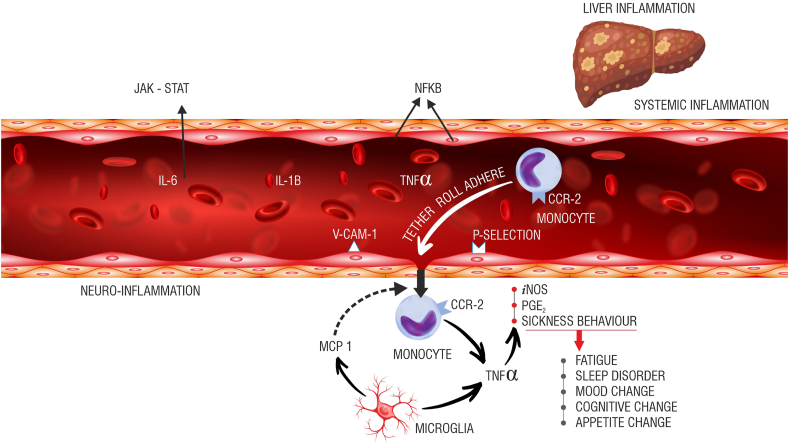
Figure 2.
Potential inflammatory pathways implicated in the causation of fatigue. The vagal afferents [not shown here] innervating the liver can respond to cytokines like Il-1b, TNF-a, and Il-6. These afferents project to different parts of the brain. The cytokines may directly interact with the cerebral endothelial cells [CECs] and generate secondary signals creating a milieu of neuro-inflammation. Nitric oxide [NO] through inducible nitric oxide synthase [iNOS] and prostaglandins [PGE2] are generated as a result of this interaction. The cytokines can directly access the brain through parts of the brain, which lacks the blood-brain barrier [BBB]. It is not a coincidence that the brain’s resident immune cells [microglia] have a greater density around these areas. A complex interaction between transmigrating activated circulating monocytes [chemokine receptor-2, CCR-2 positive] and activated microglia [monocyte chemoattractant protein-1, MCP-1 secreting] amplifies the neuro-inflammation to produce sickness behaviors, including fatigue.