Abstract
Background
Survivors of the novel coronavirus (COVID‐19) experience significant morbidity with reduced physical function and impairments in activities of daily living. The use of in‐hospital rehabilitation therapy may reduce long‐term impairments.
Objective
To determine the frequency of therapy referral and treatment amongst hospitalized COVID‐19 patients, assess for disparities in referral and receipt of therapy, and identify potentially modifiable factors contributing to disparities in therapy allocation.
Design, Setting and Participants
Retrospective cohort study using data collected from the University of Colorado Health Data Compass data warehouse assessing therapy referral rates and estimated delivery based on available administrative billing.
Measurements
Multivariable logistic regression was used to determine the association between sex and/or underrepresented minority race with therapy referral or delivery.
Results
Amongst 6239 COVID‐19‐related hospitalization, a therapy referral was present in 3952 patients (51.9%). Hispanic ethnicity was independently associated with lower odds of receipt of therapy referral (adjusted OR [aOR]: 0.78, 95% confidence interval [CI]: 0.67–0.93, p = .001). Advanced age (aOR: 1.53, 95% CI: 1.46–1.62, p < .001), greater COVID illness severity (aOR for intensive care unit admission: 1.63, 95% CI: 1.37–1.94, p < .01) and hospital stay (aOR: 1.14, 95% CI: 1.12–1.15, p < .01) were positively associated with referral.
Conclusions and Relevance
In a cohort of patients hospitalized for COVID‐19 across a multicenter healthcare system, we found that referral rates and delivery of physical therapy and/or occupational therapy sessions were significantly reduced for patients of Hispanic identity compared with patients of non‐Hispanic, Caucasian identity after adjustment for potential confounding by available demographic and illness severity variables.
BACKGROUND
Individuals who are hospitalized are at high risk for new functional dependency after hospitalization. 1 , 2 Patients who are hospitalized experience significant long‐term physical, cognitive, psychological, and functional impairments. 3 , 4 , 5 Patients hospitalized for novel coronavirus (COVID‐19) infection experience fatigue, myalgias, respiratory symptoms, impaired physical function, and cognitive deficits, 6 , 7 and they are at high risk for new disability, with more than half reporting new disability and/or functional challenges at 1 month post hospitalization. 8 Increasing illness severity, especially amongst patients requiring mechanical ventilation, is associated with a greater likelihood of posthospital morbidity. 3 Thus, it is likely that many patients will develop significant deficits requiring rehabilitation during, and following, hospitalization. 7 , 9 , 10 , 11
In‐hospital rehabilitation provided by physical therapists (PTs) and occupational therapists (OTs) may mitigate the short‐ and long‐term sequela of acute illness, such as that seen with COVID‐19. 12 , 13 Furthermore, early reports suggest that physical therapy delivered within the hospital is feasible and may improve the mobility status of patients with COVID‐19. 14 , 15 , 16 However, especially during the early months of the COVID‐19 pandemic, many patients experienced delays for receipt of in‐hospital rehabilitation services due to barriers such as infectious isolation protocols, limited personal protective equipment allocation, disease severity, and varying local pandemic procedures reducing or eliminating standard rehabilitation services. 17 , 19 These barriers likely altered the timing and delivery of early mobilization and rehabilitation therapies. Whether this reduced and/or delayed access to rehabilitation services may have contributed to disparities for patients who are racial and ethnic minorities is unknown.
Communities of color are disproportionately burdened by COVID‐19 infection; racial and ethnic minority populations are up to 5.6 times more likely to be hospitalized compared with non‐Hispanic White persons. 19 Racial and ethnic minorities also experience greater severity of disease and complications from COVID‐19 infection, 18 , 20 increasing their risk of long‐term physical and mental health impairments. While early initiation of rehabilitation services during hospitalization may reduce these debilitating consequences of COVID‐19 infection, implicit biases in referral or receipt of therapy for these rehabilitation services could contribute to the poorer outcomes observed among racial and ethnic minorities, as has been observed with referrals in other settings. 21
The purpose of this analysis was to determine whether the allocation of rehabilitation services differed among racial/ethnic minority patients compared with non‐Hispanic White patients and to identify potential explanations for disparate allocation, if present.
