Abstract
Abdominal aortic aneurysm (AAA) is a potentially life-threatening disorder with a mostly asymptomatic course where the abdominal aorta is weakened and bulged. Cytokines play especially important roles (both positive and negative) among the molecular actors of AAA development. All the inflammatory cascades, extracellular matrix degradation and vascular smooth muscle cell apoptosis are driven by cytokines. Previous studies emphasize an altered expression and a changed epigenetic regulation of key cytokines in AAA tissue samples. Such cytokines as IL-6, IL-10, IL-12, IL-17, IL-33, IL-1β, TGF-β, TNF-α, IFN-γ, and CXCL10 seem to be crucial in AAA pathogenesis. Some data obtained in animal studies show a protective function of IL-10, IL-33, and canonical TGF-β signaling, as well as a dual role of IL-4, IFN-γ and CXCL10, while TNF-α, IL-1β, IL-6, IL-12/IL-23, IL-17, CCR2, CXCR2, CXCR4 and the TGF-β noncanonical pathway are believed to aggravate the disease. Altogether data highlight significance of cytokines as informative markers and predictors of AAA. Pathologic serum/plasma concentrations of IL-1β, IL-2, IL-6, TNF-α, IL-10, IL-8, IL-17, IFN-γ, and PDGF have been already found in AAA patients. Some of the changes correlate with the size of aneurysms. Moreover, the risk of AAA is associated with polymorphic variants of genes encoding cytokines and their receptors: CCR2 (rs1799864), CCR5 (Delta-32), IL6 (rs1800796 and rs1800795), IL6R (rs12133641), IL10 (rs1800896), TGFB1 (rs1800469), TGFBR1 (rs1626340), TGFBR2 (rs1036095, rs4522809, rs1078985), and TNFA (rs1800629). Finally, 5 single-nucleotide polymorphisms in gene coding latent TGF-β-binding protein (LTBP4) and an allelic variant of TGFB3 are related to a significantly slower AAA annual growth rate.
Keywords: Aneurysm, AAA, cytokines, inflammation, TGF-β, IL-6
Introduction
Aortic aneurysm (AA) is a life-threatening disorder caused by an irreversible local enlargement of the aorta with high risk of rupture and consequent fatal bleeding. Unfortunately, the AA is usually an unpredictable finding due to its latent clinical course. In most cases, it is detected during a non-routine medical exam. 1 The AA are most commonly seen in the thoracic (thoracic aorta aneurysm, TAA) and abdominal (abdominal aorta aneurysm, AAA) aorta. 2 Despite their apparent similarity, AAA and TAA have different etiologies and underlying mechanisms. The more prevalent, AAA, is strongly associated with male sex, elderly age, dyslipidemia, increased blood pressure, and presence of atherosclerosis. In contrast, no evident correlations are found between the TAA progression and age, sex, or other cardiovascular diseases but it involves a major genetic component and association with connective tissue disorders. 3
The hallmarks of AAA are an aortic wall inflammation accompanied by a leukocytic infiltration and a degradation of the extracellular matrix (ECM), 4 meanwhile TAA is caused by a connective tissue component degradation. Also, the TAA features are a loss of vascular smooth muscle cells (VSMCs), a fragmentation and decrease in the number of elastic fibers, and an increased accumulation of proteoglycans.5-7
Thoracic and abdominal segments of the aorta have different embryological origins, and it is considered to be the most important cause for the pathogenetic differences between TAA and AAA. 8 The thoracic segment is composed of smooth muscle cells (SMCs) migrating from the neural crest, whereas the abdominal segment contains only primitive SMCs contributing to its formation. 9 This fact determines different responses of the segments to such destructive factors as high concentrations of homocysteine, angiotensin II (AngII), or transforming growth factor β (TGF-β) (more details in Ruddy et al). 10
In this review, we focus on the importance of various cytokines in AAA pathogenesis describing their predictive value and probable therapeutic application.
Cytokines are Key Regulators of AAA Development
Cytokines are crucial contributors of inflammatory alterations throughout the AAA course. Early stages of AAA are driven by an infiltration of the vascular wall by immune cells producing inflammatory factors. In subsequent stages, the increased production of cytokines leads to the activation of proteases and apoptosis of VSMCs resulting in ECM degradation and aortic wall thinning.11,12 Finally, the rupture, which is a severe outcome of AA, also depends on cytokines upregulation. 13
Dramatic shift of cytokine expression was revealed in the murine model of Angiotensin-II-(AngII)-induced AAA. An assay of cytokines in AAA tissue samples from AngII-treated ApoE−/−mice has been conducted with an antibody array of 200 cytokines, cytokine receptors, and related proteins; it has revealed that 21 of these 200 proteins are differentially expressed. These differentially expressed proteins are mostly associated with such functions as leukocytic migration and positive regulation of cell adhesion. 14
Presumably, AAA is characterized by overexpression and activation of proinflammatory transcription factors leading to upregulation of certain cytokines and enhancement of downstream cellular responses.15-17 Schönbeck et al has demonstrated that extracts of human AAA tissue predominantly contain T helper 2 (Th2)-associated cytokines and less abundant Th1-associated cytokines, whereas Th1-associated cytokines are found at higher concentrations in stenotic atherosclerotic vascular lesions.15,18
A number of studies on human samples highlight differential expression of cytokines in aneurysm tissue of AAA patients (Table 1).
Table 1.
Differential expression of cytokines and cytokine receptors in aortic samples collected from patients with AAA.
| Level | Study description | Upregulated cytokines | Downregulated cytokines | Reference |
|---|---|---|---|---|
| Protein | A 42-cytokine antibody-based protein array analysis of samples collected from 10 AAA patients and 9 non-AAA controls | IL-6, IL-1α, IL-1β, TNF-α, TNF-β, oncostatin M, IL-10, IL-8, ENA-78, GROα, MCP-1, MCP-2, RANTES, G-CSF, M-CSF | - | Middleton et al 19 |
| Protein | A 274-cytokine antibody-based protein array analysis of homogenized human aortic tissues from 12 AAA patients and 6 non-AAA controls | MCP-1, RANTES, MDC, PARC, MIP-1b, PF4, GROα, IL-8, IL-6, LIGHT, GDF15, EGF, TIMP-1, TNFSF5 | MCP-2, PDGF-AA, BMP-4, bFGF, EGFR | Yuwen et al 20 |
| Protein | Fifty-two cytokines (from human AAA tissue samples from 4 patients) analyzed in a fluorescent-bead-based multiplex assay | IL-6, MIF, LIF, IFN-γ, MCP-1, IL-8, MIG, IP-10, GROα, HGF, VEGF | - | Ohno et al 21 |
| Protein | ELISAs of IL-8 and MCP-1 in cell cultures derived from AAA and non-AAA patients | MCP-1, IL-8 | - | Koch et al 22 |
| Protein | ELISA of IL-1β in aortic biopsies from 15 AAA patients and 6 non-AAA patients | IL-1β | - | Pearce et al 23 |
| Protein | ELISAs of TNF-α and IL-1β in aortic-tissue extracts from 7 AAA patients and 5 non-AAA patients | TNF-α, IL-1β | - | Newman et al 24 |
| Protein | ELISAs of TNF-α, IL-6, and IL-8 in aortic tissue of 11 ruptured aneurysms and 32 asymptomatic aneurysms | TNF-α, IL-6, IL-8 | - | Treska et al 25 |
| Protein | Measurement of the IL-10 level in the aortic tissue of 8 AAAs and 8 tissue samples affected by aortoiliac occlusive disease (AOD) by immunoenzyme assays | IL-10 | - | Davis et al 26 |
| mRNA | Membrane-based complementary DNA expression array of total RNA (converted to cDNA) isolated from 4 AAAs and 4 normal abdominal aortic wall tissue samples | IL-8, CXCR4, PDGF-A, RANTES | - | Tung et al 27 |
| mRNA | Analysis of differential gene expression using a cDNA human cell interaction array of 265 genes | TNF-βR | - | Armstrong et al 28 |
Abbreviations: bFGF, basic fibroblast growth factor 2; BMP-4, bone morphogenetic protein 4; CXCR4 (fusin), C-X-C chemokine receptor type 4; EGF, epidermal growth factor; EGFR, EGF receptor; ENA-78 (CXCL5), epithelial neutrophil-activating peptide-78 (C-X-C motif chemokine 5); G-CSF (CSF3), granulocyte colony-stimulating factor (colony-stimulating factor 3); GDF15 (MIC-1), growth/differentiation factor 15 (macrophage inhibitory cytokine 1); GROα (CXCL1), growth-regulated protein alpha (C-X-C motif chemokine 1); HGF, hepatocyte growth factor; IFN-γ, interferon gamma; IL, interleukin; IP-10 (CXCL10), interferon γ-induced protein 10 (C-X-C motif chemokine 10); LIF, leukemia inhibitory factor; LIGHT (TNFSF14), tumor necrosis factor ligand superfamily member 14; M-CSF (CSF1), macrophage colony-stimulating factor (colony stimulating factor 1); MCP-1 (CCL2), monocyte chemoattractant protein 1 (C-C motif chemokine 2); MCP-2 (CCL8), monocyte chemoattractant protein 2 (C-C motif chemokine 8); MDC (CCL22), macrophage-derived chemokine (C-C motif chemokine 22); MIF, macrophage migration inhibitory factor; MIG (CXCL9), monokine induced by γ-interferon (C-X-C motif chemokine 9); MIP-1b (CCL4), macrophage inflammatory protein-1-beta (C-C motif chemokine 4); PARC (CCL18), pulmonary and activation-regulated chemokine (C-C motif chemokine 18); PDGF-A, platelet-derived growth factor A; PDGF-AA, platelet-derived growth factor alpha polypeptide; PF4 (CXCL4), platelet factor 4 (C-X-C motif chemokine 4); RANTES (CCL5), regulated upon activation, normal T-cell expressed and secreted (C-C motif chemokine 5); TIMP-1, tissue inhibitor of metallopeptidase 1 (metallopeptidase inhibitor 1); TNF, tumor necrosis factor; TNF-βR, tumor necrosis factor-β receptor; TNFSF5 (CD40-L), tumor necrosis factor ligand superfamily member 5 (CD40 ligand).
