Abstract
COVID-19 vaccines have been available for over a year, yet 26% of U.S. young adults remain unvaccinated. This study examines racial and ethnic disparities in young adult vaccine hesitancy and attitudes/beliefs that mediate disparities in vaccine hesitancy. Young adults (n = 2041;Mean[SD]:21.3[0.7] years-old) from a Los Angeles, CA, USA cohort were surveyed online in January–May 2021 and classified as vaccine hesitant (those who reported “Not at all likely”/“Not very likely” /“Slightly likely” to get vaccinated) versus non-hesitant (those who reported “Moderately likely”/”Very likely”/”Definitely likely” to get vaccinated or already vaccinated). Multivariable logistic regression was performed to examine racial/ethnic disparities in vaccine hesitancy. Factor analysis was conducted to create three subscales toward vaccination: positive, negative, and lack-of-access beliefs. Mediation analyses were performed to assess pathways from attitude/belief subscales to racial disparities in vaccine hesitancy. Overall 33.0% of respondents reported vaccine hesitancy. Black vs. White young adults had a higher prevalence of vaccine hesitancy (AOR[95%CI] = 4.3[2.4–7.8]), and Asians vs. Whites had a lower prevalence (AOR[95%CI] = 0.5[0.3–0.8]). Mediators explained 90% of the Black (vs. White) disparity in vaccine hesitancy, including significant indirect effects through positive belief–reducing (β = 0.23,p < .001) and negative belief–enhancing (β = 0.02,p = .04) effects. About 81% of the Asian (vs. White) disparity in vaccine hesitancy was explained by the three combined subscales, including significant positive belief–reducing (β = −0.18,p < .001) indirect effect. Substantial racial and ethnic disparities in young adult COVID-19 vaccine hesitancy were found, which were mediated by differences in attitudes and beliefs toward vaccination. Targeted education campaigns and messages are needed to promote equitable utilization of the effective vaccine.
Keywords: COVID-19, Vaccine hesitancy, Race/ethnicity, Attitude and belief, Young adults
1. Introduction
As of February 2, 2022, the coronavirus disease 2019 (COVID-19) pandemic has resulted in over 75 million cases and 895,000 deaths in the United States (Dong et al., 2020; The Centers for Disease Control and Prevention, 2020) with young adults having the highest cumulative infection incidence nationwide (The Centers for Disease Control and Prevention, 2021a). COVID-19 is infecting and killing racial minorities at a disproportionately high rate (Gold et al., 2020; Lopez 3rd et al., 2021). Blacks and Hispanics have experienced nearly three times higher rates of hospitalization and two times higher rates of deaths from COVID-19 than their White peers (The Centers for Disease Control and Prevention, 2021b).
The vaccines that are being disseminated in the U.S. have shown high efficacy against COVID-19, and a high vaccination rate is critical to avoid excess hospitalizations and deaths. About 73.6% of U.S. adults aged 18 years and older were fully vaccinated, and 87.0% received at least one dose as of January 2022 (The Centers for Disease Control and Prevention, 2021c). Young adults and racial minorities reported the lowest vaccine uptake and the lowest intent to get vaccinated (Baack et al., 2021; Daly et al., 2021; Thompson et al., 2021). It is estimated that 59.8% of adults aged 18 to 24 were fully vaccinated, and 74.0% received at least one dose compared to 79.0% and 91.5% for adults aged between 50 and 64 years old, respectively (The Centers for Disease Control and Prevention, 2021c). Meanwhile, African Americans had the highest vaccine hesitancy among all racial/ethnic groups among adults of all ages. A national study (Daly et al., 2021) estimated that 43.0% of Black adults reported that they were unsure or somewhat/unlikely to get vaccinated (vaccine hesitancy) compared to 36.4% of Hispanics, 34.8% of Whites, and 20.4% of other races in March 2021. However, no studies have assessed racial disparities in vaccine hesitancy among young adults, a priority population to manage COVID-19 transmission and control community spread. Furthermore, some important measures that particularly influence young adults' behaviors (Skinner et al., 2015; Zampetakis and Melas, 2021), such as risk-taking propensities (e.g., drug use, impulsive behavior) or perceived COVID-19 susceptibility, were not fully adjusted in existing studies on vaccine hesitancy (Daly et al., 2021; Paul et al., 2021; Szilagyi et al., 2021).
The primary barrier to vaccination has shifted from access to hesitancy after all U.S. adults became eligible for vaccines on April 19, 2021 (NRP.org, 2021). Unvaccinated people account for a vast majority of patients hospitalized for COVID-19 (Evans and Wernau, 2021). Previous research and health behavior theory have identified key domains of determinants that influence the uptake of vaccines against other diseases (e.g., influenza) (Corace et al., 2016; Schmid et al., 2017). Beliefs about the expected consequences of vaccination could either facilitate or impede vaccination. For instance, positive beliefs of the importance of vaccines in the protection and prevention of virus spreading in the community are related to high vaccination uptake or intent to get vaccinated (Baack et al., 2021; Schmid et al., 2017). Negative beliefs, such as medical mistrust or concern over side effects from vaccination, are strongly related to vaccine hesitancy, especially among Black adults (Paul et al., 2021; Szilagyi et al., 2021; Thompson et al., 2021). Misinformation and disinformation on the COVID-19 vaccine are widespread on social media networks (Basch et al., 2021; Islam et al., 2021) and can further amplify negative beliefs of vaccine effectiveness (Wilson and Wiysonge, 2020). Lack of access or lack of knowledge also contributes to low intent to get vaccinated (Schmid et al., 2017). For instance, uninsured individuals may have concerns about the cost of vaccines (Takayama et al., 2012) even though the COVID-19 vaccines are free in the United States. However, no prior studies have examined whether and to what extent these attitudes/beliefs may mediate racial disparities in vaccine hesitancy. Such information is important to public health so that precision interventions can be developed and implemented to increase vaccine uptake among vulnerable populations.
This study examined racial/ethnic differences in COVID-19 vaccine hesitancy in a cohort of young adults and further assessed whether certain attitudes and beliefs about COVID-19 vaccination statistically mediated racial/ethnic disparities in vaccine hesitancy.
