Abstract
This study aims to critically appraise the quality of vasectomy-related health information currently available on YouTube to better address patient information needs moving forward. A YouTube search was performed using the keyword “vasectomy.” The first 100 videos were assessed, with irrelevant and duplicate videos excluded. Two independent reviewers evaluated the remaining videos using the DISCERN instrument for evaluating the quality of information and the Patient Education Materials Assessment Tool for Audiovisual materials (PEMAT-A/V) for assessing the understandability and actionability of materials. Source characteristics and markers of bias and misinformation were also collected. Seventy-eight videos were included in the study, with a mean duration of 6.6 minutes and mean of 216,672 views. The median DISCERN score was poor at 28 (IQR 22–33) out of a possible 80 with mean PEMAT-AV Understandability and Actionability scores of 67.6% (±16.7%) and 33.8% (±36.2%), respectively. A medical doctor was present in 61 (78.2%) of the videos, of which 53 (86.9%) were urologists and 38 (62.2%) promoted their personal practice or institution. False statements regarding vasectomy were made in 14 (17.9%) videos. Notably, no significant difference was noted in quality, understandability, or actionability of videos created by those with personal promotion to those without. The quality of information regarding vasectomy on YouTube is poor and reaches a wide audience. Continued appraisal and creation of YouTube videos that contain quality, understandable and actionable information by urologists is necessary to ensure patients are well-informed.
Keywords: consumer health information, Internet, quality assurance, health care, permanent contraception, reproductive, vasectomy
Introduction
Vasectomy is a safe and cost-effective form of permanent contraception in the United States (US). It is associated with failure rates (post-procedure pregnancy) of just 0.15% in the first year (Shih et al., 2011). Overall failure rates are comparable to long-term reversible female contraceptives and permanent female contraception methods, such as tubal ligation. Vasectomy is further advantageous in that it has fewer perioperative complications, requires only local rather than general anesthesia, involves less time off work, and is more cost-effective (Bartz & Greenberg, 2008; Shih et al., 2011; Hendrix et al., 1999; Trussell et al., 2009; “Vasectomy Guideline - American Urological Association,” 2015). Despite these advantages, vasectomy is less commonly used as a form of contraception in the United States. The rates of vasectomy are approximately one-third that of tubal ligation and have decreased in recent years (Shih et al., 2011; Ostrowski et al., 2018). Furthermore, disparities in utilization between racial/ethnic and socioeconomic groups exist. Men are significantly less likely to use vasectomy as a contraceptive method if they are single, non-white, have received less education, are of lower-economic status, or lack access to insurance (Barone et al., 2004; Shih et al., 2011).
Common misconceptions regarding vasectomies exist across all groups and include perceived increase in risk of prostate cancer, autoimmune disease, testicular cancer, and sexual dysfunction following the procedure, all of which have discredited (Shih et al., 2011). Misunderstandings and lack of knowledge regarding the procedure itself are also common (Shih et al., 2012). The prevalence of misconceptions represents an actionable step in the vasectomy decision-making process and amplifies the importance of quality, accessible patient information in the vasectomy decision-making process (Baldé et al., 2006; Labrecque et al., 2010).
The Internet, specifically, represents a widely accessible platform for patient education and support in the vasectomy decision-making process. As of 2012, 81% of all adults used the Internet, and nearly three-fourths (72%) of those had used the Internet for health information. (Fox & Duggan, 2013). As of 2019, the Internet use rate in adults had increased to 90%, and smartphone utilization was similar across racial groups at approximately 80% (Perrin & Anderson, 2019; Perrin & Turner, 2019). This improvement of accessibility to health-related content has created an unprecedented, rapidly expanding hub of health information which, although potentially beneficial, requires quality appraisal to ensure patients are accurately informed. YouTube, the popular video search engine used by nearly three-fourth of US adults, represents a particular challenge in ensuring quality of health-related information due to its demonstrated role in disseminating health-related misinformation (Perrin & Anderson, 2019; Perrin & Turner, 2019; Wang et al., 2019). This study aims to assess the quality of vasectomy-related information on YouTube to provide an appraisal of the site’s current state as an information source on vasectomy.
