Abstract
The existing pandemic viral infection caused by severe acute respiratory syndrome coronavirus type 2 (SARS-CoV-2) leads to coronavirus disease 2019 (Covid-19). SARS-CoV-2 exploits angiotensin-converting enzyme 2 (ACE2) as an entry-point into affected cells and down-regulation of ACE2 by this virus triggers the release of pro-inflammatory cytokines and up-regulation of angiotensin II. These changes may lead to hypercytokinemia and the development of cytokine storm with the development of acute lung injury and acute respiratory distress syndrome. Different repurposed had been in use in the management of Covid-19, one of these agents is pentoxifylline (PTX) which has anti-inflammatory and antioxidant properties. Therefore, the objective of the present mini-review is to highlight the potential role of PTX in Covid-19 regarding its anti-inflammatory and antioxidant effects. PTX is a non-selective phosphodiesterase inhibitor that increases intracellular cyclic adenosine monophosphate which stimulates protein kinase A and inhibits leukotriene and tumor necrosis factor. PTX has antiviral, anti-inflammatory and immunomodulatory effects, thus it may attenuate SARS-CoV-2-induced hyperinflammation and related complications. As well, PTX can reduce hyper-viscosity and coagulopathy in Covid-19 through increasing red blood cell deformability and inhibition of platelet aggregations. In conclusion, PTX is a non-selective phosphodiesterase drug, that has anti-inflammatory and antioxidant effects thereby can reduce SARS-CoV-2 infection-hyperinflammation and oxidative stress. Besides, PTX improves red blood cells (RBCs) deformability and reduces blood viscosity so can mitigate Covid-19-induced hyper-viscosity and RBCs hyper-aggregation which is linked with the development of coagulopathy. Taken together, PTX seems to be an effective agent against Covid-19 severity.
Keywords: Covid-19, Blood viscosity, Coagulopathy, Pentoxifylline, Hyperinflammation
Introduction
The existing pandemic viral infection caused by severe acute respiratory syndrome coronavirus type 2 (SARS-CoV-2) leads to coronavirus disease 2019 (Covid-19) (Al-Kuraishy et al. 2021d). SARS-CoV-2 exploits angiotensin-converting enzyme 2 (ACE2) as an entry-point into the affected cells and down-regulation of ACE2 by this virus triggers the release of pro-inflammatory cytokines and up-regulation of angiotensin II (AngII) (Onohuean et al. 2021). These changes may lead to hypercytokinemia and the development of cytokine storm with the development of acute lung injury (ALI) and acute respiratory distress syndrome (ARDS) (Onohuean et al. 2021). The clinical presentation of Covid-19 is asymptomatic or mild symptoms in the majority of cases. However, 5–10% of patients’ progress to develop acute and critical complications requested hospitalization and assist ventilation due to the development of severe ALI and ARDS (Al-Kuraishy et al. 2021a; Al-Kuraishy and Al-Gareeb 2021).
Different repurposed had been in use in the management of Covid-19, though none of used drugs produced complete recovery (Al-Kuraishy et al. 2021c). In this sense, anti-inflammatory and antioxidant agents were trialed against SARS-CoV-2 infection in various in silico, experimental and preclinical studies. One of these agents is pentoxifylline (PTX) which has anti-inflammatory and antioxidant properties (Al-Kuraishy et al. 2019).
Therefore, the objective of the present mini-review is to highlight the potential role of PTX in Covid-19 regarding its anti-inflammatory and antioxidant effects.
Pharmacology of pentoxifylline
PTX is a derivative of xanthine (1-5-oxohexyl-3-7-dimethylxanthine) and structurally related to caffeine and theophylline (Fig. 1) (Wikipedia 2014). PTX is synthesized by introducing hexanone to theobromine extracted from cocoa bean alkaloid. PTX acts as a non-selective phosphodiesterase inhibitor (PDEI) that increases intracellular cyclic adenosine monophosphate (cAMP) which stimulates protein kinase A (PKA) and inhibits leukotriene and tumor necrosis factor (TNF) (Hussien et al. 2019). As well, PTX is regarded as an antagonist for adenosine 2 receptor (A2R) (Hussien et al. 2019). PTX reduces activation of innate immunity and release of inflammatory cytokines.
Fig. 1.
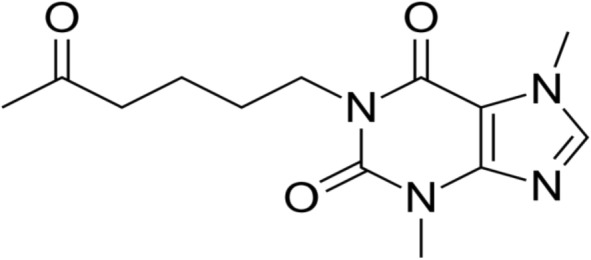
Chemical of pentoxifylline (Wikipedia 2014)
PTX was in the clinical use since 1972 and approved by Food and Drug Administration (FDA) in 1984 (Frampton and Brogden 1995). PTX is indicated in the management of peripheral vascular diseases, arterial disease-induced intermittent claudication, and chronic leg ulcers (Chandan et al. 2018). PTX decreases blood viscosity by reducing fibrinogen plasma levels, increasing red blood cell flexibility, and inhibiting platelet aggregation (Rasyid et al. 2018). It inhibits the activation and adhesion of neutrophils and reduces the formation of free radicals (Rasyid et al. 2018). As well, PTX inhibits fibrotic changes through inhibition of tumor growth factor-beta (TGF-β) connective tissue growth factor (Delanian et al. 2005).
PTX may be effective in treating sarcoidosis by inhibiting TNF-induced granuloma formation (Tong et al. 2003). Besides, it is effective against alcoholic hepatitis (Whitfield et al. 2009) and diabetic neuropathy (Hosseini et al. 2019). As well, different researches suggested that PTX could be effective in treating erectile dysfunction (Law et al. 2020), hearing loss (Lan et al. 2018), Peyronie’s disease (Ibrahim et al. 2019), and osteoradionecrosis (Kolokythas et al. 2019).
Common side effects of PTX are palpitation, flushing, headache, and arrhythmias (Chandan et al. 2018). PTX is orally active with low bioavailability (20–30%) due to extensive first-pass metabolism (Chandan et al. 2018). PTX has high plasma protein binding and 45% of it binds the erythrocyte membrane, it is metabolized by liver and excreted by renal route (Rasyid et al. 2018). PTX has short half-life about 1.6 h (Rasyid et al. 2018). PTX toxicity was reported at a dose of 80 mg/kg, leading to hypotension, flushing, and convulsion (Dianey et al. 2021). These findings suggest that PTX is a safe drug and has no serious drug–drug interaction and can be used easily.
Pleiotropic effects of pentoxifylline
Anti-inflammatory effects
PTX has potent anti-inflammatory effects by inhibiting the release of pro-inflammatory cytokines and increasing the production of anti-inflammatory cytokines in patients with acute coronary syndrome (ACS) (Fernandes et al. 2008). PTX enhances the anti-inflammatory of steroids and non-steroidal anti-inflammatory drugs for the management of inflammation in rats (Abdel-Salam et al. 2003). A prospective study comprised 64 patients with ACS treated with PTX 400 mg/day or placebo for 6 months illustrated that PTX reduced interleukin 6, 12 (IL-6, IL-12), and TNF-α with an increment of IL-10 (Fernandes et al. 2008). Dong et al. illustrated that PTX exerts anti-inflammatory effects in rats with cerebral ischemia–reperfusion injury by inhibiting cyclooxygenase 2 (COX2), inducible nitric oxide synthase (iNOS), TNF-α, matrix metalloproteinase 9 (MMP9), caspase-3 and p38 mitogen-activated protein kinase (p38MAPK) (Dong et al. 2018).
Moreover, PTX attenuates the synthesis and release of TNF-α from alveolar macrophages (AMs) and monocytes with suppression expression of IL-2 receptor on the lymphocytes (Marques et al. 1999). Tong et al. observed that PTX reduces the release of cytokine release from lipopolysaccharide (LPS)-induced activated AMs in patients with sarcoidosis (Tong et al. 2003). In a vitro study, AMs were isolated from 14 patients with sarcoidosis, and cultured with PTX or dexamethasone; both PTX and dexamethasone produced similar effects (Tong et al. 2003). Therefore, PTX can replace dexamethasone in the management of sarcoidosis.