2. Methods
2.1. Data collection
Data were drawn from a prospective cohort survey of health behavior which originally recruited 9th-grade students in Los Angeles, CA, USA schools in 2013 (n = 3396) (Leventhal et al., 2015). Participants were followed semi-annually in the classroom (paper-and-pencil surveys) from 2013 to 2017 and online after 2017. This study included participants who completed the online questionnaire from the most recent wave of data collection (January 2021 to May 2021, N = 2077, retention = 61.2% of baseline participants), and responses from this wave were analyzed cross-sectionally in the current study. This study was approved by the University of Southern California Institutional Review Board and informed consent was obtained from all participants prior to data collection.
2.2. Measures
Vaccine Hesitancy: Participants were asked whether they had received at least one dose of the COVID-19 vaccine. Those who responded “No” were further asked “If the COVID-19 vaccine were easily available to you, how likely would you be to get it?” with response options “Not at all likely,” “Not very likely,” “Slightly likely,” “Moderately likely,” “Very likely,” and “Definitely likely.” Respondents were classified as being hesitant to get vaccinated (not at all likely/not very slightly/slightly likely) or non-hesitant to get vaccinated (moderately likely/very likely/definitely likely or already vaccinated). To ensure a robust outcome, we performed three separate sensitivity analyses to test different vaccine hesitancy definitions. First, we excluded those already vaccinated (n = 238) in the analytical sample since a majority of them in the current study were vaccinated between January and March 2021 (see eFig. 1 footnote) and they were likely to be different from those not yet vaccinated; Second, we created a secondary vaccine hesitancy definition that included those responding to “slightly likely” in the non-hesitant group; Third, a raw continuous variable based on the selection of each of the response categories indicative of the magnitude of vaccine hesitancy ranging from 1 (“Already vaccinated”) to 7 (“Not at all likely”) was also analyzed.
Attitudes and beliefs about vaccine uptake: Participants were asked how much they agree or disagree with 19 statements measuring their attitudes and beliefs about COVID-19 vaccines (See Table 1 for each item) with a 5-point Likert scale (“Strongly disagree” [scored = 1], “Disagree” [=2], “Neutral” [=3], “Agree” [=4], and “Strongly disagree” [=5]), which were based on past work (Callaghan et al., 2021; Corace et al., 2016). An exploratory oblique factor analysis of responses found a three-factor solution with 4 items producing no strong loadings on any factor (<0.5) (SAS Institute Inc, 2019) and the remaining items having strong factor loadings on only one of the 3 factors (see Table 1). After dropping the 4 items, responses on the remaining 15 items were used to compute three distinct subscales which were scored based on the mean (range: 1–5) of items within each factor construct: (1) positive vaccine beliefs (7 items, Cronbach alpha = 0.93; e.g., “I believe it is important for everyone to take the COVID-19 vaccine to help end the pandemic”); (2) negative vaccine beliefs (5 items, alpha = 0.90; e.g., “I worry that the vaccine might cause long term health effects for me”); and (3) lack-of-access beliefs (3 items, alpha = 0.80; e.g., “I am concerned I can't get the vaccine because I don't have health insurance, or my insurance won't cover the vaccine.”)
Table 1.
Factor loading for attitudes and beliefs about vaccine hesitancy.
| Factor loadings4 |
||||
|---|---|---|---|---|
| Statement | Description | Factor 1-positive beliefs1 | Factor 2-negative beliefs2 | Factor 3-lack-of-access beliefs3 |
| 1 | The vaccine could protect me against getting COVID-19. | 0.81 | 0.03 | 0.02 |
| 2 | If I get the vaccine, that could protect my family and friends from getting COVID-19. | 0.79 | 0.10 | 0.06 |
| 3 | I worry that the vaccine might cause some unpleasant side effects. | 0.23 | 0.92 | −0.12 |
| 4 | I worry that the vaccine might cause long term health effects for me. | 0.05 | 0.95 | −0.06 |
| 5 | I worry that the vaccine might cause more harm than getting COVID-19. | −0.16 | 0.80 | 0.04 |
| 6 | If enough other people get the vaccine, I do not need to get it. | −0.23 | 0.36 | 0.30 |
| 7 | I am worried that the vaccine was developed too quickly. | −0.05 | 0.77 | −0.01 |
| 8 | I am worried that I could get sick with COVID-19 by taking the vaccine. | −0.05 | 0.59 | 0.12 |
| 9 | I would get a vaccine for COVID-19 if it was available for free to anyone who wanted it. | 0.86 | −0.01 | 0.05 |
| 10 | I believe it is important for everyone to take the COVID-19 vaccine to help end the pandemic. | 0.94 | 0.03 | 0.01 |
| 11 | Getting the COVID-19 vaccine is important so I can see my friends and family. | 0.94 | 0.06 | 0.02 |
| 12 | Getting the COVID-19 vaccine is important so I can go to bars, clubs, and restaurants. | 0.69 | 0.02 | 0.12 |
| 13 | I trust that the U.S. government approval of the vaccine means it is safe and effective. | 0.69 | −0.21 | 0.12 |
| 14 | I am not afraid of COVID-19, so I don't think getting a vaccine is necessary. | −0.38 | 0.11 | 0.41 |
| 15 | I am concerned I can't get the vaccine because I don't have health insurance, or my insurance won't cover the vaccine. | 0.17 | −0.05 | 0.72 |
| 16 | I am concerned I can't get the vaccine because I don't know where or how to get the vaccine. | 0.26 | −0.11 | 0.78 |
| 17 | Trying to get the vaccine is too complicated or is too much trouble. | 0.06 | 0.04 | 0.70 |
| 18 | I don't plan to get the vaccine because I don't trust doctors. | −0.34 | 0.19 | 0.47 |
| 19 | I don't need to get the vaccine because I am young and healthy. | −0.38 | 0.12 | 0.49 |
Bold indicated factor loading >0.5 and included in subscale.
Positive belief factor: Sum of items 1, 2, 9, 10, 11, 12, and 13. Cronbach coefficient alpha = 0.93.
Negative belief factor: Sum of items 3, 4, 5, 7, and 8. Cronbach coefficient alpha = 0.90.
Lack-of-access belief factor: Sum of items 15, 16, and 17. Cronbach coefficient alpha = 0.80.
Items 6, 14, 18, and 19 were dropped from final scoring they did not load onto any factor ≥ 0.5. Total eigenvalues = 11.6. Eigenvalues (proportion of total) for: Positive belief factor = 7.5 (64.1%), negative belief factor = 2.6(22.7%) and lack-of-access factor = 1.5(13.2%). The Pearson inter-correlation coefficients among these 3 subscales: −0.42 between positive beliefs and negative beliefs (p < .0001), 0.05 between positive beliefs and lack-of-access beliefs (p = .02), and 0.18 between positive beliefs and lack-of-access beliefs (p < .0001).
