Figure 1.
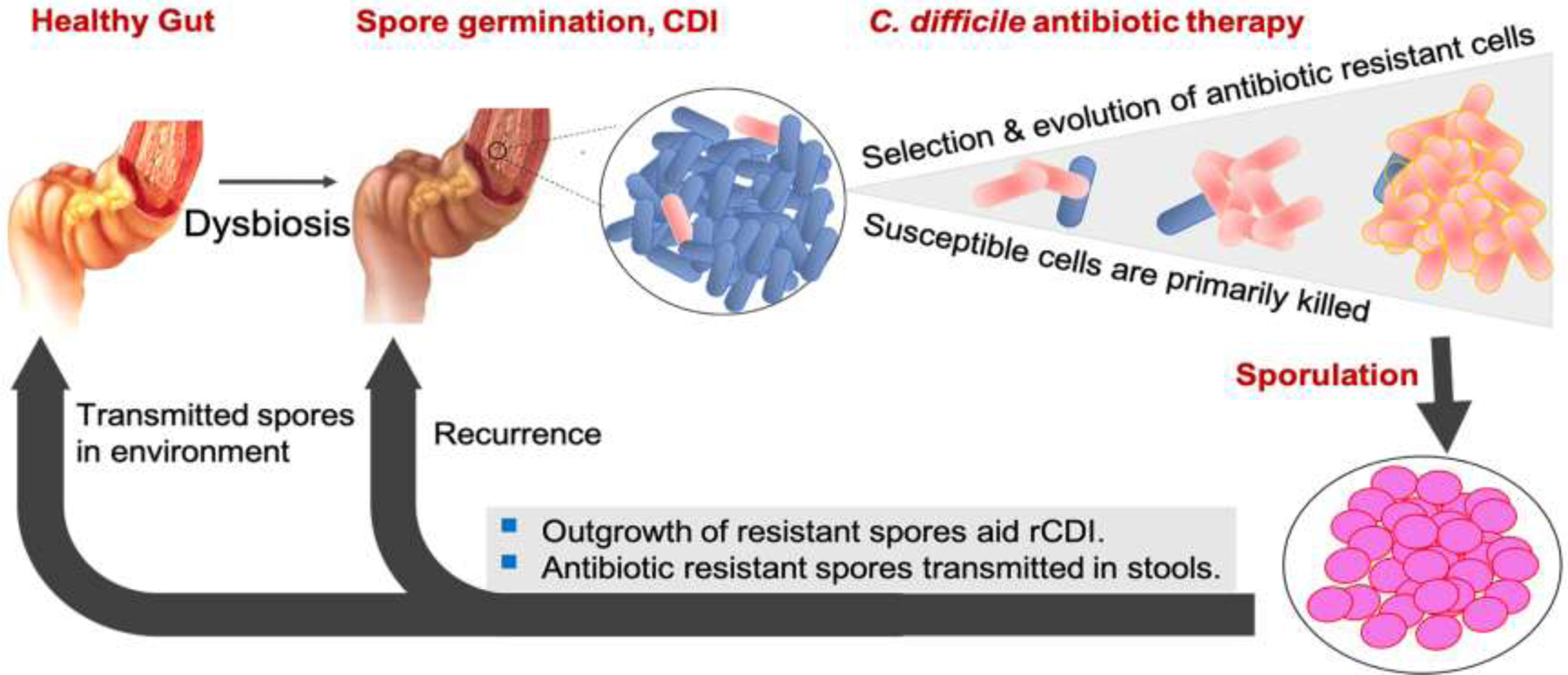
A Conceptual model demonstrating how genetic resistance to firstline antimicrobials could influence CDI recurrence. Resistant cells, including low-level resistant mutants, formed by spontaneous mutations could be selectively advantaged, even in drugs that achieve high luminal concentrations (e.g., fidaxomicin, vancomycin and rifaximin); low-level resistant mutants might be fitter than their wild type counterparts in niches with sub-physiological concentrations of drug. Sporulation by surviving low-level resistant cells increases the risk for recurrent disease. Drug-resistant spores transmitted in patient stools have an even higher likelihood of causing recurrence or acquiring further mutations that cause higher-level resistance and/or compensate for fitness costs. Strains with high-level resistance are better able to survive physiological concentrations of drug.