Methods
Search Strategy and Eligibility Screening
A YouTube search with the keyword “vasectomy” was conducted on May 18, 2020. The video title and URL of the first one hundred search results were recorded as this number encapsulates the most suggested videos while accounting for limited resources available for screening. One author viewed each video to assess for inclusion eligibility. Inclusion criteria included the following: videos describing vasectomy, vasectomy services, or vasectomy reversal. Exclusion criteria included the following: duplicate videos, videos not relevant to vasectomy with reason (e.g., TV episode on paternal court which mentions vasectomy), and videos describing vasectomy ancillary to another condition/intervention (e.g., penile implant and vasectomy following penile fracture).
Variable Extraction and Coding Process
Two validated health information evaluation tools for assessing information quality, understandability, and actionability (Supplementary Table 1) were used to evaluate the included videos. The DISCERN instrument measures the quality of consumer health information on treatment choices (Charnock et al., 1999; Charnock & Shepperd, 2004; Ernst et al., 2019). It employs 16 questions to evaluate the reliability and sourcing of information (Questions 1–8), specific details on information regarding treatment choices (Questions 9–15), and the overall quality rating of the material (Question 16). Questions are rated on a scale of one (No) to five (Yes) with two through four (Partial) representing varying degrees of completeness. Overall DISCERN scores are computed by summing the individual question scores, and the breakdown of their interpretation is included (Supplementary Table 1). The Patient Education Materials Assessment Tool (PEMAT), created by the Agency for Health care Research and Quality, allows for systematic evaluation and comparison of patient education materials through two key components: “understandability,” that is, it enables a diverse group of consumers with varying levels of health literacy to appreciate and describe key components, and “actionability,” that is, it enables this same group to identify pertinent next steps based on the materials presented (e.g., patients should refrain from sexual intercourse one week after their procedure; you should wear a jockstrap or supportive underwear for ample scrotal support after your procedure) (“PEMAT Tool for Audiovisual Materials (PEMAT-A/V,” 2013; Shoemaker et al., 2014). The PEMAT Tool for Audiovisual Materials (PEMAT-A/V), which utilizes thirteen items measuring “understandability” and 4 items measuring “actionability,” was used for this study. Materials are deemed “understandable” if at least 70% of the understandability items are met, and similar deemed “actionable” if at least 70% of the actionability items are met. In addition to the validated tools, video characteristics partially based on Schwen et al. (2020) were collected and are shown in Supplementary Table 2. Clinical variables based on the American Urological Association vasectomy guidelines, Canadian Urological Association guidelines and a systematic review on the safety and effectiveness of vasectomy, were also collected and include mention of early and/or late failure rate, mention of early complications (hematoma, infection, sperm granuloma, epididymitis–orchitis, and congestive epididymitis), mention of late complications (chronic scrotal pain and delayed vasectomy failure), mention of potential complication with prior varicocele, mention of pre-op sperm banking or in vitro fertilization following vasectomy, mention of post-vasectomy semen analysis or initial ineffective period, mention of reversal possibility, and mention of lack of sexually transmitted infection protection. (Supplementary Table 2) (Schwingl & Guess, 2000; “Vasectomy Guideline - American Urological Association,” 2015; Zini et al., 2016). All clinical variables were scored as no (0) or yes (1), and the total percentage meeting criteria for each item was computed. Summary statistics, Student’s t-test, and regression analyses to compare overall quality across different characteristic groups were then performed using Microsoft Excel and STATA 14 statistical software.
Inter-rater Reliability
Two independent evaluators, one medical student and one urology resident, coded the videos using the aforementioned tools. The primary coder (medical student) analyzed 100% of the videos of which the data were used for variable analysis. A random number generator in Google Sheets was then used to select 40% of the videos, which were then coded by the secondary reviewer to ensure inter-rater reliability. Interrater reliability (IRR) was calculated in Microsoft Excel using percent of absolute agreement and is shown in Supplementary Table 1. IRR for DISCERN was 61%, while IRR for PEMAT-AV (85%); IRR for study-specific characteristics (91%) was much higher. Because of the poor IRR reported for DISCERN, all included videos for DISCERN were rated by third reviewer and medical student, after which IRR remained at 60%. Despite this, however, mean DISCERN scores fell within two points (<1 standard deviation) across all raters.
