, active email address, fruit/vegetable intake <5 servings/day, <30 minutes of PA/day and able to engage in moderate-intensity PA. Exclusion criteria were: participation in app refinement focus group series, inability to walk up ≥2 flights of stairs or walk ≥1 city block without assistance or stopping, pregnant (due to associated hormonal and weight changes) or have plans to become pregnant in next 2 years or visual/hearing impairment or mental disability that would preclude independent app use. The eligibility criterion were developed to prioritize sedentary individuals with suboptimal dietary patterns given low prevalences of ideal levels of PA and diet LS7 components among AAs.6 These individuals may benefit most from a lifestyle intervention.47 Eligible participants completed electronic informed consent. Participants received $50 by Visa gift card at enrollment and collection of baseline data along with a personal PA monitor (Fitbit Versa 2). Participants will receive gift cards of the same value at the follow-up study time-points (immediate postintervention and 6-months post-intervention). As with recruitment outreach, follow-up with participants concerning key study timepoints/events were communicated by a variety of means (e.g., emailed timelines and reminders, telephone calls, etc.).
Randomization
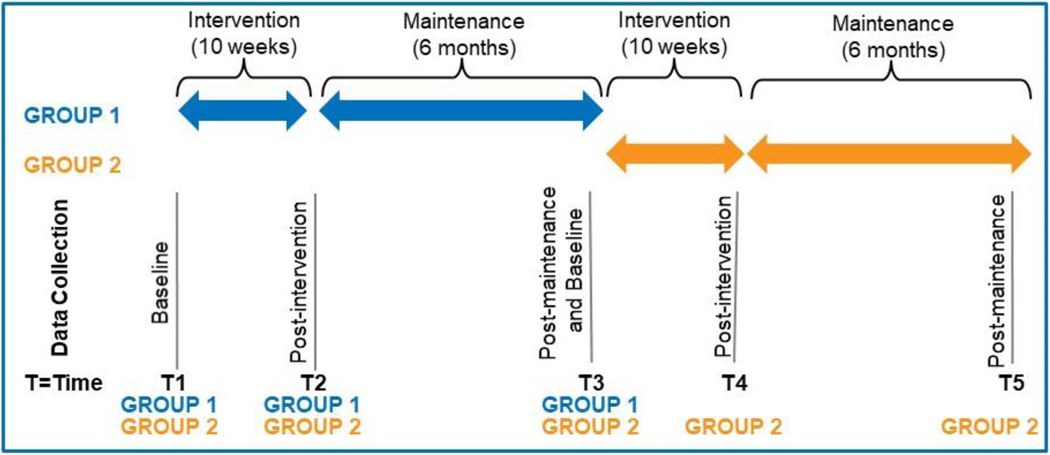
The cluster RCT design has 2 waves of implementation inclusive of 2 groups (See Figure 2): intervention (Group 1) and delayed intervention (Group 2, control group).
Figure 2.
Randomization scheme: Cluster randomized controlled trial with delayed intervention
Clusters of churches in Rochester and MSP are randomized to receive the intervention immediately following baseline health assessments including LS7 measures (Time 1, Group 1) or at post-maintenance (Time 3, Group 2). Groups 1 and 2 then complete post-intervention assessments by electronic survey of CVH behaviors, feasibility and psychosocial measures (Times 2 and 4). Both groups complete second health assessments at post-maintenance (Time 3), to allow for comparison of LS7 measures between Groups 1 and 2. Times 4 through 5 are data collection points following the intervention (post-intervention and post-maintenance) for Group 2. The study statistician randomized churches (balanced by church size), ensuring that the number of participants in Groups 1 and 2 were balanced. Churches were informed of their randomization assignment after baseline assessments.
Power analysis
The primary outcome is a comparison of average change in LS7 score from baseline (Time 1) to 6-months post-intervention (Time 3) between Groups 1 and 2. Initial power calculations were performed to estimate adequate sample size. A total of 16 churches averaging 10 participants/church (80 participants/group) was estimated to provide 85% power to detect a difference of 1.0 in average LS7 score change between groups (SD 2; 5% type-I error rate, assuming 0.01 intracluster correlation and 0.50 coefficient of variation of church sizes). The clinical significance of an at least 1-unit difference in LS7 score is based on a recent meta-analysis demonstrating that each unit increase in LS7 metrics is associated with an estimated 19% and 11% reduction in CVD and all-cause mortality, respectively.48 Based on these calculations, we initially aimed to recruit 200 participants to ensure 160 completers (assuming 20% attrition rate). However, due to recruitment challenges from the COVID-19 pandemic our recruitment goal was revised. The church goal remained at 16 churches, however a mean of five participants/church (40 participants/group) was estimated to provide 80% power to detect a difference of 1.45 in average LS7 score change between groups (effect size of 0.73, SD 2; 5% type-I error rate, assuming 0.01 intracluster correlation and 0.50 coefficient of variation). Assuming a 20% attrition rate, recruitment of at least 80 participants to ensure at least 60 completers would provide adequate power based on these adjusted calculations.
FAITH! App Intervention
Table 1 presents the content and theoretical basis of the refined FAITH! App evaluated in the RCT.
Table 1.
Content and theoretical basis of refined FAITH! App
| Feature | Description | Theoretical Framework |
|---|---|---|
| Dashboard (New) | User-specific display of baseline LS7 metrics, weekly stage of change selection (steps), tailored stage-based messaging, modules/tracking progress | Precaution Adoption Process Model |
| Social incentive (New) | Thermometer goal chart by church for tracked diet (fruit/vegetable intake) and physical activity (no. of steps, minutes) | Social Ecological Model |
| Education modules (Refined) | 10 modules with core video series on key LS7 components from health professionals, pre-post quizzes of cardiovascular health knowledge and relevant brochure content in each module integration of health disparities/equity, social determinants of health topics | Social Ecological Model |
| Self-monitoring (Refined) | Interactive tracking of fruit/vegetable intake and physical activity via a monthly calendar | Precaution Adoption Process Model |
| Sharing Board (Refined) | Moderated discussion platform and feed for participant interaction by posting healthy lifestyle practices and associated psychosocial factors through text, photographs and video | Social Ecological Model |
| Testimonials (Refined) | Church leadership and past FAITH! Program participant video accounts of their personal experiences with heart disease or healthy lifestyle change with motivational messaging | Social Ecological Model |
| Recipes | Cookbooks including heart-healthy traditional African-American cuisine | Social Ecological Model |
FAITH indicates Fostering African-American Improvement in Total Health; and LS7, Life’s Simple 7.
