Abstract
The term “monoclonal gammopathy of clinical significance” (MGCS) refers to any plasma cell or B-cell clonal disorder that does not meet the current criteria for malignant disorders but produces a monoclonal protein that directly or indirectly results in organ damage. The most commonly affected organs are the kidneys, nerves, and skin. This review summarizes the current classification of MGCS and its diagnostic and treatment approaches.
Keywords: Monoclonal gammopathy of clinical significance, Diagnosis, Management
INTRODUCTION
The concept of monoclonal gammopathy of undetermined significance (MGUS) was first introduced in 1978 [1]. It is a premalignant clonal disorder defined by the presence of a monoclonal protein (M-protein) produced by an abnormal plasma cell or B-cell but does not meet the criteria for multiple myeloma (MM), Waldenström macroglobulinemia (WM), or other malignant lymphoproliferative disorders [2]. MGUS can be found in approximately 3% of the population over 50 years of age and 5% of the population over 70 years of age [3]. The risk of progression of MGUS to a malignant disorder, such as MM, WM, or other B-cell lymphoproliferative disorders is approximately 1% annually [4], and treatment is usually not initiated until the diagnosis of these malignant disorders.
Until recently, the pathogenic role of M-proteins in kidney disease was thought to be mainly attributed to malignant conditions, such as MM and WM. However, over the last two decades, it has become clear that kidney disorders can be induced by nephrotoxic M-proteins, regardless of the tumor burden [5]. The term monoclonal gammopathy of renal significance (MGRS) was introduced in 2012 by the International Kidney and Monoclonal Gammopathy Research Group. This refers to any plasma cell or B-cell clonal disorder that does not meet the current criteria for malignant disorders but produces a nephrotoxic M-protein that directly or indirectly results in kidney disease or injury [6]. Treatment is often required to prevent renal deterioration. More recently, it has become apparent that other organ systems, such as peripheral nerves and skin, can also be affected by M-proteins produced by a small clone of plasma cells or B cells. Accordingly, the term monoclonal gammopathy of clinical significance (MGCS) was introduced in 2018 [7]. This review aimed to introduce the MGCS classification and available approaches for its diagnosis and treatment.
MGRS
M-proteins can induce kidney damage through a various mechanisms that can be separated by the presence of a high or low tumor burden [5]. Kidney damage due to a high tumor burden is represented by light-chain cast nephropathy, which requires high levels of a serum-free light chain, and usually only occurs in patients with malignant disorders, such as MM or WM [8]. Thus, light chain cast nephropathy is not considered an MGRS-related kidney disorder. MGRS is usually associated with low levels of monoclonal gammopathy produced by nonmalignant or premalignant B-cells or plasma cell clones. It should be noted that MGRS can also be associated with other hematological disorders, such as smoldering MM and WM, monoclonal B-cell lymphocytosis, and AL amyloidosis [9].
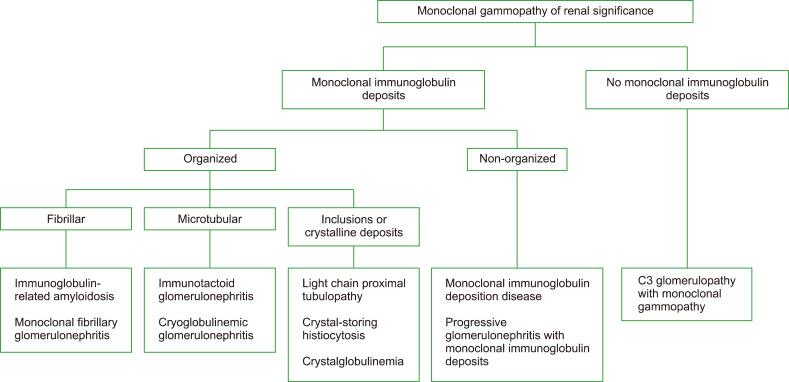
Kidney diseases associated with MGRS are mostly glomerular disorders, apart from light-chain proximal tubulopathy, and crystal-storing histiocytosis [9]. MGRS-related kidney disease can be initially categorized according to the presence or absence of monoclonal immunoglobulin deposits in the kidneys (Fig. 1). MGRS-related kidney disorders with monoclonal immunoglobulin deposits can be further subcategorized into organized and non-organized, based on the ultrastructural characteristics of the deposits. In addition, organized deposits are further subdivided into fibrillar, microtubular, and inclusion or crystalline categories.
