The aim of this study was to describe the relation between sociodemographic factors, chronic health conditions, fear of coronavirus disease 2019 (COVID-19), COVID-19 stressors, and the perception of risk from COVID-19 and their influence on the use of health protective behaviors among a sample of Arkansans during the COVID-19 pandemic. Although studies of health protective behaviors have been done at the national level, none looked specifically at rural southern states, which may differ from a national perspective. Gaining insight into how these factors influence the adoption of health-protective behaviors can help inform targeted health messaging and interventions for future public health emergencies.
Supplemental digital content is available in the text.
Key Words: COVID-19, fear, protective behaviors, sociodemographic factors
Abstract
Objectives
This study describes the relationship between sociodemographic factors, chronic conditions, coronavirus disease 2019 (COVID-19) fears and stressors, and the perception of risk from COVID-19 and the use of health protective behaviors among Arkansans during the COVID-19 pandemic.
Methods
Data collected from an online survey, administered in Arkansas between July and August 2020 (n = 1205), were used to estimate regressions. The data analysis was completed in April 2021.
Results
Wearing a face mask was the most commonly reported behavior (97.4%), followed by handwashing (97.2%). Protective behaviors increased with higher levels of fear (β = 0.030, P < 0.001), more stressors (β = 0.057, P = 0.002), and age (β = 0.006, P = 0.030). Female (β = 0.510, P < 0.001) and Black (β = 0.268, P = 0.039) respondents reported engaging in more protective behaviors than males or other races/ethnicities.
Conclusions
In future pandemic planning, there will be a need to create messaging and interventions to increase health protective behaviors directed at young adults, men, and those with lower education levels. Providers will need to address fears related to COVID-19 and help their patients to manage those fears and anxieties.
Key Points
Wearing a face mask was the most commonly reported behavior, followed by handwashing.
Protective behaviors increased with higher levels of fear, more stressors, and age.
Female respondents engaged in more protective behaviors than males, and Black respondents engaged in more protective behaviors than other races/ethnicities.
Future pandemic planning will need to create messaging and interventions to increase health protective behaviors directed at young adults, men, and those with lower education levels.
In early 2020, the first cases of coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 were diagnosed in the United States.1 In March 2020, the federal government and states began to implement mitigation efforts, including recommendations for individuals to engage in health protective behaviors to prevent COVID-19. Several protective behaviors have been recommended, including handwashing/hand sanitizing, social distancing, avoiding crowded public spaces, and wearing face masks.2
Several studies have shown these protective behaviors to be effective in slowing the spread of COVID-19.3–6 Although face mask usage increased between April 2020 (78%) and June 2020 (89%), there was no substantial change in handwashing, social distancing, and avoiding public or crowded places during the same period.7 Research conducted in the United States and Europe has shown that engagement in health protective behaviors varies by socioeconomic characteristics, with the lowest engagement of protective behaviors among younger adults (aged 18–29 years), those with lower levels of education, and boys/men.7–10 Conversely, reports of health protective behaviors are highest among older adults, those with higher incomes, and those who report higher levels of fear of COVID-19.7,11–13 Race/ethnicity also seems to play a role in the adoption of health protective behaviors. For example, Whites were less likely to report wearing a face mask than Blacks, Hispanics, or Asians.9,14 The potential effects of COVID-19 infection for people with chronic illness, including severe COVID-19, intensive care unit admission, and mortality, may increase awareness regarding their potential susceptibility to infection and lead to higher overall engagement in health protective behaviors.15 Prior research, however, has indicated that increases in stress related to COVID-19 may lead to maladaptive coping strategies (eg, denial, behavioral disengagement) and lower engagement in health protective behaviors.16
The aim of this study was to describe the relationship between sociodemographic factors, chronic health conditions, fear of COVID-19, COVID-19 stressors, and the perception of risk from COVID-19 and their influence on the use of health protective behaviors among a sample of Arkansans during the COVID-19 pandemic. Although studies of health protective behaviors have been conducted at the national level, none looked specifically at rural southern states, which may differ from a national perspective. Gaining insight into how these factors influence the adoption of health protective behaviors can help inform targeted health messaging and interventions for future public health emergencies.17
Methods
Design, Recruitment, and Study Sample
A cross-sectional survey design was used to gather information from adults (18 years of age or older) living, working, or receiving health care in Arkansas on their attitudes, knowledge, and behaviors related to COVID-19. The study protocol was approved by the University of Arkansas for Medical Sciences Institutional Review Board.