By integrating a theory-based approach, the FAITH! App was refined to provide users with personalized educational content and support to encourage ideal CVH behaviors. Individual participant LS7 and the Precaution Adoption Process Model (PAPM) were used as sound conceptual frameworks to promote behavior change based on stage-of-change according to a classification algorithm to deliver predetermined decision rule-based messages.49 For instance, individuals in early stages (1–2) received messages to increase their awareness and readiness to act (e.g., “Following 7 simple steps can improve your heart health and help you live longer”); whereas, those in advanced stages (5–6) received messages focused on performance capacity-building and positive reinforcement (e.g., “Reducing portion size and increasing PA will help you lose weight” or “Keep up the good work, you’ve eaten >5 fruit and vegetable servings today!”). Tailored messages unique to each individual’s PAPM stage were delivered via their app dashboard to inform and persuade toward consistent healthy behaviors (self-monitoring of diet and PA).12 The sharing board modifications included moderated weekly posts to foster discussion on self-efficacy, self-regulation, social support, and barriers/facilitators to healthy lifestyle with Social Ecological Model (SEM) concepts.15,50 Also, we aimed to capitalize on behavior economics by providing social incentives at the church level51–53 with a thermometer goal chart tracking diet/PA by church over the 1-year study. Top-ranked churches will be acknowledged during a post-study dissemination event.
We obtained stakeholder feedback on the refined app that will be described in a separate report. Briefly, 15 AA church congregants in Rochester and MSP were recruited for focus groups (5 per group) with a mean age (SD) of 56.9 (12.3) years; 87% were women. The focus group series was transitioned from an anticipated in-person formatting to a virtual platform (Zoom) due to the COVID-19 pandemic and unrest caused by the killing of Mr. George Floyd in Minneapolis, MN during the recruitment phase. By way of virtual communication of instructions (email, telephone, Zoom), participants downloaded the FAITH! App prototype to their personal smartphones. They were instructed to use the prototype and its core features for two weeks before the first focus group. App usability (impact, perceived usefulness, ease of use, user control) and user satisfaction (likes, dislikes, perceived cultural appropriateness) were assessed according to the Health Information Technology Usability Evaluation Model54 and Scale55,56 (Health-ITUEM/ITUES) which are systematic rubrics for evaluating mHealth apps. Key discussion points included solicited feedback on app prototype features, proposed revisions, LS7 incorporation category and integration of AA faith community cultural norms and values. Given the striking CVH disparities affecting the AA community as a whole, an emphasis was placed on tailoring to preferences of both men and women. Immediately following each focus group, a summary analysis of discussion highlights was compiled by the moderator. Synthesis of overarching themes and most salient participant feedback was completed using thematic analysis techniques57 to inform sequential intervention refinement of the app prototype components by the study team and software developers for review at subsequent focus groups.
The most commonly cited feedback from the majority of the participants (synonymous with weighting) was ultimately integrated into the refined app. Based on participant preferences, a balanced representation of men, women and families was incorporated into the app imagery, education module videos and past program participant testimonials. Additions or refinements were made to the app and the refined app proceeded to the RCT once the participant rating of the app readiness met a predetermined threshold (mean overall Health-ITUES55 score of ≥4, possible range 0 to 5). Overall user satisfaction with the refined app was high, and the app features exceeded the usability threshold goal to proceed to use in the RCT.
The app is individually tailored to promote LS7 through health education while enhancing self-efficacy, self-regulation, and social support for healthy behavior change. It includes a 10-week education modules series with a LS7 focus, interactive self-quizzes, self-monitoring of diet and PA (daily serving of fruits/vegetables and steps), and social networking (sharing board). Participants manually enter their servings of fruits/vegetables each day. The Fitbit automatically syncs daily step measurements with the app. Participants follow a weekly schedule by each LS7 component. Personalized messages guided by the theory-based models (PAPM, SEM) are delivered to each participant 3–4 times/week over the intervention phase via the app dashboard (and email per preferences). Messages are either informational, cues to action, reminders, or motivational/praise for healthy behavior change. The moderated sharing board is updated weekly with posts from reputable sources (e.g., AHA, Mayo Clinic) to foster discussion on behavior change influences and participant successes/challenges to healthy lifestyle.
Measures
Sociodemographics, relevant health history and psychosocial influences on CVH were collected by electronic surveys at baseline and will be collected at follow-up time points (immediate post-intervention and 6-months post-intervention). In-person health assessments of clinical, laboratory, and anthropometric data were performed at baseline (October to November 2020) and will occur at 6-months post-intervention at community venues by a mobile clinical research unit team of trained nursing staff. The study team implemented COVID-19 safety precautions at all health assessments such as staggering of appointments to minimize number of individuals present on-site for adequate social/physical distancing, universal mask wearing, and frequent sanitizing (hand and surface) by the study team and participants. Table 2 provides a summary of measures and the schedule of assessments.
Table 2.
Cluster, randomized controlled trial summary of measures and data collection schedule
| Data Collected | Baseline | Immediate post-intervention | 6-months post-intervention |
|---|---|---|---|
| Individual information | |||
| Demographics: Sex, age, race/ethnicity, contact information | X | ||
| Marital status | X | ||
| Education | X | ||
| Employment/Occupation status | X | ||
| Income | X | ||
| Insurance status | X | ||
| General health: medical history, health status, preventive care | X | ||
| Digital skills | |||
| Electronic health literacy: Electronic Health Literacy Scale | X | ||
| Mobile technology/Internet use skills | X | ||
| Cardiovascular health (Life’s Simple 7) measures | |||
| Blood pressure | X | X | |
| Fasting lipid panel | X | X | |
| Fasting glucose | X | X | |
| Height/weight (BMI) | X | X | |
| Cigarette smoking status | X | X | |
| Diet quality: Delta Nutrition Intervention Food Frequency Questionnaire | X | X | X |
| PA patterns: International PA Questionnaire | X | X | X |
| Feasibility measures | |||
| App engagement | X | X | |
| App usability: Health Information Technology Usability Evaluation Scale |
X | X | |
| Psychosocial measures | |||
| Diet/PA self-efficacy | X | X | X |
| Diet/PA self-regulation | X | X | X |
| Diet/PA social support | X | X | X |
| Religiosity/spirituality: Daily Spiritual Experience Scale | X | X | |
| Optimism: Life Orientation Test-Revised | X | X | |
| Perceived stress: Global Perceived Stress Scale | X | X | |
PA indicates physical activity.
Sociodemographic, health, digital skills information
At baseline, participants were queried on demographic information regarding age, socioeconomic status (education level, annual household income, insurance), marital status, self-reported general health status, and medical history (including antihypertensive, lipid lowering, and diabetes medication use). To explore digital skills, the electronic health literacy scale (eHEALS) was used to assess electronic health literacy (EHL)58 (an individual’s ability to seek, find, understand, and appraise health information from electronic sources and apply these skills toward health issues). Participants were also queried about their mobile technology/Internet use skills,59 sources of online health information, and social media use.