Fig. 1.
Categorization of MGRS-related kidney disorders.
MGRS-RELATED KIDNEY DISORDERS WITH MONOCLONAL IMMUNOGLOBULIN DEPOSITS
Lesions with organized deposits
Immunoglobulin-related amyloidosis (light chain, heavy chain, and heavy and light chain amyloidosis) and monoclonal fibrillary glomerulonephritis are two diseases characterized by fibrillar deposits. The fibrillar deposits in amyloidosis are positive for Congo red staining with diameters of 7–12 nm, whereas those in monoclonal fibrillary glomerulonephritis are typically negative for Congo red staining with diameters of 10–30 nm [9]. In addition, DnaJ homolog subfamily B member 9 is a reliable marker for fibrillary glomerulonephritis, which can further distinguish monoclonal fibrillary glomerulonephritis from amyloidosis [10].
The microtubular category consists of immunotactoid glomerulonephritis and cryoglobulinemic glomerulonephritis. Microtubules can be distinguished from fibrils by their hollow centers and large diameters (17–52 nm) [11]. Glomerular deposits in immunotactoid glomerulonephritis are uniform microtubules usually arranged in parallel arrays with subepithelial and subendothelial localization [9]. In contrast, only a small fraction of the deposits in cryoglobulinemic glomerulonephritis are organized and usually appear as short, curved, or straight microtubules [9].
MGRS disorders with crystal inclusions include light chain proximal tubulopathy (LCPT), crystal-storing histiocytosis (CSH), and crystalglobulinemia. LCPT can be classified into crystalline and non-crystalline variants. Rod-or rhomboid-shaped light-chain crystals are localized within proximal tubular cells in the crystalline variant, whereas non-crystalline light-chain inclusions accumulate in the proximal tubule cells in the non-crystalline variant [9]. In CSH, light chain crystals are found in the renal histiocytes and proximal tubular cells [12]. Crystalglobulinemic glomerulonephritis is characterized by crystal deposits of monoclonal immunoglobulin within arterioles and glomerular capillaries [13].
Lesions with non-organized deposits
MGRS disorders with nonorganized deposits include monoclonal immunoglobulin deposition disease (MIDD) and progressive glomerulonephritis with monoclonal immunoglobulin deposits (PGNMID). MIDD is characterized by linear punctate deposits in the glomerular and tubular basement membranes [9]. In PGNMID, deposits are confined to the glomeruli, causing complement activation, leading to glomerular inflammation and proliferation [5].
MGRS-RELATED KIDNEY DISORDERS WITHOUT MONOCLONAL IMMUNOGLOBULIN DEPOSITS
Not all MGRS-related kidney disorders involve monoclonal immunoglobulin deposits. In C3 glomerulopathy with monoclonal gammopathy, while there is no significant renal immunoglobulin deposition, monoclonal immunoglobulin activates complement through an alternative pathway, resulting in the C3 deposition in the glomerulus [5].
Renal biopsy is essential for the MGRS diagnosis. The incidence of both MGUS and chronic kidney disease (CKD) increases with age [3, 14]. Therefore, it is not uncommon for a patient to have both MGUS and a kidney disorder that are unrelated to each other. A recent study reported that proteinuria of ≥1.5 g/day, microscopic hematuria, and an elevated free light chain ratio were significantly associated with MGRS in patients with monoclonal gammopathy [15]. Thus, a kidney biopsy should be strongly considered in patients with monoclonal gammopathy and these laboratory findings or those experiencing rapidly progressive renal failure.