Potential respondents (N = 4431) were recruited from a volunteer research participant registry, ARresearch.org, established by the University of Arkansas for Medical Sciences. Individuals voluntarily register with ARresearch.org to be contacted about research opportunities. The registered participants are representative of the racial and ethnic makeup of Arkansas. A total of 4077 recruitment e-mails were sent to potential respondents with valid e-mail addresses. The e-mails provided a study description and the opportunity to consent for participation and complete the online survey. Free and informed consent of all of the subjects was obtained. Before providing consent, respondents verified meeting the inclusion criteria of the study.
To eliminate duplicate survey submissions, screening questions requested the first and last name, date of birth, and e-mail address of potential respondents (data were deidentified prior to the analysis). Of the 4077 e-mails, 1288 (31.5%) individuals responded and elected to participate. Eleven responses were identified as duplicates; in the case of a duplicate response, the first response was selected to remain in the sample while the second response was excluded. There were 72 respondents who were ineligible because of missing age (n = 37); being younger than age 18 years (n = 15); not living, working, or receiving healthcare in Arkansas (n = 4); or not completing the survey past the eligibility questions (n = 16). The 72 respondents deemed ineligible were excluded from all of the analyses. The final analytic sample included 1205 respondents.
Instrument and Data Collection Procedures
The survey was developed by the study team using validated questions drawn from existing instruments and survey queston databases including the Behavior Risk Factor Surveillance Survey and PhenX Toolkit.18,19 Using a link provided in the survey recruitment e-mails, respondents completed the online survey via REDCap, a Web-based application for survey administration. Survey responses were collected during the months of July 2020 and August 2020, and the data analysis was completed in April 2021. A $20 gift card was sent to respondents who completed the survey as remuneration.
Measures
Outcome Variables
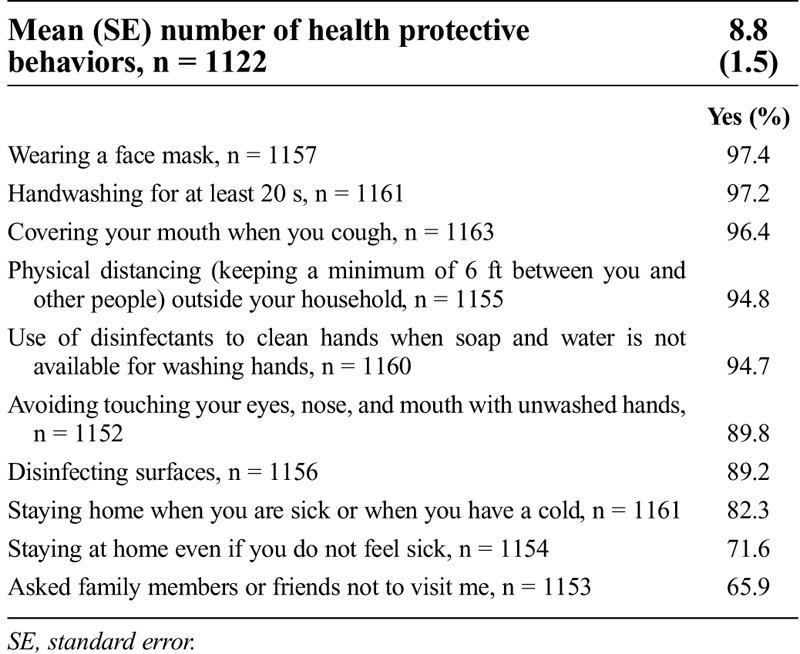
To assess health protective behaviors, respondents were asked whether they had engaged in 10 commonly suggested behaviors to prevent COVID-19 (Table 1). Health protective behavior summative scores (number of “yes” responses) were calculated, with possible scores ranging from 0 to 10.
Table 1.
Percentage of affirmative responses relating to health-protective behaviors during the past month
Sociodemographic Factors
Information was collected on respondents’ age, sex, race/ethnicity, highest level of education, income, and chronic conditions. Age (in years) was included as a continuous variable; age was also included as a categorical measure for descriptive purposes only. Sex was a dichotomous variable of male and female, and racial/ethnic background was a categorical variable of White, Black, Hispanic, and any other racial/ethnic category (because of the low number of responses in the American Indian/Alaska Native, Native Hawaiian/Pacific Islander, and Asian categories). Education was a categorical variable of high school diploma or less, some college or technical school, and a college degree or more. Income was also a categorical variable of < $25,000, $25,000 to < $50,000, $50,000 to < $75,000, and ≥ $75,000.