Furthermore, PTX inhibits activation and adhesion of T lymphocytes by inhibition of integrins induced by different intracellular signals (González-Amaro et al. 1998). However, PTX can restore the viability of T lymphocytes in hyperinflammatory conditions (Park et al. 2020). Indeed, PTX has differential effects on the production of cytokines; it increases anti-inflammatory cytokines and reduces releases of pro-inflammatory cytokines (Marcinkiewicz et al. 2000). Similarly, PTX inhibits endotoxin-induced activation of nuclear factor kappa B (NF-κB) with reduction release of pro-inflammatory cytokines in rats through inhibition of A2R and PDE (Ji et al. 2004).
These verdicts suggest that PTX has noteworthy immunological and anti-inflammatory effects through modulation of immune cells and release of inflammatory cytokines (Fig. 2).
Fig. 2.
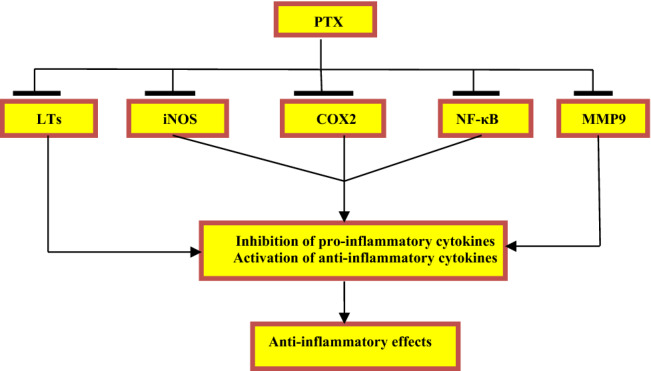
Anti-inflammatory effects of pentoxifylline (PTX): PTX inhibits activation of leukotrienes (LTs), inducible nitric oxide synthase (iNOS), cyclooxygenase 2 (COX2), nuclear factor kappa B (NF-κB), and matrix metalloproteinase 9 (MMP9) leading to inhibition release of pro-inflammatory cytokines with activation of anti-inflammatory cytokines
Antioxidant effects
PTX has antioxidant effects by scavenging free radicals and reactive oxygen species (ROS) in patients with cerebrovascular disorders (Horvath et al. 2002). Of interest, PTX had the ability to decrease radiation injury by antioxidant effect; it reduces the activity of myeloperoxidase and malondialdehyde (MDA), with increasing activity of glutathione (Hepgül et al. 2010). Noyan and colleagues demonstrated that PTX exerted an antioxidant effect against experimental short-bowel syndrome by reducing lipid peroxidation as evidenced by the reduction of MDA (Noyan et al. 2003).
Similarly, PTX attenuates oxidative stress-mediated renal injury in rats (Dávila-Esqueda and Martinez-Morales 2004). Moreover, PTX can reduce cardiac oxidative stress by increasing the activity of catalase and superoxide dismutase in rats (Mayyas et al. 2015). As well, PTX decreases oxidative stress in patients with non-alcoholic steatohepatitis (Satapathy et al. 2004). Of note, PTX improves sperm motility in patients with infertility by attenuation of oxidative stress (Oliva et al. 2009). These findings indicated that PTX has antioxidant effects by inhibiting ROS and induction of endogenous antioxidant capacity (Fig. 3).
Fig. 3.
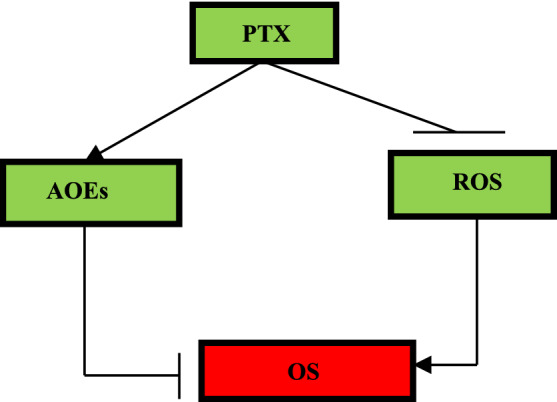
Antioxidant effects of pentoxifylline (PTX): PTX inhibits the generation of reactive oxygen species (ROS) with activation of antioxidant enzymes (AOEs)
Antiviral effects
PTX had been reported to be effective to inhibit replication of the Japanese encephalitis virus in a dose-dependent manner both in vitro and in vivo (Sebastian et al. 2009). PTX 100–200 mg/kg protects mice from a lethal dose of the Japanese encephalitis virus (Sebastian et al. 2009). It has been reported that PTX was effective against acute porcine pneumonia with a reduction of cytokine-induced tissue injury (Myers et al. 2002).
As well, PTX is effective against human immune deficiency virus 1 (HIV-1) by reducing viremia with increasing CD4+ and modulation of inflammatory cytokines (Smith et al. 2007). In addition, PTX inhibits replication of HIV-1 through suppression of TNF-α-mediated long-term repeat-driven expression which is regarded as a vector for this virus (Smith et al. 2007). Therefore, PTX blocks the transduction and replication of HIV-1.
Moreover, PTX inhibits respiratory syncytial virus-induced expression of TNF-α mRNA and TNF-α release (Tao et al. 2001). Remarkably, PTX may increase the risk of enterovirus A71-induced encephalitis by reduction of IL-6, which inversely correlated with the duration of hospitalization in patients with different viral infections (Wang et al. 2017).
Therefore, PTX has broad-spectrum antiviral effects and can reduce associated inflammatory disorders by immunomodulatory effects.
Antithrombotic effects
It has been reported that PTX had antiplatelet and antithrombotic effects and could be an alternative therapy for thromboembolism and vascular vasospasm against ischemia (Bayraktar and Tanyeri-Bayraktar 2021). Similarly, PTX inhibits adenosine-induced platelet aggregation (Timchenko et al. 2019). De-Sanctis et al. (2002) showed that PTX was effective in treating retinal vein thrombosis as compared with placebo in patients with sudden vision loss. As well, PTX inhibits fibrinogen activation, generation of fibrin and platelet hyper-reactivity in patients with disseminated intravascular coagulopathy (DIC) (Ozden et al. 2019). PTX is effective against DIC and coagulopathy in patients with Kassabach–Merit syndrome (Abdul Hadi and Hisham 2011). Indeed, PTX improves the activity of fibrinolytic pathway locally, as PTX increases the activity of streptokinase against the formation of post-operative abdominal adhesions (Jafari-Sabet et al. 2015). Moreover, PTX prevents endotoxic-induced activation of coagulation and fibrinolytic disorders (Levi et al. 1994).
The underlying antithrombotic mechanism of PTX is related to inhibiting the production of fibrinogen and increasing the fibrinolytic pathway in patients with peripheral vascular diseases (Zhang et al. 2004). In addition, PTX attenuates the production and release of platelet-derived growth factors (PDGFs) which engaged with the increase of airway smooth reactivity, vascular smooth contraction, and platelet activation (Shi and Appiah-Kubi 2020). Besides, PTX inhibits platelet activation through increasing cAMP and prostacyclin (Zhang et al. 2004).
Furthermore, red blood cells (RBCs) are involved in thrombosis since quantitative and qualitative abnormalities of RBCs as thalassemia, sickle cell anemia, and polycythemia increase the risk of coagulopathy (Al-Kuraishy and Al-Gareeb 2017; Byrnes and Wolberg 2017). RBCs increase platelets margination with the enhancement of their interaction, accumulation, and adhesion at the subendothelial area (Byrnes and Wolberg 2017). As well, the release of ADP from injured RBCs promotes platelet aggregation by increasing the interaction with P-selectin (Byrnes and Wolberg 2017). Therefore, PTX through inhibition of blood viscosity and enhancement of RBCs deformability may inhibit RBCs induced coagulopathy.