Treatment of MGRS should be determined by the nature of the clone (plasma cell or B-cell) that produces the nephrotoxic monoclonal immunoglobulin, the severity of the kidney disease, and potential for reversal of kidney damage. Patients with plasma cell clones, such as bortezomib, should be treated with chemotherapeutic agents used to treat MM [16-18]. Patients with B-cell clones expressing CD20 should be treated with rituximab-based approaches [19, 20]. In patients whose disease has not progressed to advanced CKD, the main goal of treatment is the preservation of kidney function. For those with advanced CKD, the role of clone-directed therapy should focus on reducing the risk of MGRS recurrence after kidney transplantation. Notably, high relapse rates of MGRS have been reported in patients whose monoclonal gammopathy was not fully treated before kidney transplantation. Therefore, patients who are candidates for kidney transplantation should be treated until a very good partial response is achieved [5]. In patients with advanced CKD who are not candidates for kidney transplantation, treatment should be initiated only if there is an extrarenal manifestation of the disease that requires intervention.
NEUROLOGIC MGCS
Neurologic MGCS include AL amyloidosis, POEMS syndrome (polyradiculoneuropathy, organomegaly, endocrinopathy, monoclonal plasma cell disorder, and skin changes), cryoglobulinemia, CANOMAD (chronic ataxic neuropathy, ophthalmoplegia, immunoglobulin M [IgM] paraprotein, cold agglutinins, and disialosyl antibodies), and DADS-M (distal acquired demyelinating symmetric neuropathy with M-protein). The first three are diseases with multiple systemic manifestations, while the last two (CANOMAD and DADS-M) primarily involve the nervous system [21].
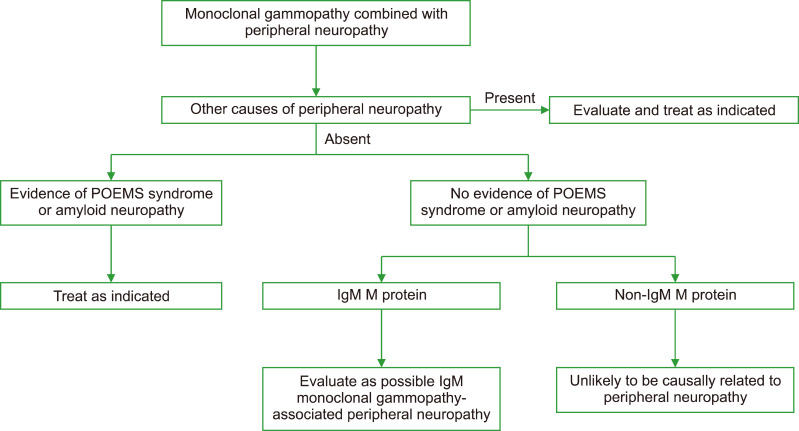
The algorithm for evaluating patients with monoclonal gammopathy combined with peripheral neuropathy is presented in Fig. 2. The first step in evaluating a patient with monoclonal gammopathy combined with peripheral neuropathy is to exclude other causes of peripheral neuropathy, such as diabetes, alcoholism, and drugs [21]. The next step would be to distinguish specific plasma cell disorders that are known to have a definite causal relationship with neuropathy (POEMS syndrome and amyloid neuropathy) from other monoclonal gammopathies associated with peripheral neuropathy. Therapy is directed at treating underlying diseases in patients with POEMS syndrome and amyloid neuropathy.
Fig. 2.
Algorithm for evaluating patients with monoclonal gammo-pathy combined with peripheral neuropathy.