Results
Video Selection and Characteristics
A total of 78 videos met inclusion criteria and were analyzed. Sixty-three (81%) videos focused specifically on vasectomy, fourteen video (18%) focused on vasectomy reversal, and one video (1%) was classified as “Other” (Video on IUD vs. Tubal Ligation vs. Vasectomy). The majority of video sources were hospital systems (n = 32, 41%) or private practice/physician groups (n = 25, 32%), while the remainder (n = 21, 27%) were posted by private companies or personal accounts. Videos were categorized as educational (n = 54, 69%), TV/news/radio (n = 8, 10%), personal experience or blog (n = 14, 18%), or advertisement (n = 2, 3%). Videos had a mean of 216,672 views with a total of 16,900,379 views and received a mean of 3,033 likes and 122 dislikes per video. The mean video duration was six minutes and thirty-five seconds. Sixty-one (78%) videos included a medical doctor, of which 53 (87%) were urologists. Of the videos including physicians, 38 (62%) promoted their personal practice or institution. False statements were made by both physicians and vloggers (video bloggers) in 13 (17%) videos and were mostly characterized by an underscoring of risks associated with vasectomy, claim of immediate effect without mentioning the post-vasectomy ineffective period, and falsely low vasectomy reversal rates.
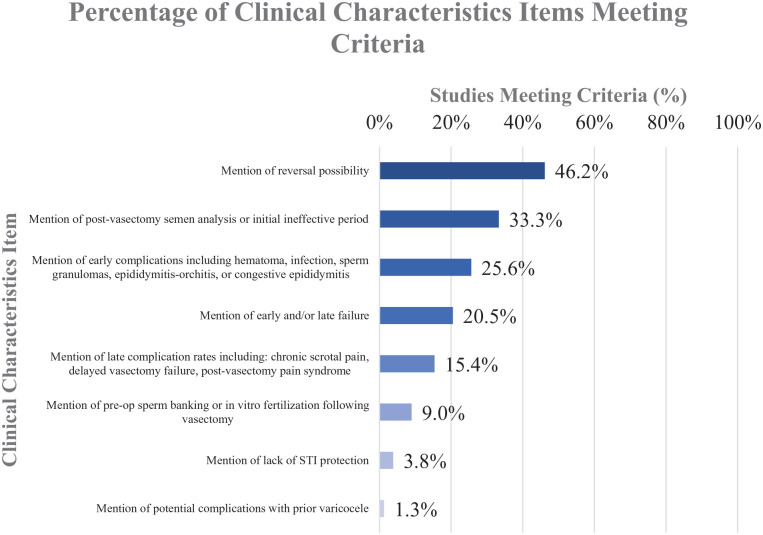
Mention of Clinical Criteria
As for clinical information related to vasectomy discussed in the videos, individual item percentages were low, with none surpassing the 50% threshold. The lowest scoring item was mention of complications with a prior varicocele at 1.3%, while the highest scoring item was mention of reversal possibility at 46.2%. The individual item breakdown is shown in Figure 1.
Figure 1.
Percentage of Clinical Criteria Items Mentioned by Individual Item.
Quality, Understandability, and Actionability Results
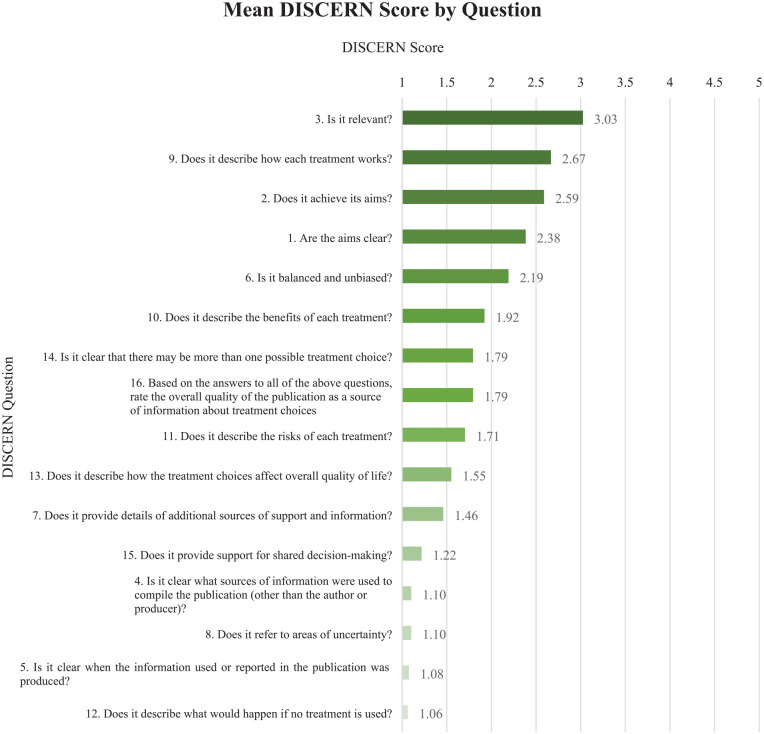
DISCERN
DISCERN score interpretations are shown in Supplementary Table 1. Across all videos, the median DISCERN score was 28 (IQR 22–33) with a mean (SD) of 28.7 (±7.3), constituting “poor” quality of overall evidence. Scores ranged from 15 (“very poor”) for videos #4 and #61 to 46 (“fair”) for videos #35 and #62 (Supplementary Table 3). Nine videos (11.5%) received scores in the “fair” range, while the remaining videos were scored as “poor” (scoring is shown in Supplementary Table 1).
