Fig. 4.
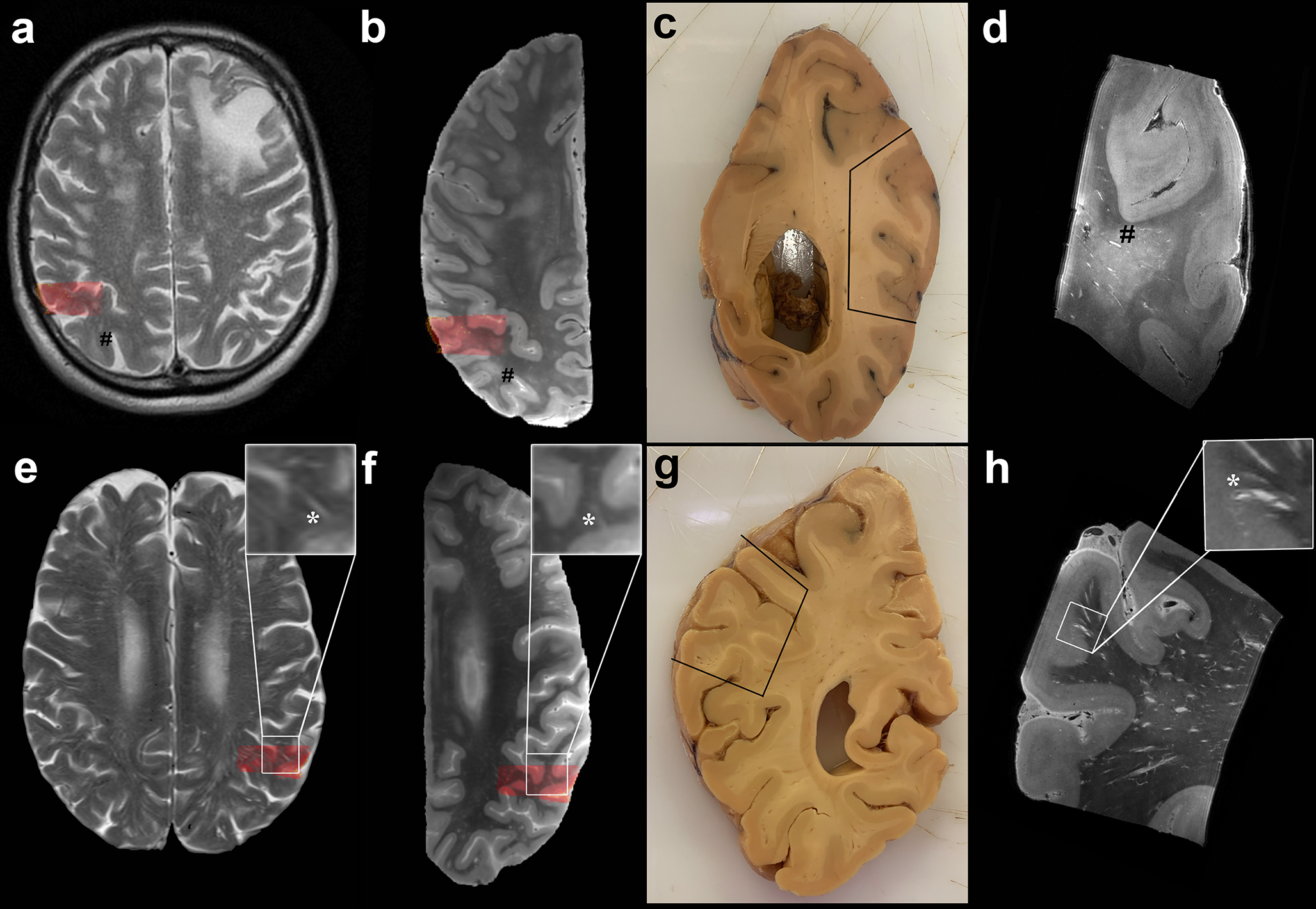
In depth characterization of MRI-visible perivascular spaces (PVS). Top row: MRI-visible PVS (mild degree) observed in the centrum semiovale on in vivo MRI of a case with neuropathologically confirmed CAA (case no. 5) (a). Corresponding ex vivo 3 tesla T2-weighted MRI scan of the right hemisphere, where some MRI-visible PVS are also observed (b) (indicated by #). Formalin fixed tissue of the same brain, on which the parietooccipital area sampled for ultra-high resolution ex vivo 7 tesla MRI is marked by the black line (c) and co-registered to in vivo and ex vivo 3 tesla MRI (red overlaid area). The enlarged PVS are clearly visible at the 100 μm isotropic resolution T2-weighted scan (#) (d). Bottom row: Evidence of severe degree of MRI-visible PVS on the T2-weighted in vivo MRI of case no. 13 (e), with corresponding ex vivo 3 tesla MRI of the left hemisphere (f), formalin fixed tissue (g) and ultra-high resolution T2-weighted scan (h). More MRI-visible PVS are observed in case no. 13 than case 5. The MRI-visible PVS appear to be confined to the WM on in vivo and ex vivo 3 tesla MRI, whereas they can be clearly seen to continue into the cortex at ultra-high resolution in this case (insets of the bottom row, *). The EPVS-related vessels are visible at 7 tesla as hypointense structures at the center of the EPVS. They originate at the pial surface as leptomeningeal vessels, dive into the cortex as cortical perforating vessels, and continue into the white matter (h). See also Supplementary Videos 1 - 3. For the purposes of registration between in vivo and ex vivo MRI the skull and the plastic bag in which the hemispheres were placed prior to scanning, were removed from the images