In the absence of POEMS syndrome or amyloid neuropathy, it is challenging to differentiate between patients in whom M-protein is causally associated with peripheral neuropathy and those in whom M-protein is not associated with neuropathy because there are no specific tests to distinguish between a true causal association and an incidental association. In general, the younger the patient, the more likely the association between M-protein and neuropathy is causal because the M-protein prevalence is <1.5% in persons aged <50 years [21]. In addition, the likelihood of a causal relationship is much higher for IgM M-proteins than for IgG or IgA M-proteins. Nerve conduction studies should be performed to distinguish between demyelinating and axonal patterns, and anti-MAG and anti-ganglioside antibody tests may help diagnose the underlying cause of neuropathy. CANOMAD is characterized by chronic neuropathy with sensory ataxia and motor weakness involving the oculomotor and bulbar muscles, occurring in the presence of monoclonal IgM directed against disialosyl ganglioside epitopes [22]. DADS-M typically presents with symmetric sensory or sensorimotor dysfunction in the lower extremities with sparing of the proximal limbs, trunk, and face [23], and involvement of the upper limbs may occur later. The treatment of CANOMAD and DADS-M includes intravenous immunoglobulin (IVIG) and rituximab.
CUTANEOUS MGCS
Cutaneous MGCS includes scleromyxedema, Schnitzler syndrome, necrobiotic xanthogranuloma (NXG), TEMPI syndrome, systemic capillary leak syndrome (SCLS), cryoglobulinemia, and POEMS syndrome (Table 1).
Table 1.
Diagnostic criteria for five selected cutaneous monoclonal gammopathy of clinical significance.
| POEMS syndromea) [26] | Scleromyxedema [24] | Schnitzler syndromeb,c) [26] | Necrobiotic xanthogranulomad) [30] | TEMPI syndrome [33] |
|---|---|---|---|---|
Mandatory major criteria
|
|
Obligate criteria
|
Major criteria
|
Major criteria
|
Other major criteria
| ||||
Minor criteria
|
Minor criteria
|
Minor criteria
|
Minor criteria
|
a)POEMS syndrome diagnosis is confirmed when both mandatory major criteria, one of the other major criteria, and one of the minor criteria are present. b)Definite diagnosis of Schnitzler syndrome: if IgM, both obligate criteria and at least2 minor criteria; if IgG, both obligate criteria and 3 minor criteria. c)Probable diagnosis of Schnitzler syndrome: if IgM, both obligate criteria and 1 minor criteria; if IgG, both obligate criteria and 2 minor criteria. d)Xanthogranuloma diagnosis is confirmed when both major criteria and at least 1 minor criterion are present. It is only applicable in the absence of a foreign body, infection, or other identifiable causes.
Scleromyxedema is a rare systemic mucinosis characterized by generalized papular and sclerodermoid cutaneous eruptions usually associated with IgG monoclonal gammopathy [24]. It can be accompanied by various extracutaneous manifestations, including involvement of the nervous, musculoskeletal, cardiac, and pulmonary systems [25]. The infiltrates are composed of mucin, but the pathophysiology of scleromyxedema remains unclear. High-dose IVIG is an effective first-line treatment for non-severe disease, whereas plasma cell-directed chemotherapy seems to be useful for refractory and severe forms of the disease [25].
Schnitzler syndrome is characterized by chronic urticaria and IgM monoclonal gammopathy [26]. However, it is rarely associated with IgG monoclonal gammopathy. Other clinical features of Schnitzler syndrome include recurrent fever, bone pain, leukocytosis, and elevated CRP levels. Interleukin (IL)-1β plays an important role in the pathophysiology of Schnitzler syndrome, and treatment with anti-IL-1 monoclonal antibodies such as anakinra, rilonacept, and canakinumab has been shown to be effective [27-29].
NXG is a non-Langerhans histiocytosis classically associated with paraproteinemia attributable to plasma cell or lymphoproliferative disorders. The classic clinical presentation is yellow-to-orange papules, plaques, and/or nodules involving the periorbital skin [30]. Cutaneous lesions can also be distributed elsewhere on the face, trunk, or extremities. The eye is the most common site of extracutaneous involvement. Other relatively rare extracutaneous involvement sites include the heart, gastrointestinal tract, liver, and lungs. Histopathologically, NXG shows palisading granulomas with lymphoplasmacytic infiltrates and zones of necrobiosis. Other characteristic features that are variably present include cholesterol clefts and/or giant cells (Toutons or foreign bodies). The pathogenesis of NXG remains largely unknown, but a role for paraprotein-lipoprotein interaction has been hypothesized [31, 32]. IVIG treatment is one of the most promising therapies, whereas plasma cell-directed therapy may be considered as a second-line therapy [26].