Primary outcomes
CVH measures (LS7 score)
CVH profiles according to LS7 were assessed by measurement of BP (average of three sitting readings), lipid panel and glucose60 (by fingerstick), height (to nearest centimeter by stadiometer), weight (with calibrated scale in kilograms), self-reported cigarette smoking status (former, current, never), dietary quality (healthy diet score according to AHA guidelines by a validated, culturally appropriate, food frequency questionnaire),61,62 and PA patterns (minutes/week of moderate and vigorous intensity PA).63 LS7 component criteria were adapted from AHA standards based on health assessment data (Supplemental Table I). A LS7 score was calculated as a composite of each LS7 component by assigning 2-points for ideal, 1-point for intermediate, or 0-points for poor.64 The total sum allows for a continuous measure of CVH ranging from poor to ideal (0–14 pts). For ease of translation and understanding, the LS7 score was categorized as 0–6 (poor), 7–8 (intermediate), and 9–14 (ideal) as previously conducted by our team.65
Intervention feasibility measures
We will assess feasibility by participant engagement with app features (goal ≥50% of participants accomplishing: initial connection and log-in to homepage/dashboard, ≥50% completion of education modules series, ≥1 entry/week of tracking for diet/PA). App usability will be assessed by the Health-ITUES (goal overall mean score ≥4).55,56
Secondary outcomes
We will ascertain the influence of several measures (using validated instruments) on LS7 score. Further, given our integrated conceptual model accounting for key SEM influences within the AA faith community to promote/hinder behavior change, we will assess multiple domains of sociocultural and environmental contexts as follows over the course of the study.
Healthy diet/regular PA self-efficacy
Participant self-efficacy or confidence to maintain healthy behaviors (healthy diet, regular PA) when faced with common barriers is assessed by validated instruments.66,67 Fruit/vegetable intake self-efficacy is assessed as how certain an individual can implement varying strategies to eat healthier foods focused on fruits/vegetables. Scores across five items are averaged to calculate a final score (ranging from 0 (certain I cannot) to 100 (certain I can)). Exercise confidence is assessed by a 12-item instrument on a 5-point scale (“I know I cannot” [1] to “I know I can” [5]), with subscales for “sticking to it” (8 items) and “making time for exercise” (4 items). Responses from each item are averaged to calculate a final score for each of the two subscales (range 1 to 5). Step count self-efficacy is measured by a 24-item instrument. Participants respond to items on a scale of 0 (certain I cannot) to 100 (certain I can) on how certain they are that they can build up their daily step-count, with the score calculated as the average of the items.
Self-regulation
Assessment of self-regulation for diet (14 items) and PA (10 items) was adapted from the Health Beliefs Survey which has demonstrated reliability and validity among AA church congregations.68,69 Participants are asked questions about strategies they have used in the past three months to eat healthier foods (three subscales: increase fruit/vegetable intake [3 items], decrease fat/calorie intake [6 items], plan and track nutrition [5 items]) or increase their daily step-count or PA. All items are measured on a 5-point scale (“never” [1] to “always” [5]). Scores across all items are averaged within each subscale to calculate a final score (range 1 to 5).
Social support
Social support for healthy diet (20 items) and PA (23 items) from family or friends are assessed using an adapted Sallis et al. scale utilized in our prior studies and in other AA church congregation samples.70–72 For social support for healthy diet, participants are asked how much encouragement or discouragement (5 items from family, 5 items from friends for each respectively) they receive to eat healthier. All items are measured on a 5-point scale (“never” [1] to “very often” [5]) and items are summed within each subscale with a possible score range of 5 to 25. Social support for PA assesses subscales of family participation [10 items], family rewards and punishment [3 items], and friend participation [10 items]). All items are measured on a 5-point scale (“never” [1] to “very often” [5]) and items are summed within each subscale with possible scores ranging from 10–50 for participation, and 3–15 for rewards/punishment. Higher scores imply greater encouragement or discouragement, participation, or rewards/punishment for all social support instruments.
Religiosity/spirituality
Religiosity is assessed as religious attendance using items selected and adapted from the Fetzer Multidimensional Measurement of Religiousness/Spirituality.73 Religious attendance (in-person) is assessed by a single-item asking how often participants attend (“go to”) religious services or meetings (scale 1= “more than once a week” to 5= “never”). Religious attendance (virtual/remote) is assessed by a single item – “How often do you watch or listen to religious programs on TV, radio or online?” – with six response options (1=“several times a day” to 6= “never”). Spirituality is measured by the short version of the Daily Spiritual Experience Scale (DSES) which assesses ordinary daily experiences according to theistic and non-theistic experiences of spirituality in six domains.74,75 The 15 items of the DSES are each rated using a 6-point Likert scale with 1 “never or almost never” to 6 “many times a day.” The DSES score is calculated as the mean of the 15 items, ranging from 1 to 6.
Optimism
The Life Orientation Test-Revised (LOT-R) is used to measure optimism.76 The LOT-R is a 6-item instrument rated on a 5-point scale from 1 (I disagree a lot) to 5 (I agree a lot).Participants respond to three positively worded items (e.g., “I’m always optimistic about my future”) and three negatively worded items (e.g., “If something can go wrong for me, it will”). The LOT-R score is calculated as the sum of the 6 items ranging from 6 (least optimistic) to 30 (most optimistic), after first reversing the negatively worded items.
Perceived stress
Perceived stress is measured using the Global Perceived Stress Scale which was validated in a population of AA adults with adaptation from standardized stress scales and within our study on stress and CVH in AAs.65,77–79 The 8-item instrument measures global perceptions of stressful experiences over the prior 12 months in domains such as employment, legal issues, and racism/discrimination. Participants rate the severity of each domain according to a range of “not stressful” (1) to “very stressful” (3) with a total sum ranging from 0 to 24.
Statistical methods
Descriptive statistics/unadjusted analyses
For the baseline data reported in this paper, descriptive statistics were summarized with frequencies/percentages and means/standard deviations comparing Group 1 and 2 participants. At subsequent study time-points, study measures will be summarized and compared between groups using χ2 tests for categorical variables and 2-sample t-tests for continuous variables. Differences between baseline and each follow-up will be calculated for continuous measures. These differences will be examined overall and within each group, with paired t-tests. The distribution of categorical outcomes (e.g., LS7 component category: poor, intermediate, ideal) will be compared between baseline and each follow-up with McNemar’s tests.
Regression models for adjusted analyses
Paired differences from baseline for LS7 score and other continuous outcomes (outlined above) will be compared between intervention and control groups after adjusting for a prioriselected baseline covariates using linear regression models with generalized estimating equations (GEE) to account for correlated data within church. Covariates include age, sex, education, income, insurance status, medical history, and medication use. Similarly, logistic regression models with GEE will be used to examine adjusted associations with the probability of intermediate/ideal levels of CVH at the second timepoint (using poor CVH as referent). Effect modification by sex will be explored. All analyses will be conducted using SAS, v9.4 (SAS Institute, Inc., Cary, NC). P values <0.05 will be considered statistically significant.