IL-6
IL-6 is a pleiotropic proinflammatory cytokine responsible for initiation of acute phase response. 29 Once IL-6 is secreted to the bloodstream from an altered region, systemic inflammatory response arises. 30 Numerous preclinical and clinical studies have uncovered a pathological role of high and dysregulated IL-6 expression in the development of inflammatory, autoimmune, and oncological diseases in humans. 31
To initiate a signaling cascade, IL-6 binds to a heterodimeric complex consisting of membrane IL-6 receptor (mIL-6R) and a subunit of gp130. 32 Only a few cells express mIL-6R, while almost all cells have gp130 on their surface. Cells synthesizing gp130 without mIL-6R do not interact with IL-6 but are able to respond to an IL-6 complex containing the soluble form of IL-6R (sIL-6R), which is generated by proteolytic cleavage of mIL-6R. This process has been termed trans-signaling. In contrast, to proinflammatory functions of IL-6 trans-signaling, IL-6 classic signaling mediates regenerative and anti-inflammatory activities.32,33
IL-6 takes part in the pathogenesis of various cardiovascular diseases. In particular, in patients with AAA, there is an increased level of circulating IL-6, which may correlate with the aorta diameter.34-36 Moreover, Yuwen et al revealed that IL-6 is expressed within an AAA in patients but is undetectable in the corresponding tissue of a control group. 20 The concentration of IL-6 in an AA-affected aortic wall is severalfold higher than the concentration of IL-6 in progressive atherosclerotic stenotic lesions of the aorta, suggesting that IL-6 is a proinflammatory factor associated with dilatation rather than stenosis. 37 According to Nishihara et al, inhibition of sIL-6R by a monoclonal antibody reduces the aorta diameter in the murine model of CaCl2-induced AAA. 38 Paige et al showed that the prevention of AAA progression and of aorta rupture is achieved only via selective blockade of the trans-pathway of IL-6 signaling, whereas inhibition of both pathways (trans- and classic) does not correlate with improved survival. 39
Jones et al reported that the 174C→G polymorphism in the IL6 gene is associated with the worst survival among AAA patients and a higher level of IL-6 in blood plasma. 40 Another interesting finding of this study is that the aneurysm wall appears to be an important source of circulating IL-6. Smallwood et al presented an association between the IL-6-572G>C polymorphism in the promoter region of the IL6R gene encoding IL-6 receptor and the risk of AAA. 41 Moreover, while studying VSMCs isolated from patients with AAA and controls, Boddy et al found altered DNA methylation in IL6R. 42
IgG4-associated diseases are recently described systemic disorders affecting various tissues, including the aorta (IgG4-AA: IgG4-associated aortic aneurysm). IgG4-AA is a consequence of tissue infiltration by plasma cells that produce IgG4. 43 Patients with this pathology have strikingly elevated levels of IL-6 in the tissue of the affected blood vessel and in peripheral blood. 44 In IgG4-AA, serum concentration of IL-6 correlates with higher IgG4 levels, which may perform an important function in the pathogenesis and progression of this disease. Numerous cell populations, including the endothelium, mesenchymal cells, and macrophages in the adventitia, promote IL-6 overexpression in IgG4-AA. IL-6 may be a useful biomarker of disease activity, and inhibition of IL-6 may serve as a new effective avenue for treatment of IgG4-AA. 45
In addition, recent studies showed an association between elevated IL-6 levels and poor postoperative prognosis. A surgical intervention is necessary if an aneurysm is large or ruptured. This operation entails prolonged clamping of the vessel, thus contributing to ischemia. Splanchnic ischemia, a well-known complication of aortic surgery, triggers the synthesis of proinflammatory cytokines, the most important of which is IL-6. Elevated levels of this cytokine during this pathology and after the surgical operation cause serious systemic adverse reactions in various organs/tissues, especially the lungs, kidneys, and myocardium, thereby resulting in multiple organ dysfunction syndrome. 46
IL-12
The IL-12 family is a group of heterodimeric cytokines that includes IL-12, IL-23, IL-27, and IL-35. 47 IL-12 is produced by activated antigen-presenting cells, especially macrophages, and consists of subunits p35 and p40. IL-12 has an influence on hematopoiesis and is required for T-cell-dependent immune and inflammatory responses, regulation of cytokine synthesis by (and proliferation of) T and natural killer (NK) cells, and differentiation of T cells.48,49 IL-12 and IL-23 control differentiation into (and proliferation of) Th1 and Th17 cells, respectively. 50 IL-23 is produced predominantly by macrophages and dendritic cells and activates memory T cells. IL-23 contains 2 subunits: p40 (just as IL-12 does) and p19 (which is absent in IL-12). 48 The impact of IL-12 on cells is mediated by a receptor complex consisting of IL-12Rβ1 and IL-12Rβ2. The receptor of IL-23 is composed of IL-12Rβ1 and IL-23R. Stimulation by IL-12 and IL-23 triggers receptor-associated Janus kinases (JAKs) and phosphorylation of STAT proteins in target cells. Janus tyrosine kinase Tyk binds to IL-12Rβ1, while JAK binds to IL-23R as well as IL-12Rβ2. 51
IL-12 is a potent proinflammatory cytokine that is detectable at elevated concentrations in patients with AAA. 52 In a murine model of AngII-dependent AAA, IL12p40 deficiency increases TGF-β2 and IL-10 expression and reduces the inflammatory response. IL12p40-deficient mice have a predominantly anti-inflammatory profile, and such animals are protected from many inflammatory and immune-system-mediated conditions.53,54 Yan et al demonstrated that in a murine model of elastase-induced AAA, administration of neutralizing monoclonal antibodies against IL-12 and IL-23 attenuates the development of AAA. Furthermore, IL12p40 inhibition significantly reduced macrophage expansion and suppressed the production of several macrophage-related inflammatory mediators, including IL-6, TNF-α, and matrix metalloproteinase 9 (MMP-9). 55
IL-17
IL-17A, the founding member cytokine of the IL-17 family, was cloned in 1993 and was originally named cytotoxic T lymphocyte-associated antigen 8. 56 The production of IL-17A is regulated by the transcription factor RORγt.57-59 Th17 cell and its secretory IL-17 have been repeatedly shown to be involved in the induction of tissue inflammation in autoimmune diseases such as rheumatoid arthritis, psoriasis, and multiple sclerosis.60,61
IL-17 has also been found as a crucial regulator of inflammation and apoptosis in AAA. In various experimental models of AAA, a decrease in the IL-17 level helps to weaken or prevent aneurysm development. For instance, anti-IL-17 activity was found as crucial for AAA attenuation mediated by cardiac glycosides digoxin and its derivatives. Normally cardiac glycosides are being prescribed to attenuate heart failure because of their ability to restore calcium imbalance in cardiomyocytes. According to Huh et al, digoxin and its derivatives can also inhibit Th17 differentiation and IL-17A production via selective antagonism of the RORγt transcription factor. Wei et al also reported that digoxin arrests the progression of experimental AAA by suppressing differentiation into Th17 cells and IL-17A expression.58,59 In the model of elastase-induced AAA, treatment with mesenchymal stem cells causes inhibition of IL-17A attenuated aneurysm progression and reduced the levels of other inflammatory cytokines. 62 Furthermore, in a model of AngII-induced AAA and aortic dissection, 2 weeks of treatment with an anti-IL-17A antibody reduced aortic dilatation and prevented aneurysm dissection. 63 Clinical research with 476 AAA patients and 200 controls shows a positive correlation between plasma levels of IL-17A and cross-sectional AAA area. 64
TGF-β
The family of TGF-β, including 3 isoforms (TGF-β1, TGF-β2, and TGF-β3), represents bifunctional regulators that either inhibit or stimulate cell proliferation. TGF-β was originally isolated as a cytokine that, together with EGF, induces cell transformation and growth of selected fibroblast cell lines. 65 Later, it was proven that TGF-β can either stimulate or inhibit cell proliferation, depending on the experimental conditions. 66 Research into the mechanisms underlying aneurysm and aortic dissection have shed light on the importance of TGF-β activity for the maintenance of aortic-wall integrity.
There are 2 TGF-β signaling pathways, and both play an important part in aneurysm formation. In the canonical pathway, TGF-β binds to its type I or type II receptor on the cell surface. The resultant complex phosphorylates SMAD2 (mothers against decapentaplegic homolog 2) or SMAD3, thus leading to heterotrimerization with SMAD4, their nuclear translocation, and SMAD-dependent gene transcription. 67 In the noncanonical pathway, TGF-β launches RhoA and mitogen-activated protein kinase cascades, the latter of which includes extracellular signal-regulated kinase (ERK), N-terminal Jun kinase (JNK), and p38. TGF-β activates them, thereby causing their phosphorylation to p-ERK, p-JNK, and p-p38, respectively. 68 TGF-β takes part in the pathogenesis of AAA and TAA. In AAA, TGF-β controls key processes including ECM remodeling, survival and proliferation of VSMCs, and initiation of the immune/inflammatory response. 69
Several connective tissue disorders highlight the role of TGF-β in AAA. For instance, unbalanced TGF-β signaling is recognized as one of the key factors in the pathogenesis of Marfan syndrome, a disease usually complicated by AA formation. 70 Normally, TGF-β signaling is limited by fibrillin 1. 71 Because the gene encoding fibrillin 1 (FBN1) is mutated in Marfan syndrome, TGF-β signaling is enhanced resulting in increased secretion of MMPs. Moreover, Loeys–Dietz syndrome, another Mendelian disease clinically overlapping with Marfan syndrome, is caused by a mutation in TGF-βR1 (TGF-β receptor 1), TGF-βR2, TGF-β1, or TGF-β3 or in downstream effectors of the TGF-β pathway: SMAD2 or SMAD3.72-75
According to Holm et al, SMAD-independent TGF-β signaling is implicated in the pathogenesis of AA in mice with Marfan syndrome. In their study, selective inhibition of ERK1/2 in the noncanonical TGF-β pathway slowed the progression of AA, whereas in SMAD4-deficient mice (canonical pathway), exacerbation of AA and earlier death of the mice were observed. 76 Zhang et al also demonstrated that depletion of SMAD4 in VSMCs leads to inflammation in the aortic wall, suggesting SMAD4-dependent TGF-β signaling in VSMCs protects from AA formation and dissection. 77
In a murine model of elastase-induced AAA, inhibition of TGF-β activity promotes progression of aortic dilatation via reduction of SMAD2/3 phosphorylation. 78 In a model of AngII-induced AA, inhibition of TGF-β increases dilatation and accelerates the rupture of AAA and TAA. 2 According to Angelov et al, systemic blockade of TGF-β (neutralization by an antibody) aggravates the AAA course, whereas genetic inactivation of TGF-β specifically in VSMCs significantly accelerates TAA development in combination with the spread of intramural hematomas, thinning of the media, and thickening of the adventitia. 79 Dai et al reported that overexpression of TGF-β1 in a pre-existing AAA by endovascular gene therapy helps to stabilize the vessel diameter, to preserve elastin, to decrease the infiltration by monocytes-macrophages and T lymphocytes, and to reduce the amounts of MMP-2 and MMP-9. The research showed, that in parallel with the suppression of the destructive process, the TGF-β1 overexpression triggered endoluminal reconstruction, replacing the thrombus with vascular smooth muscle and an intima rich in collagen and elastin. 80
Thompson et al found that 5 SNPs in LTBP4 and an allelic variant of TGFB3 are associated with a significant decrease in AAA growth in a UK cohort. They demonstrated altered growth in carriers of 2 common haplotypes of LTBP4 and a single haplotype of TGFB3. 81
Thus, certain mechanisms underlying the impact of TGF-β on the development of AAA are not clear enough. Possibly, the canonical TGF-β signaling pathway prevents AA progression via SMAD4-dependent up-regulation of expression of VSMC-specific gene markers resulting in acceleration of proliferation and migration of VSMCs as well as increased production of collagen. In a similar way, during atherosclerotic vascular lesions, the canonical TGF-β pathway promotes restenosis of the arteries, enhancing the proliferation of neointimal cells and the accumulation of collagen. 82
For example, in atherosclerotic vascular lesions, this pathway promotes restenosis of the arteries, enhancing the proliferation of neointimal cells and the accumulation of collagen.