Chronic Health Conditions, COVID-19 Fear, Stressors, and Perceptions of Risk
Chronic conditions are calculated as a count of physical and mental health conditions (eg, diabetes mellitus, heart disease, cancer, depression), with a possible range of 0 to 15. The COVID-19 Fear Scale includes questions asking about the level of concern over issues related to the COVID-19 pandemic, including concerns about finances, being infected or infecting others, and concerns regarding the overall economy and returning to normalcy postpandemic (α = 0.86).19 The COVID-19 Fear Scale scores range from 0 to 42, with higher scores indicating a higher level of fear. The COVID-19 Stress Scale includes COVID-19 stressors, including stress surrounding the health and financial effects and access to medical supplies for one’s self, a child, or others (α = 0.76). The Stress Scale scores range from 0 to 13, with higher scores indicating a higher level of stress related to COVID-19. The Perceived Susceptibility to COVID-19 Scale includes questions and statements such as, “What do you think your chances are of getting COVID-19?”, “What do you think your chances are of dying from COVID-19?”, “I know how to protect myself from COVID-19”, and “For me, avoiding an infection with COVID-19 in the current situation is…?” (α = 0.52).19 The perceived susceptibility scores have a range of 0 to 8, with higher scores indicating a higher perceived susceptibility to COVID-19.
Analytical Strategy
The descriptive statistics report means and standard deviations (SDs) for continuous variables and the frequency and percentages for categorical variables. To evaluate sociodemographic differences in health protective behaviors during the COVID-19 pandemic, we entered each socioeconomic predictor variable into a separate regression model. In the final model, multivariable regression with full-information maximum likelihood estimation was used to determine the association between the included variables and the number of protective behaviors engaged in during the COVID-19 pandemic. Full-information maximum likelihood was used to account for missing data, and sensitivity tests using multiple imputation with chained equations were performed with similar results (see Supplemental Digital Content Tables, http://links.lww.com/SMJ/A269). Analysis was completed using STATA version 16 (StataCorp, College Station, TX), and a P ≤ 0.05 was considered statistically significant.
Results
Demographics
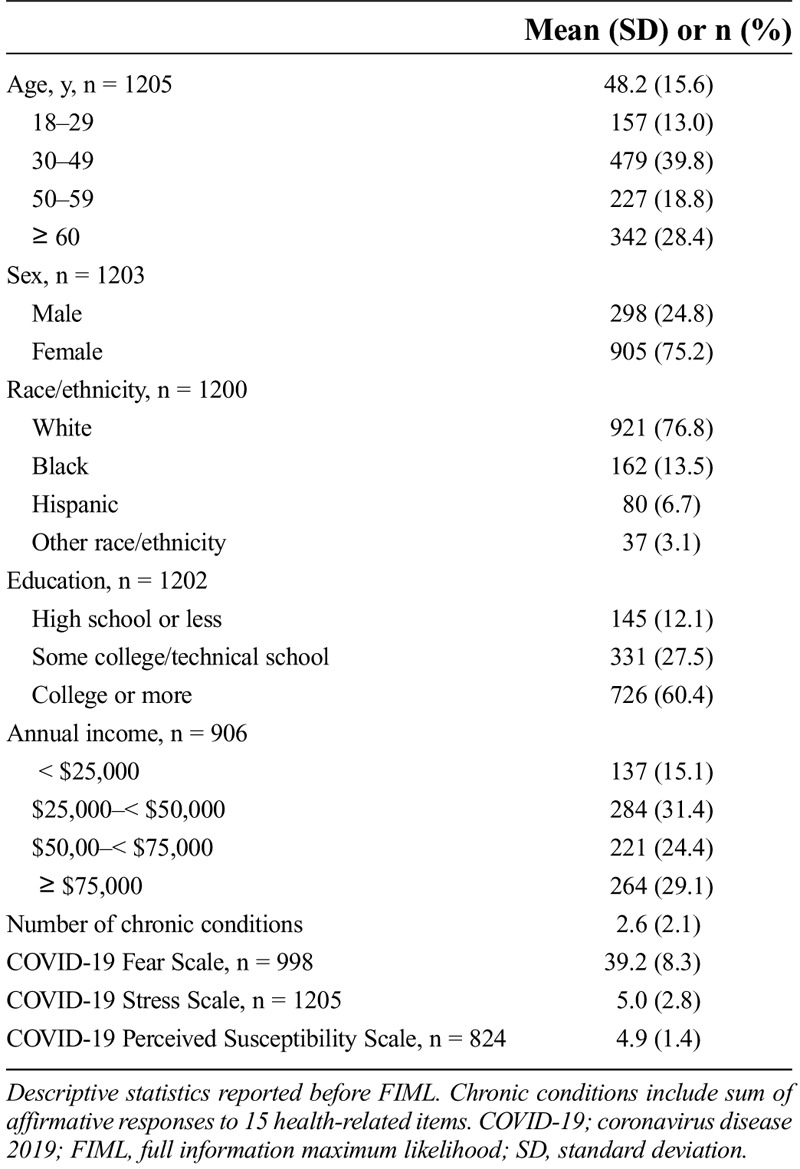
Characteristics of the respondents are presented in Table 2. The majority of the respondents were White and female and reported high levels of income and education. The mean number of chronic conditions reported by the respondents were 2.6 (SD ±2.1) conditions. Respondents had a mean score of 39.2 (SD ±8.3) on the COVID-19 Fear Scale, a mean score of 5.0 (SD ±2.8) on the COVID-19 Stress Scale, and a mean score of 4.9 (SD = 1.4) on the Perceived Susceptibility to COVID-19 Scale.