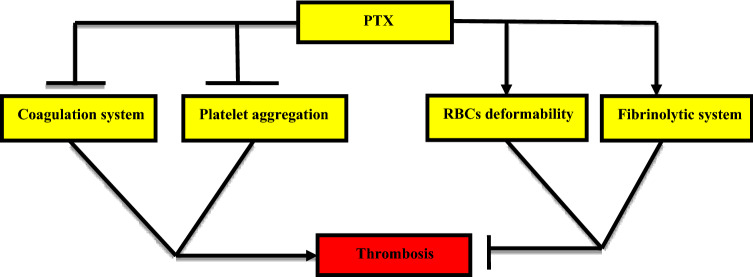
These findings confirm the potential antithrombotic effect of PTX through modulation of coagulation pathway and inhibition of platelet aggregations (Fig. 4).
Fig. 4.
Antithrombotic mechanism of pentoxifylline (PTX): PTX inhibits coagulation system and platelet aggregations, stimulates red blood cells (RBCs) deformability, and fibrinolytic pathway with subsequent inhibition of thrombosis
Anti-acute lung injury
ALI is a common complication in different viral infections including SARS-CoV-2 infection (Onohuean et al. 2021). It has been reported that PTX was effective against ALI in chronic endotoxemia as evident by reduction of intercellular adhesion molecule 1 (ICAM-1) and IL-6 in LPS-induced ALI in rats (Michetti et al. 2003). Sunil et al. demonstrated that PTX can reduce lung toxicity and nitrogen mustard-induced ALI by reduction of oxidative stress and release of pro-inflammatory cytokines as well as expression of COX2 and MMP9 on the activated AMs (Sunil et al. 2014). Furthermore, PTX improves gas exchange and reduces lung inflammation in sepsis-induced ALI (Oliveira-Júnior et al. 2006).
The potential mechanism of PTX in the amelioration of ALI could be through modulation of inflammatory cytokines, reduction of oxidative stress and inhibition of ischemic-reperfusion injury (Pawlik et al. 2005). Thus, these observations pointed out that PTX is effective against ALI induced by toxins and chemicals and could be of benefit in the management of ALI.
Potential role of pentoxifylline in Covid-19
Effects on the inflammatory and oxidative burden
In Covid-19, exaggerated immune response and high release of pro-inflammatory cytokines mainly TNF-α and IL-6 are linked with the development of cytokine storm, ALI, ARDS and multi-organ injury (Al-Kuraishy et al. 2022a; b). Therefore, PTX could be effective against Covid-19-induced ALI and ARDS through inhibition of TNF-α and IL-6 (Hendry et al. 2020). As well, PTX attenuates ALI through inhibition of A2R which is linked with induction of inflammatory cascades during ALI (Effendi et al. 2020). Adenosine is released due to cell injury and serves as a mediator of inflammation during SARS-CoV-2 infection (Abouelkhair 2020). Therefore, targeting of the adenosinergic pathway in SARS-CoV-2 infection could reduce Covid-19 severity. Hendry and colleagues proposed that PTX through modulation of inflammatory cytokines and blood viscosity might be a therapeutic option in the management of Covid-19 (Hendry et al. 2020).
Furthermore, phosphodiesterase inhibitors like PTX inhibit the synthesis of leukotriene synthesis by neutrophils through increasing intracellular cAMP (Peters-Golden et al. 2005). Al-kuraishy et al. (2021b) revealed that the leukotriene pathway is activated in Covid-19 and linked with the development of pulmonary and extra-pulmonary complications. As well, PTX decreases the expression of COX2 in the pancreases of diabetic rats (Garcia et al. 2014). Similarly, COX2 is over-activated in Covid-19 causing induction and propagation of inflammatory reactions (Perricone et al. 2020). Thus, PTX could be effective against systemic complications induced by Covid-19 through modulation of the leukotriene pathway.
It has been shown that oxidative stress is augmented in Covid-19 due to the generation of ROS and reduction of endogenous antioxidant capacity leading to endothelial dysfunction (ED) and thrombosis (de Las Heras et al. 2020). Of note, PTX has a potent antioxidant effect (Noyan et al. 2003), therefore, could be effective against Covid-19-induced oxidative stress. Chavarria et al. illustrated that the antioxidant effect of PTX can improve outcomes in Covid-19 patients (Chavarría et al. 2021). A prospective study involved 110 Covid-19 patients treated with standard therapy in conjugation with PTX with several antioxidants showed that PTX added a potential benefit against Covid-19 severity as evident by reduction of IL-6 and c-reactive protein (CRP) (Chavarría et al. 2021).
Of note, sepsis induces neutrophil activation with subsequent release of ROS, and inhibition of nitric oxide (NO) causing an increase in adhesion molecules and platelet aggregation and/or coagulopathy (Kaur et al. 2018). Likewise, lung ischemia is developed due to oxidation caused by the over-activation of iNOS and nicotinamide adenine dinucleotide phosphate (NADPH) oxidase (Mittal et al. 2014). Delgado-Roche and Mesta (2020) observed that oxidative stress plays a critical role in the induction of ALI/ARDS in SARS-CoV-2 infection through activation of iNOS. However, NO may reduce in severe Covid-19 due to reduction in the synthesis of NO by hypoxia or consumption of NO by ROS (Delgado-Roche and Mesta 2020). PTX can attenuate oxidative stress-induced renal injury by reducing the activity of NADPH oxidase (Ozturk et al. 2019). In addition, PTX reduces inflammatory reactions and oxidative stress by modulation activity of iNOS (de Oliveira Garcia et al. 2015). Therefore, PTX can attenuate SARS-CoV-2 infection-induced oxidative stress via the regulation of activated iNOS and NADPH oxidase.
Indeed, viral infections including SARS-CoV-2 infection-induced oxidative stress trigger the formation of oxidized phospholipids which activate toll-like receptor 4 (TLR4) and NF-κB leading to hyperinflammation-mediated ALI/ARDS (Monji et al. 2020). It was reported that PTX attenuated morphine-induced inflammation by inhibiting the activity of TLR4 in rats (Chehrei et al. 2017). Similarly, PTX mitigated endotoxin-induced release of pro-inflammatory cytokines through suppression of NF-κB activation (Ji et al. 2004). In addition, PTX through inhibition of AMs can inhibit the release of pro-inflammatory cytokines during the development of ALI/ARDS (Tong et al. 2003). Interestingly, the mechanistic target of rapamycin (mTOR) is involved in the induction of autophagy and viral replication including SARS-CoV-2, therefore, inhibition of mTOR might be of therapeutic value in the suppression of viral infection (Karam et al. 2021). It has been shown that PTX inhibits mTOR and autophagy (Hekmat et al. 2020).
Therefore, PTX through inhibition of TLR4, mTOR and NF-κB signaling pathway can reduce the interaction between oxidative stress and inflammatory reaction in Covid-19.
In SARS-CoV-2 infection, nod-like receptor pyrin 3 (NLRP3) inflammasome is activated leading to the activation release of IL-1β and IL-18 from activated macrophages. Activated NLRP3 inflammasome contributes in the activation of other inflammatory signaling pathways causing the development of cytokine storm and tissue injury (Freeman and Swartz 2020). It has been shown that caffeine; PTX and other phosphodiesterase inhibitors inhibit the expression of NLRP3 inflammasome directly or indirectly by suppression of MAPK and NF-κB (Zhao et al. 2019). As well, oxidative stress and pro-inflammatory cytokines trigger activation and propagation of NLRP3 inflammasome activity in patients with cardiovascular complications (Sharma et al. 2018). In virtue of it antioxidant and anti-inflammatory effects, PTX could be effective against Covid-19 severity through inhibition of NLRP3 inflammasome.
A pilot study comprised 38 patients with severe Covid-19 to study the potential effect of PTX on lymphocyte count and lactate dehydrogenase (LDH) showed that PTX reduced LDH by 29.61% (95% CI 15.11–44.10) and increased in lymphocyte count by 64.25% (95% CI 15.11–83–116.68) (Maldonado et al. 2021). High LDH serum level indicates tissue damage and is correlated with the severity of ALI in SARS-CoV-2 infection (Xiong et al. 2020). Similarly, lymphopenia is regarded as an independent biomarker of Covid-19 severity (Seyit et al. 2021). Monji et al. (2020) observed that PTX therapy could be an effective agent against Covid-19 severity through the improvement of microcirculation and tissue oxygenation by reducing inflammatory/oxidative burden and blood viscosity. Therefore, reduction of LDH serum level and elevation of lymphocyte count following PTX therapy in Covid-19 indicates a promising therapeutic role of PTX against Covid-19 severity.