IL-10
IL-10 is a major pleiotropic immunoregulatory cytokine that plays a key role in the alleviation of allergic and inflammatory diseases. 83 IL-10 is produced by both innate- and adaptive-immunity cells, including dendritic cells, macrophages, mast cells, NK cells, eosinophils, neutrophils, B cells, regulatory T cells, and Th1, Th2, and Th17 lymphocytes. 84 IL-10 prevents the secretion of inflammatory cytokines and regulates the differentiation and proliferation of T cells, B cells, NK cells, mast cells, granulocytes, dendritic cells, keratinocytes, and endothelial cells. 85
There is evidence that the immunoregulatory properties of IL-10 may be involved in AA development because the IL-10-1082 “A” polymorphism (associated with lower IL-10 production) is more common in patients with AAA, and patients with this polymorphism are at a higher risk of AAA. Plasma IL-10 concentrations are significantly lower in patients with AAA than in comparable patients with stenotic aortic atherosclerotic lesions. Besides, in a model of AngII-induced AAA, genetic or pharmacological depletion of IL-10 increases the susceptibility to aneurysm formation and rupture.12,86,87
IL-10 reduces inflammation in aneurysm tissue, thereby contributing to the proliferation and phenotypic transformation of VSMCs, inhibiting degradation of VSMCs and rupture of elastic fibers, and delaying aneurysm development in a rabbit model of elastase-induced AAA. 88
Vucevic et al found a negative correlation between IL-6 and IL-10 expression levels in aortic samples derived from AAA patients. On the basis of this finding, they subdivided the AAAs into 2 cytokine-producing groups and showed that tissue samples in the IL-6high/IL-10low group contained higher percentages of granulocytes, HLA-DR+ cells, and CD68+ cells but lower percentages of lymphocytes and plasma cells as compared to the IL-6low/IL-10high group. 89
IFN-γ
IFN-γ (originally called macrophage activating factor) is a key player in driving cellular immunity, 90 produced mainly by CD4+ T cells. 91 Cellular responses to IFN-γ are initiated by its interaction with a heterodimeric receptor consisting of interferon gamma receptor 1 and 2. 92 Downstream effects of IFN-γ include macrophage activation, synthesis of MMPs and cysteine proteinases and inhibition of chemokines that attract cells to inflammatory sites.93,94
The inflammatory infiltrate of AAA is mainly composed of macrophages expressing MMP-12 and of T lymphocytes, which are the main producers of IFN-γ. The participation of IFN-γ in AAA pathogenesis has been proven by numerous research; for example, Schönbeck et al reported elevated levels of IFN-γ in AAA tissues, 18 and serum of AAA patients. 34
Nonetheless, the role of IFN-γ in the development of AAA is dual: evidently, this cytokine promotes either proinflammatory or anti-inflammatory processes, depending on the disease stage, the model of AAA, and other unknown factors. According to King et al, IFN-γ and its effector chemokine CXCL10 attenuate AAA development, whereas deficiencies of both IFN-γ and CXCL10 in mice induce AAA formation. The opposite effects of the IFN-γ deficiency between AAA and aortic stenosis can be explained by the localization of these processes in different tissue layers of the vessel and by the accumulation of various types of inflammatory cells and cytokines in the affected tissue. 95 Shimizu et al also demonstrated that the IFN-γ signaling blockade observed in IFN-γ receptor-null mice enhances AAA formation after aortic allograft transplantation. 96
In contrast, increased concentrations of IFN-γ accelerate the AAA growth rate, and the serum concentration of IFN-γ directly correlates with aneurysm progression according to Juvonen et al 34 In addition, Xiong et al showed the crucial role of IFN-γ secreted by CD4+ T-cells. In this study, CD4 deficient mice were resistant to AAA formation only before restoration of IFN-γ levels. 97 Similar data were presented by Kuivaniemi et al: CD4−/− mice with decreased IFN-γ expression were resistant to the induction of AAA. 98
Presumably, IFN-γ promotes AAA formation possibly via stimulating MMP synthesis, but later, in the already formed AA, IFN-γ attenuates the progression of the pathology. Nevertheless, further research have to shed light on this cytokine in the focus of AAA.
TNF-α and IL-1β
Both TNF-α and IL-1 are key proinflammatory cytokines of innate-immune-response initiation, mediating the recruitment, activation, and adhesion of circulating phagocytic cells and terminating the innate immune response. 99
Kaneko et al reported increased expression of TNF-α converting enzyme (Tace) in human AAA samples as compared with normal aorta, suggesting up-regulation of TNF-α in aneurysm tissue. Moreover, temporal systemic deletion of Tace in mice with periaortic application of CaCl2 resulted in decrease of AAA size and attenuation of extracellular matrix disruption and aortic wall inflammation. 100
Xiong et al revealed that genetic or pharmacological blockade of TNF-α resulted in resistance to aneurysm formation in CaCl2-induced AAA murine model. TNF-α deficiency also attenuated matrix MMP 2 and MMP-9 expression as well as macrophage infiltration into the aortic tissue. In addition, Food and Drug Administration-approved TNF-α antagonist, infliximab, was shown to inhibit aneurysm growth. 101
In a study on 7 AAA tissue samples and 5 control aortic-tissue samples, TNF-α proved to be upregulated significantly in the AAA extracts; IL-1β concentration was also significantly higher in the AAA tissue samples. 24
Study on 34 subjects with AAA and 34 matched non-AAA controls revealed significantly increased IL-1α and IL-1β plasma levels in AAA patients. Moreover, peripheral blood mononuclear cells derived from male patients with AAA were found to express significantly higher mRNA levels of IL1B compared with control group. 102 In a model of AngII-induced AAA, inhibition of IL-1β by an antibody (01BSUR) inhibits the formation of AAA. 103 Johnston et al revealed significant protection against elastase-induced AAA formation in mice with genetic deletion of IL-1β or IL-1R. 104 Similarly, according to Meher et al, IL-1β-knockout mice demonstrated significantly lower infiltration of neutrophils to aorta and were protected from AAA. Moreover, this protection was abolished by adoptive transfer of wild-type neutrophils. 105
In a model of β-aminopropionitrile-induced dissecting AA, Jiang et al found dramatic upregulation of IL-1β in aortic samples but not in the bloodstream. The study also revealed that IL-1β can locally participate in AAA formation via the activation of MMP-2 and MMP-9 and via degradation of elastin fibers because these alterations ultimately weaken biomechanical properties of the aortic wall. 106
In contrast, Hingorani et al revealed that only TNF-α, but not IL-1 inhibition was able to completely block elastase-induced dilatation in a rat model of AAA. 107 A similar finding was reported by Batra et al, only TNF-α exerted an AAA-aggravating impact. Genetic deletion of IL-1β and IL-1R did not inhibit aneurysm formation. Moreover, IL-1R–/– mice developed larger aneurysms than did their wild-type controls. 108 Thus, both TNF-α and IL-1β are important factors for AAA progression but, apparently, depending on particular pathological conditions their role can be displayed differently.
Recently, B cell-activating factor (BAFF, BLyS, or TALL-1), a member of TNF family cytokines, was identified as a factor contributing to AAA formation. In a murine model of AAA, the level of lesion was decreased by the injection of BAFF antagonists both before and after the model induction. BAFF is a critical survival factor for mature B cells, supporting their differentiation as well as antibody class switching, and antibody secretion, that could explain its promoting role in the AAA development as a pro-inflammatory cytokine. 109
IL-4
IL-4 is a signature cytokine of type 2 immune response and crucial regulator of atopic diseases. 110
In a study by Shimizu et al, murine aortic allografts transplanted into IFN-γ–deficient hosts manifested severe AAA formation, which was prevented by an anti-IL-4 antibody. 96 Liu et al revealed a protective function of eosinophil-secreted IL-4 in clinical observations and murine studies. Their results showed that eosinophil deficiency exacerbates the growth of AngII perfusion-induced AAA in Apoe−/− and eosinophil-deficient Apoe−/−ΔdblGATA mice. They concluded that eosinophils exert a protective action against AAA by releasing IL-4 and cationic proteins such as mEar1 to regulate macrophage and monocyte polarization and to block NF-κB (nuclear factor kappa-light-chain-enhancer of activated B cells) activation in aortic inflammatory and vascular cells. 111
IL-32
IL-32 is a cytokine inducing crucial inflammatory cytokines such as TNFα and IL-6 and its expression is elevated in various inflammatory and viral infectious diseases. 112 According to Bengts et al, the expression of proinflammatory cytokine IL-32 is significantly higher in AAA tissue samples than in control groups. Furthermore, IL-32 turned out to be predominantly expressed in VSMCs and T-cell-rich regions. The highest level of IL-32 mRNA was observed in the intima/media layer of AAA. However, there were no differences observed in the plasma levels of IL-32 between the control and experimental group. 113
IL-33
IL-33 is a tissue-derived nuclear cytokine from the IL-1 family abundantly expressed in endothelial cells, epithelial cells and fibroblast-like cells, both during homeostasis and inflammation. 114 Daily intraperitoneal administration of recombinant IL-33 or transgene IL-33 overexpression ameliorated periaortic CaPO4 injury-induced and aortic elastase exposure-induced AAA in mice, as evidenced by reduced aortic reorganization, leukocytes infiltration and connective tissue degradation as well as lower apoptosis in the lesion. 115
Chemokine family
Chemokines are a family of small secreted peptide cytokines regulating various cell functions, first of all, immune-cell recruitment. They are known to play essential roles in a number of pathological conditions, including inflammation, atherosclerosis, altered hematopoiesis, and cancer. C-X-C motif chemokine ligand 12 (CXCL12, also referred to as SDF-1: stromal cell-derived factor 1) is a homeostatic CXC chemokine that possesses 7 isoforms and binds to CXCR4 and CXCR7 (C-X-C chemokine receptors type 4 and type 7). 116
Using 32 aneurysm sac specimens from AAA patients and 12 matching nonaneurysmal aortic samples from transplant donors, Tanios et al revealed increased mRNA and protein expression of CXCR4 and CXCL12 in the AAA tissue samples. The mRNA expression of CXCR4 and CXCL12 was 9.6- and 4.6-fold higher in AAA than in nonaneurysmal aorta samples (P = .0004 and P < .0001, respectively). Likewise, the protein level of CXCR4 was 3.2-fold higher in the AAA wall than in the nonaneurysmal aortic tissue (P < .0001), although CXCL12 could not be detected. 117
Michineau et al revealed increased levels of CXCR4 mRNA in both the human AAA wall and the mouse aortic wall affected by CaCl2-induced AAA. Furthermore, in murine AAA model, CXCR4 blockade by AMD3100 decreased the infiltration by adventitial macrophages, inhibited aneurysm formation, and prevented aortic-wall destruction by reducing the mRNA levels of MMP-12, MMP-14, MCP-1, MIP-1β, MIP-2α, RANTES, IL-1β, IL-6, TNF-α, and E-selectin. 118
Finally, pharmacological inhibition of CXCR2119,120 and genetic depletion of CCR2 121 markedly reduced AngII-induced AAA formation in ApoE−/− mice.