TEMPI syndrome is a rare disease characterized by telangiectasias, elevated erythropoietin and erythrocytosis, monoclonal gammopathy, perinephric fluid collection, and intrapulmonary shunting [33]. The initial clinical presentations of most patients are telangiectasias and erythrocytosis. Telangiectasias are most prominent on the face, trunk, and hands and are rarely seen on the lower extremities. Notable laboratory findings are elevated serum erythropoietin levels and the lack of a JAK2 mutation. Monoclonal gammopathy is a hallmark feature of TEMPI syndrome and does not appear to have immunoglobulin or light chain specificity, unlike POEMS syndrome, wherein the monoclonal antibody is almost always lambda-restricted. Pulmonary shunting is not evident on high-resolution computed tomography of the chest and is best quantified by 99mTc macroaggregated albumin scintigraphy. Perinephric fluid has the same chemical composition as serum [34]. Plasma cell-directed therapies, including bortezomib, daratumumab, and lenalidomide, appear to be effective with a rapid and remarkable treatment response [35-38].
Cryoglobulinemia is defined as the persistent presence of cryoglobulins in serum. Cryoglobulin is an abnormal immunoglobulin that precipitates at low temperatures and dissolves when the temperature increases [39]. Cutaneous manifestations develop in nearly all patients but can affect almost any organ system, including the musculoskeletal, peripheral nerve, renal, and pulmonary systems. Type I cryoglobulinemia is characterized by a single monoclonal immunoglobulin from plasma cells or lymphoproliferative disorders. In type II cryoglobulinemia, cryoglobulins comprise a mixture of polyclonal immunoglobulins and one or more monoclonal immunoglobulins, whereas type III cryoglobulinemia involves only polyclonal immunoglobulins. Type II/III cryoglobulinemia may also be related to plasma cell or lymphoproliferative disorders but is more often associated with infectious diseases, particularly chronic HCV infection and autoimmune diseases, such as Sjögren’s syndrome and lupus.
Type I cryoglobulinemia often causes occlusive symptoms due to occlusion of the capillary lumen [39]. Skin manifestations include cold-induced symptoms and purpura; however, they can also induce distal ischemia and skin necrosis. Small-vessel vasculitis is the primary cause of morbidity in type II/III cryoglobulinemia. Purpura is observed in most patients; however, distal ischemia or skin necrosis is rare. The treatment strategy for cryoglobulinemia is to treat the underlying disorder. Therefore, treatment is directed at the underlying plasma cell or lymphoproliferative disorder in patients with type I cryoglobulinemia and at the underlying infectious or autoimmune disorder in patients with type II/III cryoglobulinemia.
SCLS is a rare disorder characterized by recurrent episodes of sudden-onset shock and anasarca caused by plasma extravasation (up to 70% of the total plasma volume) [40]. The diagnostic triad of SCLS is the “3 Hs”: 1) hypotension (typically systolic blood pressure of <90 mmHg), 2) hemoconcentration (hematocrit >49% to 50% in men and 43–45% in women), and 3) hypoalbuminemia (<3.0 g/dL) in the absence of secondary causes for such abnormalities. The underlying mechanism of SCLS remains unelucidated. MGUS is present in 68–85% of SCLS patients, most commonly of the IgGk isotype. Nevertheless, as MGUS is not specific to this syndrome, SCLS remains clinically diagnosed. Supportive care with intravenous fluids sufficient to counteract intravascular volume depletion and maintain organ perfusion is used during its acute attack, which usually subsides after a few days. IVIG prophylaxis is recommended because it is associated with a reduction in SCLS attacks in most patients [41].