These findings suggest that PTX could be effective against Covid-19 through modulation of inflammatory and oxidative burden.
Effects on the renin–angiotensin system
Renin–angiotensin system (RAS) has been shown to be dysregulated in Covid-19 due to down-regulation of ACE2 which is necessary for the conversion of vasoconstrictor and pro-inflammatory AngII to vasodilator and anti-inflammatory Ang1-7 (Al-Kuraishy et al. 2020). High circulating AngII level is linked with the development of ALI/ARDS, ED, oxidative stress and release of pro-inflammatory cytokines (Sfera et al. 2020). Therefore, AngII receptor blockers (ARBs) have been shown to be protective against Covid-19 severity through inhibition of vasoconstrictor AngII receptor type 1 (AT1R) (Lopes et al. 2021).
It was reported that PTX inhibits the expression of AT1R without a significant effect on blood pressure (Brie et al. 2016). In clinical trials, PTX had been shown to improve the effect of ARBs in patients with diabetic nephropathy through modulation the effect of AngII (Navarro et al. 2005). In addition, experimental studies demonstrated that PTX inhibits the expression of AT1R mRNA (Guggilam et al. 2008). Navarro et al. demonstrated that PTX modulates the expression of renal ACE through inhibition of pro-inflammatory cytokines in rats (Navarro et al. 2006). Moreover, PTX may attenuate the development of hypertension through the modulation of RAS in rats with induced metabolic syndrome (Azhar and El-Bassossy 2015). In addition, PTX decreases cardiac fibrosis and inflammation in AngII-induced hypertension in rats (Zhang et al. 2016).
Depending on these findings, PTX could be effective against AngII-mediated complications in Covid-19.
Effects on blood viscosity and coagulopathy
It has been shown that blood viscosity and RBC aggregation are increased in Covid-19 patients and linked with risk of thrombosis and life-threatening complications (Nader et al. 2021). A cohort study involved 172 hospitalized Covid-19 patients compared with 38 healthy controls revealed that Covid-19 patients had higher blood viscosity despite of low hematocrit with exaggerated RBC aggregation (Nader et al. 2021). As well, hyper-aggregation of RBCs correlated with thrombosis and extensive lung lesion, and poor clinical outcomes in Covid-19 patients (Nader et al. 2021). Similarly, reduction of RBCs deformability due to structural changes in RBC membrane was confirmed in Covid-19 patients as evidenced by the increased level of schistocytes (Kubánková et al. 2021).
Furthermore, SARS-CoV-2 infection is associated with systemic and pulmonary microthrombosis leading to pulmonary dysfunction and development of ALI/ARDS (Suh et al. 2021). SARS-CoV-2 infection-induced thrombosis is reported to cause acute myocardial injury in about 20% and acute ischemic stroke up to 5% in hospitalized patients (Suh et al. 2021). Down-regulation of ACE2, ED, inflammatory and oxidative stress disorders with platelet hyper-activation could be the possible mechanisms of thrombosis in Covid-19 (Gomez-Mesa et al. 2021). Besides, platelet hyper-activation in SARS-CoV-2 infection contribute to increase factor XII and von Willebrand factor with subsequent spread of pro-coagulant and pro-inflammatory activities in systemic circulation (Taus et al. 2020).
Of note, PTX has the ability to reduce blood viscosity and coagulopathy by increasing RBCs deformability and inhibition of platelet reactivity respectively (Rasyid et al. 2018; Ozden et al. 2019). Therefore, PTX could be a possible therapeutic modality against Covid-19-induced hyper-viscosity and coagulopathy.
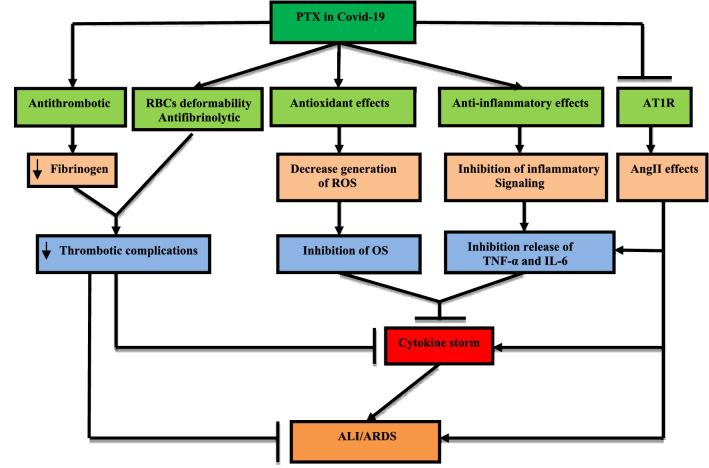
Taken together, in virtue of its anti-inflammatory, antioxidant and antithrombotic effects, PTX could be the possible drug in the management of Covid-19 (Fig. 5).
Fig. 5.
Role of pentoxifylline (PTX) in Covid-19: PTX inhibits expression of angiotensin 1 receptor (AT1R) with reduction of angiotensin II (AngII)-mediated progression of cytokine storm and development of acute lung injury (ALI)/acute respiratory distress syndrome (ARDS): PTX antioxidant effect reduces the generation of reactive oxygen species (ROS) and the development of oxidative stress (OS). PTX anti-inflammatory effects inhibit release of IL-6 and tumor necrosis factor alpha (TNF-α). PTX through inhibition of fibrinogen, activation of antifibrinolytic and RBCs deformability inhibits thrombosis
The present review had several limitations including the rareness of clinical studies regarding the role of PTX in Covid-19 and most of the beneficial effects in Covid-19 were speculative. However, this review highlighted the most important effects of PTX in Covid-19. This review recommends future studies to confirm the possible role of PTX in the management of Covid-19.
Anti-SARS-CoV-2 activity of pentoxifylline
The anti-SARS-CoV-2 activity of PTX has not been evaluated and tested in both in vitro and vivo studies, though its activity was tested against various viral infections (Assimakopoulos et al. 2020). As SARS-CoV-2 infection continues to cause global upheaval, researchers, and scientists are in racing and competing to find and discover optimal animal models to study Covid-19 pathogenesis. Of note, SARS-CoV-2 transmission between ferrets and cats could be an integral animal model for SARS-CoV-2 transmission (Lakdawala and Menachery 2020). However, aged and young cynomolgus macaques infected with SARS-CoV-2 failed to develop clinical symptoms of Covid-19 despite of prolong shedding of this virus in the upper and lower respiratory tract. Thus, these animal models show distinct forms regarding SARS-CoV-2 transmission and development of Covid-19 (Lakdawala and Menachery 2020). The main obstacle in for induction of mouse SARS-CoV-2 infection is the lack of suitable receptors to recruit viral infection since mouse ACE2 does not sufficiently bind SARS-CoV-2 spike protein (Wan et al. 2020). As different models for SARS-CoV-2 infection are under investigations and testing phase and some biotech companies bypassed animal model studies and gone to phase I clinical trials. In this state, bypassing of animal studies for testing novel or repurposed drugs in SARS-CoV-2 infection may reduce our knowledge about human clinical outcomes (Deb et al. 2020). Notably, SARS-CoV-2 has high genomic similarity with SARS-CoV (Al-Kuraishy and Al-Gareeb 2021) and PTX was found to be ineffective against replication of SARS-CoV in mice (Hendry et al. 2020). Despites of these limitations, K18-hACE2 transgenic mice that were initially developed for SARS studies are used in a recent study to evaluate therapeutic intervention in treating Covid-19 (Zheng et al. 2021).
Conclusion
PTX is a non-selective phosphodiesterase drug, has anti-inflammatory and antioxidant effects thereby can reduce SARS-CoV-2 infection-hyperinflammation and oxidative stress. Besides, PTX improves RBCs deformability and reduces blood viscosity so can mitigate Covid-19-induced hyper-viscosity and RBC hyper-aggregation which is linked with the development of coagulopathy. Taken together, PTX seems to be an effective agent against Covid-19 severity. Further preclinical and clinical studies are warranted to confirm these effects in this regard.