Table 2.
Demographic characteristics of respondents
Health Protective Behaviors
Table 1 reports the percentage of respondents who answered affirmatively to engaging in each health protective behavior during the COVID-19 pandemic. The majority of respondents reported engaging in each of the protective behaviors. The use of face masks was the most commonly reported protective behavior (97.4%), followed by handwashing for at least 20 seconds (97.2%). Only 65.9% of respondents reported that they would ask friends or family not to visit during the COVID-19 pandemic, and 71.6% of respondents reported they would stay home even if they were not feeling sick. The mean number of protective behaviors engaged in was 8.8 (standard error 1.5).
Sociodemographic Predictors of Health Protective Behaviors
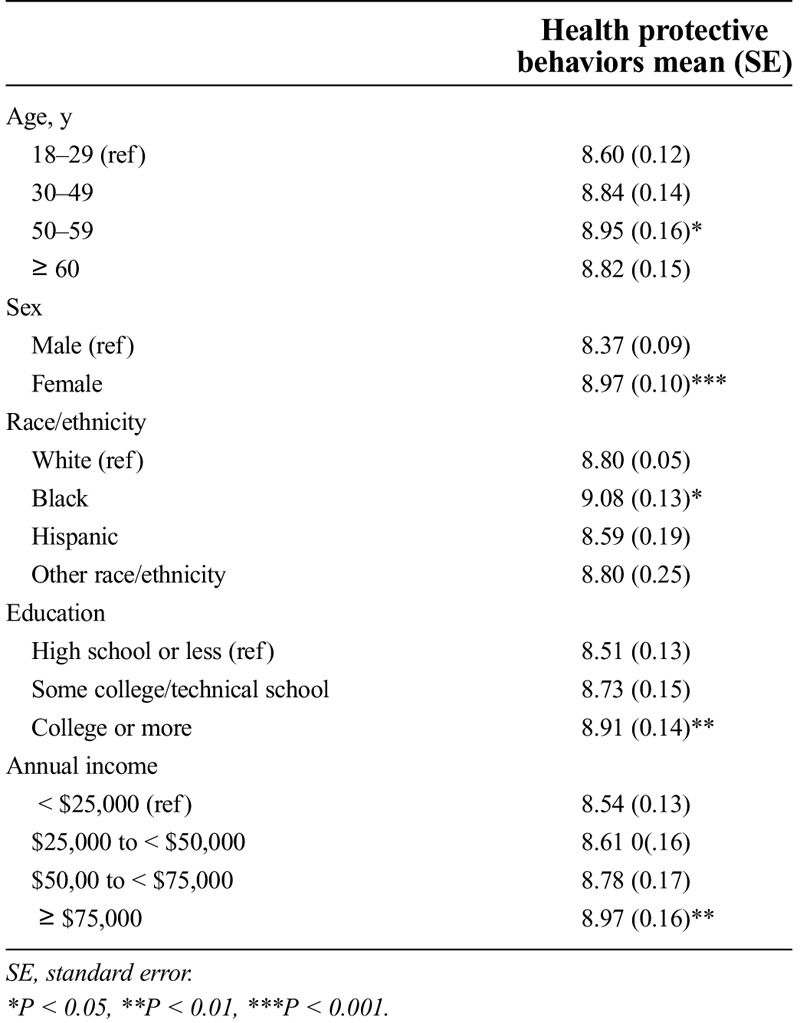
Demographic differences in the mean number of health protective behaviors engaged in were noted for age, sex, race/ethnicity, education, and annual income (Table 3). Respondents between the ages of 50 and 59 reported engaging in more health protective behaviors (mean 8.95, P = 0.03) than those in the youngest age category (18–29 years). Women engaged in more health protective behaviors (mean 8.97, P < 0.001) than men, and Black respondents engaged in more health protective behaviors (mean 9.08, P = 0.03) than other racial and ethnic groups. Respondents with a college degree or more (mean 8.91, P = 0.005) and those with annual incomes > $75,000/year (mean 8.97, P = 0.008) engaged in more health protective behaviors than those with lower levels of education or lower annual incomes.