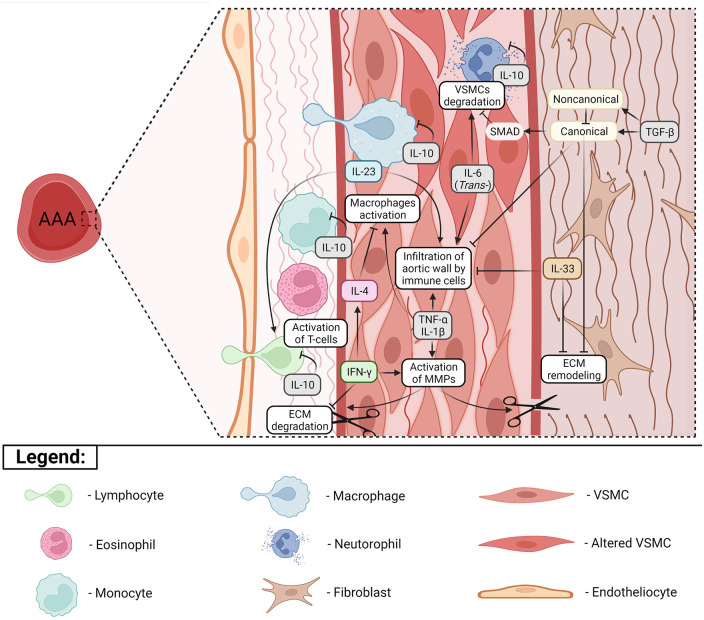
Current highlights of the role of listed cytokines in AAA progression are presented in Figure 1.
Figure 1.
Contribution of several key cytokines in AAA formation. Aneurysmal damage of abdominal aorta is primarily driven by infiltration of the aortic wall by immune cells, to fit: lymphocytes, monocytes, macrophages and neutrophils. Subsequent inflammatory activation leads to increased production of matrix metalloproteases (MMPs), which cause remodeling of extracellular matrix (ECM), disrupting connective tissue fibers. Most crucial regulators orchestrating accumulation of immune cells are TNF-α, IL-1β (via trans-signaling) and IL-6. These cytokines are not only able to attract different types of immune cells but they also may be produced by a wide range of cells, both immune and mesenchymal. The same inflammatory effect can also be mediated by IL-23 (mostly produced by macrophages), the cytokine which normally sends strong activating signals to T-lymphocytes. In contrast, IL-10 is a cytokine which prevents inflammatory activation, arising beneficial effects in AAA. One of regulators with a controversial role in AAA formation is IFN-γ. On the one hand this cytokine activates degradation of ECM, but on the other hand IFN-γ may prevent macrophages activation via facilitating the release of IL-4. Another 2-faced cytokine is TGF-β, which can mediate both positive effects such as decrease of vascular smooth muscle cells (VSMCs) apoptosis via canonical SMAD-dependent pathway and negative effects via non-canonical pathway. Color indicates the type of cell which produces cytokine (blue—macrophages, pink—eosinophil, green—lymphocyte, beige—fibroblast, gray—various types of cells).
Predictive Value of Cytokines
With all crucial involvement in the development of AAA cytokines might serve appropriate for diagnosis making and outcomes prediction. Herein we present a brief summary of research revealing predictive value of minimally invasive tests such as genotyping or biochemical analysis.
Polymorphisms of genes
Unlike TAA, AAA has no major genetic component. Nevertheless, Table 2 presents 13 polymorphisms significantly associated with the risk of AAA.
Table 2.
Associations between polymorphisms in genes encoding cytokines and the risk or severity of AAA.
| Gene | SNP/loci | Reference | Population/Country | Cases/ controls | Methods | Risk allele | OR (p-value) | Main conclusions |
|---|---|---|---|---|---|---|---|---|
| CCR2 | V64I (rs1799864) | Katrancioglu et al 122 | Turkey | 100 patients with AAA and 138 individuals with normal aortic diameter | Polymerase chain reaction restriction fragment length polymorphism (PCR-RFLP) | I | 2.31 (0.01) | Significant relationship between CCR2 V64I polymorphism (OR: 2.31, 95% CI: 1.19-4.46, P = .01) and presence of AAA in multivariate regression analysis |
| IL6 | IL-6-572G>C (rs1800796) | Smallwood et al 41 | Australia | 677 men with screen-detected AAAs and 656 age-matched controls | TaqMan-based PCR | C | 5.78 (0.031) | Polymorphism is associated with AAA |
| -174G/C (rs1800795) | Jabłońska et al 123 | Austria | 104 patients with AAA and 112 healthy volunteers | PCR-RFLP | C | 2.15 (0.015) | Polymorphism is associated with increased risk of AAA | |
| IL6R | rs12133641 | Jones et al 40 | 104 830 European (U.S., Australia, Iceland, The Netherlands, U.K., New Zealand) | 4972 European-ancestry cases, 99 858 European-ancestry controls. Replication: 2482 European-ancestry cases, 2750 cases, 2645 European-ancestry controls, 5263 controls | Genome-wide genotyping array (Affymetrix, Illumina) | А | 1.14 (5 × 10−13) | Polymorphism is associated with increased risk of AAA |
| IL10 | IL-10-1082 (rs1800896) | Bown et al 124 | USA | 389 patients with AAA and 404 healthy controls | Kompetitive allele-specific PCR (KASP) | A | 1.50 (0.014) | “A” allele of IL-10 -1082G/A is significantly associated with AAA |
| Bown et al 125 | UK | 100 patients with AAA and 100 age-matched and sex-matched control subjects | Induced heteroduplex genotyping | A | 1.8 (0.03) | “A” allele of IL-10 -1082G/A is significantly associated with AAA (OR = 1.8; 95% CI = 0.9-3.6; P = .03). | ||
| Wang et al 86 | China | 381 cases and 381 controls | PCR-RFLP | A | 1.34 (0.04) | “A” allele of IL-10-1082G/A is significantly associated with AAA | ||
| TGFB1 | rs1800469 | Zuo et al 126 | China | 155 cases and 310 controls | Typer 4.0 software (Mass ARRAY Compact System; Sequenom, San Diego, CA, USA). | T | 1.35 (0.03) | rs1800469-T (in TGFB1) is associated with increased risk of AAA in Chinese population |
| TGFBR1 | rs1626340 | Baas et al 127 | Dutch | 736 cases and 1024 controls | GoldenGate assay on Illumina BeadStation 500 GX (Illumina Inc., San Diego, CA, USA) with TaqMan Assays on Demand (Applied Biosystems, Foster City, CA, USA) | A | 1.32 (0.001) | rs1626340 (in TGFBR1) correlates with AAA risk in Dutch population |
| TGFBR2 | rs1036095 | Baas et al 127 | Dutch | 736 cases and 1024 controls | GoldenGate assay on Illumina BeadStation 500 GX (Illumina) with Taqman Assays on Demand (Applied Biosystems) | C | 1.32 (0.001) | rs1036095 and rs4522809 (in TGFBR2) are associated with increased AAA risk in Dutch population |
| rs4522809 | A | 1.28 (0.0004) | ||||||
| g.42917C>T (rs1078985) | Golledge et al 128 | New Zealand | 1043 subjects from New Zealand, of whom 654 had an AAA | Illumina Golden Gate assay on a BeadLab System (Illumina) | C | 0.64 (0.020) | rs1078985 (in TGFBR2) is weakly associated with AAA among healthy male subjects according to a codominant model. In a recessive genetic model, the minor allele homozygote (CC) is associated with reduced prevalence of AAA (OR: 0.64 (95% CI: 0.45-0.93); P = .020) | |
| TNFA | TNF-α 308G/A (rs1800629) | Jabłońska et al 123 | Austria | 104 patients with AAA and 112 healthy volunteers | PCR-RFLP | A | 1.97 (0.02) | TNF-α-238G/A gene polymorphism is associated with increased risk of AAA |
| SMAD2 * | c.C833T, p.A278V (NM_001003652.3/ENST00000402690) | Zhang et al 129 | China | 1 case | Exome sequencing and Sanger sequencing | Novel missense mutation (c.833CNT, p.A278V) in the SMAD2 gene is the causal variant of familial AAA | ||
| CCR5 | Delta-32 polymorphism | Ghilardi et al 130 | Italy | 70 patients with AAA and 172 healthy controls | PCR | Δ Δ 32 | 2.7 (0.002) | A genetic risk factor distinguishes AAA from arterial occlusive disease in humans: CCR5 Delta 32 deletion |
Does not belong to the cytokine superfamily but is directly involved in TGF-β signaling.
Serum and plasma levels of cytokines
Measurement of blood serum/plasma cytokines’ concentrations is one of the sensitive assays for the detection of a number of diseases. Besides inflammatory processes, blood levels of cytokines can be influenced by aging, physical exercise, psychiatric disorders, cancer, obesity, pain, and other factors.131,132 The concentration levels of cytokines are usually measured in picograms per milliliter and can vary widely. For example, in healthy persons serum concentration of IL-10 varies from 0.01 to 19.8 pg/mL, while IFN-γ concentration from 0.14 to 126.8 pg/mL. 133 The Table 3 summarizes studies revealing changed blood levels of cytokines in AAA patients (Table 3).
Table 3.
Relation between AAA and plasma levels of various cytokines.