CONCLUSION
MGCS is a new diagnostic term to better classify patients with organ damage due to M-protein produced by a clone of non-malignant plasma cells or B-cells. The introduction of MGCS has raised clinicians’ awareness that small amounts of M-protein can cause several serious clinical conditions, wherein the kidneys, nerves, and skin are usually affected. The diagnosis of MGCS requires the exclusion of chance associations because of the high prevalence of M-protein, especially in the elderly population. Clinical and histopathological aspects must be considered in a causal association between organ damage and M-proteins. In many cases, the appropriate treatment is clone-directed eradication, based on agents previously limited to patients with overt hematologic malignancies. In other cases, treatments, such as IVIG and anti-IL-1 monoclonal antibodies may provide favorable outcomes.
Footnotes
Authors’ Disclosures of Potential Conflicts of Interest
No potential conflicts of interest relevant to this article were reported.
REFERENCES
- 1.Kyle RA. Monoclonal gammopathy of undetermined significance. Natural history in 241 cases. Am J Med. 1978;64:814–26. doi: 10.1016/0002-9343(78)90522-3. [DOI] [PubMed] [Google Scholar]
- 2.Mouhieddine TH, Weeks LD, Ghobrial IM. Monoclonal gammopathy of undetermined significance. Blood. 2019;133:2484–94. doi: 10.1182/blood.2019846782. [DOI] [PubMed] [Google Scholar]
- 3.Kyle RA, Therneau TM, Rajkumar SV, et al. Prevalence of monoclonal gammopathy of undetermined significance. N Engl J Med. 2006;354:1362–9. doi: 10.1056/NEJMoa054494. [DOI] [PubMed] [Google Scholar]
- 4.Kyle RA, Larson DR, Therneau TM, et al. Long-term follow-up of monoclonal gammopathy of undetermined significance. N Engl J Med. 2018;378:241–9. doi: 10.1056/NEJMoa1709974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Leung N, Bridoux F, Nasr SH. Monoclonal gammopathy of renal significance. N Engl J Med. 2021;384:1931–41. doi: 10.1056/NEJMra1810907. [DOI] [PubMed] [Google Scholar]
- 6.Leung N, Bridoux F, Hutchison CA, et al. Monoclonal gammopathy of renal significance: when MGUS is no longer undetermined or insignificant. Blood. 2012;120:4292–5. doi: 10.1182/blood-2012-07-445304. [DOI] [PubMed] [Google Scholar]
- 7.Fermand JP, Bridoux F, Dispenzieri A, et al. Monoclonal gammopathy of clinical significance: a novel concept with therapeutic implications. Blood. 2018;132:1478–85. doi: 10.1182/blood-2018-04-839480. [DOI] [PubMed] [Google Scholar]
- 8.Sanders PW, Booker BB. Pathobiology of cast nephropathy from human Bence Jones proteins. J Clin Invest. 1992;89:630–9. doi: 10.1172/JCI115629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Leung N, Bridoux F, Batuman V, et al. The evaluation of monoclonal gammopathy of renal significance: a consensus report of the International Kidney and Monoclonal Gammopathy Research Group. Nat Rev Nephrol. 2019;15:45–59. doi: 10.1038/s41581-018-0077-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nasr SH, Vrana JA, Dasari S, et al. DNAJB9 is a specific immunohistochemical marker for fibrillary glomerulonephritis. Kidney Int Rep. 2017;3:56–64. doi: 10.1016/j.ekir.2017.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nasr SH, Fidler ME, Cornell LD, et al. Immunotactoid glomerulopathy: clinicopathologic and proteomic study. Nephrol Dial Transplant. 2012;27:4137–46. doi: 10.1093/ndt/gfs348. [DOI] [PubMed] [Google Scholar]