Race and ethnicity: Participants were asked to select one race and ethnicity status that best describes them. Given the small sample size in some cells, we grouped race and ethnicity into 5 categories: White, Black, Hispanic, Asian, and other (those who reported “American Indian or Alaska Native,” “Native Hawaiian or Pacific Islander,” “Multiracial,” or “Other.”)
Covariates: To adjust for potential confounding effects, we included a variety of covariates:
Survey months: January–May 2021 were coded as a categorical variable (1–5).
Sociodemographic covariates: self-reported age (years, continuous), gender (male vs. female), insurance (private, Medicaid/VA/Others, no insurance), post-high school degree program (yes/no), personal financial situation (living comfortably vs. just meet or don't meet basic expenses), working status (full time, part time, no job, or no response), and sexual orientation identity (straight vs. all others).
Risk-taking propensities: We characterized the propensity to risk-taking by including past 30-day use of alcohol (yes/no) and a binary variable that measures use of any tobacco product, any cannabis product, or any illicit drug or nonmedical use of prescription drug. Both of these measures were assessed during the 2021 assessment wave. In addition, we included the following measures collected during the 9th grade (fall 2013) survey wave to control for stable (heritable) risk-taking and rule-breaking personality traits and behaviors: ever use of any substance, the Temperament and Character Inventory (TCI) Impulsivity subscale (Cloninger et al., 1993), and past 6-month frequency of engagement in 11 different delinquent behaviors (e.g., stealing, lying to parents; summed) (Thompson et al., 2007). Finally, we included the UPPS-P Impulsive Behavior combined scale which includes negative urgency, positive urgency, lack of premeditation, lack of persistence, and sensation seeking subscales (Whiteside and Lynam, 2001), which was first measured in the 10th grade.
Social Distancing and Perceived COVID-19 susceptibility during the pandemic: Self-reported frequency of practicing physical distancing (staying >6 ft away from other people) in the past 2 weeks (Infrequent [“Sometimes” or “Rarely”] vs. Frequent [“Usually,” “Always,” or “Not been in public places”]) was assessed. Past 2-week frequency of engaging in 4 social recreational activities ((i.e., visit restaurant, bar, or club; host party with >10 people; attend party with >10 people; and visit indoor public venue (e.g., mall)) were also measured as a continuous outcome (range: 0–28). (Leventhal et al., 2021) Mask wearing in the past 2 weeks was measured by a binary outcome (Infrequent [“less than half of the time” or “Never”] vs. Frequent [“Always,” “More than half of the time,” or “Not gone to any places with other people”]). We also assessed the perceived likelihood of contracting COVID-19 coronavirus and perceived likelihood of dying from COVID-19 coronavirus if they were to be infected (100-point visual analogue scales, with ‘no chance’ and ‘definitely’ as anchors (0−100)).
2.3. Statistical analysis
Descriptive statistics of sample demographic characteristics were reported by count and percentage for categorical variables and mean and standard deviation (SD) for continuous variables, overall and stratified by vaccine hesitancy status. Multivariable logistic regression was conducted to estimate associations of race/ethnicity and sociodemographic factors, risk-taking propensities, and perceived COVID-19 vulnerability with the likelihood of vaccine hesitancy. We further tested the multicollinearity in the model to ensure that all included covariates have a variance inflation factor (VIF) less than 2.5 (Johnston et al., 2018). Missing covariate data were relatively small (Ns missing range: 0–72) and managed with multi-imputation using 20 multiply-imputed data sets (Rubin, 2004). Linear regression models were performed in the supplementary analysis with the continuous vaccine hesitancy scale (1–7) as the outcome variable.
For racial and ethnic groups with significant differences in vaccine hesitancy relative to White participants, mediation analyses were performed. Mediation tests of pathways from racial/ethnic group membership to the likelihood of vaccine hesitancy through the three vaccine attitude/belief subscales as simultaneous mediators were examined. The analysis yielded estimates on total effects, indirect effects, direct effects, the proportion of mediation. Significant sociodemographic covariates associated with vaccine hesitancy were adjusted for in the mediation analysis.
Odds ratios (ORs) adjusted ORs (AORs), linear model weights (bs), or mediation standardized estimates (βs) with 95% CIs were calculated. Regression analyses were conducted using SAS 9.4 (Cary, NC) and mediation analyses were conducted using Mplus 8.3 (MUTHEN & MUTHEN). P-values<.05 (two-tailed) were considered significant.
3. Results
3.1. Analytic samples
As depicted in Supplementary eFigure 1, 2041 participants provided responses about their vaccine uptake or likelihood of taking a vaccine, constituting the analytic sample. As shown in Table 1, the analytical sample of young adults was sociodemographically diverse (age, M[SD] = 21.3[0.7] years with a range of 18–24 years old; 47.3% of Hispanics, 19.1% of Asians, 4.5% of non-Hispanic Blacks; 61.7% were females; 24.5% had non-straight sexual orientation). 23.3% of participants responded in January 2021, 56.1% in February, 12.8% in March, 5.1% in April, and 2.7% in May.
The distribution of vaccine hesitancy responses included 325 (15.9%) reporting “not at all likely” to take a vaccine, 169 (8.3%) “not very likely”, 180 (8.8%) “slightly likely”, 240 (11.8%) “moderately likely”, 236 (11.6%) “very likely”, 653 (32.0%) “definitely likely”, and 238 (11.7%) already vaccinated. After recoding the responses, there were 674 (33.0%) classified as vaccine hesitant and 1367 (67.0%) were vaccine non-hesitant, and the distribution of vaccine hesitant vs. non-hesitant was similar across survey months (p = .99) but significantly different across all sociodemographic factors except gender (see Table 2 ).
Table 2.