Process and health equity evaluation
In line with CBPR, we will evaluate the equitable processes within our overarching academic-community partnership to promote health equity. Using the synergistic framework for evaluating equity within CBPR partnerships, we will evaluate dimensions of partnership effectiveness in addressing health inequities using metrics outlined by Ward and colleagues.80
Dissemination of results
We have identified key audiences for dissemination of our study findings including the FAITH! CSC, all partnering AA churches and local AA community at-large (Rochester and MSP, MN), state and regional public health organizations (e.g., Departments of Health, local affiliate AHA) and the academic community (nationally and internationally). To ensure that the findings from our research informs community level health interventions to promote CVH and thereby maximize the benefit to underserved AA communities, our dissemination strategy has been co-developed by the academic-community partner team. For community members, we will hold community-wide events to provide the overall results in a clear and succinct manner with incorporation of slide and video presentations and culturally appropriate infographics. We will also share our findings through social media (e.g., Facebook, Twitter), lay press (newspapers, magazines), and radio/TV outlets for proactive dissemination of our study findings to our prioritized population. The academic-community partner team will jointly present executive summaries of the study findings to key influential governmental organizations and stakeholders to inform health policy, environmental and systems change in the Rochester and MSP areas. We will publish peer-reviewed articles in high impact academic journals and research summaries for professional journals all written and co-authored with community partners.
Results
Participants
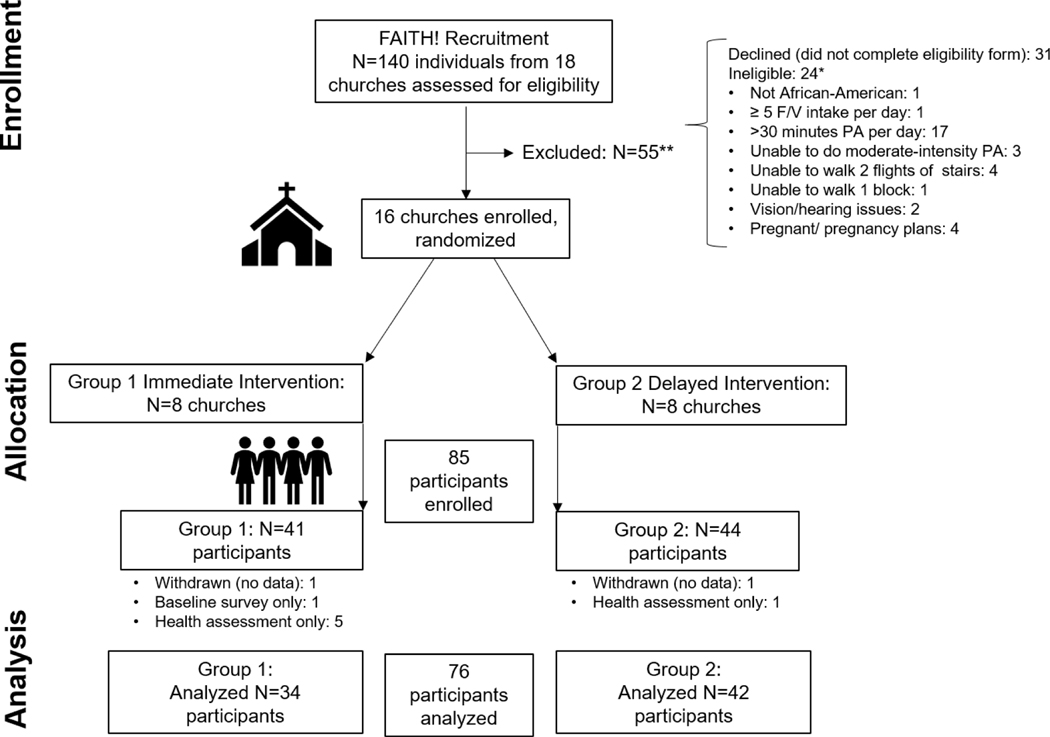
Among 18 churches, 140 individuals expressed interest in participating to the study team by attending a kickoff event or completing a program interest form. A total of 16 churches (N=4 Rochester, N=12 MSP) were enrolled in the RCT and randomized to Groups 1 and 2. After screening, 85 participants (60% of approached individuals) met study inclusion criteria, were enrolled and distributed amongst their respective enrolled church (N=41 in Group 1, N=44 in Group 2). The most common reasons for exclusion included: incomplete eligibility form (n=31) and >30 minutes PA/day (n=17). Of the 85 participants enrolled, 76 completed both the baseline health assessment and electronic survey (See Figure 3 for modified CONSORT flow diagram). Baseline characteristics of study participants included in the analysis are summarized in Table 3.
Figure 3.
Modified CONSORT flow diagram F/V indicates fruit/vegetable; PA, physical activity
Table 3.
Cluster, randomized controlled trial participant baseline characteristics*
| Overall Sample (N=76)† | |
|---|---|
|
| |
| Sex | |
| Male | 22 (28.9%) |
| Female | 54 (71.1%) |
| Age, Mean (SD) | 54.5 (12.3) |
| Range | (21.0–86.0) |
| Marital status | |
| Single | 20 (27.8%) |
| Divorced | 10 (13.9%) |
| Widowed | 1 (1.4%) |
| Married or committed relationship | 41 (56.9%) |
| Education level | |
| High school graduate or less | 8 (11.1%) |
| Some college | 23 (31.9%) |
| Technical or Associate degree | 13 (18.1%) |
| College graduate or higher | 28 (38.9%) |
| Employment status | |
| Employed, at least part-time | 56 (77.8%) |
| Unemployed | 6 (8.3%) |
| Retired | 10 (13.9%) |
| Household income category | |
| <$35,000 | 14 (18.4%) |
| $35,000-$49,999 | 14 (18.4%) |
| $50,000-$74,999 | 21 (27.6%) |
| ≥$75,000 | 15 (19.7%) |
| Not disclosed | 12 (15.8%) |
| Healthcare insurance | |
| Yes | 64 (88.9%) |
| No/Don’t know | 8 (11.1%) |
| Has health care professional, seen on regular basis | |
| Yes | 59 (77.6%) |
| No | 17 (22.4%) |
| Health conditions as communicated by a health care professional | |
| Overweight/Obesity | 54 (71.1%) |
| Hypertension | 47 (61.8%) |
| Type 2 Diabetes‡ | 20 (27.0%) |
| Hyperlipidemia | 32 (42.1%) |
| Current cigarette smoker § | 2 (2.7%) |
| Electronic health literacy score, Mean (SD)||| | 27.9 (6.0) |
| <26 | 18 (23.7%) |
| ≥26 | 58 (76.3%) |
| Mobile technology/Internet use skills, Mean (SD)# | 4.0 (1.1) |
N (%) shown unless otherwise specified.
Frequencies not adding to column total indicate missing data.
Denominator N=74.
Denominator N=75
Possible range 8 [low] to 40 [high].
Possible range 1 [low] to 5 [high].
The mean EHL score for all participants is 27.9 (SD 6) with 76.3% categorized at the high level (≥26). Mobile technology/Internet skills were rated at a mean of 4.0 (SD 1.1), in the relatively high range.
Primary outcome
The primary outcome, mean LS7 score and its associated individual components, are presented for the overall sample at baseline in Table 4.
Table 4.
