Figure 1.
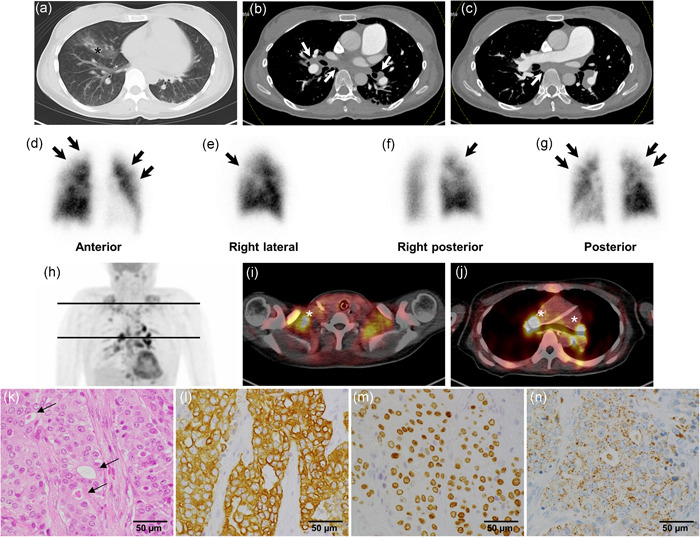
Contrast‐enhanced computed tomography (CT), lung perfusion scintigraphy, 18F‐fluorodeoxyglucose positron emission tomography (FDG‐PET)/CT, and histology of the right subclavian lymph node biopsy specimens during diagnostic evaluation. (a) Chest CT shows an infiltrative shadow in the right middle lobe (black asterisk). (b and c) Contrast‐enhanced CT shows mediastinal and bilateral hilar lymphadenopathy (white arrows) without obvious findings of pulmonary thromboembolism or mass in any organs indicating malignancy. (d–g) Lung perfusion scintigraphy shows multiple subsegmental perfusion defects (black arrows) in the subpleural portion of both lungs. Note: They are relatively small and light compared with the typical characteristics of chronic thromboembolic pulmonary hypertension. (h–j) FDG‐PET/CT shows multiple abnormal uptakes (white asterisks) in the mediastinal, bilateral hilar, bilateral supraclavicular, and subclavian lymph nodes. (k) Lymph nodes are replaced by predominantly solid sheets and nests of tumor cells with very focal gland formation with mucin (arrows), suggesting metastatic adenocarcinoma (hematoxylin and eosin staining). Immunohistochemistry panels show that (l) cytokeratin (CK) 7 (brown), (m) thyroid transcription factor‐1 (brown), and (n) napsin A (brown) are all positive. Considering that p40, CK5/6, CK20, and thyroglobulin were negative markers (data not shown), these results indicate that lung adenocarcinoma is the most probable primary lesion