The individual questions and statistics are shown in Figure 2. Overall question performance was low. The highest performing question across videos was question 3, “Is it relevant”?, while the lowest scoring questions were “Is it clear when the information used or reported in the publication was produced?” and “Does it describe what would happen if no treatment is used?.” Scores on questions measuring use of sources and areas of uncertainty were generally low, while questions on aims of the video, description of how the treatment works, and relevance performed best. Videos with a main focus on vasectomy (28.7±7.3) had no significant differences in mean (±SD) scores to those focused on vasectomy reversal (28.6±7.7) (p=.95). The video with the most overall views (Video 22) at 6,441,400 had a score of 20, which is considered “very poor” quality. Videos in which the physician promoted their personal practice or institution demonstrated no significant difference in mean DISCERN score in comparison with those without.
Figure 2.
Mean DISCERN Score by Individual Question.
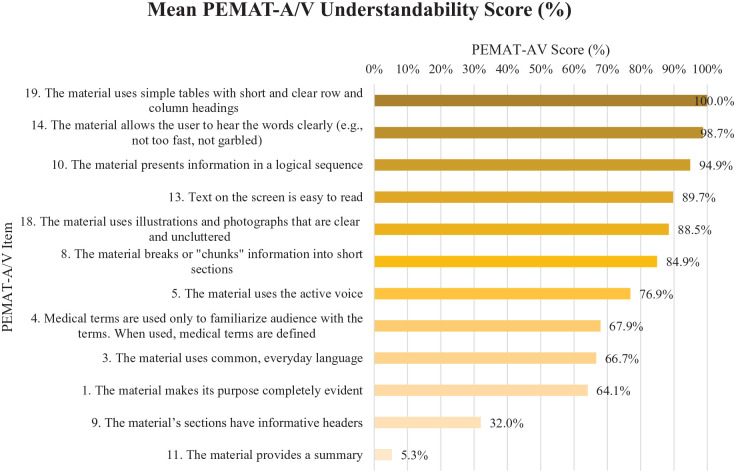
PEMAT-A/V Understandability
The mean (SD) PEMAT-A/V Understandability score for the videos was 67.6% (±16.9%) of criteria met. Scores ranged from 22.2% to 100% of criteria met, as shown in Supplementary Table 3. The majority of the videos (55.1%) met overall understandability criteria (≥70% of criteria met). The individual item breakdown is shown in Figure 3. The highest scoring items were item 19, “The material uses simple tables with short and clear row and column headings” and item 14, “The material allows the user to hear the words clearly,” at 100% and 98.7%, respectively. The lowest scoring item was item 11, “The material provides a summary,” at only 5.3%. Videos focusing on vasectomy had no significant difference in mean understandability score at 68.2% (±17.5%) vs. 64.2% (±15.1%) for vasectomy reversal (p=.39).
Figure 3.
Mean PEMAT-A/V Understandability Percentage of Criteria Met for Each Individual Item. Note, Item 19 Only Applies to Videos Which Include Tables in the Video (n = 1).
Note. PEMAT-A/V = Patient Education Materials Assessment Tool for Audiovisual materials.