Primary outcome measures: Life’s Simple 7 (LS7) score and individual components*
| Total (N=76)† | |
|---|---|
|
| |
| LS7 Score ‡ | |
| N | 71 |
| Mean (SD) | 6.8 (1.9) |
| Poor | 31 (43.7%) |
| Intermediate | 25 (35.2%) |
| Ideal | 15 (21.1%) |
| Physical Activity | |
| Poor | 20 (27.8%) |
| Intermediate | 36 (50.0%) |
| Ideal | 16 (22.2%) |
| Healthy Diet Score | |
| Poor | 47 (61.8%) |
| Intermediate | 28 (36.8%) |
| Ideal | 1 (1.3%) |
| Smoking | |
| Poor | 2 (2.7%) |
| Intermediate | 21 (28.0%) |
| Ideal | 52 (69.3%) |
| Body Mass Index | |
| Poor | 49 (64.5%) |
| Intermediate | 19 (25.0%) |
| Ideal | 8 (10.5%) |
| Blood Pressure | |
| Poor | 44 (57.9%) |
| Intermediate | 29 (38.2%) |
| Ideal | 3 (3.9%) |
| Cholesterol | |
| Poor | 11 (14.5%) |
| Intermediate | 35 (46.1%) |
| Ideal | 30 (39.5%) |
| Glucose | |
| Poor | 6 (7.9%) |
| Intermediate | 22 (28.9%) |
| Ideal | 48 (63.2%) |
N (%) shown unless otherwise specified.
Frequencies not adding to column total indicate missing data.
Sum of seven LS7 components, possible range 0–14.
Overall, the participants had poor CVH with a mean (SD) LS7 score of 6.8 (1.9; 43.7% of participants in poor category). The highest proportions of participants with LS7 components at the poor category level were for BMI (64.5%), diet (61.8%), and BP (57.9%). Smoking and glucose had the highest proportions of participants in the ideal category (69.3%, 63.2%, respectively).
Discussion
In this CBPR-guided study, we successfully recruited participants to both a focus group series and RCT to refine and rigorously test a CVH and wellness app for AAs. Our strenuous and community-focused recruitment process allowed us to meet our recruitment goals. The refinement of the FAITH! App through an iterative approach resulted in the intervention receiving favorable usability and satisfaction ratings and yielded a fully functional, culturally relevant app ready for testing in the RCT. Enrolled participants in the RCT were predominantly women (reflective of the demographics of the AA church)81 and demonstrated overall poor CVH, thus overall high cardiometabolic risk at baseline. This confirms the rationale for this study which is supported by: 1) the preponderance of evidence demonstrating CVH disparities within racial/ethnic minority groups, particularly among AA men and women1–5,82 2) extensive epidemiologic evidence showing graded benefits of ideal CVH in lowering lifetime risk of CVD and mortality, 3) recent guidelines from the American College of Cardiology/AHA,14,83 recommending a focus on the SDOH in community level interventions to promote CVH, and 4) robust observational data showing high EHL in AAs and their willingness to participate in mHealth research.24–26
The cluster RCT with delayed intervention design differs in several ways from the previous pilot study conducted by our study team. Firstly, the design was informed by the positive results on the LS7 within our prioritized population in our preliminary work40 and the encouragement of our study participants and community partners to expand the intervention to more area churches. The church eligibility criteria are more rigorous to allow for assessment of key factors influencing church enrollment into clinical trials and academic community partnerships, which will be reported elsewhere. The intervention has been reinvigorated with integration of new behavioral theoretical frameworks (e.g., PAPM, SEM) and features to facilitate healthy lifestyle change while simultaneously focusing on the SDOH. Further, our study design is now multi-faceted with inclusion of both qualitative and quantitative aims as well as an innovative, randomized intervention with two study arms (immediate and delayed intervention) to allow all partnering churches to receive the intervention.
There were several lessons learned that are primarily related to participant recruitment during the COVID-19 pandemic. Given the plethora of competing demands and hardships faced by our study population as a result of the pandemic, our team faced significant recruitment challenges. Although the recruitment goal for number of participants was modified to a more practical goal, we remained focused on continuing the study to maintain accountability to our prioritized population and their community-identified health need—a key CBPR tenet.31 Further, we not only had to be diligent in following up with potential participants about the goals of the study through multiple means (telephone, email, social media), but we also had to demonstrate empathy regarding the impact of the public health crisis. As such, we also launched a FAITH! CSC-led, COVID-19 church emergency preparedness initiative in over 100 area AA churches to provide churches with accurate and reliable information on COVID-19, community-based resources, and wellness topics.84 This not only strengthened our trust and credibility with this community but also demonstrated that our primary goal with the CBPR partnership was to improve the overall health of the community, not just meeting recruitment goals. This tactic undoubtedly contributed to us meeting our recruitment goals. Further, due to limitations on community-facing events, we were forced to transition many of our anticipated face-to-face recruitment events (church recruitment, kick-off, launch session) to virtual delivery (via Zoom). Surprisingly, these virtual sessions were well-attended and were deemed a time-efficient, highsatisfaction, and convenient means to review the study components. This new paradigm of virtually “meeting people where they are” complemented our planned digitally-administered intervention through the FAITH! App. The FAITH! Trial employed a CBPR approach that centered the priorities of community partners in the development and implementation of the study which likely engendered community partner buy-in and consequently, participant enrollment in the trial. Further research should continue to explore the role of CBPR in increasing the enrollment of racial/ethnic minorities in clinical trials.
Conclusions
The data generated from this pilot RCT will provide rich information regarding the impact of an mHealth lifestyle intervention to promote CVH among AAs as well as unique sociocultural contextual factors that might influence their CVH. Furthermore, the FAITH! Trial can serve as a framework for other clinical investigators to bridge health promotion and research methods using community-based interventions and increase participation in health-related research in AAs, a population disproportionately underrepresented in clinical studies.
Supplementary Material
Acknowledgments
We would also like to show appreciation to all past and current FAITH! Community Steering Committee members for their unwavering support. Their input has enhanced the impact of the FAITH! Program as a whole by virtue of remaining steadfast in our mutual goal to achieve cardiovascular health equity in Minnesota and beyond through community outreach and interventions.
Sources of Funding
The research reported herein was supported by the National Institutes of Health (NIH)/National Institute on Minority Health and Health Disparities (NIMHD) (Grant No. 1 R21 MD013490–01), the Clinical and Translational Science Awards (CTSA) (Grant No. UL1 TR000135) from the National Center for Advancing Translational Sciences (NCATS) to Mayo Clinic and the Mayo Clinic Center for Health Equity and Community Engagement in Research. Dr. Brewer was supported by the American Heart Association-Amos Medical Faculty Development Program (Grant No. 19AMFDP35040005), NCATS (CTSA Grant No. KL2TR002379) and the Centers for Disease Control and Prevention (CDC, Grant No. CDC-DP181817) during the implementation of this work. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of NCATS, NIH or CDC. The funding bodies had no role in study design; in the collection, analysis, and interpretation of data; writing of the manuscript; and in the decision to submit the manuscript for publication.