METHODS
We performed a retrospective cohort study using electronic health record (EHR) data from 12 hospitals within the University of Colorado health system. Data extraction services were provided by the Health Data Compass Data Warehouse project (healthdatacompass.org). Data collected from March 2020 until April 2021 were included in the analysis. All patients age 18 years and older with an identified COVID‐19 diagnosis (defined by the presence of a positive polymerase chain reaction test or a COVID‐19‐associated diagnosis code documented in the UCHealth EHR) were included in the analysis. 22 Our outcome of therapy referral was defined as the presence of a referral for PT and/or OT consultation during the hospitalization. There was a significant overlap between PT and OT consultation (>87% overlap), thus we combined referrals into one outcome variable, particularly given that OT often performs PT services within our hospital. Race, ethnicity, and sex were self‐reported in the EHR by patients at registration in the UCHealth system. We excluded female patients admitted for obstetrics (OB)‐related admissions, patients not yet discharged at the time of data delivery, and patients who died within 48 h of admission from our analyses. When reviewing referral data, we found that there were differences between referral and actual receipt (defined by the presence of a billing charge noting actual therapy delivery). Therefore, we performed an additional analysis limited to a single hospital (University of Colorado Hospital Anschutz Medical Center) where billing data (procedural charge code for PT and/or OT evaluation) were available. This billing data allowed for the comparison of actual receipt of bedside PT and/or OT services versus referral requests only to determine if there were differences in the odds of receipt of rehabilitation therapy services for minority groups compared with non‐Hispanic White persons.
We performed descriptive statistics to describe the receipt of PT/OT referral amongst different racial/ethnic groups and between sexes. Racial/ethnic groups were defined as: non‐Hispanic White (reference), non‐Hispanic African American or Black, Hispanic, or other. We performed bivariate analyses (χ 2 tests, t tests, analysis of variance (ANOVA) or nonparametric equivalent, as appropriate) to determine whether predictors of therapy referral differed amongst these groups. Multivariable, mixed‐effects logistic regression models tested whether there was an independent association between race and ethnicity with the receipt of PT and/or OT referral. We adjusted for potential confounders and potentially modifiable predictors including length of stay, intensive care unit (ICU) admission, age, sex, prehospital independence with activities of daily living (ADL) and mobility (as assessed by nursing on admission), use of a mobility device at baseline, use of translation services, and categorical time. We included two measures of baseline function (i.e., prehospital ADL/mobility independence and mobility device usage) as it is difficult to measure function with a single construct. There are a number of patients who are functionally limited, but are not limited in mobility such that they require assistive devices for mobility. Therefore, using both measures in our model adjusts for a wider spectrum of functional deficits to better adjust for baseline function. A random effect for the hospital region was included in the model. We were unable to stratify by individual site given relatively small numbers of patients at some hospitals and existing data‐sharing agreements at the individual hospital level with the Compass group. The baseline functional data (independence in ADLs/mobility and use of a mobility device) was found to be missing in 19.6% and 20.6% of the cohort, respectively. For analysis purposes, we structured these variables to reflect evidence of impairment, grouping answers indicating nonimpairment (independent ADLs or no use of mobility device) and missing values together. Additionally, we performed a sensitivity analysis with the removal of the ADL variable without change in the overall conclusions drawn. All analyses were conducted via R statistical software with a p value of <.05 considered statistically significant. The overall χ 2 or ANOVA p value is reported in the racial/ethnicity bivariate analyses (no pairwise comparisons performed).
RESULTS
We identified patients across the UCHealth system admitted with a diagnosis of COVID‐19. After exclusion of the OB‐related admissions (n = 263), we identified 6239 COVID‐19‐related hospitalizations (Table 1). A referral for PT and/or OT was present in 3077 (49.3%) patients. Therapy referral and delivery varied over time (Figure 1). Patients with a PT and/or OT referral were more likely to require ICU admission (35.5% vs. 14.8%, p < .01) and/or mechanical ventilation (21.8% vs. 7.7%, p < .01).