Author contributions
The authors equally participated in the development of the manuscript and provided their final approval of all content and submission for publication.
Funding
This work was funded by the Deanship of Scientific Research at Jouf University under grant No (DSR-2021-01-0376).
Data availability
Not applicable.
Declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical statement
This article does not contain any studies with human participants or animals performed by any of the authors.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Gomaa Mostafa-Hedeab, Email: Gomaa@ju.edu.sa.
Hayder M. Al-kuraishy, Email: Hayderm36@yahoo.com
Ali I. Al-Gareeb, Email: Dr.alialgareeb78@yahoo.com
Hebatallah M. Saad, Email: heba.magdy@mau.edu.eg
Gaber El-Saber Batiha, Email: gaberbatiha@gmail.com.
References
- Abdel-Salam OM, Baiuomy AR, El-Shenawy SM, Arbid MS. The anti-inflammatory effects of the phosphodiesterase inhibitor pentoxifylline in the rat. Pharmacol Res. 2003;47:331–340. doi: 10.1016/S1043-6618(03)00002-1. [DOI] [PubMed] [Google Scholar]
- Abdul Hadi ME, Hisham A. Pentoxifylline as a successful drug treatment for disseminated intravascular coagulopathy in Kassabach–Merrit syndrome. Sudan Med Monit. 2011;6(2):89–91. [Google Scholar]
- Abouelkhair MA. Targeting adenosinergic pathway and adenosine A2A receptor signaling for the treatment of COVID-19: a hypothesis. Med Hypotheses. 2020;144:110012. doi: 10.1016/j.mehy.2020.110012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Kuraishy HM, Al-Gareeb AI. Comparison of deferasirox and deferoxamine effects on iron overload and immunological changes in patients with blood transfusion-dependent β-thalassemia. Asian J Transfus Sci. 2017;11(1):13. doi: 10.4103/0973-6247.200768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Kuraishy HM, Al-Gareeb AI. Acute kidney injury and COVID-19. Egypt J Intern Med. 2021;33:1–5. doi: 10.1186/s43162-021-00064-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Kuraishy HM, Al-Gareeb AI, Hussien NR. Synergistic effect of berberine and pentoxifylline in attenuation of acute kidney injury. Int J Crit Illn Inj Sci. 2019;9:69. doi: 10.4103/IJCIIS.IJCIIS_85_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Kuraishy HM, Al-Gareeb AI, Al-Niemi MS, Al-Buhadily AK, Al-Harchan NA, Lugnier C. COVID-19 and phosphodiesterase enzyme type 5 inhibitors. J Microsc Ultrastruct. 2020;8(4):141. doi: 10.4103/JMAU.JMAU_63_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Kuraishy HM, Al-Gareeb AI, Alkazmi L, Alexiou A, Batiha GE. Levamisole therapy in COVID-19. Viral Immunol. 2021;34:722–725. doi: 10.1089/vim.2021.0042. [DOI] [PubMed] [Google Scholar]
- Al-Kuraishy HM, Al-Gareeb AI, Almulaiky YQ, Cruz-Martins N, Batiha GE. Role of leukotriene pathway and montelukast in pulmonary and extrapulmonary manifestations of Covid-19: the enigmatic entity. Eur J Pharmacol. 2021;15:174196. doi: 10.1016/j.ejphar.2021.174196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Kuraishy HM, Al-Gareeb AI, Alqarni M, Cruz-Martins N, El-Saber Batiha G. Pleiotropic effects of tetracyclines in the management of COVID-19: emerging perspectives. Front Pharmacol. 2021;12:136. doi: 10.3389/fphar642822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Kuraishy HM, Al-Gareeb AI, Alzahrani KJ, Alexiou A, Batiha GE. Niclosamide for Covid-19: bridging the gap. Mol Biol Rep. 2021;48:8195–8202. doi: 10.1007/s11033-021-06770-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Kuraishy HM, Al-Gareeb AI, Al-Hussaniy HA, Al-Harcan NA, Alexiou A, Batiha GE. Neutrophil extracellular traps (NETs) and Covid-19: a new frontiers for therapeutic modality. Int Immunopharmacol. 2022;104:108516. doi: 10.1016/j.intimp.2021.108516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Kuraishy HM, Al-Gareeb AI, Batiha GE. The possible role of ursolic acid in Covid-19: a real game changer. Clin Nutr ESPEN. 2022;47:414–417. doi: 10.1016/j.clnesp.2021.12.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Assimakopoulos SF, Seintis F, Marangos M. Pentoxifylline and complicated COVID-19: a pathophysiologically based treatment proposal. Med Hypotheses. 2020;143:109926. doi: 10.1016/j.mehy.2020.109926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azhar A, El-Bassossy HM. Pentoxifylline alleviates hypertension in metabolic syndrome: effect on low-grade inflammation and angiotensin system. J Endocrinol Investig. 2015;38(4):437–445. doi: 10.1007/s40618-014-0209-z. [DOI] [PubMed] [Google Scholar]
- Bayraktar S, Tanyeri-Bayraktar B. Pentoxifylline in the treatment of neonatal vasospasm and thromboembolism: an observational case series study. J Clin Pharm Ther. 2021 doi: 10.1111/jcpt.13565. [DOI] [PubMed] [Google Scholar]
- Brie D, Sahebkar A, Penson PE, Dinca M, Ursoniu S, Serban MC, Zanchetti A, Howard G, Ahmed A, Aronow WS, Muntner P. Effects of pentoxifylline on inflammatory markers and blood pressure: a systematic review and meta-analysis of randomized controlled trials. J Hypertens. 2016;34(12):2318–2329. doi: 10.1097/HJH.0000000000001086. [DOI] [PubMed] [Google Scholar]
- Byrnes JR, Wolberg AS. Red blood cells in thrombosis. Blood. 2017;130(16):1795–1799. doi: 10.1182/blood-2017-03-745349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandan N, Boen M, Lake EP, Aronson I. Successful treatment of two individual cases of generalized granuloma annulare with amoxicillin/clavulanic acid and a combination of doxycycline and pentoxifylline. Dermatol Online J. 2018;24:13030. doi: 10.5070/D3248041159. [DOI] [PubMed] [Google Scholar]
- Chavarría AP, Vázquez RR, Cherit JG, Bello HH, Suastegui HC, Moreno-Castañeda L, Estrada GA, Hernández F, González-Marcos O, Saucedo-Orozco H, Manzano-Pech L. Antioxidants and pentoxifylline as coadjuvant measures to standard therapy to improve prognosis of patients with pneumonia by COVID-19. Comput Struct Biotechnol J. 2021;19:1379–1390. doi: 10.1016/j.csbj.2021.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chehrei S, Moradi M, Ghiabi HR, Falahi M, Kaviani S, Ghanbari A. Pentoxifylline besides naltrexone recovers morphine-induced inflammation in male reproductive system of rats by regulating Toll-like receptor pathway. Andrologia. 2017;49(9):e12749. doi: 10.1111/and.12749. [DOI] [PubMed] [Google Scholar]
- Dávila-Esqueda ME, Martinez-Morales F. Pentoxifylline diminishes the oxidative damage to renal tissue induced by streptozotocin in the rat. Exp Diabetes Res. 2004;5(4):245–251. doi: 10.1080/154386090897974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Las Heras N, Martín Giménez VM, Ferder L, Manucha W, Lahera V. Implications of oxidative stress and potential role of mitochondrial dysfunction in COVID-19: therapeutic effects of vitamin D. Antioxidants. 2020;9(9):897. doi: 10.3390/antiox9090897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Oliveira Garcia FA, Rebouças JF, Balbino TQ, da Silva TG, de Carvalho-Júnior CH, Cerqueira GS, de Castro Brito GA, de Barros Viana GS. Pentoxifylline reduces the inflammatory process in diabetic rats: relationship with decreases of pro-inflammatory cytokines and inducible nitric oxide synthase. J Inflamm. 2015;12(1):1. doi: 10.1186/s12950-015-0080-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Sanctis MT, Cesarone MR, Belcaro G, Incandela L. Treatment of retinal vein thrombosis with pentoxifylline: a controlled, randomized trial. Angiology. 2002;53:S35. [PubMed] [Google Scholar]