Role of the Funder/Sponsor
The analysis was designed and performed by the authors independent from the funders. The authors are solely responsible for the design and conduct of this study, analyses, interpretation of data, the drafting and editing of the report and its final contents. The corresponding and senior authors had direct access to all the data analyzed and reported in this study and had final responsibility for the decision to submit for publication.
Abbreviations
- AA
African-American
- AHA
American Heart Association
- CBPR
community-based participatory research
- CSC
Community Steering Committee
- CV
cardiovascular
- CVH
cardiovascular health
- CVD
cardiovascular disease
- DSES
Daily Spiritual Experience Scale
- eHEALS
Electronic Health Literacy Scale
- EHL
electronic health literacy
- FAITH
Fostering African-American Improvement in Total Health
- Health-ITUEM
Health Information Technology Usability Evaluation Model
- Health-ITUES
Health Information Technology Usability Evaluation Scale
- LOT-R
Life Orientation Test-Revised
- LS7
Life’s Simple 7
- mHealth
mobile health
- MSP
Minneapolis-St. Paul
- PA
physical activity
- PAMP
Precaution Adoption Process Model
- SEM
Social Ecological Model
- SDOH
social determinants of health
Footnotes
Registration: ClinicalTrials.gov Identifier: NCT03777709
Supplemental Materials
Table I. American Heart Association Life’s Simple 7: Definition of Poor, Intermediate, and Ideal Cardiovascular Health for Each Component/Metric
Declarations of interest
None
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Tabb LP, Ortiz A, Judd S, Cushman M, McClure LA. Exploring the Spatial Patterning in Racial Differences in Cardiovascular Health Between Blacks and Whites Across the United States: The REGARDS Study. J Am Heart Assoc. 2020;9(9):e016556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Carnethon MR, Pu J, Howard G, et al. Cardiovascular Health in African Americans: A Scientific Statement From the American Heart Association. Circulation. 2017;136(21):e393–e423. [DOI] [PubMed] [Google Scholar]
- 3.Diaz CL, Shah NS, Lloyd-Jones DM, Khan SS. State of the Nation’s Cardiovascular Health and Targeting Health Equity in the United States: A Narrative Review. JAMA Cardiol. 2021;6(8):963970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shay CM, Ning H, Allen NB, et al. Status of cardiovascular health in US adults: prevalence estimates from the National Health and Nutrition Examination Surveys (NHANES) 2003–2008. Circulation. 2012;125(1):45–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bambs C, Kip KE, Dinga A, Mulukutla SR, Aiyer AN, Reis SE. Low prevalence of “ideal cardiovascular health” in a community-based population: the heart strategies concentrating on risk evaluation (Heart SCORE) study. Circulation. 2011;123(8):850–857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Djousse L, Petrone AB, Blackshear C, et al. Prevalence and changes over time of ideal cardiovascular health metrics among African-Americans: the Jackson Heart Study. Prev Med. 2015;74:111–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lloyd-Jones DM, Hong Y, Labarthe D, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s strategic Impact Goal through 2020 and beyond. Circulation. 2010;121(4):586–613. [DOI] [PubMed] [Google Scholar]
- 8.Elgazzar R, Nolan TS, Joseph JJ, Aboagye-Mensah EB, Azap RA, Gray DM, 2nd. Communityengaged and community-based participatory research to promote American Heart Association Life’s Simple 7 among African American adults: A systematic review. PLoS One. 2020;15(9):e0238374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lu Y, Ezzati M, Rimm EB, Hajifathalian K, Ueda P, Danaei G. Sick Populations and Sick Subpopulations: Reducing Disparities in Cardiovascular Disease Between Blacks and Whites in the United States. Circulation. 2016;134(6):472–485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Campbell MK, Hudson MA, Resnicow K, Blakeney N, Paxton A, Baskin M. Church-based health promotion interventions: evidence and lessons learned. Annu Rev Public Health. 2007;28:213234. [DOI] [PubMed] [Google Scholar]
- 11.Yanek LR, Becker DM, Moy TF, Gittelsohn J, Koffman DM. Project Joy: faith based cardiovascular health promotion for African American women. Public Health Rep. 2001;116 Suppl 1:68–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lemacks J, Wells BA, Ilich JZ, Ralston PA. Interventions for improving nutrition and physical activity behaviors in adult African American populations: a systematic review, January 2000 through December 2011. Prev Chronic Dis. 2013;10:E99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Whitt-Glover MC, Keith NR, Ceaser TG, Virgil K, Ledford L, Hasson RE. A systematic review of physical activity interventions among African American adults: evidence from 2009 to 2013. Obes Rev. 2014;15 Suppl 4:125–145. [DOI] [PubMed] [Google Scholar]
- 14.Havranek EP, Mujahid MS, Barr DA, et al. Social Determinants of Risk and Outcomes for Cardiovascular Disease: A Scientific Statement From the American Heart Association. Circulation. 2015;132(9):873–898. [DOI] [PubMed] [Google Scholar]
- 15.Coughlin SS, Smith SA. Community-Based Participatory Research to Promote Healthy Diet and Nutrition and Prevent and Control Obesity Among African-Americans: a Literature Review. J Racial Ethn Health Disparities. 2017;4(2):259–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brewer LC, Cooper LA. Race, discrimination, and cardiovascular disease. Virtual Mentor. 2014;16(6):455–460. [PMC free article] [PubMed] [Google Scholar]
- 17.Williams DR, Cooper LA. COVID-19 and Health Equity-A New Kind of “Herd Immunity”. JAMA. 2020;323(24):2478–2480. [DOI] [PubMed] [Google Scholar]
- 18.Yancy CW. COVID-19 and African Americans. JAMA. 2020;323(19):1891–1892. [DOI] [PubMed] [Google Scholar]
- 19.Vasquez Reyes M. The Disproportional Impact of COVID-19 on African Americans. Health Hum Rights. 2020;22(2):299–307. [PMC free article] [PubMed] [Google Scholar]
- 20.Tai DBG, Shah A, Doubeni CA, Sia IG, Wieland ML. The Disproportionate Impact of COVID-19 on Racial and Ethnic Minorities in the United States. Clin Infect Dis. 2021;72(4):703–706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Turner-Lee N SB, Miller J. Minorities, mobile broadband and the management of chronic diseases. In. Joint Center for Political and Economic Studies. Washington, DC2012. [Google Scholar]
- 22.Pew Research Center, 2021. Mobile Fact Sheet. Retrieved from: https://www.pewinternet.org/fact-sheet/mobile/. Accessed on January 4, 2022.