Table 1.
Baseline characteristics of patients hospitalized with a diagnosis of COVID‐19 infection within the UCHealth system between March and April 2021, stratified by PT/OT referral request
| No referral | PT/OT referral | |
|---|---|---|
| n | 3162 | 3077 |
| Demographics | ||
| Mean age (years) (SD) | 54.6 (16.4) | 67.9 (15.2) |
| Categorical age (%) | ||
| ≥65 | 878 (27.8) | 1934 (62.9) |
| >40–<65 | 1603 (50.7) | 974 (31.7) |
| ≤40 | 681 (21.5) | 169 (5.5) |
| Male (%) | 1785 (56.5) | 1678 (54.5) |
| Categorical race/ethnicity (%) | ||
| Black or African American, non‐Hispanic | 253 (8.0) | 262 (8.5) |
| Hispanic | 1166 (36.9) | 815 (26.5) |
| Other | 283 (9.0) | 294 (9.6) |
| White, non‐Hispanic | 1460 (46.2) | 1706 (55.4) |
| Translation services utilized for language (%) | 596 (18.8) | 482 (15.7) |
| Payer source (%) | ||
| Commercial | 1117 (35.3) | 486 (15.8) |
| Medicaid | 656 (20.7) | 439 (14.3) |
| Medicare | 868 (27.5) | 1873 (60.9) |
| Other/unknown | 521 (16.5) | 279 (9.1) |
| Mean body mass index (SD) | 32.2 (8.3) | 30.2 (7.9) |
| Outcomes | ||
| Discharged home (%) | 2627 (83.1) | 1386 (45.0) |
| Admitted to the ICU (%) | 468 (14.8) | 1093 (35.5) |
| Median days prior to ICU admission [IQR] | 0.8 [0.5, 1.5] | 0.9 [0.6, 2.5] |
| Mechanically ventilated (%) | 245 (7.7) | 671 (21.8) |
| Median hospital length of stay in days [IQR] | 4 [2.0, 6.0] | 8.0 [4.0, 15.0] |
| In‐hospital death (%) | 306 (9.7) | 337 (11.0) |
| In‐hospital death within 48 h of admission (%) | 64 (2.0) | 22 (0.7) |
| Hospitalized at end of cohort follow‐up period (%) | 25 (0.8) | 24 (0.8) |
| PT/OT outcomes | ||
| Patient is not independent with ADLs/mobility, prehospital (%) | 243 (7.7) | 693 (22.5) |
| Use of a mobility assistive device, prehospital (%) | 150 (4.7) | 669 (21.7) |
| Patient using mobility device AND not independent with ADLs and/or mobility (%) | 36 (1.1) | 266 (8.6) |
Abbreviations: ADL, activities of daily living; ICU, intensive care unit; IQR, interquartile range; OT, occupational therapy; PT, physical therapy.
Figure 1.
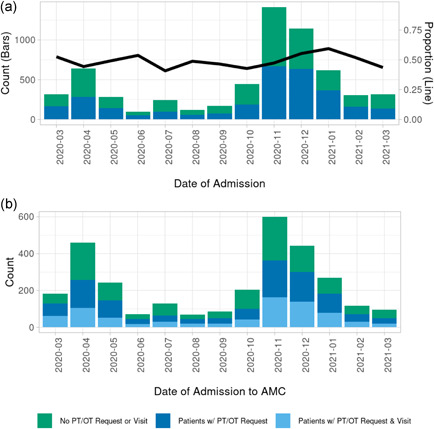
(a) Physical therapy (PT) and occupational therapy (OT) referral rates over time compared with admissions. (b) PT and/or OT delivery at Anschutz Medical Center compared with the proportion of PT/OT referrals.