Table 3.
Sociodemographic differences in the mean (SE) number of health-protective behaviors: results of bivariate regressions (n = 1205)
Association between COVID-19 Fears, COVID-19 Stress, and Health Protective Behaviors
The results of the multivariate regression model indicate that an increase in the level of COVID-19 fear increases the number of reported health protective behaviors (β = 0.030, P < 0.001) (Table 4). Increases in COVID-19 stressors also increased engagement in health protective behaviors (β = 0.057, P = 0.002). Neither the perceived susceptibility to COVID-19 infection (β = 0.030, P = 0.456) nor the number of chronic conditions reported (β = –0.011, P = 0.663) influenced engagement in health protective behaviors.
Table 4.
Summary of multivariable regression analysis using full maximum likelihood for variables predicting number of protective behaviors engaged in (n = 1205)
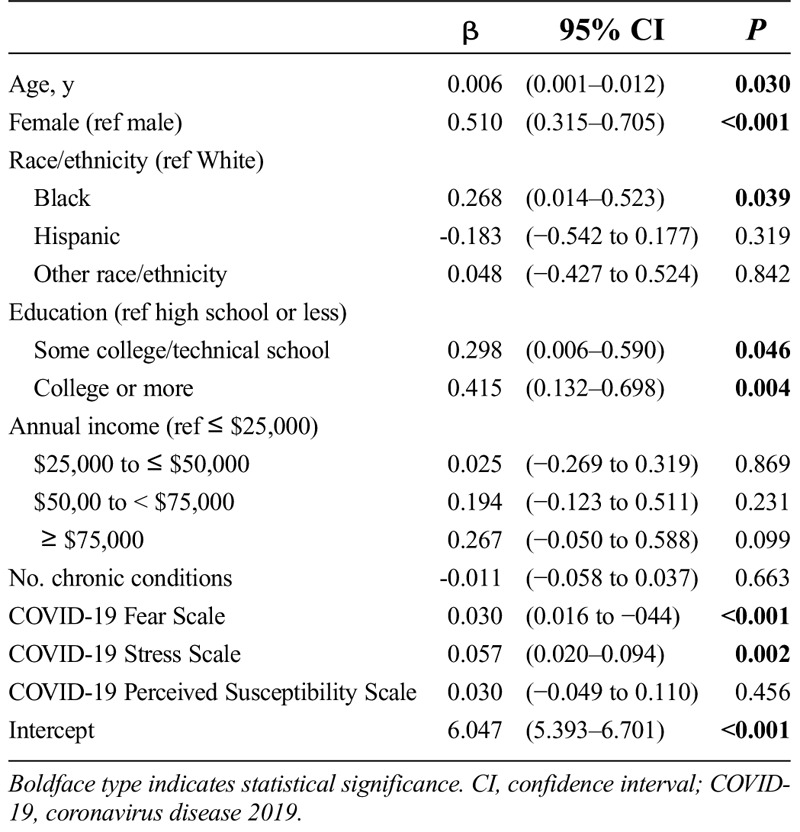
Consistent with the results of the bivariate regression models, the number of protective behaviors increased with age (β = 0.006, P = 0.030). Females (β = 0.510, P < 0.001) and Black respondents (β = 0.268, P = 0.039) reported engaging in more health protective behaviors than males or respondents of any other race/ethnicity, respectively. Respondents with at least some college or technical school (β = 0.298, P = 0.046) or a college degree or more (β = 0.415, P = 0.004) reported higher engagement in health protective behaviors than those with a high school education or less. Income level was not significant in the final model.