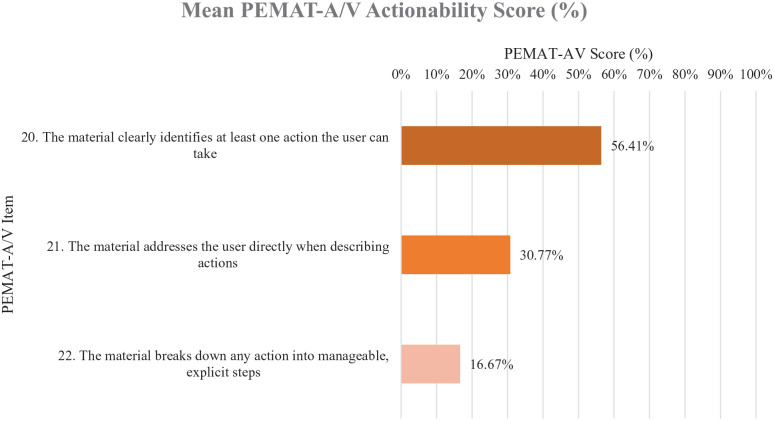
PEMAT-A/V Actionability
PEMAT-A/V actionability scores were much lower compared to understandability scores, with a mean (SD) of 33.8% (±36.2%). Scores ranged from 0 (n = 34) to 100% (n = 10), with only 7.8% of videos meeting overall actionability criteria (≥70% of criteria met). The individual item breakdown is shown in Figure 4. Item 20, “The material clearly identifies at least one action the user can take,” scored the highest at 56.4%, while item 22, “The material breaks down any action into manageable”, explicit steps at only 16.7% of videos meeting criteria. Videos focusing on vasectomy demonstrated no significant difference to those at 32.8% (±36.3%) vs. 38.1% (±41.0%) for vasectomy reversal (p=.66).
Figure 4.
Mean PEMAT-A/V Actionability Score for Each Individual Item.
Note. PEMAT-A/V = Patient Education Materials Assessment Tool for Audiovisual materials.
Regression Analysis
There was a significant positive correlation (p < .001) between DISCERN scores and both PEMAT-AV Understandability and Actionability scores. No other significant correlations were noted, including the relationships between views and validated tools.
Top-Rated Videos
Supplementary Table 4 includes the video title, URL, and scores from validated tools of the top-performing videos rated “fair” by DISCERN criteria.
Discussion
This work expands upon prior assessments of vasectomy-related information on the Internet. A 2003 study assessed search engine performance on vasectomy procedure results without using validated tools, while a 2018 study assessed online vasectomy discussion boards for common themes without using validated tools (Murphy et al., 2003; Samplaski, 2018). To the authors’ knowledge, our report is the only report using validated tools or specifically assessing YouTube as a source of vasectomy-related information.
We noted an inadequate overall quality of vasectomy-related information on YouTube. Videos consistently failed to meet criteria across the two validated tools. DISCERN scores represented “poor” quality of information in the selected videos, with no videos rated “good” or “excellent.” The videos receiving a score of “fair” are shown in Supplementary Table 4 and represent the highest quality of available patient information on YouTube evaluated in our study. Videos severely underperformed in terms of PEMAT-A/V Actionability criteria, demonstrating a lack of actionable items for patients to take in the vasectomy decision-making process. The rating of the most viewed video in our study as “very poor” quality was especially concerning. These results are consistent with the findings from Schwen et al., Ernst et al., a systematic review on quality of health information on the Internet by Daraz et al., and a recent study by Szmuda et al. focusing on quality of health information on YouTube specifically for COVID-19, which all demonstrate a current state of suboptimal quality of health information on the Internet (Daraz et al., 2020; Ernst et al., 2019; Schwen et al., 2020; Szmuda et al., 2020).
Despite this, several strengths of information assessed in our study were noted. A majority of videos met PEMAT-A/V Understandability criteria and videos were generally relevant and described each treatment to fairly well, based on DISCERN scores. In addition, nearly half of the videos mentioned the possibility of reversal if desired, and over half of videos identifying at least one discrete action in the vasectomy process the user can take. These strengths must be incorporated and improved upon in future dissemination of vasectomy-related information on the Internet.