- Deb B, Shah H, Goel S. Current global vaccine and drug efforts against COVID-19: pros and cons of bypassing animal trials. J Biosci. 2020;45(1):1. doi: 10.1007/s12038-020-00053-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delanian S, Porcher R, Rudant J, Lefaix JL. Kinetics of response to long-term treatment combining pentoxifylline and tocopherol in patients with superficial radiation-induced fibrosis. J Clin Oncol. 2005;23:8570–8579. doi: 10.1200/JCO.2005.02.4729. [DOI] [PubMed] [Google Scholar]
- Delgado-Roche L, Mesta F. Oxidative stress as key player in severe acute respiratory syndrome coronavirus (SARS-CoV) infection. Arch Med Res. 2020;51(5):384–387. doi: 10.1016/j.arcmed.2020.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dianey GC, Kaur H, Dosanjh HS, Narayanan J, Singh J, Yadav A, Kumar D, Luu SD, Sharma A, Singh PP, Alberto HA. Sunlight powered degradation of pentoxifylline Cs0.5Li0.5FeO2 as a green reusable photocatalyst: Mechanism, kinetics and toxicity studies. J Hazard Mater. 2021;416:125762. doi: 10.1016/j.jhazmat.2021.125762. [DOI] [PubMed] [Google Scholar]
- Dong J, Yuan X, Xie W. Pentoxifylline exerts anti-inflammatory effects on cerebral ischemia reperfusion-induced injury in a rat model via the p38 mitogen-activated protein kinase signaling pathway. Mol Med Rep. 2018;17:1141–1147. doi: 10.3892/mmr.2017.7953. [DOI] [PubMed] [Google Scholar]
- Effendi WI, Nagano T, Kobayashi K, Nishimura Y. Focusing on adenosine receptors as a potential targeted therapy in human diseases. Cells. 2020;9(3):785. doi: 10.3390/cells9030785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernandes JL, de Oliveira RT, Mamoni RL, Coelho OR, Nicolau JC, Blotta MH, Serrano CV., Jr Pentoxifylline reduces pro-inflammatory and increases anti-inflammatory activity in patients with coronary artery disease—a randomized placebo-controlled study. Atherosclerosis. 2008;196:434–442. doi: 10.1016/j.atherosclerosis.2006.11.032. [DOI] [PubMed] [Google Scholar]
- Frampton JE, Brogden RN. Pentoxifylline (oxpentifylline) Drugs Aging. 1995;7:480–503. doi: 10.2165/00002512-199507060-00007. [DOI] [PubMed] [Google Scholar]
- Freeman TL, Swartz TH. Targeting the NLRP3 inflammasome in severe COVID-19. Front Immunol. 2020;11:1518. doi: 10.3389/fimmu.2020.01518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia FA, Pinto SF, Cavalcante AF, Lucetti LT, Menezes SM, Felipe CF, Alves AP, Brito GA, Cerqueira GS, Viana GS. Pentoxifylline decreases glycemia levels and TNF-alpha, iNOS and COX-2 expressions in diabetic rat pancreas. Springerplus. 2014;3(1):1–1. doi: 10.1186/2193-1801-3-283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gomez-Mesa JE, Galindo-Coral S, Montes MC, Martin AJ. Thrombosis and coagulopathy in COVID-19. Curr Probl Cardiol. 2021;46(3):100742. doi: 10.1016/j.cpcardiol.2020.100742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- González-Amaro R, Portales-Pérez D, Baranda L, Redondo JM, Martínez-Martínez S, Yáñez-Mó M, García-Vicuña R, Cabañas C, Sánchez-Madrid F. Pentoxifylline inhibits adhesion and activation of human T lymphocytes. J Immunol. 1998;161:65–72. [PubMed] [Google Scholar]
- Guggilam A, Patel KP, Haque M, Ebenezer PJ, Kapusta DR, Francis J. Cytokine blockade attenuates sympathoexcitation in heart failure: cross-talk between nNOS, AT-1R and cytokines in the hypothalamic paraventricular nucleus. Eur J Heart Fail. 2008;10(7):625–634. doi: 10.1016/j.ejheart.2008.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hekmat M, Schaalan MF, Rahmo RM, Farag DB, Khedr LH. Implications of miRNAs on TGF-β/TAK1/mTOR pathway in mediating the renoprotective effects of pentoxifylline against cisplatin-induced nephrotoxicity in rats. Toxicol Appl Pharmacol. 2020;404:115184. doi: 10.1016/j.taap.2020.115184. [DOI] [PubMed] [Google Scholar]
- Hendry BM, Stafford N, Arnold AD, Sangwaiya A, Manglam V, Rosen SD, Arnold J. Hypothesis: pentoxifylline is a potential cytokine modulator therapeutic in COVID-19 patients. Pharmacol Res Perspect. 2020;8(4):e00631. doi: 10.1002/prp2.631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hepgül G, Tanrıkulu S, Ünalp HR, Akguner T, Erbil Y, Olgaç V, Ademoğlu E. Preventive effect of pentoxifylline on acute radiation damage via antioxidant and anti-inflammatory pathways. Dig Dis Sci. 2010;55(3):617–625. doi: 10.1007/s10620-009-0780-x. [DOI] [PubMed] [Google Scholar]
- Horvath B, Marton Z, Halmosi R, Alexy T, Szapary L, Vekasi J, Biro Z, Habon T, Kesmarky G, Toth K. In vitro antioxidant properties of pentoxifylline, piracetam, and vinpocetine. Clin Neuropharmacol. 2002;25(1):37–42. doi: 10.1097/00002826-200201000-00007. [DOI] [PubMed] [Google Scholar]
- Hosseini F, Mohammadbeigi A, Aghaali M, Borujerdi R, Parham M. Effect of pentoxifylline on diabetic distal polyneuropathy in type 2 diabetic patients: a randomized trial. J Res Med Sci. 2019;24:89. doi: 10.4103/jrms.JRMS_115_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussien NR, Al-Kuraishy HM, Al-Gareeb AI. Berberine and pentoxifylline: a novel combination in amelioration of acute kidney injury. J Pak Med Assoc. 2019;69(8):93–97. [PubMed] [Google Scholar]
- Ibrahim A, Gazzard L, Alharbi M, Rompré-Brodeur A, Aube M, Carrier S. Evaluation of oral pentoxifylline, colchicine, and penile traction for the management of Peyronie’s disease. Sex Med. 2019;7:459–463. doi: 10.1016/j.esxm.2019.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jafari-Sabet M, Shishegar A, Saeedi AR, Ghahari S. Pentoxifylline increases antiadhesion effect of streptokinase on postoperative adhesion formation: involvement of Fibrinolytic pathway. Indian J Surg. 2015;77(3):837–842. doi: 10.1007/s12262-013-1025-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ji Q, Zhang L, Jia H, Yang J, Xu J. Pentoxifylline inhibits endotoxin-induced NF-kappa B activation and associated production of proinflammatory cytokines. Ann Clin Lab Sci. 2004;34(4):427–436. [PubMed] [Google Scholar]
- Karam BS, Morris RS, Bramante CT, Puskarich M, Zolfaghari EJ, Lotfi-Emran S, Ingraham NE, Charles A, Odde DJ, Tignanelli CJ. mTOR inhibition in COVID-19: a commentary and review of efficacy in RNA viruses. J Med Virol. 2021;93(4):1843–1846. doi: 10.1002/jmv.26728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaur R, Kaur M, Singh J. Endothelial dysfunction and platelet hyperactivity in type 2 diabetes mellitus: molecular insights and therapeutic strategies. Cardiovasc Diabetol. 2018;17(1):1–7. doi: 10.1186/s12933-018-0763-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kolokythas A, Rasmussen JT, Reardon J, Feng C. Management of osteoradionecrosis of the jaws with pentoxifylline–tocopherol: a systematic review of the literature and meta-analysis. Int J Oral Maxillofac Surg. 2019;48:173–180. doi: 10.1016/j.ijom.2018.08.007. [DOI] [PubMed] [Google Scholar]
