Figure 1: Consort Diagram of Randomization of GDM Screening Methods and Analytical Comparison Groups.
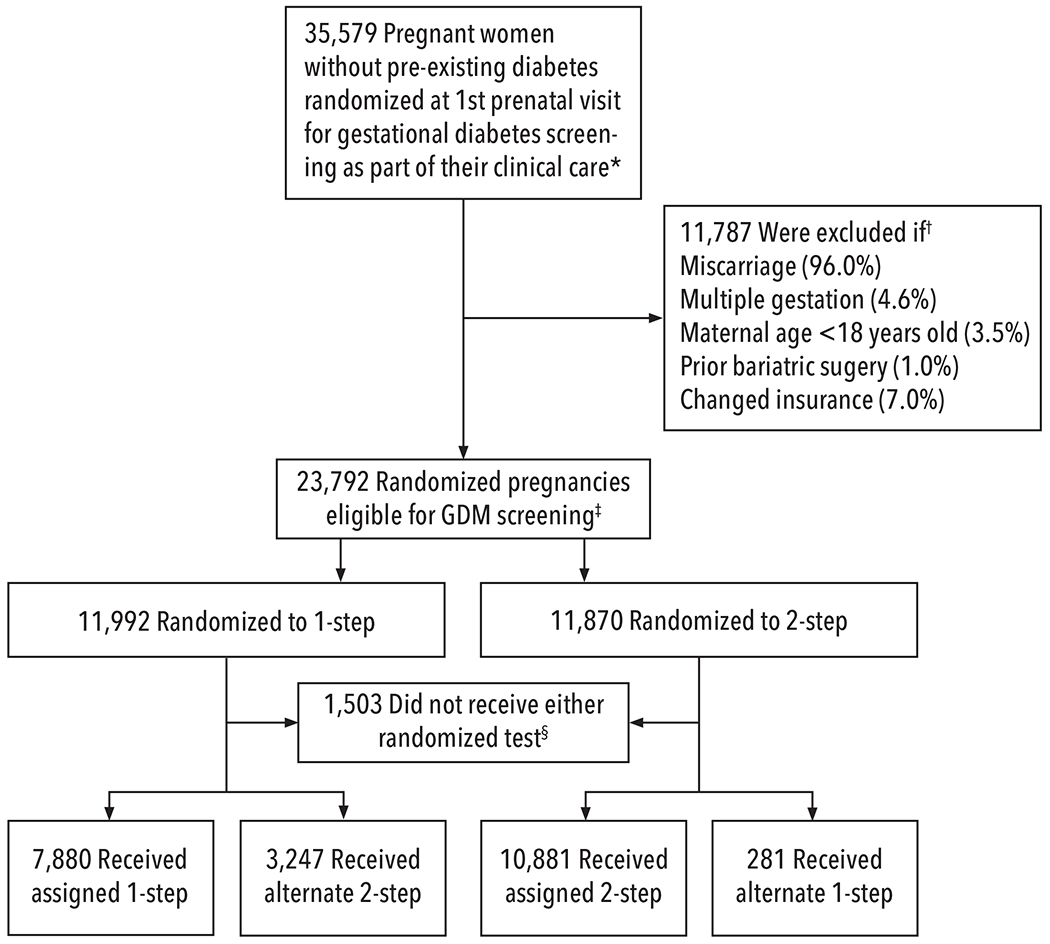
☆All pregnancies were randomized to 1-step or 2-step GDM screening strategies within the EMR as part of clinical care at their first prenatal visit. The 1 step (75g 2 hour OGTT) approach diagnosed GDM based on IADPSG criteria,9 and the 2-step screening approach by Carpenter and Coustan criteria.1
†Percentages do not add up to 100% as some pregnancies met multiple exclusion criteria. The major reason for exclusion was miscarriage (as randomization occurred at the 1st prenatal visit, in many cases this visit also determined non-viability, or miscarriage, on the same day of randomization and before any GDM screening was ordered); terminations were also included in this exclusion category. Change of insurance during pregnancy was an exclusion as we were unable to evaluate outcomes in these pregnancies.
‡Intention-to-treat analyses (ITT) were planned. Due to unanticipated lower adherence to the fasting 1-step at both sites, we continued randomizing until we enrolled enough pregnancies with 1-step screening to have adequate statistical power, and conducted additional analyses - inverse probability (IP) weighted ITT - both with and without adjustment for factors related to non-adherence.13,19,20 Factors related to lower adherence included both maternal and provider characteristics as well as provider reliance on non-fasting tests to ensure that GDM screening was completed at a visit.13 These pragmatic barriers to adherence could not be adequately addressed without putting patients at risk of not receiving GDM screening.
§Among the 1,503 pregnancies that did not receive either 1-step or 2-step screening, 1,450 (6.1%) were unscreened (778 [6.5%] randomized to 1-step and 672 (5.7%) randomized to 2-step), and these pregnancies presented on average at a mean of 18.9 weeks’ gestation compared to 10.5 weeks for pregnancies with screening. There were also 53 pregnancies that had other clinically recommended screening in the first trimester (HbA1c or FPG)9 but did not have either randomized GDM screening approach.