Discussion
The aim of our study was to examine the relationship between sociodemographic factors, chronic health conditions, fear of COVID-19, COVID-19 stressors, the perception of risk from COVID-19, and engagement in health protective behaviors among a sample of Arkansans during the COVID-19 pandemic. Overall, the majority of respondents reported engaging in high levels of health protective behaviors, including handwashing, use of hand sanitizers, wearing a face mask, and social distancing. The number of respondents reporting face mask use (97.4%) is higher than in previous nationally representative studies, in which 89% of respondents reported wearing face masks in June 2020.7 This is likely because of the face mask mandate put into place by Arkansas Governor Asa Hutchinson via executive order on July 20, immediately before distribution of the survey.20
Fewer Arkansans reported staying home when not sick or asking family and friends not to visit compared with other protective behaviors. Given that the severe acute respiratory syndrome coronavirus 2, the virus that causes COVID-19, is transmissible even in presymptomatic and asymptomatic cases,21 the lower rates of staying home when not sick and asking family and friends not to visit is concerning and was likely a contributing factor to prior surges of COVID-19 in Arkansas.22 Although the survey did not ask where individuals were spending their time, staying home and limiting in-person contact as much as possible were recommended to avoid infection and curb the spread of COVID-19. Social isolation, such as staying home alone for long periods, however, is difficult for underresourced communities, including those with lower levels of education. For example, our results indicate that increased education is associated with engaging in an increased number of protective health behaviors. People with lower levels of education may be more likely to work in jobs in which they are unable to work from home. Furthermore, individuals with higher levels of education have greater access to resources and may have had more opportunity to understand and engage with specific recommended behaviors, such as working from home.23 Work in northwest Arkansas has shown the effectiveness of support services providing assistance with basic needs to allow people to isolate or quarantine in reducing the level of infection in an underresourced community.24 Providing support services for underresourced communities, including provision of essential items such as food and medications, coordination with worksites, and coordination with community social and behavioral health services should be considered a vital part of future pandemic response plans.24,25
The number of health protective behaviors engaged in were higher for older adults, particularly for those in the 50- to 59-year-old age group, which is consistent with prior research.7 Lower levels of engagement in health protective behaviors among younger adults (18–29 years) may help to explain the increases in COVID-19 cases in this age group.7 The increases in cases among young adults often were followed by increases in cases among older at-risk populations.7 In addition, engagement in health protective behaviors was higher among female and Black individuals.9,14 Prior research has shown sex and racial/ethnic background can influence engagement in health protective behaviors, and these results support those findings.8,9,14,26 Despite increased engagement with health protective behaviors, Black and other minority populations had a higher prevalence of COVID-19.27 The disparities in infection rates are likely the result of existing inequalities, which lead to minority populations living in denser neighborhoods in multigenerational housing and having a higher likelihood of working in essential job categories.28 In planning for future responses to public health emergencies, officials will need to prioritize the development of clear and targeted messaging and behavior modification tactics, especially for younger adults, White individuals, and men to encourage engagement with health protective behaviors.
Prior research has indicated that fear and stress may be normal and functional responses to a public health emergency such as the COVID-19 pandemic,11 and our results indicate an increase in fear and the number of stressors experienced is associated with an increase in engagement with health protective behaviors.29 Providing clear and easy-to-follow guidance for protecting one’s self from COVID-19 may function as a method of coping with fear and stress, allowing individuals to satisfy their need to act even in situations in which so much is not within their control.30 It is important that healthcare providers and mental health professionals parse out differences in functional fear, which can serve a protective role, and pathological levels of negative emotions and behaviors.11,30 In addition, framing protective health behaviors beyond an avoidance framework (ie, to avoid getting sick) and situating these behaviors as normal, everyday actions may help attenuate the anxiety–health behavior relationship.
Increased engagement in health protective behaviors was not associated with an increase in the number of chronic conditions reported. People with chronic conditions, including diabetes mellitus and hypertension, are susceptible to severe COVID-19 disease, which has been elaborated on through numerous mediums (eg, television, print media) throughout the pandemic.31 Although increased engagement in health protective behaviors is beneficial for people with chronic conditions and should be expected, heightened awareness of the dangers of COVID-19 also may increase anxiety and fear, leading to maladaptive behaviors (eg, denial, behavioral disengagement) that ultimately are not protective.16,30 Future work will need to consider the complex interplay between physical and mental health and the role they play in the response of an individual to the COVID-19 pandemic. Healthcare professionals will need to be aware of the needs of their patients with chronic conditions and provide support and guidance to their patients in dealing with threats such as COVID-19.