| Protein | Cohort | Type of sample | Phenotype/Predictive value | Reference |
|---|---|---|---|---|
| IL-1α | 101 AAA patients | Serum | • IL-1α, proinflammatory cytokine not normally detectable in the circulation was observed in the majority of patients with infrarenal AAA • No correlations with maximum AAA diameter and growth rate |
Ahmad et al 134 |
| 34 pairs of AAA patients and age/sex-matched non-AAA patients | Plasma | Significantly increased IL-1α plasma levels in AAA patients. | Wu et al 102 | |
| IL-1β | 86 AAA patients/30 non-AAA subjects | Plasma | Increased plasma levels in AAA patients (P < .05) | Treska et al 135 |
| 345 patients with AAA and 30 healthy volunteers | Plasma | Increased plasmatic concentrations in AAA patients (P < .001) | Treska et al 136 | |
| 9 samples from AAA patients and 15 samples from non-AAA patients | Plasma | IL-1β was not detectable in the plasma of AAA patients (n = 9) but was detectable in most samples (7/10) in the control group (n = 10) | Batra et al 108 | |
| 34 pairs of AAA patients and age/sex-matched non-AAA patients | Plasma | Significantly increased IL-1β plasma levels in AAA patients. | Wu et al 102 | |
| IL-2 | 86 AAA patients/30 non-AAA subjects | Plasma | Increased plasma levels in AAA patients (P < .05) | Treska et al 135 |
| 345 patients with AAA and 30 healthy volunteers | Plasma | Increased plasma concentrations in AAA patients (P < .001) | Treska et al 136 | |
| IL-6 | 86 AAA patients/30 non-AAA subjects | Plasma | Increased plasma levels in AAA patients (P < .05) | Treska et al 135 |
| 120 non-AAA outpatients | Serum | Positive correlation of IL-6 serum levels with aortic diameter (P < .01) | Rohde et al 36 | |
| 90 AAA patients | Plasma | IL-6 levels were increased with increasing AAA diameter and symptoms however not reaching significant correlation | Treska et al 137 | |
| 27 AAA patients and 15 non-AAA subjects | Plasma | • Higher plasma levels in AAA patients • Positive correlation between AAA surface area and mean plasma IL-6 concentration |
Dawson et al 138 | |
| 360 AAA patients and 219 healthy subjects | Plasma | • Significantly (P < .0001) increased plasma levels in AAA patients • Significant difference in plasma levels between patients with different AAA sizes (P = .0002) |
Flondell-Sité et al 139 | |
| 345 patients with AAA and 30 healthy volunteers | Plasma | Increased plasma concentrations in AAA patients (P < .001) | Treska et al 136 | |
| 476 AAA patients and 200 non-AAA controls | Plasma | Reduced level in AAA patients | Liao et al 64 | |
| IL-8 | 86 AAA patients/30 non-AAA subjects | Plasma | • Significant difference in plasma levels in relation to the size of AAA (P < .05) • Correlation of plasma levels with the size of the AAA in hypertonic patients (p < .05) |
Treska et al 135 |
| 90 AAA patients | Plasma | IL-8 levels (P < .05) showed a statistically significant correlation with the diameter of AAA | Treska et al 137 | |
| 345 patients with AAA and 30 healthy volunteers | Plasma | Significant correlation with AAA diameter (P < .05) | Treska et al 136 | |
| IL-10 | 476 AAA patients and 200 non-AAA controls | Plasma | • Reduced plasma levels in AAA patients, P < .001 • Significant protective factor against human AAA with OR 0.91 (P = .011) • Positive correlation with maximal annual AAA growth rate (P = .036) |
Liao et al 64 |
| IL-17A | 476 AAA patients and 200 non-AAA controls | Plasma | • Reduced plasma levels in AAA patients, P < .001 (P = .028) • Positive correlation with maximal cross-sectional AAA area (P = .044) |
Liao et al 64 |
| IFN-γ | 476 AAA patients and 200 non-AAA controls | Plasma | • Significantly lower plasma IFN-γ levels in AAA patients (P = .021) • Significant protective factor against human AAA with OR at 0.91 (P = .044) • Positive correlation with maximal cross-sectional AAA area (P = .009) |
Liao et al 64 |
| TNF-α | 86 AAA patients/30 non-AAA subjects | Plasma | • Increased plasma levels in AAA patients (P < .05) • Correlation of plasma levels with AAA size in hypertonic patients (P < .01) |
Treska et al 135 |
| 90 AAA patients | Plasma | • Increased plasma levels in AAA patients (P < .0001) • Negative correlation between plasma levels of TNF-α and symptoms of AAA (P < .05) |
Treska et al 137 | |
| 360 AAA patients and 219 healthy subjects | Plasma | Significantly higher plasma levels in AAA patients (P < .0001) | Flondell-Sité et al 139 | |
| 345 patients with AAA and 30 healthy volunteers | Plasma | Significantly lower concentrations in symptomatic patients with AAA rupture (P < .05). | Treska et al 136 | |
| PDGF | 86 AAAs/30 non-AAA samples | Plasma | Increased plasma levels in AAA (P < .05) | Treska et al 135 |
Prospects of This Research Field
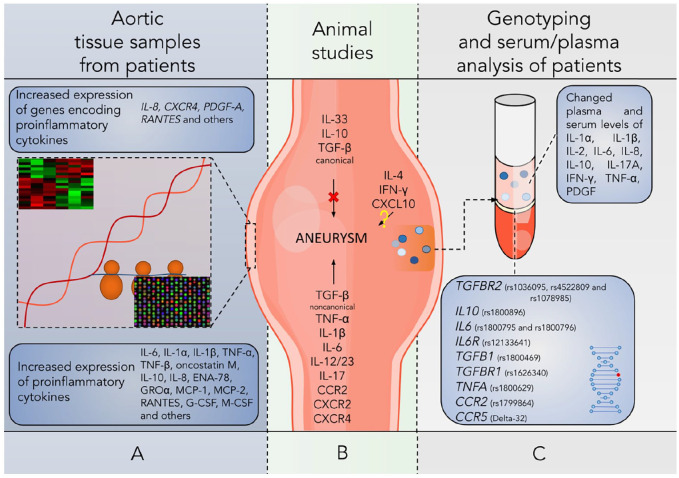
Nowadays, there is no effective pharmacotherapy of AAA that can mitigate the disease course and prevent ruptures. Therefore, a search for drug targets is obviously crucial in further studies. Cytokines are key participants in the regulation of AAA development (Figure 2), therefore managing their effects may become an appropriate step to alleviate the damage to the aortic wall. For instance, Bernal et al showed that therapy based on suppressor of cytokine signaling 1 (SOCS1) inhibits a common signaling pathway (JAK/STAT) of inflammatory cytokines, thus hindering AAA development in a murine model, as evidenced by limited aortic expansion and elastin degradation, preservation of VSMCs in the media, and reduced leukocytic infiltration. 140
Figure 2.
Summary representation of current data revealing implication of different cytokines in AAA. (A) Aneurysm samples collected from patients are characterized by expression of pro-inflammatory cytokines on the transcriptome and protein levels. (B) Study on mice show that pharmacological or genetic blockade of L-10, IL-33, and canonical TGF-β signaling aggravate AAA course, whereas inhibition of TNF-α, IL-1β, IL-6, IL-12/IL-23, IL-17, CCR2, CXCR2, CXCR4 and the TGF-β noncanonical pathway attenuate the disease. At the same time, animal studies show controversial role of IL-4, IFN-γ and CXCL10. (C) Population genetics studies revealed that carriers of particular mutations of genes CCR2 (rs1799864), CCR5 (Delta-32), IL6 (rs1800796 and rs1800795), IL6R (rs12133641), IL10 (rs1800896), TGFB1 (rs1800469), TGFBR1 (rs1626340), TGFBR2 (rs1036095, rs4522809, rs1078985), and TNFA (rs1800629) have increased risk of AAA development.
Noteworthy, detection of changed concentrations of cytokine do not clarify if it plays positive or negative role as levels of molecular participant can be imbalanced due to both adaptive or aggravating mechanisms. In fact, only effects of down- or upregulation of different cytokines pathways using pharmacological or genetic tools in experimental models of AAA can shed light on its role in the disease progression.
The pharmacological and genetic studies on AAA have confirmed by now the causative role of increased TNF-α, IL-1β, IL-6, IL-12/IL-23, IL-17, CCR2, CXCR2, CXCR4, and the TGF-β (non-canonical pathway) signaling as well as protective functions of IL-10, IL-33, and canonical TGF-β signaling. The effects of IFN-γ, CXCL10 and IL-4 on AAA are ambiguous and require further research (Figure 2B). In this way, we may consider that regarding these cytokines as drug targets is challenging for AAA treatment, thus the issue needs further investigation.
It is extremely relevant to look for new ways to predict the onset and course of AA, especially because of its high clinical significance and a long asymptomatic period in many patients. For instance, Blumel et al offer a simple and elegant “thumb palm test” to reveal the ascending AA (a variant of TAA) with a high level of specificity. 141 Thanks to the literature review, we guess that a quantitative assessment of some cytokines may have certain diagnostic value in the AAA. Although, the cytokines use is seriously limited there, as their concentrations are able to change significantly even in the blood of generally healthy persons but also in a wide range of comorbidities. A possible solution is a search of appropriate integrative indicators and coefficients based on the ratio of various cytokines’ levels in AAA. This approach is already successfully applied in clinical practice when analyzing numerous biochemical parameters, namely the fibrinogen-to-albumin ratio as a new clinical marker of microinflammation 142 ; the CRP/albumin ratio as an independent prognostic marker in different types of cancer, 143 and as a scoring system for determining the stage and activity of an inflammatory disease 142 ; the De Ritis (AST/ALT) ratio for the diagnosis and prognosis making in liver diseases, myocardial infarction, acute ischemic stroke, peripheral artery disease, and kidney injury 144 ;the blood urea nitrogen-to-creatinine ratio as an independent prognostic indicator of poor outcomes in various diseases, such as heart failure, kidney injury, and stroke 145 ; finally, the atherogenic index of plasma (a logarithm of the ratio between plasma triglyceride and high density lipoprotein cholesterol levels) as a sensitive marker of the risk to develop atherosclerosis and cardiovascular disease. 146 Identifying highly sensitive and specific relations between cytokines in the context of AAA seems to be an appropriate approach to create various test systems and diagnostic panels. This strategy undoubtedly requires additional research.
Conclusion
Despite cytokines being key regulators of AAA progression, the certain mechanisms underlying their contribution have yet to be clarified. However, existing data opens up novel directions for the prevention and therapy of AAA and related disorders. One may also observe especially promising results revealing diagnostic and predictive value of cytokines for AAA patients. Obviously, further studies in this research field might bring some breakthroughs for prolongation of lifespan in persons struggling with AAA.
Footnotes
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the State Assignment (Laboratory of Genetic Technologies and Genome Editing for Biomedicine and Veterinary of Belgorod State National Research University).
Declaration Of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author Contributions: OAP—literature analysis, drafting the article, editing. VOS—main idea, conceptualization, drafting the article, critical revision of the content, editing. AEB—main idea, drafting the article, editing, graphical design. OYB—collection and analysis of data related to population genetics studies, editing. GAP, AAV, AVD, MVK, MVP, NKS—drafting the article, editing, references formalization. All authors read and approved the manuscript.
Statement on Ethics: Ethical approval and informed consent were not required for the review.