- Kubánková M, Hohberger B, Hoffmanns J, Fürst J, Herrmann M, Guck J, Kräter M. Physical phenotype of blood cells is altered in COVID-19. Biophys J. 2021;120(14):2838–2847. doi: 10.1016/j.bpj.2021.05.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lakdawala SS, Menachery VD. The search for a COVID-19 animal model. Science. 2020;368(6494):942–943. doi: 10.1126/science.abc6141. [DOI] [PubMed] [Google Scholar]
- Lan WC, Wang CY, Lin CD. Pentoxifylline versus steroid therapy for idiopathic sudden sensorineural hearing loss with diabetes. J Int Adv Otol. 2018;14:176. doi: 10.5152/iao.2018.4690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Law YX, Tai BC, Tan YQ, Lata RN, Lee KC. A small group randomized double-blind placebo-controlled study to evaluate the efficacy of daily pentoxifylline in the management of patients with erectile dysfunction with suboptimal treatment response to sildenafil. Sex Med. 2020;8:14–20. doi: 10.1016/j.esxm.2019.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levi M, ten Cate H, Bauer KA, van der Poll T, Edgington TS, Büller HR, Van Deventer SJ, Hack CE, ten Cate JW, Rosenberg RD. Inhibition of endotoxin-induced activation of coagulation and fibrinolysis by pentoxifylline or by a monoclonal anti-tissue factor antibody in chimpanzees. J Clin Investig. 1994;93(1):114–120. doi: 10.1172/JCI116934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopes RD, Macedo AV, Silva PG, Moll-Bernardes RJ, Dos Santos TM, Mazza L, Feldman A, Arruda GD, Denílson C, Camiletti AS, Sousa De. AS effect of discontinuing vs continuing angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers on days alive and out of the hospital in patients admitted with COVID-19: a randomized clinical trial. JAMA. 2021;325(3):254–264. doi: 10.1001/jama.2020.25864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maldonado V, Hernandez-Ramírez C, Oliva-Pérez EA, Sánchez-Martínez CO, Pimentel-González JF, Molina-Sánchez JR, Jiménez-Villalba YZ, Chávez-Alderete J, Loza-Mejía MA. Pentoxifylline decreases serum LDH levels and increases lymphocyte count in COVID-19 patients: results from an external pilot study. Int Immunopharmacol. 2021;90:107209. doi: 10.1016/j.intimp.2020.107209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcinkiewicz J, Grabowska A, Lauterbach R, Bobek M. Differential effects of pentoxifylline, a non-specific phosphodiesterase inhibitor, on the production of IL-10, IL-12 p40 and p35 subunits by murine peritoneal macrophages. Immunopharmacology. 2000;49(3):335–343. doi: 10.1016/S0162-3109(00)00249-6. [DOI] [PubMed] [Google Scholar]
- Marques LJ, Zheng L, Poulakis N, Guzman J, Costabel U. Pentoxifylline inhibits TNF-α production from human alveolar macrophages. Am J Respir Crit Care Med. 1999;159:508–511. doi: 10.1164/ajrccm.159.2.9804085. [DOI] [PubMed] [Google Scholar]
- Mayyas F, Alzoubi KH, Al-Taleb Z. An evaluation of the effect of pentoxifylline on blood pressure and myocardial oxidative status following intake of western diet. Clin Exp Hypertens. 2015;37(8):666–673. doi: 10.3109/10641963.2015.1047944. [DOI] [PubMed] [Google Scholar]
- Michetti C, Coimbra R, Hoyt DB, Loomis W, Junger W, Wolf P. Pentoxifylline reduces acute lung injury in chronic endotoxemia. J Surg Res. 2003;115(1):92–99. doi: 10.1016/S0022-4804(03)00219-1. [DOI] [PubMed] [Google Scholar]
- Mittal M, Siddiqui MR, Tran K, Reddy SP, Malik AB. Reactive oxygen species in inflammation and tissue injury. Antioxid Redox Signal. 2014;20(7):1126–1167. doi: 10.1089/ars.2012.5149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monji F, Siddiquee AA, Hashemian F. Can pentoxifylline and similar xanthine derivatives find a niche in COVID-19 therapeutic strategies? A ray of hope in the midst of the pandemic. Eur J Pharmacol. 2020;887:173561. doi: 10.1016/j.ejphar.2020.173561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myers MJ, Baarsch MJ, Murtaugh MP. Effects of pentoxifylline on inflammatory cytokine expression and acute pleuropneumonia in swine. Immunobiology. 2002;205(1):17–34. doi: 10.1078/0171-2985-00108. [DOI] [PubMed] [Google Scholar]
- Nader E, Nougier C, Boisson C, Poutrel S, Catella J, Martin F, Charvet J, Girard S, Havard-Guibert S, Martin M, Rezigue H. Increased blood viscosity and red blood cell aggregation in patients with COVID-19. Am J Hematol. 2021;97(3):283–292. doi: 10.1002/ajh.26440. [DOI] [PubMed] [Google Scholar]
- Navarro JF, Mora C, Muros M, García J. Additive antiproteinuric effect of pentoxifylline in patients with type 2 diabetes under angiotensin II receptor blockade: a short-term, randomized, controlled trial. J Am Soc Nephrol. 2005;16(7):2119–2126. doi: 10.1681/ASN.2005010001. [DOI] [PubMed] [Google Scholar]
- Navarro JF, Milena FJ, Mora C, León C, García J. Renal pro-inflammatory cytokine gene expression in diabetic nephropathy: effect of angiotensin-converting enzyme inhibition and pentoxifylline administration. Am J Nephrol. 2006;26(6):562–570. doi: 10.1159/000098004. [DOI] [PubMed] [Google Scholar]
- Noyan T, Önem Ö, Ramazan Şekeroğlu M, Köseoğlu B, Dülger H, Bayram İ, Sadık Yalçinkaya A, Bakan V. Effects of erythropoietin and pentoxifylline on the oxidant and antioxidant systems in the experimental short bowel syndrome. Cell Biochem Funct. 2003;21(1):49–54. doi: 10.1002/cbf.991. [DOI] [PubMed] [Google Scholar]
- Oliva A, Dotta A, Multigner L. Pentoxifylline and antioxidants improve sperm quality in male patients with varicocele. Fertil Steril. 2009;91(4):1536–1539. doi: 10.1016/j.fertnstert.2008.09.024. [DOI] [PubMed] [Google Scholar]
- Oliveira-Júnior IS, Brunialti MK, Koh IH, Junqueira VB, Salomão R. Effect of pentoxifylline on lung inflammation and gas exchange in a sepsis-induced acute lung injury model. Braz J Med Biol Res. 2006;39(11):1455–1463. doi: 10.1590/S0100-879X2006001100009. [DOI] [PubMed] [Google Scholar]
- Onohuean H, Al-Kuraishy HM, Al-Gareeb AI, Qusti S, Alshammari EM, Batiha GE. Covid-19 and development of heart failure: mystery and truth. Naunyn Schmiedebergs Arch Pharmacol. 2021;394:2013–2021. doi: 10.1007/s00210-021-02147-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ozden MG, Koksal G, Oz H. Comparison of antithrombin iii and pentoxifylline treatments in gram negative sepsis patients developing disseminated intravascular coagulation. Medeni Med J. 2019;34(3):233. doi: 10.5222/MMJ.2019.05935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ozturk H, Cetinkaya A, Firat TS, Tekce BK, Duzcu SE, Ozturk H. Protective effect of pentoxifylline on oxidative renal cell injury associated with renal crystal formation in a hyperoxaluric rat model. Urolithiasis. 2019;47(5):415–424. doi: 10.1007/s00240-018-1072-8. [DOI] [PubMed] [Google Scholar]
- Park SJ, Choi SH, Cho YD, Kim JY, Cho HJ, Lim CS, Kim KH, Kim WY. Pentoxifylline restores T Cell viability in hyper-inflammatory conditions. Res Sq. 2020 doi: 10.21203/rs.3.rs-131764/v1. [DOI] [Google Scholar]