- 12.El Hamel C, Thierry A, Trouillas P, et al. Crystal-storing histiocytosis with renal Fanconi syndrome: pathological and molecular characteristics compared with classical myeloma- associated Fanconi syndrome. Nephrol Dial Transplant. 2010;25:2982–90. doi: 10.1093/ndt/gfq129. [DOI] [PubMed] [Google Scholar]
- 13.Gupta V, El Ters M, Kashani K, Leung N, Nasr SH. Crystalglobulin- induced nephropathy. J Am Soc Nephrol. 2015;26:525–9. doi: 10.1681/ASN.2014050509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Delanaye P, Glassock RJ, Pottel H, Rule AD. An age-calibrated definition of chronic kidney disease: rationale and benefits. Clin Biochem Rev. 2016;37:17–26. [PMC free article] [PubMed] [Google Scholar]
- 15.Klomjit N, Leung N, Fervenza F, Sethi S, Zand L. Rate and predictors of finding monoclonal gammopathy of renal significance (MGRS) lesions on kidney biopsy in patients with monoclonal gammopathy. J Am Soc Nephrol. 2020;31:2400–11. doi: 10.1681/ASN.2020010054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sayed RH, Wechalekar AD, Gilbertson JA, et al. Natural history and outcome of light chain deposition disease. Blood. 2015;126:2805–10. doi: 10.1182/blood-2015-07-658872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mikhael JR, Schuster SR, Jimenez-Zepeda VH, et al. Cyclophosphamide- bortezomib-dexamethasone (CyBorD) produces rapid and complete hematologic response in patients with AL amyloidosis. Blood. 2012;119:4391–4. doi: 10.1182/blood-2011-11-390930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cohen C, Royer B, Javaugue V, et al. Bortezomib produces high hematological response rates with prolonged renal survival in monoclonal immunoglobulin deposition disease. Kidney Int. 2015;88:1135–43. doi: 10.1038/ki.2015.201. [DOI] [PubMed] [Google Scholar]
- 19.Chauvet S, Frémeaux-Bacchi V, Petitprez F, et al. Treatment of B-cell disorder improves renal outcome of patients with monoclonal gammopathy-associated C3 glomerulopathy. Blood. 2017;129:1437–47. doi: 10.1182/blood-2016-08-737163. [DOI] [PubMed] [Google Scholar]
- 20.Gumber R, Cohen JB, Palmer MB, et al. A clone-directed approach may improve diagnosis and treatment of proliferative glomerul-onephritis with monoclonal immunoglobulin deposits. Kidney Int. 2018;94:199–205. doi: 10.1016/j.kint.2018.02.020. [DOI] [PubMed] [Google Scholar]
- 21.Chaudhry HM, Mauermann ML, Rajkumar SV. Monoclonal gammopathy-associated peripheral neuropathy: diagnosis and management. Mayo Clin Proc. 2017;92:838–50. doi: 10.1016/j.mayocp.2017.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yuki N, Uncini A. Acute and chronic ataxic neuropathies with disialosyl antibodies: a continuous clinical spectrum and a common pathophysiological mechanism. Muscle Nerve. 2014;49:629–35. doi: 10.1002/mus.24192. [DOI] [PubMed] [Google Scholar]
- 23.Doneddu PE, Cocito D, Manganelli F, et al. Atypical CIDP: diagnostic criteria, progression and treatment response. Data from the Italian CIDP Database. J Neurol Neurosurg Psychiatry. 2019;90:125–32. doi: 10.1136/jnnp-2018-318714. [DOI] [PubMed] [Google Scholar]
- 24.Rongioletti F, Merlo G, Carli C, et al. Histopathologic characteristics of scleromyxedema: a study of a series of 34 cases. J Am Acad Dermatol. 2016;74:1194–200. doi: 10.1016/j.jaad.2015.12.021. [DOI] [PubMed] [Google Scholar]
- 25.Mahévas T, Arnulf B, Bouaziz JD, et al. Plasma cell-directed therapies in monoclonal gammopathy-associated scleromyxedema. Blood. 2020;135:1101–10. doi: 10.1182/blood.2019002300. [DOI] [PubMed] [Google Scholar]