ORCID iDs: Andrei E Belykh  https://orcid.org/0000-0001-9766-2104
https://orcid.org/0000-0001-9766-2104
Gennadii A Piavchenko  https://orcid.org/0000-0001-7782-3468
https://orcid.org/0000-0001-7782-3468
Artem A Venediktov  https://orcid.org/0000-0002-5604-0461
https://orcid.org/0000-0002-5604-0461
Nikolay K Shakhpazyan  https://orcid.org/0000-0003-3386-7746
https://orcid.org/0000-0003-3386-7746
References
- 1. Kim HW, Stansfield BK. Genetic and epigenetic regulation of aortic aneurysms. Biomed Res Int. 2017;2017:7268521-7268612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Chen X, Rateri DL, Howatt DA, et al. TGF-β neutralization enhances AngII-Induced aortic rupture and aneurysm in both thoracic and abdominal regions. PLoS One. 2016;11:e0153811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Clift PF, Cervi E. A review of thoracic aortic aneurysm disease. Echo Res Pract. 2020;7:R1-R10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Lindberg S, Zarrouk M, Holst J, Gottsäter A. Inflammatory markers associated with abdominal aortic aneurysm. Eur Cytokine Netw. 2016;27:75-80. [DOI] [PubMed] [Google Scholar]
- 5. Lu H, Rateri D, Bruemmer D, Cassis L, Daugherty A. Involvement of the renin–angiotensin system in abdominal and thoracic aortic aneurysms. Clin Sci. 2012;123:531-543. [DOI] [PubMed] [Google Scholar]
- 6. Guo DC, Papke CL, He R, Milewicz DM. Pathogenesis of thoracic and abdominal aortic aneurysms. Ann N Y Acad Sci. 2006;1085:339-352. [DOI] [PubMed] [Google Scholar]
- 7. Goldfinger JZ, Halperin JL, Marin ML, Stewart AS, Eagle KA, Fuster V. Thoracic aortic aneurysm and dissection. J Am Coll Cardiol. 2014;64:1725-1739. [DOI] [PubMed] [Google Scholar]
- 8. Wiegreffe C, Christ B, Huang R, Scaal M. Remodeling of aortic smooth muscle during avian embryonic development. Dev Dyn. 2009;238:624-631. [DOI] [PubMed] [Google Scholar]
- 9. Kuivaniemi H, Ryer EJ, Elmore JR, Tromp G. Understanding the pathogenesis of abdominal aortic aneurysms. Expert Rev Cardiovasc Ther. 2015;13:975-987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ruddy JM, Jones JA, Ikonomidis JS. Pathophysiology of thoracic aortic aneurysm (TAA): is it not one uniform aorta? Role of embryologic origin. Prog Cardiovasc Dis. 2013;56:68-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Sakalihasan N, Limet R, Defawe O. Abdominal aortic aneurysm. Lancet. 2005;365:1577-1589. [DOI] [PubMed] [Google Scholar]
- 12. Adam M, Kooreman NG, Jagger A, et al. Systemic upregulation of IL-10 (Interleukin-10) using a nonimmunogenic vector reduces growth and rate of dissecting abdominal aortic aneurysm. Arterioscler Thromb Vasc Biol. 2018;38:1796-1805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Choke E, Thompson MM, Dawson J, et al. Abdominal aortic aneurysm rupture is associated with increased medial neovascularization and overexpression of proangiogenic cytokines. Arterioscler Thromb Vasc Biol. 2006;26:2077-2082. [DOI] [PubMed] [Google Scholar]
- 14. Li Y, Yang D, Sun B, et al. Discovery of crucial cytokines associated with abdominal aortic aneurysm formation by protein array analysis. Exp Biol Med. 2019;244:1648-1657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Lindeman J, Abdul-Hussien H, Schaapherder A, et al. Enhanced expression and activation of pro-inflammatory transcription factors distinguish aneurysmal from atherosclerotic aorta: IL-6- and IL-8-dominated inflammatory responses prevail in the human aneurysm. Clin Sci. 2008;114:687-697. [DOI] [PubMed] [Google Scholar]
- 16. Luo YW, Zhao Z, Li FN, Zhang J. The effect pathways analysis in the abdominal aortic aneurysms. Eur Rev Med Pharmacol Sci. 2013;17:1245-1251. [PubMed] [Google Scholar]
- 17. Golledge ALV, Walker P, Norman PE, Golledge J. A systematic review of studies examining inflammation associated cytokines in human abdominal aortic aneurysm samples. Dis Markers. 2009;26:181-188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Schönbeck U, Sukhova GK, Gerdes N, Libby P. T(H)2 predominant immune responses prevail in human abdominal aortic aneurysm. Am J Pathol. 2002;161:499-506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Middleton RK, Lloyd GM, Bown MJ, Cooper NJ, London NJ, Sayers RD. The pro-inflammatory and chemotactic cytokine microenvironment of the abdominal aortic aneurysm wall: a protein array study. J Vasc Surg. 2007;45:574-580. [DOI] [PubMed] [Google Scholar]
- 20. Yuwen L, Ciqiu Y, Yi S, et al. A pilot study of protein microarray for simultaneous analysis of 274 cytokines between abdominal aortic aneurysm and normal aorta. Angiology. 2019;70:830-837. [DOI] [PubMed] [Google Scholar]
- 21. Ohno T, Aoki H, Ohno S, et al. Cytokine profile of human abdominal aortic aneurysm: involvement of JAK/STAT Pathway. Ann Vasc Dis. 2018;11:84-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Koch AE, Kunkel SL, Pearce WH, et al. Enhanced production of the chemotactic cytokines interleukin-8 and monocyte chemoattractant protein-1 in human abdominal aortic aneurysms. Am J Pathol. 1993;142:1423-1431. [PMC free article] [PubMed] [Google Scholar]
- 23. Pearce WH, Sweis I, Yao JST, McCarthy WJ, Koch AE. Interleukin-1β and tumor necrosis factor-α release in normal and diseased human infrarenal aortas. J Vasc Surg. 1992;16:784-789. [PubMed] [Google Scholar]
- 24. Newman KM, Jean-Claude J, Li H, Ramey WG, Tilson MD. Cytokines that activate proteolysis are increased in abdominal aortic aneurysms. Circulation. 1994;90:II224-II227. [PubMed] [Google Scholar]
- 25. Treska V, Kocova J, Boudova L, et al. Inflammation in the wall of abdominal aortic aneurysm and its role in the symptomatology of aneurysm. Cytokines Cell Mol Ther. 2002;7:91-97. [DOI] [PubMed] [Google Scholar]
- 26. Davis VA, Persidskaia RN, Baca-Regen LM, Fiotti N, Halloran BG, Baxter BT. Cytokine pattern in aneurysmal and occlusive disease of the aorta. J Surg Res. 2001;101:152-156. [DOI] [PubMed] [Google Scholar]
- 27. Tung WS, Lee JK, Thompson RW. Simultaneous analysis of 1176 gene products in normal human aorta and abdominal aortic aneurysms using a membrane-based complementary DNA expression array. J Vasc Surg. 2001;34:143-150. [DOI] [PubMed] [Google Scholar]
- 28. Armstrong PJ, Johanning JM, Calton WC, et al. Differential gene expression in human abdominal aorta: aneurysmal versus occlusive disease. J Vasc Surg. 2002;35:346-414. [DOI] [PubMed] [Google Scholar]
- 29. Baumann H, Gauldie J. The acute phase response. Immunol Today. 1994;15:74-80. [DOI] [PubMed] [Google Scholar]
- 30. Heinrich PC, Castell JV, Andus T. Interleukin-6 and the acute phase response. Biochem J. 1990;265:621-636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Yao X, Huang J, Zhong H, et al. Targeting interleukin-6 in inflammatory autoimmune diseases and cancers. Pharmacol Ther. 2014;141:125-139. [DOI] [PubMed] [Google Scholar]
- 32. Rose-John S. The soluble interleukin 6 receptor: advanced therapeutic options in inflammation. Clin Pharmacol Ther. 2017;102:591-598. [DOI] [PubMed] [Google Scholar]
- 33. Scheller J, Chalaris A, Schmidt-Arras D, Rose-John S. The pro- and anti-inflammatory properties of the cytokine interleukin-6. Biochim Biophys Acta. 2011;1813:878-888. [DOI] [PubMed] [Google Scholar]
- 34. Juvonen J, Surcel HM, Satta J, et al. Elevated circulating levels of inflammatory cytokines in patients with abdominal aortic aneurysm. Arterioscler Thromb Vasc Biol. 1997;17:2843-2847. [DOI] [PubMed] [Google Scholar]
- 35. Jones KG, Brull DJ, Brown LC, et al. Interleukin-6 (IL-6) and the prognosis of abdominal aortic aneurysms. Circulation. 2001;103:2260-2265. [DOI] [PubMed] [Google Scholar]
- 36. Rohde LEP, Arroyo LH, Rifai N, et al. Plasma concentrations of interleukin-6 and abdominal aortic diameter among subjects without aortic dilatation. Arterioscler Thromb Vasc Biol. 1999;19:1695-1699. [DOI] [PubMed] [Google Scholar]
- 37. Kokje VBC, Gäbel G, Koole D, et al. IL-6: A Janus-like factor in abdominal aortic aneurysm disease. Atherosclerosis. 2016;251:139-146. [DOI] [PubMed] [Google Scholar]
- 38. Nishihara M, Aoki H, Ohno S, et al. The role of IL-6 in pathogenesis of abdominal aortic aneurysm in mice. PLoS One. 2017;12:e0185923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Paige E, Clément M, Lareyre F, et al. Interleukin-6 receptor signaling and abdominal aortic aneurysm growth rates. Circ Genom Precis Med. 2019;12:e002413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Jones GT, Tromp G, Kuivaniemi H, et al. Meta-analysis of genome-wide association studies for abdominal aortic aneurysm identifies four new disease-specific risk loci. Circ Res. 2017;120:341-353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Smallwood L, Allcock R, van Bockxmeer F, et al. Polymorphisms of the interleukin-6 gene promoter and abdominal aortic aneurysm. Eur J Vasc Endovasc Surg. 2008;35:31-36. [DOI] [PubMed] [Google Scholar]
- 42. Boddy AM, Lenk GM, Lillvis JH, Nischan J, Kyo Y, Kuivaniemi H. Basic research studies to understand aneurysm disease. Drug News Perspect. 2008;21:142-148. [PubMed] [Google Scholar]
- 43. Sugaya A, Misawa Y, Ohki SI, Takazawa I, Uesugi S. A case of immunoglobulin g4-related aortic diseases. Clin Case Rep. 2018;6:606-608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Akiyama M. Regarding “Upregulated interleukins (IL-6, IL-10, and IL-13) in immunoglobulin G4-related aortic aneurysm patients”. J Vasc Surg. 2017;66:1919. [DOI] [PubMed] [Google Scholar]
- 45. Kasashima S, Kawashima A, Zen Y, et al. Upregulated interleukins (IL-6, IL-10, and IL-13) in immunoglobulin g4-related aortic aneurysm patients. J Vasc Surg. 2018;67:1248-1262. [DOI] [PubMed] [Google Scholar]
- 46. Mojtahedzadeh M, Chelkeba L, Ranjvar-Shahrivar M, et al. Randomized trial of the effect of magnesium sulfate continuous infusion on IL-6 and CRP serum levels following abdominal aortic aneurysm surgery. Iran J Pharm Res. 2016;15:951-956. [PMC free article] [PubMed] [Google Scholar]
- 47. Vignali DA, Kuchroo VK. IL-12 family cytokines: immunological playmakers. Nat Immunol. 2012;13:722-728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Cua DJ, Sherlock J, Chen Y, et al. Interleukin-23 rather than interleukin-12 is the critical cytokine for autoimmune inflammation of the brain. Nature. 2003;421:744-748. [DOI] [PubMed] [Google Scholar]
- 49. Germann T, Rüde E. Interleukin-12. Int Arch Allergy Immunol. 1995;108:103-112. [DOI] [PubMed] [Google Scholar]
- 50. Teng MW, Bowman EP, McElwee JJ, et al. IL-12 and IL-23 cytokines: from discovery to targeted therapies for immune-mediated inflammatory diseases. Nat Med. 2015;21:719-729. [DOI] [PubMed] [Google Scholar]