Continued regulation of this information, however, is essential to ensure patients are accurately informed. The prevalence of misinformation through false statements made by physicians in our study, consisting mostly of falsely low risks and complications, along with the high personal promotion rate of videos and the low rates of mention of clinical characteristics (of which were predominantly risks) is especially concerning in that it may promote vasectomy utilization for physician or practice benefit rather than those of the patient. It is also important to note that although some videos included in the study were not intended for educational use, the algorithm used by YouTube for video results does not currently filter videos by genre (such as promotion, personal blog, or education), which makes all videos equally likely to be returned during a search query when keeping other factors such as views constant. This introduces patient susceptibility to biased and misinformed videos into the search process, which is why all videos with vasectomy as the primary focus were rated as equal. For this reason, initial search results returning vasectomy reversal were also included in the analysis, as they could have undue effect on the vasectomy decision-making process.
Regarding utilization rates, ensuring adequate knowledge represents an equitable intervention point to increasing awareness and understanding of vasectomy as a form of contraception across groups. When controlling for socioeconomic and educational factors, racial disparities in utilization predominate. Black and Latino males are 80% and 60% less likely to have a vasectomy than white males, respectively, while black (22%) and Latina females (20%) undergo permanent contraceptive procedures at much higher rates compared with black (1%) and Latino (3%) males (Eisenberg et al., 2009; Shih et al., 2011). Rates of knowledge of what a vasectomy is have been demonstrated to be lower in Latino males (54%) compared with white males (96%) (Shih et al., 2012) Similarly, black females (58.9%) have more frequently endorsed the notion that tubal ligation reversal could easily restore fertility than white females (39.7%), both of which coincide with overall utilization rates (Shih et al., 2012). Perceived ease of reversibility of female permanent contraceptive procedures is also a common misconception that has specifically been associated with black and Latino couples (Shih et al., 2012). These disparities only amplify the importance of dissemination of quality health information on the Internet, especially when noting that black and Latino users are less likely to seek information from a doctor or other healthcare professional and more likely to rely on their smartphone to seek health information than white users (Fox & Duggan, 2013). It is also worth mentioning that there are notable income-based disparities in the use of male and female permanent contraceptive procedures, and, although equitable access to the Internet has improved in recent years, disparities persist and equitable targets for improving rates of vasectomy usage across low-income groups must be considered.
There are several limitations of this study. First, the fluidity of the information sources paired with the constantly evolving nature of YouTube as a search engine could render some of the results in this study outdated, further demonstrating the need for ongoing information evaluation. Second, DISCERN scores, especially in the partial (2–4) range, are subjective and could have an impact on overall scoring. The relatively low inter-rater reliability for DISCERN scores reflects this limitation and findings using this tool must be interpreted with this considered. Third, DISCERN has not been validated in this setting, as it was originally intended for written materials. However, most of the quality characteristics it employs in rating materials are not specific to written materials, which has allowed for the use of DISCERN as a tool for measure of quality in a number of previous studies (Daraz et al., 2020). Fourth, this study does not assess whether the videos achieve certain cultural competencies or if there is a certain level of educational attainment needed to comprehend the information presented other than the PEMAT-A/V Understandability score, and furthermore, ratings were determined by two medical students and a urology resident with presumed health literacy above that of the general population and thus could influence ratings. Further studies assessing these factors could categorize the accessibility of the information regarding vasectomy on YouTube (Sun et al., 2019). Fifth, mention of effects on sexual function including vasectomy’s effect on sexual desire, the ability to get/maintain an erection, the ability to have an orgasm, and return to sexual activity, were not assessed and should be further explored in future studies. The measured clinical characteristics were chosen specifically for this study, and their validity as a tool must be substantiated if they are to be used in future studies. Sixth, race/ethnicity of patients and physicians were not evaluated due to potential bias inherent in perceived race as determined by the raters, and should be evaluated in further studies using community stakeholders to determine consensus on perceived race of different individuals present in videos.
Conclusions
The quality of most vasectomy-related information on YouTube is inadequate with undesirable rates of misinformation. Accurate portrayal of risks and benefits in an understandable manner, along with concrete actions the patient can take in the vasectomy decision-making process, are important steps in equitably improving knowledge and dispelling misconceptions regarding vasectomy.
Supplemental Material
Supplemental material, sj-docx-1-jmh-10.1177_15579883221094716 for Assessing Vasectomy-Related Information on YouTube: An Analysis of the Quality, Understandability, and Actionability of Information by Jacob J. Lang, Zane Giffen, Stephen Hong, Jonathan Demeter, Ahmed El-Zawahry, Puneet Sindhwani and Obi Ekwenna in American Journal of Men’s Health
Footnotes
Author Contributions: Conceptualization: O.E., Z.G., J.L., A.E.-Z., P.S.