PT/OT referral: Differences by patient race and ethnicity
Overall PT and/or OT referral differed by racial/ethnic group (p < .01), with Hispanic patients less likely to receive PT and/or OT referral (41 vs. 54% in non‐Hispanic White). Among patients receiving a PT and/or OT referral, most identified as non‐Hispanic White (55.4%), while 26.5% identified as Hispanic (any race) and 8.5% identified as non‐Hispanic Black (Table 2). The remaining 9.6% identified as a race or ethnicity other than White, Black, or Hispanic. Patients of Hispanic ethnicity were younger, on average, less likely to have Medicare, and more likely to have Medicaid than patients identified as White non‐Hispanic. Black non‐Hispanic patients were less likely to have baseline independence with all ADLs/mobility (49 vs. 55% in non‐Hispanic White), while Hispanic patients were more likely to be independent at baseline (60 vs. 55% in non‐Hispanic White). Patients who were Hispanic were less likely to require an assistive device prior to admission (14 vs. 26% in non‐Hispanic White). Significant differences between one or more groups were also detected in the probability of ICU admission, mechanical ventilation, length of stay, and discharge to home (all p < .001). Patients who were Black (non‐Hispanic) or Hispanic were more likely to require ICU admission and/or require mechanical ventilation; hospitalizations were also longer compared with patients who were White non‐Hispanic. Patients who were Hispanic were more likely to discharge home (51 vs. 42% in non‐Hispanic White). In‐hospital mortality was not significantly different by race and/or ethnicity amongst patients receiving a referral for PT/OT (p = .21).
Table 2.
PT/OT referral subset stratified by reported race and/or ethnicity
| Variable | Black or African American, non‐Hispanic | Hispanic | Other | White, non‐Hispanic | p Value | |
|---|---|---|---|---|---|---|
| n | 262 | 815 | 294 | 1706 | ||
| Age (years), mean (SD) | 65.54 (14.94) | 62.31 (15.52) | 66.07 (16.61) | 71.23 (13.94) | <.001 | |
| Categorical age (%) | <.001 | |||||
| ≥65 | 145 (55.3) | 378 (46.4) | 176 (59.9) | 1235 (72.4) | ||
| >40–<65 | 97 (37.0) | 367 (45.0) | 92 (31.3) | 418 (24.5) | ||
| ≤40 | 20 (7.6) | 70 (8.6) | 26 (8.8) | 53 (3.1) | ||
| Male (%) | 138 (52.7) | 450 (55.2) | 158 (53.7) | 932 (54.6) | .897 | |
| Patient is not independent with ADLs/mobility (%) | 50 (19.1) | 132 (16.2) | 69 (23.5) | 442 (25.9) | <.001 | |
| Assistive mobility device used (%) | 66 (25.2) | 111 (13.6) | 41 (13.9) | 451 (25.9) | <.001 | |
| Patient using mobility device AND not independent with ADLs and/or mobility (%) | 23 (8.8) | 38 (4.7) | <20a | 189 (11.1) | <.001 | |
| Payer source (%) | <.001 | |||||
| Commercial | 37 (14.1) | 137 (16.8) | 49 (16.7) | 263 (15.4) | ||
| Medicaid | 57 (21.8) | 189 (23.2) | 62 (21.1) | 131 (7.7) | ||
| Medicare | 153 (58.4) | 337 (41.3) | 148 (50.3) | 1235 (72.4) | ||
| Other/unknown | 15 (5.7) | 152 (18.7) | 35 (11.9) | 77 (4.5) | ||
| Translation services utilized for language (%) | <20a | 374 (45.9) | 82 (27.9) | <20a | <.001 | |
| Mean body mass index (SD) | 31.13 (7.49) | 31.61 (8.10) | 27.81 (6.61) | 29.88 (7.86) | <.001 | |
| Discharged to home (%) | 114 (43.5) | 414 (50.8) | 142 (48.3) | 716 (42.0) | <.001 | |
| Admitted to the ICU (%) | 114 (43.5) | 406 (49.8) | 126 (42.9) | 447 (26.2) | <.001 | |
| Median days to ICU admission [IQR] | 0.90 [0.60, 3.05] | 0.90 [0.60, 2.18] | 0.90 [0.60, 2.58] | 1.00 [0.70, 2.85] | .223b | |
| Use of mechanical ventilation (%) | 79 (30.2) | 282 (34.6) | 79 (26.9) | 231 (13.5) | <.001 | |
| Median hospital length of stay [IQR] | 9.0 [4.0, 18.0] | 11.0 [5.0, 21.0] | 8.0 [5.0, 17.0] | 7.0 [4.0, 12.0] | <.001b | |
| In‐hospital death (%) | 27 (10.3) | 87 (10.7) | 43 (14.6) | 180 (10.6) | .21 | |
Abbreviations: ADL, activities of daily living; ICU, intensive care unit; IQR, interquartile range; OT, occupational therapy; PT, physical therapy.