Sample characteristics, overall and by vaccine hesitancy statusa (n = 2041).
| Overall sample | Vaccine hesitancy (yes) | Vaccine hesitancy (no) | P-valuef | |
|---|---|---|---|---|
| Overallb | 2041 (100.0) | 674 (33.0) | 1367 (67.0) | |
| Age, mean (SD)c | 21.3(0.7) | 21.3(1.0) | 21.3(0.5) | 0.61 |
| Survey Month (2021) | 0.99 | |||
| January | 475 (23.3) | 317 (23.2) | 158 (23.4) | |
| February | 1145 (56.1) | 771 (56.4) | 374 (55.5) | |
| March | 261 (12.8) | 173 (12.7) | 88 (13.1) | |
| April | 105 (5.1) | 69 (5.0) | 36 (5.3) | |
| May | 55 (2.7) | 37 (2.7) | 18 (2.7) | |
| Race/ethnicityd | <0.0001 | |||
| NH_Whites | 328 (16.3) | 102 (15.5) | 226 (16.7) | |
| NH_Blacks | 91 (4.5) | 58 (8.8) | 33 (2.4) | |
| Hispanics | 949 (47.3) | 376 (57.3) | 573 (42.4) | |
| Asians | 384 (19.1) | 53 (8.1) | 331 (24.5) | |
| Other | 256 (12.7) | 67 (10.2) | 189 (14.0) | |
| Sexc | 0.07 | |||
| Male | 782 (38.3) | 277 (41.1) | 505 (36.9) | |
| Female | 1259 (61.7) | 397 (58.9) | 862 (63.1) | |
| Health Insuranced | <0.0001 | |||
| Private | 1011 (50) | 249 (37.4) | 762 (56.1) | |
| Medicaid/VA/others | 843 (41.7) | 341 (51.2) | 502 (37.0) | |
| No insurance | 170 (8.4) | 76 (11.4) | 94 (6.9) | |
| In a degree programd | <0.0001 | |||
| No | 799 (39.3) | 377 (56.1) | 422 (31.0) | |
| Yes | 1235 (60.7) | 295 (43.9) | 940 (69.0) | |
| Personal financial Situationd | 0.003 | |||
| Live comfortably | 806 (39.7) | 235 (35.1) | 571 (41.9) | |
| Just meet or don't meet basic expense | 1226 (60.3) | 435 (64.9) | 791 (58.1) | |
| Working Statusd | <0.0001 | |||
| Full time | 433 (21.3) | 203 (30.2) | 230 (16.9) | |
| Part time | 795 (39.1) | 226 (33.6) | 569 (41.8) | |
| No job or no response | 806 (39.6) | 243 (36.2) | 563 (41.3) | |
| Sexual Minorityd, e | <0.0001 | |||
| Straight | 1534 (75.5) | 544 (81.1) | 990 (72.7) | |
| Non-straight | 499 (24.5) | 127 (18.9) | 372 (27.3) |
Vaccine hesitant group (not at all likely/not very slightly/slightly likely) vs. willing to take a vaccine group (moderately likely/very likely/definitely likely or already vaccinated).
N/row(%);
Age in the range of 18 to 24 years old.
N/column(%).
Straight vs. non-straight (lesbian, gay, bisexual, queer, questioning, or other sexual orientation).
Rao-Scott χ2 test for group differences.
3.2. Association of race/ethnicity with vaccine hesitancy
As shown in Table 3 , there were significant disparities in vaccine hesitancy among racial/ethnic groups. Black young adults had a higher prevalence of vaccine hesitancy (63.7%, AOR[95%CI] =4.3[2.4–7.8]) and Asians had a lower prevalence (13.8%, AOR[95%CI] = 0.5[0.3–0.8]) than Whites (31.1%). Hispanic (vs. White) participants had a higher prevalence of vaccine hesitancy (39.6, OR[95%CI] =1.5[1.1–1.9]) in the univariate model, but the difference was attenuated to be insignificant after adjusting for covariates. Results of covariate associations are in eTable 1. Pairwise comparisons also identified significant disparities in vaccine hesitancy across some racial and ethnic groups, such as Hispanics vs. Blacks (AOR[95%CI] =0.3[0.2–0.6]), Asians vs. Blacks (AOR[95%CI] =0.1[0.1–0.2]), and other races vs. Blacks (AOR[95%CI] =0.3[0.2–0.6]).
Table 3.
Demographics and factors associated with vaccine hesitancy in young adults.
| Prevalence of vaccine hesitancy (%) | OR (95% CI) | P-value | AOR (95% CI)a | P-valuea | |
|---|---|---|---|---|---|
| Race/ethnicity | |||||
| Whites | 31.1 | Reference | Reference | ||
| Blacksb | 63.7 | 3.9 (2.4–6.3) | <0.0001 | 4.3 (2.4–7.8) | <0.0001 |
| Hispanicsb | 39.6 | 1.5 (1.1–1.9) | 0.01 | 1.3 (1.0–1.8) | 0.10 |
| Asiansb | 13.8 | 0.4 (0.2–0.5) | <0.0001 | 0.5 (0.3–0.8) | 0.001 |
| Otherb, c | 26.2 | 0.8 (0.5–1.1) | 0.19 | 0.8 (0.6–1.3) | 0.44 |
Multivariable logistic regression models adjusted for all covariates listed in eTable 1. Missing covariate data (ns missing range: 0–72) were managed with multi-imputation using 20 multiply imputed data sets.
Pair-wise comparison: Hispanics vs. blacks (OR[95% CI] =0.4[0.2–0.6], p < .0001; AOR[95% CI]) = 0.3[0.2–0.6], p < .0001); Asians vs. blacks (OR[95% CI] =0.1[0.1–0.2], p < .0001; AOR[95% CI] = 0.1[0.1–0.2], p < .0001); other races vs. blacks (OR[95% CI] =0.2[0.1–0.2], p < .0001; AOR[95% CI] = 0.2[0.1–0.4], p < .0001); Asians vs. Hispanics (OR[95% CI] =0.2[0.2–0.3], p < .0001; AOR[95% CI] =0.4[0.3–0.6], p < .0001); other races vs. Hispanics (OR[95% CI] = 0.5[0.4–0.7], p < .0001; AOR[95% CI] =0.7[0.5–0.9], p = .02); other races vs. Asians (OR[95% CI]) = 2.2[1.5–3.3], p < .0001; AOR[95% CI] =1.6[1.0–2.4], p = .03).
Other included those who reported their racial and ethnic status as “American Indian or Alaska native,” “native Hawaiian or Pacific islander,” “multiracial,” or “other.”
Supplementary Tables 2–4 present racial and ethnic disparities across different vaccine hesitancy definitions and the results are consistent with the main analysis.