Data curation: J.L., Z.G., S.H., J.D.
Formal analysis: J.L., Z.G.
Methodology: J.L., Z.G., O.E.
Project administration: O.E., Z.G.
Supervision: O.E., P.S.
Validation: J.L., Z.G., S.H., J.D.
Visualization: J.L.
Writing—original draft: J.L., Z.G., Writing—review & editing, Investigation: All Authors.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethics Statement: This study was determined to be exempt from institutional review board review as it does not use human subject information.
ORCID iD: Jacob J. Lang  https://orcid.org/0000-0003-0956-3021
https://orcid.org/0000-0003-0956-3021
Supplemental Material: Supplemental material for this article is available online.
References
- Baldé A., Légaré F., Labrecque M. (2006). Assessment of needs of men for decision support on male sterilization. Patient Education and Counseling, 63(3), 301–307. 10.1016/j.pec.2006.04.010 [DOI] [PubMed] [Google Scholar]
- Barone M. A., Johnson C. H., Luick M. A., Teutonico D. L., Magnani R. J. (2004). Characteristics of men receiving vasectomies in the United States, 1998-1999. Perspectives on Sexual and Reproductive Health, 36(1), 27–33. 10.1363/psrh.36.27.04 [DOI] [PubMed] [Google Scholar]
- Bartz D., Greenberg J. A. (2008). Sterilization in the United States. Reviews in Obstetrics and Gynecology, 1(1), 23–32. [PMC free article] [PubMed] [Google Scholar]
- Charnock D., Shepperd S., Needham G., Gann R. (1999). DISCERN: An instrument for judging the quality of written consumer health information on treatment choices. Journal of Epidemiology and Community Health, 53(2), 105–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charnock D., Shepperd S. (2004). Learning to DISCERN online: Applying an appraisal tool to health websites in a workshop setting. Health Education Research, 19(4), 440–446. 10.1093/her/cyg046 [DOI] [PubMed] [Google Scholar]
- Daraz L., Morrow A. S., Ponce O. J., Beuschel B., Farah M. H, Katabi A., Alsawas M., Majzoub A. M., Benkhadra R., Seisa M. O., Ding J., Prokop L., Murrad M. H. (2020). Can patients trust online health information? A meta-narrative systematic review addressing the quality of health information on the internet. Journal of General Internal Medicine, 34(9), 1884–1891. 10.1007/s11606-019-05109-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenberg M. L., Henderson J. T., Amory J. K., Smith J. F., Walsh T. J. (2009). Racial differences in vasectomy utilization in the United States: Data from the National Survey of Family Growth. Urology, 74(5), 1020–1024. 10.1016/j.urology.2009.06.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ernst M. M., Chen D., Kennedy K., Jewell T., Sajwani A., Foley C., Sandberg D. E. (2019). Disorders of sex development (DSD) web-based information: Quality survey of DSD team websites. International Journal of Pediatric Endocrinology, 2019, Article 1. 10.1186/s13633-019-0065-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox S., Duggan M. (2013). Health online 2013. Pew Research Centre. https://www.pewresearch.org/internet/2013/01/15/health-online-2013/
- Hendrix N. W., Chauhan S. P., Morrison J. C. (1999). Sterilization and its consequences. Obstetrical & Gynecological Survey, 54(12), 766–777. 10.1097/00006254-199912000-00005 [DOI] [PubMed] [Google Scholar]
- Labrecque M., Paunescu C., Plesu I., Stacey D., Légaré F. (2010). Evaluation of the effect of a patient decision aid about vasectomy on the decision-making process: A randomized trial. Contraception, 82(6), 556–562. 10.1016/j.contraception.2010.05.003 [DOI] [PubMed] [Google Scholar]
- Murphy J. O., Sweeney K. J., O’Mahony J. C., Johnston S. M., Conlon K., Keane F. B., Tierney S. (2003). Surgical informatics on the internet: Any improvement? The Surgeon, 1(3), 177–179. 10.1016/s1479-666x(03)80100-2 [DOI] [PubMed] [Google Scholar]
- Ostrowski K. A., Holt S. K., Haynes B., Davies B. J., Fuchs E. F., Walsh T. J. (2018). Evaluation of vasectomy trends in the United States. Urology, 118, 76–79. 10.1016/j.urology.2018.03.016 [DOI] [PubMed] [Google Scholar]