- 51. Floss DM, Klöcker T, Schröder J, et al. Defining the functional binding sites of interleukin 12 receptor β1 and interleukin 23 receptor to Janus kinases. Mol Biol Cell. 2016;27:2301-2316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Jedynak M, Siemiatkowski A, Gacko M, Mroczko B, Borkowski J, Szmitkowski M. Ocena stezenia interleukiny-12 w surowicy chorych poddawanych operacji rekonstrukcji aorty brzusznej z powodu tetniaka–badania wstepne [Serum concentration of interleukin-12 (IL-12) in patients undergoing abdominal aortic aneurysm repair–preliminary report]. Pol Arch Med Wewn. 2004;112:1173-1179. [PubMed] [Google Scholar]
- 53. Sharma N, Dev R, Belenchia AM, et al. Deficiency of IL12p40 (Interleukin 12 p40) promotes ang II (angiotensin II)-Induced abdominal aortic aneurysm. Arterioscler Thromb Vasc Biol. 2019;39:212-223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Sharma N, Hans CP. Interleukin 12p40 deficiency promotes abdominal aortic aneurysm by activating CCN2/MMP2 pathways. J Am Heart Assoc. 2021;10:e017633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Yan H, Hu Y, Akk A, Ye K, Bacon J, Pham CTN. Interleukin-12 and -23 blockade mitigates elastase-induced abdominal aortic aneurysm. Sci Rep. 2019;9:10447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Monin L, Gaffen SL. Interleukin 17 family cytokines: signaling mechanisms, biological activities, and Therapeutic Implications. Cold Spring Harb Perspect Biol. 2018;10:a028522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Ho AW, Gaffen SL. IL-17RC: a partner in IL-17 signaling and beyond. Semin Immunopathol. 2010;32:33-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Wei Z, Wang Y, Zhang K, et al. Inhibiting the Th17/IL-17A-related inflammatory responses with digoxin confers protection against experimental abdominal aortic aneurysm. Arterioscler Thromb Vasc Biol. 2014;34:2429-2438. [DOI] [PubMed] [Google Scholar]
- 59. Huh JR, Leung MW, Huang P, et al. Digoxin and its derivatives suppress TH17 cell differentiation by antagonizing RORγt activity. Nature. 2011;472:486-490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Korn T, Bettelli E, Oukka M, Kuchroo VK. IL-17 and Th17 cells. Annu Rev Immunol. 2009;27:485-517. [DOI] [PubMed] [Google Scholar]
- 61. Sugaya M. The role of th17-related cytokines in atopic dermatitis. Int J Mol Sci. 2020;21:131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Sharma AK, Lu G, Jester A, et al. Experimental abdominal aortic aneurysm formation is mediated by IL-17 and attenuated by mesenchymal stem cell treatment [published correction appears in Circulation. 2012 Oct 23;126:e278]. Circulation. 2012;126:S38-S45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Ju X, Ijaz T, Sun H, et al. Interleukin-6-signal transducer and activator of transcription-3 signaling mediates aortic dissections induced by angiotensin II via the T-helper lymphocyte 17-interleukin 17 axis in C57BL/6 mice. Arterioscler Thromb Vasc Biol. 2013;33:1612-1621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Liao M, Liu CL, Lv BJ, et al. Plasma cytokine levels and risks of abdominal aortic aneurysms: A population-based prospective cohort study. Ann Med. 2015;47:245-252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Roberts AB, Anzano MA, Lamb LC, Smith JM, Sporn MB. New class of transforming growth factors potentiated by epidermal growth factor: isolation from non-neoplastic tissues. Proc Natl Acad Sci USA. 1981;78:5339-5343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Tucker RF, Shipley GD, Moses HL, Holley RW. Growth inhibitor from BSC-1 cells closely related to platelet type beta transforming growth factor. Science. 1984;226:705-707. [DOI] [PubMed] [Google Scholar]
- 67. Kang JS, Liu C, Derynck R. New regulatory mechanisms of TGF-beta receptor function. Trends Cell Biol. 2009;19:385-394. [DOI] [PubMed] [Google Scholar]
- 68. Moustakas A, Heldin CH. Non-Smad TGF-beta signals. J Cell Sci. 2005;118:3573-3584. [DOI] [PubMed] [Google Scholar]
- 69. Wang Y, Krishna S, Walker PJ, Norman P, Golledge J. Transforming growth factor-β and abdominal aortic aneurysms. Cardiovasc Pathol. 2013;22:126-132. [DOI] [PubMed] [Google Scholar]
- 70. Benke K, Ágg B, Szilveszter B, et al. The role of transforming growth factor-beta in Marfan syndrome. Cardiol J. 2013;20:227-234. [DOI] [PubMed] [Google Scholar]
- 71. Chaudhry SS, Cain SA, Morgan A, Dallas SL, Shuttleworth CA, Kielty CM. Fibrillin-1 regulates the bioavailability of TGFbeta1. J Cell Biol. 2007;176:355-367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Loeys BL, Chen J, Neptune ER, et al. A syndrome of altered cardiovascular, craniofacial, neurocognitive and skeletal development caused by mutations in TGFBR1 or TGFBR2. Nat Genet. 2005;37:275-281. [DOI] [PubMed] [Google Scholar]
- 73. Loeys BL, Schwarze U, Holm T, et al. Aneurysm syndromes caused by mutations in the TGF-beta receptor. N Engl J Med. 2006;355:788-798. [DOI] [PubMed] [Google Scholar]
- 74. Schepers D, Tortora G, Morisaki H, et al. A mutation update on the LDS-associated genes TGFB2/3 and SMAD2/3. Hum Mutat. 2018;39:621-634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Bertoli-Avella AM, Gillis E, Morisaki H, et al. Mutations in a TGF-β ligand, TGFB3, cause syndromic aortic aneurysms and dissections. J Am Coll Cardiol. 2015;65:1324-1336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Holm TM, Habashi JP, Doyle JJ, et al. Noncanonical TGFβ signaling contributes to aortic aneurysm progression in Marfan syndrome mice. Science. 2011;332:358-361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Zhang P, Hou S, Chen J, et al. Smad4 deficiency in smooth muscle cells initiates the formation of aortic aneurysm. Circ Res. 2016;118:388-399. [DOI] [PubMed] [Google Scholar]
- 78. Lareyre F, Clément M, Raffort J, et al. TGFβ (Transforming Growth Factor-β) blockade induces a human-like disease in a nondissecting mouse model of abdominal aortic aneurysm. Arterioscler Thromb Vasc Biol. 2017;37:2171-2181. [DOI] [PubMed] [Google Scholar]
- 79. Angelov SN, Hu JH, Wei H, Airhart N, Shi M, Dichek DA. TGF-β (Transforming growth factor-β) signaling protects the thoracic and abdominal aorta from angiotensin II-Induced pathology by distinct mechanisms. Arterioscler Thromb Vasc Biol. 2017;37:2102-2113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Dai J, Losy F, Guinault AM, et al. Overexpression of transforming growth factor-beta1 stabilizes already-formed aortic aneurysms: a first approach to induction of functional healing by endovascular gene therapy. Circulation. 2005;112:1008-1015. [DOI] [PubMed] [Google Scholar]
- 81. Thompson AR, Cooper JA, Jones GT, et al. Assessment of the association between genetic polymorphisms in transforming growth factor beta, and its binding protein (LTBP), and the presence, and expansion, of abdominal aortic aneurysm. Atherosclerosis. 2010;209:367-373. [DOI] [PubMed] [Google Scholar]
- 82. Bobik A. Transforming growth factor-betas and vascular disorders. Arterioscler Thromb Vasc Biol. 2006;26:1712-1720. [DOI] [PubMed] [Google Scholar]
- 83. Trifunović J, Miller L, Debeljak Ž, Horvat V. Pathologic patterns of interleukin 10 expression–a review. Biochem Med. 2015;25:36-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Mollazadeh H, Cicero AFG, Blesso CN, Pirro M, Majeed M, Sahebkar A. Immune modulation by curcumin: the role of interleukin-10. Crit Rev Food Sci Nutr. 2019;59:89-101. [DOI] [PubMed] [Google Scholar]
- 85. Moore KW, de Waal Malefyt R, Coffman RL, O’Garra A. Interleukin-10 and the interleukin-10 receptor. Annu Rev Immunol. 2001;19:683-765. [DOI] [PubMed] [Google Scholar]
- 86. Wang F, Quan QQ, Zhang CL, Li YB, Jiang TB. Association between polymorphisms in the interleukin-10 gene and risk of abdominal aortic aneurysm. Genet Mol Res. 2015;14:17599-17604. [DOI] [PubMed] [Google Scholar]
- 87. Meng X, Yang J, Zhang K, et al. Regulatory T cells prevent angiotensin II-induced abdominal aortic aneurysm in apolipoprotein E knockout mice. Hypertension. 2014;64:875-882. [DOI] [PubMed] [Google Scholar]
- 88. Zhu H, Qu X, Zhang C, Yu Y. Interleukin-10 promotes proliferation of vascular smooth muscle cells by inhibiting inflammation in rabbit abdominal aortic aneurysm. Int J Clin Exp Pathol. 2019;12:1260-1271. [PMC free article] [PubMed] [Google Scholar]
- 89. Vucevic D, Maravic-Stojkovic V, Vasilijic S, et al. Inverse production of IL-6 and IL-10 by abdominal aortic aneurysm explant tissues in culture. Cardiovasc Pathol. 2012;21:482-489. [DOI] [PubMed] [Google Scholar]
- 90. Kak G, Raza M, Tiwari BK. Interferon-gamma (IFN-γ): Exploring its implications in infectious diseases. Biomol Concepts. 2018;9:64-79. [DOI] [PubMed] [Google Scholar]
- 91. Ito S, Ansari P, Sakatsume M, et al. Interleukin-10 inhibits expression of both interferon alpha- and interferon gamma- induced genes by suppressing tyrosine phosphorylation of STAT1. Blood. 1999;93:1456-1463. [PubMed] [Google Scholar]
- 92. Schroder K, Hertzog PJ, Ravasi T, Hume DA. Interferon-gamma: an overview of signals, mechanisms and functions. J Leukoc Biol. 2004;75:163-189. [DOI] [PubMed] [Google Scholar]
- 93. Wang Z, Zheng T, Zhu Z, et al. Interferon gamma induction of pulmonary emphysema in the adult murine lung. J Exp Med. 2000;192:1587-1600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Hu X, Ivashkiv LB. Cross-regulation of signaling pathways by interferon-gamma: implications for immune responses and autoimmune diseases. Immunity. 2009;31:539-550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. King VL, Lin AY, Kristo F, et al. Interferon-gamma and the interferon-inducible chemokine CXCL10 protect against aneurysm formation and rupture. Circulation. 2009;119:426-435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Shimizu K, Shichiri M, Libby P, Lee RT, Mitchell RN. Th2-predominant inflammation and blockade of IFN-gamma signaling induce aneurysms in allografted aortas [published correction appears in J Clin Invest. 2004 Sep;114(5):739]. J Clin Investig. 2004;114:300-308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Xiong W, Zhao Y, Prall A, Greiner TC, Baxter BT. Key roles of CD4+T cells and IFN-γ in the development of abdominal aortic aneurysms in a murine model. J Immunol. 2004;172:2607-2612. [DOI] [PubMed] [Google Scholar]
- 98. Kuivaniemi H, Platsoucas CD, Tilson MD, 3rd. Aortic aneurysms: an immune disease with a strong genetic component. Circulation. 2008;117:242-252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Ott LW, Resing KA, Sizemore AW, et al. Tumor necrosis factor-alpha- and interleukin-1-induced cellular responses: coupling proteomic and genomic information. J Proteome Res. 2007;6:2176-2185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Kaneko H, Anzai T, Horiuchi K, et al. Tumor necrosis factor-α converting enzyme is a key mediator of abdominal aortic aneurysm development. Atherosclerosis. 2011;218:470-478. [DOI] [PubMed] [Google Scholar]