- 23.Ray R, Sewell AA, Gilbert KL, Roberts JD. Missed Opportunity? Leveraging Mobile Technology to Reduce Racial Health Disparities. J Health Polit Policy Law. 2017;42(5):901–924. [DOI] [PubMed] [Google Scholar]
- 24.James DC, Harville C 2nd, Whitehead N, Stellefson M, Dodani S, Sears C. Willingness of African American Women to Participate in e-Health/m-Health Research. Telemed J E Health. 2016;22(3):191–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.James DC, Harville C 2nd, Sears C, Efunbumi O, Bondoc I. Participation of African Americans in e-Health and m-Health Studies: A Systematic Review. Telemedicine journal and e-health : the official journal of the American Telemedicine Association. 2016. [DOI] [PubMed] [Google Scholar]
- 26.James DC, Harville C 2nd., eHealth Literacy, Online Help-Seeking Behavior, and Willingness to Participate in mHealth Chronic Disease Research Among African Americans, Florida, 2014–2015. Preventing chronic disease. 2016;13:E156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Afshin A, Babalola D, McLean M, et al. Information Technology and Lifestyle: A Systematic Evaluation of Internet and Mobile Interventions for Improving Diet, Physical Activity, Obesity, Tobacco, and Alcohol Use. J Am Heart Assoc. 2016;5(9). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ganesan AN, Louise J, Horsfall M, et al. International Mobile-Health Intervention on Physical Activity, Sitting, and Weight: The Stepathlon Cardiovascular Health Study. J Am Coll Cardiol. 2016;67(21):2453–2463. [DOI] [PubMed] [Google Scholar]
- 29.Burke LE, Ma J, Azar KM, et al. Current Science on Consumer Use of Mobile Health for Cardiovascular Disease Prevention: A Scientific Statement From the American Heart Association. Circulation. 2015;132(12):1157–1213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pearson TA, Palaniappan LP, Artinian NT, et al. American Heart Association Guide for Improving Cardiovascular Health at the Community Level, 2013 update: a scientific statement for public health practitioners, healthcare providers, and health policy makers. Circulation. 2013;127(16):1730–1753. [DOI] [PubMed] [Google Scholar]
- 31.Israel BA, Eng E., Schulz AJ, Parker EA Methods in community-based participatory research for health. 1 ed. San Francisco: Jossey-Bass; 2005. [Google Scholar]
- 32.Smith SA, Whitehead MS, Sheats JQ, Ansa BE, Coughlin SS, Blumenthal DS. Community-based participatory research principles for the African American community. J Ga Public Health Assoc. 2015;5(1):52–56. [PMC free article] [PubMed] [Google Scholar]
- 33.Wieland ML, Njeru JW, Alahdab F, Doubeni CA, Sia IG. Community-Engaged Approaches for Minority Recruitment Into Clinical Research: A Scoping Review of the Literature. Mayo Clin Proc. 2021;96(3):733–743. [DOI] [PubMed] [Google Scholar]
- 34.Wieland ML, Doubeni CA, Sia IG. Community Engagement With Vulnerable Populations. Mayo Clin Proc. 2020;95(9S):S60–S62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Brewer LC, Fortuna KL, Jones C, et al. Back to the Future: Achieving Health Equity Through Health Informatics and Digital Health. JMIR Mhealth Uhealth. 2020;8(1):e14512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Brewer LC, Jenkins S, Lackore K, et al. mHealth Intervention Promoting Cardiovascular Health Among African-Americans: Recruitment and Baseline Characteristics of a Pilot Study. JMIR Res Protoc. 2018;7(1):e31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Manjunath C, Ifelayo O, Jones C, et al. Addressing Cardiovascular Health Disparities in Minnesota: Establishment of a Community Steering Committee by FAITH! (Fostering African-American Improvement in Total Health). Int J Environ Res Public Health. 2019;16(21). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Brewer LC, Morrison EJ, Balls-Berry JE, et al. Preventing cardiovascular disease: Participant perspectives of the FAITH! Program. J Health Psychol. 2019;24(12):1710–1723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Brewer LC, Hayes SN, Caron AR, et al. Promoting cardiovascular health and wellness among African-Americans: Community participatory approach to design an innovative mobile-health intervention. PLoS One. 2019;14(8):e0218724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Brewer LC, Hayes SN, Jenkins SM, et al. Improving Cardiovascular Health Among African-Americans Through Mobile Health: the FAITH! App Pilot Study. J Gen Intern Med. 2019;34(8):1376–1378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Brewer LC, Kumbamu A, Smith C, et al. A Cardiovascular Health and Wellness Mobile Health Intervention Among Church-Going African Americans: Formative Evaluation of the FAITH! App. JMIR Form Res. 2020;4(11):e21450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wallerstein N OJ, Duran B, Tafoya G, Belone L, Rae R. CBPR: What predicts outcomes? In: Minkler M, Wallerstein N , editors. Community-based participatory research for health. 2nd ed. San Francisco, CA: Jossey Bass; 2008. [Google Scholar]
- 43.Wallerstein N, Duran B. Community-based participatory research contributions to intervention research: the intersection of science and practice to improve health equity. Am J Public Health. 2010;100 Suppl 1:S40–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Belone L, Lucero JE, Duran B, et al. Community-Based Participatory Research Conceptual Model: Community Partner Consultation and Face Validity. Qual Health Res. 2016;26(1):117–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Brand DJ, Alston RJ. The Brand’s PREACH Survey: A Capacity Assessment Tool for Predicting Readiness to Engage African American Churches in Health. J Relig Health. 2018;57(4):1246–1255. [DOI] [PubMed] [Google Scholar]
- 46.Brand DJ, Alston RJ. The Brand’s PREACH Model: Predicting Readiness to Engage African American Churches in Health. Health Promot Pract. 2017;18(5):763–771. [DOI] [PubMed] [Google Scholar]
- 47.Caperchione CM, Duncan MJ, Rosenkranz RR, et al. Recruitment, screening, and baseline participant characteristics in the WALK 2.0 study: A randomized controlled trial using web 2.0 applications to promote physical activity. Contemp Clin Trials Commun. 2016;2:25–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Aneni EC, Crippa A, Osondu CU, et al. Estimates of Mortality Benefit From Ideal Cardiovascular Health Metrics: A Dose Response Meta-Analysis. J Am Heart Assoc. 2017;6(12). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Weinstein ND. The precaution adoption process. Health Psychol. 1988;7(4):355–386. [DOI] [PubMed] [Google Scholar]
- 50.McKenzie JF, Neiger BL, Thackeray R. Planning, Implementing, and Evaluating Health Promotion Programs : a Primer. . 7 ed. Boston: Pearson; 2017. [Google Scholar]
- 51.Asch DA, Rosin R. Engineering Social Incentives for Health. N Engl J Med. 2016;375(26):25112513. [DOI] [PubMed] [Google Scholar]
- 52.Rogers T, Milkman KL, Volpp KG. Commitment devices to improve unhealthy behaviors--reply. JAMA. 2014;312(15):1592–1593. [DOI] [PubMed] [Google Scholar]
- 53.Patel MS, Benjamin EJ, Volpp KG, et al. Effect of a Game-Based Intervention Designed to Enhance Social Incentives to Increase Physical Activity Among Families: The BE FIT Randomized Clinical Trial. JAMA Intern Med. 2017;177(11):1586–1593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Brown W 3rd, Yen PY, Rojas M, Schnall R. Assessment of the Health IT Usability Evaluation Model (Health-ITUEM) for evaluating mobile health (mHealth) technology. J Biomed Inform. 2013;46(6):1080–1087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Schnall R, Cho H, Liu J. Health Information Technology Usability Evaluation Scale (Health-ITUES) for Usability Assessment of Mobile Health Technology: Validation Study. JMIR Mhealth Uhealth. 2018;6(1):e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Yen PY, Wantland D, Bakken S. Development of a Customizable Health IT Usability Evaluation Scale. AMIA Annu Symp Proc. 2010;2010:917–921. [PMC free article] [PubMed] [Google Scholar]
- 57.Bradley EH, Curry LA, Devers KJ. Qualitative data analysis for health services research: developing taxonomy, themes, and theory. Health services research. 2007;42(4):1758–1772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Norman CD, Skinner HA. eHealth Literacy: Essential Skills for Consumer Health in a Networked World. J Med Internet Res. 2006;8(2):e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Van Deursen AJ, Helsper EJ, Eynon R. Measuring Digital Skills. From Digital Skills to Tangible Outcomes project report (2014). http://www.lse.ac.uk/media@lse/research/DiSTO/Pdf/Measuring-Digital-Skills.pdf. Accessed December 19, 2017.