- 26.Dispenzieri A. Monoclonal gammopathies of clinical significance. Hematology Am Soc Hematol Educ Program. 2020;2020:380–8. doi: 10.1182/hematology.2020000122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Néel A, Henry B, Barbarot S, et al. Long-term effectiveness and safety of interleukin-1 receptor antagonist (anakinra) in Schnitzler's syndrome: a French multicenter study. Autoimmun Rev. 2014;13:1035–41. doi: 10.1016/j.autrev.2014.08.031. [DOI] [PubMed] [Google Scholar]
- 28.Krause K, Weller K, Stefaniak R, et al. Efficacy and safety of the interleukin-1 antagonist rilonacept in Schnitzler syndrome: an open-label study. Allergy. 2012;67:943–50. doi: 10.1111/j.1398-9995.2012.02843.x. [DOI] [PubMed] [Google Scholar]
- 29.Krause K, Bonnekoh H, Ellrich A, et al. Long-term efficacy of canakinumab in the treatment of Schnitzler syndrome. J Allergy Clin Immunol. 2020;145:1681–6. e5. doi: 10.1016/j.jaci.2019.12.909. [DOI] [PubMed] [Google Scholar]
- 30.Nelson CA, Zhong CS, Hashemi DA, et al. A multicenter cross-sectional study and systematic review of necrobiotic xanthogranuloma with proposed diagnostic criteria. JAMA Dermatol. 2020;156:270–9. doi: 10.1001/jamadermatol.2019.4221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Szalat R, Arnulf B, Karlin L, et al. Pathogenesis and treatment of xanthomatosis associated with monoclonal gammopathy. Blood. 2011;118:3777–84. doi: 10.1182/blood-2011-05-356907. [DOI] [PubMed] [Google Scholar]
- 32.Szalat R, Pirault J, Fermand JP, et al. Physiopathology of necrobiotic xanthogranuloma with monoclonal gammopathy. J Intern Med. 2014;276:269–84. doi: 10.1111/joim.12195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sykes DB, O'Connell C, Schroyens W. The TEMPI syndrome. Blood. 2020;135:1199–203. doi: 10.1182/blood.2019004216. [DOI] [PubMed] [Google Scholar]
- 34.Bazari H, Attar EC, Dahl DM, Uppot RN, Colvin RB. Case records of the Massachusetts General Hospital. Case 23-2010. A 49-year-old man with erythrocytosis, perinephric fluid collections, and renal failure. N Engl J Med. 2010;363:463–75. doi: 10.1056/NEJMcpc1004086. [DOI] [PubMed] [Google Scholar]
- 35.Kwok M, Korde N, Landgren O. Bortezomib to treat the TEMPI syndrome. N Engl J Med. 2012;366:1843–5. doi: 10.1056/NEJMc1202649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Schroyens W, O'Connell C, Sykes DB. Complete and partial responses of the TEMPI syndrome to bortezomib. N Engl J Med. 2012;367:778–80. doi: 10.1056/NEJMc1205806. [DOI] [PubMed] [Google Scholar]
- 37.Sykes DB, Schroyens W. Complete responses in the TEMPI syndrome after treatment with daratumumab. N Engl J Med. 2018;378:2240–2. doi: 10.1056/NEJMc1804415. [DOI] [PubMed] [Google Scholar]
- 38.Liang SH, Yeh SP. Relapsed multiple myeloma as TEMPI syndrome with good response to salvage lenalidomide and dexamethasone. Ann Hematol. 2019;98:2447–50. doi: 10.1007/s00277-019-03761-4. [DOI] [PubMed] [Google Scholar]
- 39.Desbois AC, Cacoub P, Saadoun D. Cryoglobulinemia: an update in 2019. Joint Bone Spine. 2019;86:707–13. doi: 10.1016/j.jbspin.2019.01.016. [DOI] [PubMed] [Google Scholar]
- 40.Druey KM, Parikh SM. Idiopathic systemic capillary leak syndrome (Clarkson disease) J Allergy Clin Immunol. 2017;140:663–70. doi: 10.1016/j.jaci.2016.10.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Xie Z, Chan EC, Long LM, Nelson C, Druey KM. High-dose intravenous immunoglobulin therapy for systemic capillary leak syndrome (Clarkson disease) Am J Med. 2015;128:91–5. doi: 10.1016/j.amjmed.2014.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]