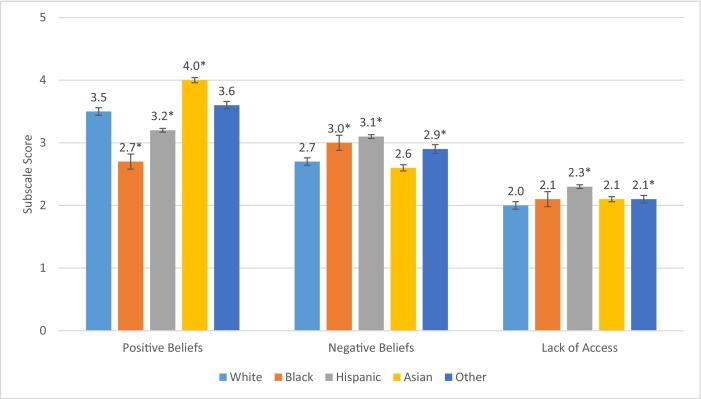
3.3. Racial/ethnic differences in attitudes and beliefs toward COVID-19 vaccination
Overall, the mean (standard deviation: SD) of positive belief, negative belief and lack-of-access belief scores were 3.4(1.0), 2.9(1.0), and 2.2(0.9), respectively. The mean scores indicate that the average respondent report was in the middle range of possible responses of disagree (=2), neutral (=3), or agree (=4) and not on the extreme ends of the response range. The inter-correlations among these 3 subscales were relatively moderate with Pearson correlation coefficients of −0.42 between positive beliefs and negative beliefs, 0.05 between positive beliefs and lack-of-access beliefs, and 0.18 between positive beliefs and lack-of-access beliefs. As shown in Figure 1 , Asians had the highest positive belief score (4.0[0.8]; equivalent to ‘agree’ to all items), followed by other races (3.6[1.0]), Whites (3.5[1.2]), Hispanics (3.2[1.0]), and Blacks (2.7[1.1]; in between ‘disagree’ and ‘neutral’ responses). In contrast, Hispanics had the highest negative belief score in vaccine uptake (3.1[1.0]), followed by Blacks (3.0[1.1]), other races (2.9[1.0]), Whites (2.7[1.1], and Asians (2.6[0.9]). The lack-of-access belief score was highest among Hispanics, followed by other races, Blacks, Asians, and Whites (See Fig. 1).
Fig. 1.
Mean positivea, negativeb, and lack-of-accessc attitudes and beliefsd about vaccines, by Race/Ethnic Group.
aPositive belief subscale is the mean of 5-point Likert scale (from 1 strongly unlikely to 5 strongly likely) of 7 items: 1) The vaccine could protect me against getting COVID-19; 2) If I get the vaccine, that could protect my family and friends from getting COVID-19; 3) I would get a vaccine for COVID-19 if it was available for free to anyone who wanted it.; 4) I believe it is important for everyone to take the COVID-19 vaccine to help end the pandemic; 5) Getting the COVID-19 vaccine is important so I can see my friends and family; 6) Getting the COVID-19 vaccine is important so I can go to bars, clubs, and restaurants; 7) I trust that the U.S. government approval of the vaccine means it is safe and effective.
bNegative belief subscale is the mean of 5-point Likert scale (from 1 strongly unlikely to 5 strongly likely) of 5 items: 1) I worry that the vaccine might cause some unpleasant side effects; 2) I worry that the vaccine might cause long term health effects for me; 3) I worry that the vaccine might cause more harm than getting COVID-19. 4) I am worried that the vaccine was developed too quickly. 5) I am worried that I could get sick with COVID-19 by taking the vaccine.
cLack-of-access belief subscale is the mean of 5-point Likert scale (from 1 strongly unlikely to 5 strongly likely) of 3 items: 1) I am concerned I can't get the vaccine because I don't have health insurance, or my insurance won't cover the vaccine. 2) I am concerned I can't get the vaccine because I don't know where or how to get the vaccine. 3)Trying to get the vaccine is too complicated or is too much trouble.
*: General linear model was performed for pairwise comparison (vs. White) with p-value <.05.
Error bar indicates the standard error.
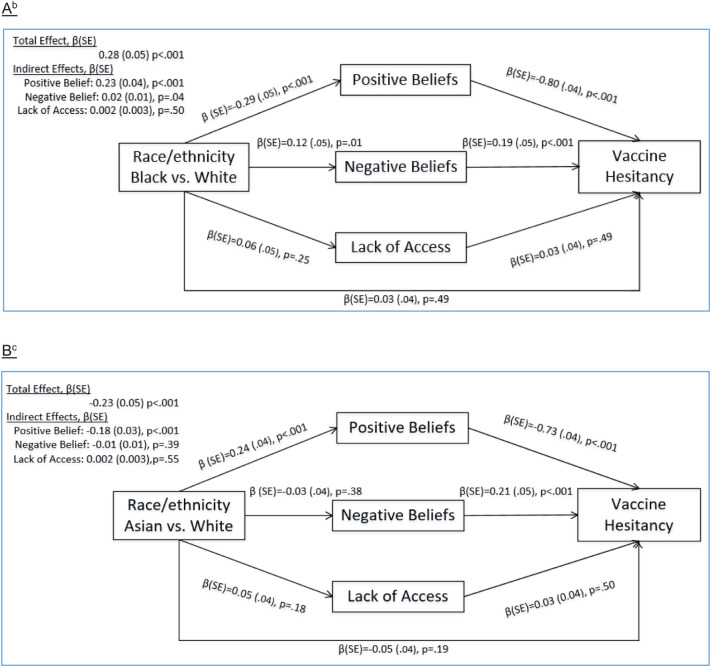
3.4. Mediation analysis
Given significant differences of Black and Asian vs. White participants, we conducted mediation analyses of these pairwise race disparity comparisons adjusted by significant sociodemographic covariates associated with vaccine hesitancy. Of the total effect association of Black (vs. White) disparity in vaccine hesitancy (βtotal effect = 0.28, p < .001, Fig. 2A), the three vaccine attitude and belief subscales collectively explained 90% race/ethnicity-hesitancy association. That is, after adjusting for the three mediator variables, the association of Black vs. White race was only one-tenth as large as it was without adjusting for the mediators. In the multiple-mediator model, the Black vs. White disparity was significantly mediated by Black participants having lower positive beliefs, which were associated with higher odds of vaccine hesitancy (βindirect effect = 0.23, p < .001). Black participants also had higher negative beliefs, which were positively associated with vaccine hesitancy (βindirect effect = 0.02, p = .04). Lack-of-access beliefs did not mediate the Black vs. White race/ethnicity difference in hesitancy. Of the Asian (vs. White) total association with lower vaccine hesitancy (βtotal effect = −0.23, p < .001, Fig. 2 B), the combined set of three attitude/belief subscales explained 81% of the total association. The only significant pathway was through Asians having higher positive beliefs, which was associated with lower hesitancy (βindirect effect = −0.18, p < .001). The lack-of-access or negative belief subscales did not mediate Asian vs. white differences in vaccine hesitancy.