This study is not without limitations. The sampling frame was limited to those who had registered with ARresearch and, therefore, may not be generalizable to populations outside Arkansas; however, the results may provide insight into the health protective behaviors adopted by individuals who are similar to the study sample. In addition, all of the measures used were self-reported and, therefore, carry the risk of social desirability bias. This limitation is reduced through the use of validated questions, and prior work demonstrated the limited effects of self-report even for sensitive questions (eg, substance use).32 Scales and measures related to COVID-19 have continuously evolved, and given when this survey was designed, not all of the measures are what we would have chosen later in the pandemic when validated measures were more readily available (eg, the Perceived Vulnerability to COVID-19 Scale uses questions with different Likert scales). Moreover, COVID-19 and recommendations for health protective behaviors have rapidly evolved, and because of the cross-sectional nature of the study, we are not adequately able to account for changes in state policies or personal behaviors over time. Despite the limitations, this article adds to the knowledge of the engagement in and the correlates of health protective behaviors during the COVID-19 pandemic.
Conclusions
Our study outlines Arkansans’ engagement with health protective behaviors during the COVID-19 pandemic. The results show high levels of engagement with behaviors such as social distancing and face mask wearing. The study also demonstrates lower engagement with behaviors such as staying at home when not sick and avoiding gathering with people outside one’s household. Future pandemic planning will need to consider how to create clear and compelling messaging and interventions to increase these behaviors to the level needed for community-wide protection. In addition, specific attention will need to be directed to creating targeted messaging and interventions for young adults, White individuals, men, and people with lower education levels. Healthcare providers and mental health professionals will need to address fears and stressors related to COVID-19 in both healthy populations and those with chronic conditions, and providers will need to counsel their patients on managing the fears and anxieties that may be maladaptive.
Footnotes
Supplemental digital content is available for this article. Direct URL citations appear in the printed text, and links to the digital files are provided in the HTML text of this article on the journal’s Web site (http://sma.org/smj).
The project described was supported by the University of Arkansas for Medical Sciences Translational Research Institute, grant no. UL1 TR003107, through the National Center for Advancing Translational Sciences of the National Institutes of Health (NIH). The authors did not report any financial relationships or conflicts of interest. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Contributor Information
Jennifer A. Andersen, Email: jaandersen@uams.edu.
Brett Rowland, Email: mbrowland@uams.edu.
Shawn M. Ratcliff, Email: sratcliff@huskers.unl.edu.
Holly C. Felix, Email: felixholly@uams.edu.
References
- 1.Holshue ML DeBolt C Lindquist S, et al. First case of 2019 novel coronavirus in the United States. N Engl J Med 2020;382:929–936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention . Public health recommendations for community-related exposure. https://www.cdc.gov/coronavirus/2019-ncov/php/public-health-recommendations.html. Accessed April 20, 2020.
- 3.Hsiang S Allen D Annan-Phan S, et al. The effect of large-scale anti-contagion policies on the COVID-19 pandemic. Nature 2020;584:262–267. [DOI] [PubMed] [Google Scholar]
- 4.Hendrix MJ. Absence of apparent transmission of SARS-CoV-2 from two stylists after exposure at a hair salon with a universal face covering policy—Springfield, Missouri, May 2020. MMWR Morb Mortal Wkly Rep 2020;69:930–932. [DOI] [PubMed] [Google Scholar]
- 5.Lyu W, Wehby GL. Community use of face masks and COVID-19: evidence from a natural experiment of state mandates in the US. Health Aff 2020;39:1419–1425. [DOI] [PubMed] [Google Scholar]
- 6.Matrajt L, Leung T. Evaluating the effectiveness of social distancing interventions to delay or flatten the epidemic curve of coronavirus disease. Emerg Infect Dis 2020;26:1740–1748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hutchins HJ Wolff B Leeb R, et al. COVID-19 mitigation behaviors by age group—United States, April–June 2020. Morb Mortal Wkly Rep 2020;69(43):1584–1590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lüdecke D, von dem Knesebeck O. Protective behavior in course of the COVID-19 outbreak—survey results from Germany. Front Public Health 2020;8:572561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hearne BN, Niño MD. Understanding how race, ethnicity, and gender shape mask-wearing adherence during the COVID-19 pandemic: evidence from the COVID Impact Survey. J Racial Ethn Health Dispar 2022;9:176–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nivette A Ribeaud D Murray A, et al. Non-compliance with COVID-19-related