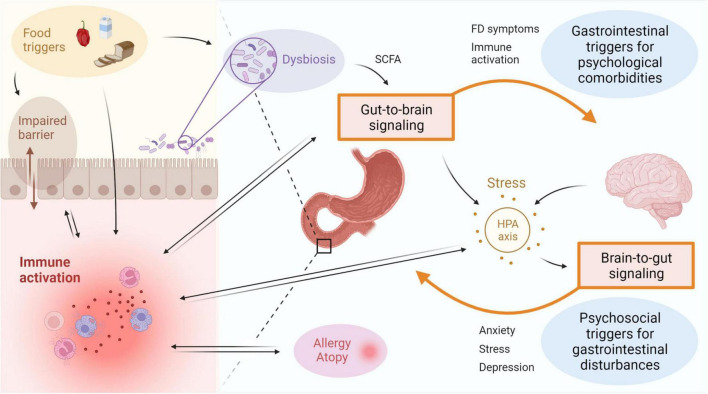
FIGURE 2.
Immune activation is linked to disturbances of the gut-brain-axis in FD. Bidirectional interaction between the gut and the brain involves GI symptoms and immune activation as potential triggers for psychological comorbidities, as well as psychosocial factors including stress, anxiety or depression resulting in gastroduodenal alterations. Activation of the HPA axis is suggested to play an important role, with both central and gut-derived mediators directly leading to induction of stress, which in turn can trigger GI symptoms. Factors associated to the intestinal inflammatory environment include microbial alterations and barrier impairments, both of which can be a cause or consequence of immune activation. The gut microbiota is also suggested to influence gut-to-brain communication directly or indirectly via metabolites such as SCFA. Food triggers are a major determinant of the microbiota composition and can also directly induce immune activation and impact barrier function. A relation between duodenal immune activation and allergy or atopy is proposed, but directionality and causality need to be established. FD: functional dyspepsia, GI: gastrointestinal, HPA: hypothalamic-pituitary-adrenal, SCFA: short-chain fatty acids. This figure was created in BioRender.