Fig. 2.
Mediation of Racial/Ethnic Differences in Vaccine Hesitancy via Positive, Negative, and Lack-of-access-Related Attitudes and Beliefs toward Vacinesa.
a: Standardized estimates (βs) of total, direct, and indirect effects, and component paths from two simultaneous mediator path analysis models: Black (vs. White) and Asian (vs. White). Mediation analysis was adjusted by significant demographic covariates (i.e., health insurance status, in a degree program and sexual orientation status) associated with vaccine hesitancy. Other significant covariates (i.e., social distancing, risk-taking behaviors) were not included due to their high correlations with attributes and beliefs.
b: The total effect for the association between race/ethnicity (Black vs. White) and vaccine hesitancy, βtotal effect, was 0.28. The indirect effects from positive beliefs, negative beliefs, and lack of access beliefs were 0.23, 0.02, and 0.002, respectively. The Black vs. White vaccine hesitancy disparity was mediated by Black participants having lower positive beliefs (β = −0.29, p < .001), which were negatively associated with vaccine hesitancy (β = −0.80, p < .001). The Black vs. White disparity in vaccine hesitancy was also mediated by Blacks having higher negative beliefs (β = 0.12, p = .01), which were positively associated with vaccine hesitancy (β = 0.19, p < .001). The Black vs. White difference in vaccine hesitancy was not significantly mediated by lack of access beliefs (β = 0.06, p = .25).
c: The total effect for the association between race/ethnicity (Asian vs. White) with vaccine hesitancy estimate, βtotal effect, was −0.23. The indirect effects from positive beliefs, negative beliefs, and lack of access beliefs were − 0.18, −0.01, and − 0.002, respectively. The Asian vs. White vaccine hesitancy disparity was mediated by Asian participants having higher positive beliefs (β = 0.24, p < .001), which were negatively associated with vaccine hesitancy (β = −0.73, p < .001). The Asian vs. White difference in vaccine hesitancy was not significantly mediated by negative beliefs (β = −0.03, p = .38) or lack of access beliefs (β = 0.05, p = .18).
4. Discussion
Although previous studies have reported vaccine hesitancy disparities in general populations of adults, (Daly et al., 2021; Szilagyi et al., 2020; Thompson et al., 2021) this study provided new evidence of substantial racial and ethnic differences in vaccine hesitancy in a diverse sample of young adults. About one-third of young adults overall reported COVID-19 vaccine hesitancy in this study. Blacks had four times greater odds than Whites (AOR = 4.3) to report vaccine hesitancy, whereas Asians had 5-times lower odds of vaccine hesitancy than Whites. One strength of our findings is the inclusion of 19 different covariates in the multivariable analyses to account for other sociodemographics, risk-taking propensities, and perceived susceptibility to COVID-19. Many of the significant correlates of vaccine hesitancy identified in this study (e.g., insurance coverage, sexual minority, substance use, and perceived risk of contracting COVID-19) parallel findings from other studies in COVID-19 or other vaccines (e.g., influenza) hesitancy (Callaghan et al., 2021; Paul et al., 2021; Takayama et al., 2012; Yeung et al., 2016). Though young adults have lower hospitalization and mortality rate than older adults (Gold et al., 2020; The Centers for Disease Control and Prevention, 2021a), they are more likely to be interacting with other people and are more likely to spread the virus if not vaccinated. The substantial racial and ethnic disparity in vaccine hesitancy demonstrated here may further exacerbate the disproportionate burden of severe illness and death from COVID-19 in racial/ethnic minority communities (e.g., Blacks (Lopez 3rd et al., 2021; The Centers for Disease Control and Prevention, 2021a)).
It is imperative to identify effective intervention strategies to persuade hesitant young adults to get vaccinated that are culture and age specific. Previous studies have documented that trust in COVID-19 vaccines was an important factor in the decision to get vaccinated among U.S. adults (Baack et al., 2021; Szilagyi et al., 2021), and the trust in the vaccine was particularly lower in the Black population than in the White population (Daly et al., 2021), partly due to historical mistreatment, limited Black participants in clinical trials or bad personal experiences (Flores et al., 2021; Robert Wood Johnson Foundation, 2017). This study extended previous literature by demonstrating that racial/ethnicity-based disparities in vaccine hesitancy were largely mediated by racial differences in particular attitudes and beliefs toward COVID-19 vaccination. Our findings have direct implications for developing targeted outreach and educational messaging campaigns to increase vaccine uptake. For instance, we found that positive belief of vaccine uptake is the primary factor that mediates the disparity in vaccine hesitancy in Black young adults and provides an advantage in producing lower vaccine hesitancy among Asians compared to White participants. These types of positive vaccine beliefs toward vaccines for other diseases (e.g., influenza) have been shown to be malleable in response to the education and messaging campaigns (Lawes-Wickwar et al., 2021). The current findings indicate that government officials, public health agencies, and community organizations can develop educational messages to emphasize the importance of vaccines to prevent the spread of COVID-19 to family members and friends and others in their own community (beyond merely reducing the risk of self-infection). We acknowledge, however, the need for tailoring messaging, as one size does not fit all, and other factors, including the person providing the message (in addition to the message content per se) though multiple channels (e.g., influencer, digital media), may be important (Privor-Dumm and King, 2020).
Misinformation about vaccines' safety, efficacy, and side effects is prevalent on social media (Islam et al., 2021; Wilson and Wiysonge, 2020), and young adults are particularly exposed to social media (Pew Research Center, 2021). Our study identified a wide disparity in the negative belief of vaccine uptake between Blacks or Hispanics and Whites. These differences in negative COVID-19 vaccination beliefs partially mediated the association of Black vs. White race/ethnicity with vaccine hesitancy. Further steps are needed to disseminate trusted information about vaccine approval and research on side effects by harnessing social media and key influencers, including clinicians and health practitioners. This calls for a varied number of interventions to debunk myths and counter misinformation on social media. Although lack of access was considered a barrier during the survey period to get more people fully vaccinated, our results showed that it did not mediate Black vs. White or Asian vs. White disparities in vaccine hesitancy, which may persist after the COVID-19 vaccine became widely available without targeted efforts and interventions.