- Pawlik MT, Schreyer AG, Ittner KP, Selig C, Gruber M, Feuerbach S, Taeger K. Early treatment with pentoxifylline reduces lung injury induced by acid aspiration in rats. Chest. 2005;127(2):613–621. doi: 10.1378/chest.127.2.613. [DOI] [PubMed] [Google Scholar]
- Perricone C, Triggianese P, Bartoloni E, Cafaro G, Bonifacio AF, Bursi R, Perricone R, Gerli R. The anti-viral facet of anti-rheumatic drugs: lessons from COVID-19. J Autoimmun. 2020;111:102468. doi: 10.1016/j.jaut.2020.102468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters-Golden M, Canetti C, Mancuso P, Coffey MJ. Leukotrienes: underappreciated mediators of innate immune responses. J Immunol. 2005;174(2):589–594. doi: 10.4049/jimmunol.174.2.589. [DOI] [PubMed] [Google Scholar]
- Rasyid A, Harris S, Nurhayati E, Prihartono J. Pentoxifylline in acute ischemic stroke patients with blood hyperviscosity. Int J Appl Pharm. 2018;10:307–310. doi: 10.22159/ijap.2018.v10s1.68. [DOI] [Google Scholar]
- Satapathy SK, Garg S, Chauhan R, Sakhuja P, Malhotra V, Sharma BC, Sarin SK. Beneficial effects of tumor necrosis factor-α inhibition by pentoxifylline on clinical, biochemical, and metabolic parameters of patients with nonalcoholic steatohepatitis. Am J Gastroenterol. 2004;99(10):1946–1952. doi: 10.1111/j.1572-0241.2004.40220.x. [DOI] [PubMed] [Google Scholar]
- Sebastian L, Desai A, Madhusudana SN, Ravi V. Pentoxifylline inhibits replication of Japanese encephalitis virus: a comparative study with ribavirin. Int J Antimicrob Agents. 2009;33(2):168–173. doi: 10.1016/j.ijantimicag.2008.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seyit M, Avci E, Nar R, Senol H, Yilmaz A, Ozen M, Oskay A, Aybek H. Neutrophil to lymphocyte ratio, lymphocyte to monocyte ratio and platelet to lymphocyte ratio to predict the severity of COVID-19. Am J Emerg Med. 2021;40:110–114. doi: 10.1016/j.ajem.2020.11.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sfera A, Osorio C, Jafri N, Diaz EL, Campo Maldonado JE. Intoxication with endogenous angiotensin II: a COVID-19 hypothesis. Front Immunol. 2020;11:1472. doi: 10.3389/fimmu.2020.01472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma A, Tate M, Mathew G, Vince JE, Ritchie RH, De Haan JB. Oxidative stress and NLRP3-inflammasome activity as significant drivers of diabetic cardiovascular complications: therapeutic implications. Front Physiol. 2018;9:114. doi: 10.3389/fphys.2018.00114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi X, Appiah-Kubi K. Platelet-derived growth factors (PDGFs) are key players in the stimulation of airway smooth muscle cells (ASMCs) alteration in asthma and chronic obstructive pulmonary disease (COPD) with multifarious inhibitors at an early stage of development. Curr Proteom. 2020;17(4):324–332. doi: 10.2174/1570164617666190906151348. [DOI] [Google Scholar]
- Smith JA, Nunnari G, Preuss M, Pomerantz RJ, Daniel R. Pentoxifylline suppresses transduction by HIV-1-based vectors. Intervirology. 2007;50(5):377–386. doi: 10.1159/000109752. [DOI] [PubMed] [Google Scholar]
- Suh YJ, Hong H, Ohana M, Bompard F, Revel MP, Valle C, Gervaise A, Poissy J, Susen S, Hékimian G, Artifoni M. Pulmonary embolism and deep vein thrombosis in COVID-19: a systematic review and meta-analysis. Radiology. 2021;298(2):E70–80. doi: 10.1148/radiol.2020203557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sunil VR, Vayas KN, Cervelli JA, Malaviya R, Hall L, Massa CB, Gow AJ, Laskin JD, Laskin DL. Pentoxifylline attenuates nitrogen mustard-induced acute lung injury, oxidative stress and inflammation. Exp Mol Pathol. 2014;97(1):89–98. doi: 10.1016/j.yexmp.2014.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tao X, Peng Y, Yang Y. Effect of pentoxifylline on the expression level of TNF-α induced by respiratory syncytial virus-infected human alveolar macrophages. J Clin Intern Med. 2001;03:190–191. [Google Scholar]
- Taus F, Salvagno G, Canè S, Fava C, Mazzaferri F, Carrara E, Petrova V, Barouni RM, Dima F, Dalbeni A, Romano S. Platelets promote thromboinflammation in SARS-CoV-2 pneumonia. Arterioscler Thromb Vasc Biol. 2020;40(12):2975–2989. doi: 10.1161/ATVBAHA.120.315175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Timchenko TV, Pogorely VE, Voronkov AV, Markova OM, Shcherbakova LI, Kompantsev VA, Medvetsky AI, Platonova AY. Experimental study of anti-thrombotic activity of pentoxyfillin microparticles: based on poly-dl-lactide-co-glycolide in comparison with pentoxyfillin. Фapмaция и Фapмaкoлoгия. 2019;7(2):97–104. [Google Scholar]
- Tong Z, Dai H, Chen B, Abdoh Z, Guzman J, Costabel U. Inhibition of cytokine release from alveolar macrophages in pulmonary sarcoidosis by pentoxifylline: comparison with dexamethasone. Chest. 2003;124:1526–1532. doi: 10.1378/chest.124.4.1526. [DOI] [PubMed] [Google Scholar]
- Wan Y, Shang J, Graham R, Baric RS, Li F. Receptor recognition by the novel coronavirus from Wuhan: an analysis based on decade-long structural studies of SARS coronavirus. J Virol. 2020;94(7):e00127–e220. doi: 10.1128/JVI.00127-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang LC, Yao HW, Chang CF, Wang SW, Wang SM, Chen SH. Suppression of interleukin-6 increases enterovirus A71 lethality in mice. J Biomed Sci. 2017;24(1):1–9. doi: 10.1186/s12929-017-0401-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitfield K, Rambaldi A, Wetterslev J, Gluud C. Pentoxifylline for alcoholic hepatitis. Cochrane Database Syst Rev. 2009;2009(4):CD007339. doi: 10.1002/14651858.CD007339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wikipedia (2014) Pentoxifylline. http://en.wikipedia.org/wiki/Pentoxifylline. Accessed 1 Mar 2022
- Xiong Y, Sun D, Liu Y, Fan Y, Zhao L, Li X, Zhu W. Clinical and high-resolution CT features of the COVID-19 infection: comparison of the initial and follow-up changes. Investig Radiol. 2020;55(6):332–339. doi: 10.1097/RLI.0000000000000674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang M, Xu YJ, Mengi SA, Arneja AS, Dhalla NS. Therapeutic potentials of pentoxifylline for treatment of cardiovascular diseases. Exp Clin Cardiol. 2004;9(2):103. [PMC free article] [PubMed] [Google Scholar]
- Zhang X, Meng F, Song J, Zhang L, Wang J, Li D, Li L, Dong P, Yang B, Chen Y. Pentoxifylline ameliorates cardiac fibrosis, pathological hypertrophy, and cardiac dysfunction in angiotensin II-induced hypertensive rats. J Cardiovasc Pharmacol. 2016;67(1):76–85. doi: 10.1097/FJC.0000000000000316. [DOI] [PubMed] [Google Scholar]
- Zhao W, Ma L, Cai C, Gong X. Caffeine inhibits NLRP3 inflammasome activation by suppressing MAPK/NF-κB and A2aR signaling in LPS-Induced THP-1 macrophages. Int J Biol Sci. 2019;15(8):1571. doi: 10.7150/ijbs.34211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng J, Wong LY, Li K, Verma AK, Ortiz ME, Wohlford-Lenane C, Leidinger MR, Knudson CM, Meyerholz DK, McCray PB, Perlman S. COVID-19 treatments and pathogenesis including anosmia in K18-hACE2 mice. Nature. 2021;589(7843):603–607. doi: 10.1038/s41586-020-2943-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.