- PEMAT Tool for Audiovisual Materials (PEMAT-A/V). (2013). https://www.ahrq.gov/ncepcr/tools/self-mgmt/pemat-av.html
- Perrin A., Anderson M. (2019). Share of U.S. adults using social media, including Facebook, is mostly unchanged since 2018. Pew Research Centre. https://www.pewresearch.org/fact-tank/2019/04/10/share-of-u-s-adults-using-social-media-including-facebook-is-mostly-unchanged-since-2018/
- Perrin A., Turner E. (2019). Smartphones help blacks, Hispanics bridge some—but not all—digital gaps with whites. Pew Research Centre. https://www.pewresearch.org/fact-tank/2019/08/20/smartphones-help-blacks-hispanics-bridge-some-but-not-all-digital-gaps-with-whites/
- Samplaski M. K. (2018). A thematic analysis of online discussion boards for vasectomy. Urology, 111, 32–38. 10.1016/j.urology.2017.06.061 [DOI] [PubMed] [Google Scholar]
- Schwen Z., Patel H., Biles M., Cheaib J., Alam R., Pavlovich C. (2020). PD09-12 AN EVALUATION OF MISINFORMATION FOR ERECTILE DYSFUNCTION FOLLOWING RADICAL PROSTATECTOMY ON YOUTUBE. The Journal of Urology, 203(Suppl. 4), e179–e179. 10.1097/JU.0000000000000836.012 [DOI] [Google Scholar]
- Schwingl P. J., Guess H. A. (2000). Safety and effectiveness of vasectomy. Fertility and Sterility, 73(5), 923–936. 10.1016/s0015-0282(00)00482-9 [DOI] [PubMed] [Google Scholar]
- Shih G., Dubé K., Sheinbein M., Borrero S., Dehlendorf C. (2012). He’s a real man: A qualitative study of the social context of couples’ vasectomy decisions among a racially diverse population. American Journal of Men’s Health, 7(3), 206–213. 10.1177/1557988312465888. [DOI] [PubMed] [Google Scholar]
- Shih G., Turok D. K., Parker W. J. (2011). Vasectomy: The other (better) form of sterilization. Contraception, 83(4), 310–315. 10.1016/j.contraception.2010.08.019 [DOI] [PubMed] [Google Scholar]
- Shoemaker S. J., Wolf M. S., Brach C. (2014). Development of the atient Education Materials Assessment Tool (PEMAT): A new measure of understandability and actionability for print and audiovisual patient information. Patient Education and Counseling, 96(3), 395–403. 10.1016/j.pec.2014.05.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun Y., Zhang Y., Gwizdka J., Trace C. B. (2019). Consumer evaluation of the quality of online health information: Systematic literature review of relevant criteria and indicators. Journal of Medical Internet Research, 21(5), Article e12522. 10.2196/12522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szmuda T., Syed M. T., Singh A., Ali S., Özdemir C., Słoniewski P. (2020). YouTube as a source of patient information for coronavirus disease (COVID-19): A content-quality and audience engagement analysis. Reviews in Medical Virology, 30(5), Article e2132. 10.1002/rmv.2132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trussell J., Lalla A. M., Doan Q. V., Reyes E., Pinto L., Gricar J. (2009). Cost effectiveness of contraceptives in the United States. Contraception, 79(1), 5–14. 10.1016/j.contraception.2008.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vasectomy Guideline—American Urological Association. (2015). https://www.auanet.org/guidelines/vasectomy-guideline#x3371
- Wang Y., McKee M., Torbica A., Stuckler D. (2019). Systematic literature review on the spread of health-related misinformation on social media. Social Science & Medicine, 240, Article 112552. 10.1016/j.socscimed.2019.112552 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zini A., Grantmyre J., Chan P. (2016). CUA guideline: Vasectomy. Canadian Urological Association Journal, 10, E274–E278. 10.5489/cuaj.4017 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-jmh-10.1177_15579883221094716 for Assessing Vasectomy-Related Information on YouTube: An Analysis of the Quality, Understandability, and Actionability of Information by Jacob J. Lang, Zane Giffen, Stephen Hong, Jonathan Demeter, Ahmed El-Zawahry, Puneet Sindhwani and Obi Ekwenna in American Journal of Men’s Health