This study has limitations. First, vaccine hesitancy measures are self-reported and are subject to recall bias. Second, the young adult sample was from Los Angeles, CA and may not be generalizable to other regions. Third, some cell sizes were small, which precluded the analysis of vaccine hesitancy in some racial groups (e.g., American Indians/Alaska Natives, Multiracial) separately. Fourth, our main analyses included those who were already vaccinated as vaccine non-hesitant, but the findings are consistent after excluding those already vaccinated. Finally, the study was conducted between January 2021 and May 2021, when vaccine availability changed rapidly. Although this study did not identify a significant mediation effect on the lack-of-access factor, including access to vaccines, vaccine hesitancy, and the reasons behind hesitancy may change over time. Continuous monitoring of vaccine hesitancy is warranted.
Increasing vaccination against COVID-19 in young adults is a public health priority to achieve population-level immunity and end the pandemic, and to reduce large disparities in vaccinations among racial/ethnic populations. This study identified significant racial/ethnic disparities in vaccine hesitancy among young adult subpopulations that were largely mediated by positive and negative beliefs toward vaccine uptake. Targeted public education and messaging, through reliable and credible sources, countering social media myths, and messaging that responds to questions and concerns of varied groups, may mitigate vaccine hesitancy and reduce disparities in at-risk subpopulations, thus promoting equitable utilization of the effective vaccine.
Conflicts of interest
The authors report no potential conflicts of interest.
Funding
Research reported in this publication was supported by National Institute on Drug Abuse Award Number K24DA048160 (Leventhal) and Award Number K01DA042950 (Barrington-Trimis). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Role of funder
The funding agency had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Financial disclosure
The authors have no financial relationships relevant to this article to disclose.
Author contribution
Concept and design: Dai, Leventhal. Acquisition, analysis, or interpretation of data: Dai, Barrington-Trimis, Unger, Baezconde- Garbanati, Leventhal. Drafting of the manuscript: Dai, Leventhal. Critical revision of the manuscript for important intellectual content: Dai, Barrington-Trimis, Unger, Baezconde- Garbanati, Leventhal Statistical analysis: Dai. Obtained funding: Leventhal, Barrington-Trimis.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ypmed.2022.107077.
Appendix A. Supplementary data
Supplementary material
References
- Baack B.N., Abad N., Yankey D., Kahn K.E., Razzaghi H., Brookmeyer K., Kolis J., Wilhelm E., Nguyen K.H., et al. COVID-19 vaccination coverage and intent among adults aged 18-39 years - United States, march-may 2021. MMWR Morb. Mortal. Wkly Rep. 2021;70:928–933. doi: 10.15585/mmwr.mm7025e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basch C.H., Meleo-Erwin Z., Fera J., Jaime C., Basch C.E. A global pandemic in the time of viral memes: COVID-19 vaccine misinformation and disinformation on TikTok. Hum. Vaccin. 2021;17(8):2373–2377. doi: 10.1080/21645515.2021.1894896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Callaghan T., Moghtaderi A., Lueck J.A., Hotez P., Strych U., Dor A., Fowler E.F., Motta M. Correlates and disparities of intention to vaccinate against COVID-19. Soc. Sci. Med. 2021;272 doi: 10.1016/j.socscimed.2020.113638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cloninger C.R., Svrakic D.M., Przybeck T.R. A psychobiological model of temperament and character. Arch. Gen. Psychiatry. 1993;50:975–990. doi: 10.1001/archpsyc.1993.01820240059008. [DOI] [PubMed] [Google Scholar]
- Corace K.M., Srigley J.A., Hargadon D.P., Yu D., MacDonald T.K., Fabrigar L.R., Garber G.E. Using behavior change frameworks to improve healthcare worker influenza vaccination rates: a systematic review. Vaccine. 2016;34:3235–3242. doi: 10.1016/j.vaccine.2016.04.071. [DOI] [PubMed] [Google Scholar]
- Daly M., Jones A., Robinson E. Public trust and willingness to vaccinate against COVID-19 in the US from October 14, 2020, to march 29, 2021. JAMA. 2021;325:2397–2399. doi: 10.1001/jama.2021.8246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong E., Du H., Gardner L. The Lancet Infectious Diseases; 2020. An Interactive Web-Based Dashboard to Track COVID-19 in Real Time.https://gisanddata.maps.arcgis.com/apps/opsdashboard/index.html#/bda7594740fd40299423467b48e9ecf6 Dashboard available at. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans M, Wernau J. Unvaccinated Americans are behind rising Covid-19 hospitalizations. Wall Street J. 2021 https://www.wsj.com/articles/unvaccinated-covid-19-hospitalizations-11626528110 Available at. [Google Scholar]
- Flores L.E., Frontera W.R., Andrasik M.P., Del Rio C., Mondriguez-Gonzalez A., Price S.A., Krantz E.M., Pergam S.A., Silver J.K. Assessment of the inclusion of racial/ethnic minority, female, and older individuals in vaccine clinical trials. JAMA Netw. Open. 2021;4 doi: 10.1001/jamanetworkopen.2020.37640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gold J.A.W., Rossen L.M., Ahmad F.B., Sutton P., Li Z., Salvatore P.P., Coyle J.P., DeCuir J., Baack B.N., et al. Race, ethnicity, and age trends in persons who died from COVID-19 - United States, may-august 2020. MMWR Morb. Mortal. Wkly Rep. 2020;69:1517–1521. doi: 10.15585/mmwr.mm6942e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Islam M.S., Kamal A.M., Kabir A., Southern D.L., Khan S.H., Hasan S.M.M., Sarkar T., Sharmin S., Das S., et al. COVID-19 vaccine rumors and conspiracy theories: the need for cognitive inoculation against misinformation to improve vaccine adherence. PLoS One. 2021;16 doi: 10.1371/journal.pone.0251605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston R., Jones K., Manley D. Confounding and collinearity in regression analysis: a cautionary tale and an alternative procedure, illustrated by studies of British voting behaviour. Qual. Quant. 2018;52:1957–1976. doi: 10.1007/s11135-017-0584-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawes-Wickwar S., Ghio D., Tang M.Y., Keyworth C., Stanescu S., Westbrook J., Jenkinson E., Kassianos A.P., Scanlan D., et al. A rapid systematic review of public responses to health messages encouraging vaccination against infectious diseases in a pandemic or epidemic. Vaccines (Basel) 2021;9 doi: 10.3390/vaccines9020072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leventhal A.M., Strong D.R., Kirkpatrick M.G., Unger J.B., Sussman S., Riggs N.R., Stone M.D., Khoddam R., Samet J.M., et al. Association of Electronic Cigarette use with Initiation of combustible tobacco product smoking in early adolescence. JAMA. 2015;314:700–707. doi: 10.1001/jama.2015.8950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leventhal A.M., Dai H., Barrington-Trimis J.L., McConnell R., Unger J.B., Sussman S., Cho J. Association of Political Party Affiliation with Physical Distancing among Young Adults during the COVID-19 pandemic. JAMA Intern. Med. 2021;181:399–403. doi: 10.1001/jamainternmed.2020.6898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez L., 3rd, Hart L.H., 3rd, Katz M.H. Racial and ethnic health disparities related to COVID-19. JAMA. 2021;325:719–720. doi: 10.1001/jama.2020.26443. [DOI] [PubMed] [Google Scholar]
- NRP.org Biden Says All Adults Will Be Vaccine Eligible By April 19. 2021. https://www.npr.org/sections/coronavirus-live-updates/2021/04/06/984745020/biden-will-direct-states-to-make-all-adults-vaccine-eligible-by-april-19 Available at.