- 101. Xiong W, MacTaggart J, Knispel R, Worth J, Persidsky Y, Baxter BT. Blocking TNF-α attenuates aneurysm formation in a murine model. J Immunol. 2009;183:2741-2746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Wu X, Cakmak S, Wortmann M, et al. Sex- and disease-specific inflammasome signatures in circulating blood leukocytes of patients with abdominal aortic aneurysm. Mol Med. 2016;22:505-518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Isoda K, Akita K, Kitamura K, et al. Inhibition of interleukin-1 suppresses angiotensin II-induced aortic inflammation and aneurysm formation. Int J Cardiol. 2018;270:221-227. [DOI] [PubMed] [Google Scholar]
- 104. Johnston WF, Salmon M, Su G, et al. Genetic and pharmacologic disruption of interleukin-1β signaling inhibits experimental aortic aneurysm formation. Arterioscler Thromb Vasc Biol. 2013;33:294-304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Meher AK, Spinosa M, Davis JP, et al. Novel role of IL (Interleukin)-1β in neutrophil extracellular trap formation and abdominal aortic aneurysms. Arterioscler Thromb Vasc Biol. 2018;38:843-853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Jiang YF, Guo LL, Zhang LW, et al. Local upregulation of interleukin-1 beta in aortic dissecting aneurysm: correlation with matrix metalloproteinase-2, 9 expression and biomechanical decrease. Interact Cardiovasc Thorac Surg. 2019;28:344-352. [DOI] [PubMed] [Google Scholar]
- 107. Hingorani A, Ascher E, Scheinman M, et al. The effect of tumor necrosis factor binding protein and interleukin-1 receptor antagonist on the development of abdominal aortic aneurysms in a rat model. J Vasc Surg. 1998;28:522-526. [DOI] [PubMed] [Google Scholar]
- 108. Batra R, Suh MK, Carson JS, et al. IL-1β (Interleukin-1β) and TNF-α (Tumor necrosis factor-α) impact abdominal aortic aneurysm formation by differential effects on macrophage polarization. Arterioscler Thromb Vasc Biol. 2018;38:457-463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Spinosa MD, Montgomery WG, Lempicki M, et al. B cell-activating factor antagonism attenuates the growth of experimental abdominal aortic aneurysm. Am J Pathol. 2021;191:2231-2244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Ho IC, Miaw SC. Regulation of IL-4 expression in immunity and diseases. Adv Exp Med Biol. 2016;941:31-77. [DOI] [PubMed] [Google Scholar]
- 111. Liu CL, Liu X, Zhang Y, et al. Eosinophils protect mice from Angiotensin-II perfusion-induced abdominal aortic aneurysm. Circ Res. 2021;128:188-202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Kim S. Interleukin-32 in inflammatory autoimmune diseases. Immune Netw. 2014;14:123-127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Bengts S, Shamoun L, Kunath A, et al. Altered IL-32 signaling in abdominal aortic aneurysm. J Vasc Res. 2020;57:236-244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Cayrol C, Girard JP. Interleukin-33 (IL-33): A nuclear cytokine from the IL-1 family. Immunol Rev. 2018;281:154-168. [DOI] [PubMed] [Google Scholar]
- 115. Li J, Xia N, Wen S, et al. IL (Interleukin)-33 suppresses abdominal aortic aneurysm by enhancing regulatory T-cell expansion and activity. Arterioscler Thromb Vasc Biol. 2019;39:446-458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Shi Y, Riese DJ, 2nd, Shen J. The role of the CXCL12/CXCR4/CXCR7 chemokine axis in cancer. Front Pharmacol. 2020;11:574667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Tanios F, Pelisek J, Lutz B, et al. CXCR4: A potential marker for inflammatory activity in abdominal aortic aneurysm wall. Eur J Vasc Endovasc Surg. 2015;50:745-753. [DOI] [PubMed] [Google Scholar]
- 118. Michineau S, Franck G, Wagner-Ballon O, Dai J, Allaire E, Gervais M. Chemokine (C-X-C motif) receptor 4 blockade by AMD3100 inhibits experimental abdominal aortic aneurysm expansion through anti-inflammatory effects. Arterioscler Thromb Vasc Biol. 2014;34:1747-1755. [DOI] [PubMed] [Google Scholar]
- 119. Nie H, Wang HX, Tian C, et al. Chemokine (C-X-C motif) receptor 2 blockade by SB265610 inhibited angiotensin II-induced abdominal aortic aneurysm in Apo E-/- mice. Heart Vessels. 2019;34:875-882. [DOI] [PubMed] [Google Scholar]
- 120. Sun B, Li F, Lai S, et al. Inhibition of CXCR2 alleviates the development of abdominal aortic aneurysm in Apo E-/- mice. Acta Cir Bras. 2021;36:e360105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121. Ishibashi M, Egashira K, Zhao Q, et al. Bone marrow-derived monocyte chemoattractant protein-1 receptor CCR2 is critical in angiotensin II-induced acceleration of atherosclerosis and aneurysm formation in hypercholesterolemic mice. Arterioscler Thromb Vasc Biol. 2004;24:e174-e178. [DOI] [PubMed] [Google Scholar]
- 122. Katrancioglu N, Manduz S, Karahan O, et al. The role of the CCR2 gene polymorphism in abdominal aortic aneurysms. Angiology. 2011;62:140-143. [DOI] [PubMed] [Google Scholar]
- 123. Jabłońska A, Zagrapan B, Neumayer C, et al. Polymorphisms in the IL-6 and TNF-α gene are associated with an increased risk of abdominal aortic aneurysm. Int J Cardiol. 2021;329:192-197. [DOI] [PubMed] [Google Scholar]
- 124. Bown MJ, Lloyd GM, Sandford RM, et al. The interleukin-10-1082 ‘A’ allele and abdominal aortic aneurysms. J Vasc Surg. 2007;46:687-693. [DOI] [PubMed] [Google Scholar]
- 125. Bown MJ, Burton PR, Horsburgh T, Nicholson ML, Bell PR, Sayers RD. The role of cytokine gene polymorphisms in the pathogenesis of abdominal aortic aneurysms: a case-control study. J Vasc Surg. 2003;37:999-1005. [DOI] [PubMed] [Google Scholar]
- 126. Zuo S, Xiong J, Wei Y, et al. Potential interactions between genetic polymorphisms of the transforming growth factor-β pathway and environmental factors in abdominal aortic aneurysms. Eur J Vasc Endovasc Surg. 2015;50:71-77. [DOI] [PubMed] [Google Scholar]
- 127. Baas AF, Medic J, van ‘t Slot R, et al. Association of the TGF-beta receptor genes with abdominal aortic aneurysm. Eur J Hum Genet. 2010;18:240-244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. Golledge J, Clancy P, Jones GT, et al. Possible association between genetic polymorphisms in transforming growth factor beta receptors, serum transforming growth factor beta1 concentration and abdominal aortic aneurysm. Br J Surg. 2009;96:628-632. [DOI] [PubMed] [Google Scholar]
- 129. Zhang W, Zeng Q, Xu Y, et al. Exome sequencing identified a novel SMAD2 mutation in a Chinese family with early onset aortic aneurysms. Clin Chim Acta. 2017;468:211-214. [DOI] [PubMed] [Google Scholar]
- 130. Ghilardi G, Biondi ML, Battaglioli L, Zambon A, Guagnellini E, Scorza R. Genetic risk factor characterizes abdominal aortic aneurysm from arterial occlusive disease in human beings: CCR5 delta 32 deletion. J Vasc Surg. 2004;40:995-1000. [DOI] [PubMed] [Google Scholar]
- 131. Bugge E, Wynn R, Mollnes TE, Reitan SK, Grønli OK. Cytokine profiles and diagnoses in elderly, hospitalized psychiatric patients. BMC Psychiatry. 2018;18:315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132. Parkitny L, McAuley JH, Kelly PJ, Di Pietro F, Cameron B, Moseley GL. Multiplex cytokine concentration measurement: how much do the medium and handling matter? Mediators Inflamm. 2013;2013:890706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133. Kim HO, Kim HS, Youn JC, Shin EC, Park S. Serum cytokine profiles in healthy young and elderly population assessed using multiplexed bead-based immunoassays. J Transl Med. 2011;9:113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134. Ahmad M, Kuravi S, Hodson J, et al. The relationship between serum interleukin-1α and asymptomatic infrarenal abdominal aortic aneurysm size, morphology, and growth rates. Eur J Vasc Endovasc Surg. 2018;56:130-135. [DOI] [PubMed] [Google Scholar]
- 135. Treska V, Topolcan O, Wenham PW, Pecen L, Kocová J. Metabolismus cytokinů u aneuryzmatu brisní aorty [Cytokine metabolism in aneurysms of the abdominal aorta]. Rozhl Chir. 1998;77:225-229. [PubMed] [Google Scholar]
- 136. Treska V, Topolcan O, Kocová J, et al. Plazmatické hladiny prozánetlivých cytokinů u aneuryzmatu abdominální aorty [Plasmatic levels of proinflammatory cytokines in abdominal aortic aneurysms]. Rozhl Chir. 2011;90:37-41. [PubMed] [Google Scholar]
- 137. Treska V, Topolcan O, Pecen L. Cytokines as plasma markers of abdominal aortic aneurysm. Clin Chem Lab Med. 2000;38:1161-1164. [DOI] [PubMed] [Google Scholar]
- 138. Dawson J, Cockerill GW, Choke E, Belli AM, Loftus I, Thompson MM. Aortic aneurysms secrete interleukin-6 into the circulation. J Vasc Surg. 2007;45:350-356. [DOI] [PubMed] [Google Scholar]
- 139. Flondell-Sité D, Lindblad B, Kölbel T, Gottsäter A. Cytokines and systemic biomarkers are related to the size of abdominal aortic aneurysms. Cytokine. 2009;46:211-215. [DOI] [PubMed] [Google Scholar]
- 140. Bernal S, Lopez-Sanz L, Jimenez-Castilla L, et al. Protective effect of suppressor of cytokine signalling 1-based therapy in experimental abdominal aortic aneurysm. Br J Pharmacol. 2021;178:564-581. [DOI] [PubMed] [Google Scholar]
- 141. Blumel R, Patel K, Rizzo JA, et al. Accuracy of the “Thumb-Palm Test” for detection of ascending aortic aneurysm. Am J Cardiol. 2021;150:114-116. [DOI] [PubMed] [Google Scholar]
- 142. Gemcioglu E, Davutoglu M, Catalbas R, et al. Predictive values of biochemical markers as early indicators for severe COVID-19 cases in admission. Future Virol. 2021;16: 353-367. [Google Scholar]
- 143. Liang Y, Xiao W, Guan YX, et al. Prognostic value of the C-reactive protein/Albumin ratio (CAR) in patients with operable soft tissue sarcoma. Oncotarget. 2017;8:98135-98147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144. Gultekin Y, Bolat A, Hatice K, Tekeli Kunt A. Does aspartate aminotransferase to alanine aminotransferase ratio predict acute kidney injury after cardiac surgery? Heart Surg Forum. 2021;24:E506-E511. [DOI] [PubMed] [Google Scholar]
- 145. Deng L, Qiu S, Wang C, et al. Effects of the blood urea nitrogen to creatinine ratio on haemorrhagic transformation in AIS patients with diabetes mellitus. BMC Neurol. 2019;19:63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146. Choudhary MK, Eräranta A, Koskela J, et al. Atherogenic index of plasma is related to arterial stiffness but not to blood pressure in normotensive and never-treated hypertensive subjects. Blood Press. 2019;28:157-167. [DOI] [PubMed] [Google Scholar]