public health measures among young adults in Switzerland: insights from a longitudinal cohort study. Soc Sci Med 2021;268:113370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Harper CA Satchell LP Fido D, et al. Functional fear predicts public health compliance in the COVID-19 pandemic. Int J Ment Health Addict 2021;19:1875–1888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Coroiu A Moran C Campbell T, et al. Barriers and facilitators of adherence to social distancing recommendations during COVID-19 among a large international sample of adults. PloS One 2020;15:e0239795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bearth A, Luchsinger L, Siegrist M. Reactions of older Swiss adults to the COVID-19 pandemic: a longitudinal survey on the acceptance of and adherence to public health measures. Soc Sci Med 2021;280:114039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fisher KA Barile JP Guerin RJ, et al. Factors associated with cloth face covering use among adults during the COVID-19 pandemic — United States, April and May 2020. Morb Mortal Wkly Rep 2020;69:933–937. [DOI] [PubMed] [Google Scholar]
- 15.Laires PA Dias S Gama A, et al. The association between chronic disease and serious COVID-19 outcomes and its influence on risk perception: survey study and database analysis. JMIR Public Health Surveill 2021;7:e22794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Umucu E, Lee B. Examining the impact of COVID-19 on stress and coping strategies in individuals with disabilities and chronic conditions. Rehabil Psychology 2020;65:193–198. [DOI] [PubMed] [Google Scholar]
- 17.Van Bavel JJ Baicker K Boggio PS, et al. Using social and behavioural science to support COVID-19 pandemic response. Nature Hum Behav 2020;4:460–471. [DOI] [PubMed] [Google Scholar]
- 18.Centers for Disease Control and Prevention . 2019 BRFSS Questionnaire. https://www.cdc.gov/brfss/questionnaires/pdf-ques/2019-BRFSS-Questionnaire-508.pdf. Accessed June 24, 2020.
- 19.PhenX Toolkit. COVID-19 protocol library. https://www.phenxtoolkit.org/covid19. Accessed April 21, 2020. [Google Scholar]
- 20.Arkansas State Chamber of Commerce . Gov. Hutchinson issues face mask mandate for Arkansas Effective July 20. https://www.arkansasstatechamber.com/news-publications/news-releases/gov-hutchinson-issues-face-mask-mandate-for-arkansas-effective-july-20. Accessed March 5, 2022.
- 21.Johansson MA Quandelacy TM Kada S, et al. SARS-CoV-2 transmission from people without COVID-19 symptoms. JAMA Netw Open 2021;4:e2035057-e2035057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Centers for Disease Control and Prevention . COVID Data Tracker. https://covid.cdc.gov/covid-data-tracker. Accessed March 23, 2022.
- 23.Papageorge NW Zahn MV Belot M, et al. Socio-demographic factors associated with self-protecting behavior during the Covid-19 pandemic. J Popul Econ 2021;34:691–738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.English E Long CR Langston K, et al. A community partnership for home delivery of food boxes to COVID-19 quarantined and isolated families. J Hunger Environ Nutr 2021;16:19–28. [Google Scholar]
- 25.McElfish PA, Purvis RS, Willis DE, Riklon S. COVID-19 Disparities among Marshallese Pacific Islanders. Prev Chronic Dis 2021;18(200407). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jones J Sullivan PS Sanchez TH, et al. Similarities and differences in COVID-19 awareness, concern, and symptoms by race and ethnicity in the United States: cross-sectional survey. J Med Internet Res 2020;22:e20001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ogedegbe G Ravenell J Adhikari S, et al. Assessment of racial/ethnic disparities in hospitalization and mortality in patients with COVID-19 in New York City. JAMA Netw Open 2020;3:e2026881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Perry A, Harshbarger D, Romer C. Mapping racial inequity amid COVID-19 underscores policy discrimination against Black Americans. https://www.brookings.edu/blog/the-avenue/2020/04/16/mapping-racial-inequity-amid-the-spread-of-covid-19. Published April 16, 2020. Accessed March 5, 2022.
- 29.Wise T Zbozinek TD Michelini G, et al. Changes in risk perception and self-reported protective behaviour during the first week of the COVID-19 pandemic in the United States. R Soc Open Sci 2020;7:200742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schimmenti A, Billieux J, Starcevic V. The four horsemen of fear: an integrated model of understanding fear experiences during the COVID-19 pandemic. Clin Neuropsychiatry 2020;17:41–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zaki N, Alashwal H, Ibrahim S. Association of hypertension, diabetes, stroke, cancer, kidney disease, and high-cholesterol with COVID-19 disease severity and fatality: a systematic review. Diabetes Metab Syndr 2020;14:1133–1142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Habecker P, Ivanich J. Unintended interviewer bias in a community-based participatory research randomized control trial among American Indian youth. In: Olson K Smyth JD Dykema J, et al., eds. Interviewer Effects from a Total Survey Error Perspective. Boca Raton, FL: Chapman & Hall/CRC; 2020:137. [Google Scholar]