- Paul E., Steptoe A., Fancourt D. Attitudes towards vaccines and intention to vaccinate against COVID-19: implications for public health communications. Lancet Reg. Health Eur. 2021;1 doi: 10.1016/j.lanepe.2020.100012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pew Research Center Social Media Use in 2021. 2021. https://www.pewresearch.org/internet/2021/04/07/social-media-use-in-2021/ Available at.
- Privor-Dumm L., King T. Community-based strategies to engage pastors can help address vaccine hesitancy and health disparities in black communities. J. Health Commun. 2020;25:827–830. doi: 10.1080/10810730.2021.1873463. [DOI] [PubMed] [Google Scholar]
- Robert Wood Johnson Foundation Discrimination in America: Experiences and Views on Affects of Discrimination Across Major Population Groups in the United States. 2017. https://www.rwjf.org/en/library/research/2017/10/discrimination-in-america--experiences-and-views.html Available at.
- Rubin D.B. John Wiley & Sons; 2004. Multiple Imputation for Nonresponse in Surveys. [Google Scholar]
- SAS Institute Inc . 2019. SAS® 9.4 and SAS® Viya® 3.4 Programming Documentation: The FACTOR Procedure. [Google Scholar]
- Schmid P., Rauber D., Betsch C., Lidolt G., Denker M.L. Barriers of influenza vaccination intention and behavior - a systematic review of influenza vaccine hesitancy, 2005–2016. PLoS One. 2017;12 doi: 10.1371/journal.pone.0170550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skinner C.S., Tiro J., Champion V.L. Health Behavior: Theory, Research, Practice. 2015. Background on the health belief model; p. 75. [Google Scholar]
- Szilagyi P.G., Thomas K., Shah M.D., Vizueta N., Cui Y., Vangala S., Kapteyn A. National trends in the US public’s likelihood of getting a COVID-19 vaccine-April 1 to December 8, 2020. JAMA. 2020;325(4):396–398. doi: 10.1001/jama.2020.26419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szilagyi P.G., Thomas K., Shah M.D., Vizueta N., Cui Y., Vangala S., Fox C., Kapteyn A. The role of trust in the likelihood of receiving a COVID-19 vaccine: results from a national survey. Prev. Med. 2021;153 doi: 10.1016/j.ypmed.2021.106727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takayama M., Wetmore C.M., Mokdad A.H. Characteristics associated with the uptake of influenza vaccination among adults in the United States. Prev. Med. 2012;54:358–362. doi: 10.1016/j.ypmed.2012.03.008. [DOI] [PubMed] [Google Scholar]
- The Centers for Disease Control and Prevention . US Department of Health and Human Services, CDC; Atlanta, GA: 2020. Coronavirus Disease 2019 (COVID-19): Cases in U.S.https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html [Google Scholar]
- The Centers for Disease Control and Prevention CDC COVID Data Tracker: Demographic Trends of COVID-19 Cases and Deaths in the US Reported to CDC. 2021. https://stacks.cdc.gov/view/cdc/99332 Avaialable at.
- The Centers for Disease Control and Prevention COVID-19: Risk for COVID-19 Infection, Hospitalization, and Death By Race/Ethnicity. 2021. https://www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-discovery/hospitalization-death-by-race-ethnicity.html Available at.
- The Centers for Disease Control and Prevention COVID Data Tracker: COVID-19 Vaccinations in the United States. 2021. https://covid.cdc.gov/covid-data-tracker/#vaccinations Available at.
- Thompson M.P., Ho C.H., Kingree J.B. Prospective associations between delinquency and suicidal behaviors in a nationally representative sample. J. Adolesc. Health. 2007;40:232–237. doi: 10.1016/j.jadohealth.2006.10.016. [DOI] [PubMed] [Google Scholar]
- Thompson H.S., Manning M., Mitchell J., Kim S., Harper F.W.K., Cresswell S., Johns K., Pal S., Dowe B., et al. Factors associated with racial/ethnic group-based medical mistrust and perspectives on COVID-19 vaccine trial participation and vaccine uptake in the US. JAMA Netw. Open. 2021;4 doi: 10.1001/jamanetworkopen.2021.11629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whiteside S.P., Lynam D.R. The five factor model and impulsivity: using a structural model of personality to understand impulsivity. Personal. Individ. Differ. 2001;30:669–689. [Google Scholar]
- Wilson S.L., Wiysonge C. Social media and vaccine hesitancy. BMJ Glob. Health. 2020:5. doi: 10.1136/bmjgh-2020-004206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeung M.P., Lam F.L., Coker R. Factors associated with the uptake of seasonal influenza vaccination in adults: a systematic review. J. Public Health (Oxf.) 2016;38:746–753. doi: 10.1093/pubmed/fdv194. [DOI] [PubMed] [Google Scholar]
- Zampetakis L.A., Melas C. The health belief model predicts vaccination intentions against COVID-19: a survey experiment approach. Appl. Psychol. Health Well Being. 2021;13:469–484. doi: 10.1111/aphw.12262. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material