- 60.American Diabetes A. 2. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes-2020. Diabetes Care. 2020;43(Suppl 1):S14–S31. [DOI] [PubMed] [Google Scholar]
- 61.Carithers TC, Talegawkar SA, Rowser ML, et al. Validity and calibration of food frequency questionnaires used with African-American adults in the Jackson Heart Study. J Am Diet Assoc. 2009;109(7):1184–1193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Carithers T, Dubbert PM, Crook E, et al. Dietary assessment in African Americans: methods used in the Jackson Heart Study. Ethn Dis. 2005;15(4 Suppl 6):S6–49-55. [PubMed] [Google Scholar]
- 63.Kim Y, Park I, Kang M. Convergent validity of the international physical activity questionnaire (IPAQ): meta-analysis. Public Health Nutr. 2013;16(3):440–452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Thacker EL, Gillett SR, Wadley VG, et al. The American Heart Association Life’s Simple 7 and incident cognitive impairment: The REasons for Geographic And Racial Differences in Stroke (REGARDS) study. J Am Heart Assoc. 2014;3(3):e000635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Brewer LC, Redmond N, Slusser JP, et al. Stress and Achievement of Cardiovascular Health Metrics: The American Heart Association Life’s Simple 7 in Blacks of the Jackson Heart Study. J Am Heart Assoc. 2018;7(11). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Norman GJ, Carlson JA, Sallis JF, Wagner N, Calfas KJ, Patrick K. Reliability and validity of brief psychosocial measures related to dietary behaviors. Int J Behav Nutr Phys Act. 2010;7:56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Carlson JA, Sallis JF, Wagner N, et al. Brief physical activity-related psychosocial measures: reliability and construct validity. J Phys Act Health. 2012;9(8):1178–1186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Anderson ES, Wojcik JR, Winett RA, Williams DM. Social-cognitive determinants of physical activity: the influence of social support, self-efficacy, outcome expectations, and self-regulation among participants in a church-based health promotion study. Health Psychol. 2006;25(4):510520. [DOI] [PubMed] [Google Scholar]
- 69.Anderson ES, Winett RA, Wojcik JR, Williams DM. Social cognitive mediators of change in a group randomized nutrition and physical activity intervention: social support, self-efficacy, outcome expectations and self-regulation in the guide-to-health trial. J Health Psychol. 2010;15(1):21–32. [DOI] [PubMed] [Google Scholar]
- 70.Sallis JF, Grossman RM, Pinski RB, Patterson TL, Nader PR. The development of scales to measure social support for diet and exercise behaviors. Prev Med. 1987;16(6):825–836. [DOI] [PubMed] [Google Scholar]
- 71.Brewer LC, Balls-Berry JE, Dean P, Lackore K, Jenkins S, Hayes SN. Fostering African-American Improvement in Total Health (FAITH!): An Application of the American Heart Association’s Life’s Simple 7 among Midwestern African-Americans. J Racial Ethn Health Disparities. 2017;4(2):269281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Wilcox S, Laken M, Parrott AW, et al. The faith, activity, and nutrition (FAN) program: design of a participatory research intervention to increase physical activity and improve dietary habits in African American churches. Contemp Clin Trials. 2010;31(4):323–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Multidimensional Measurement of Religiousness/Spirituality for Use in Health Research. Kalamazoo (MI): Fetzer Institute and National Institute on Aging; 1999. [Google Scholar]
- 74.Underwood LG, Teresi JA. The daily spiritual experience scale: development, theoretical description, reliability, exploratory factor analysis, and preliminary construct validity using health-related data. Ann Behav Med. 2002;24(1):22–33. [DOI] [PubMed] [Google Scholar]
- 75.Loustalot F, Wyatt SB, Sims M, Ellison CG, Taylor HA, Underwood L. Psychometric testing of the daily spiritual experiences scale among African Americans in the Jackson Heart Study. J Relig Health. 2011;50(3):675–685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Hernandez R, Kershaw KN, Siddique J, et al. Optimism and Cardiovascular Health: Multi-Ethnic Study of Atherosclerosis (MESA). Health Behav Policy Rev. 2015;2(1):62–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Payne TJ, Wyatt SB, Mosley TH, et al. Sociocultural methods in the Jackson Heart Study: conceptual and descriptive overview. Ethn Dis. 2005;15(4 Suppl 6):S6–38-48. [PubMed] [Google Scholar]
- 78.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–396. [PubMed] [Google Scholar]
- 79.LePore SJ. Measurement of chronic stressors. In: Cohen S, Kessler RC, Gordon LU, ed. Measuring Stress: A Guide for Health and Social Scientists. New York: Oxford University Press:102–120. [Google Scholar]
- 80.Ward M, Schulz AJ, Israel BA, Rice K, Martenies SE, Markarian E. A conceptual framework for evaluating health equity promotion within community-based participatory research partnerships. Eval Program Plann. 2018;70:25–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Pew Research Center, 2009. A Religious Portrait of African-Americans. Retrieved from:https://www.pewforum.org/2009/01/30/a-religious-portrait-of-african-americans/. Accessed December 31, 2021.
- 82.Azap RA, Nolan TS, Gray DM, et al. Association of Socioeconomic Status With Ideal Cardiovascular Health in Black Men. Journal of the American Heart Association. 2021;10(23):e020184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;140(11):e596–e646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Brewer LC, Asiedu GB, Jones C, et al. Emergency Preparedness and Risk Communication Among African American Churches: Leveraging a Community-Based Participatory Research Partnership COVID-19 Initiative. Prev Chronic Dis. 2020;17:E158. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.