Suppressed count.
Nonparametric testing.
In adjusted analyses, Hispanic ethnicity (vs. White, non‐Hispanic) and male sex remained independently associated with reduced odds of receipt of PT and/or OT referral (p < .01) (Table 3). Increased age, greater illness severity, Medicaid or Medicare insurance status (vs. commercial payer), and patients who were nonindependent with ADLs and mobility at baseline were more likely to receive a referral for PT and/or OT. To explore whether the association with Hispanic ethnicity was related to a language barrier, we included the need for translation services in the model. In total, 333 (21%) ICU patients and 745 (16%) floor patients required translation services. Patients who identified as a racial or ethnic minority and required translation services were significantly less likely to receive PT and/or OT referral (p < .01; reference: patients who do not identify as a racial or ethnic minority, regardless of interpreter use). Conversely, there was no difference in receipt of referral for identified racial/ethnic minorities who did not require translation services (p = .25). Finally, to explore the impact of illness severity on this relationship, we stratified by ICU status and found that the disparities were more pronounced amongst patients admitted to the hospital floor compared with those admitted to the intensive care unit (Figure S1).
Table 3.
Multivariable model of PT/OT referral by race/ethnicity (n = 6153)
| Adjusted odds ratio | 95% Confidence interval | |||
|---|---|---|---|---|
| Variable | Est | LL | UL | p Value |
| Race/ethnicity (REF: White, non‐Hispanic) | ||||
| Black or African American, non‐Hispanic | 1.02 | 0.80 | 1.29 | .87 |
| Hispanic | 0.78 | 0.67 | 0.91 | .001 |
| Other | 1.02 | 0.81 | 1.28 | .87 |
| Admission to the intensive care unit | 1.63 | 1.37 | 1.94 | <.001 |
| Age (per 10‐year period) | 1.53 | 1.46 | 1.62 | <.001 |
| Hospital days | 1.14 | 1.12 | 1.15 | <.001 |
| Male gender | 0.83 | 0.73 | 0.94 | 0.003 |
| Payer source (REF: commercial/managed) | ||||
| Medicaid | 1.71 | 1.40 | 2.09 | <.001 |
| Medicare | 2.18 | 1.81 | 2.62 | <.001 |
| Other/unknown | 1.24 | 1.00 | 1.55 | .05 |
| Categorical time (REF: Jan 2021–April 202 | ||||
| March 2020–May 2020 | 0.67 | 0.55 | 0.82 | <.001 |
| June 2020–Sept 2020 | 0.81 | 0.64 | 1.03 | .08 |
| Oct 2020–Dec 202 | 0.73 | 0.63 | 0.86 | <.001 |
| Nonindependent with activities of daily living/mobility, prehospital | 2.23 | 1.85 | 2.68 | <.001 |
Abbreviations: EST, estimate; LL, lower limit; OT, occupational therapy; PT, physical therapy; UL, upper limit.
In adjusted analyses stratified by gender, males who were Hispanic (adjusted OR [aOR], 0.7, 95% confidence interval [CI]: 0.5–0.8, p < .001) had significantly lower odds of receiving a referral for PT and/or OT consultation compared with males who were non‐Hispanic, White. In the same adjusted analysis, there was not a significant difference in the odds of referral for PT and/or OT consultation for females who were Hispanic compared with White females who were non‐Hispanic (p = .67) (Table S1).
In a subset of patients (n = 2218) with available data on receipt of PT and/or OT services (Table S3), Hispanic ethnicity was similarly associated with a reduced proportion of ever receiving PT and/or OT, after adjustment for age, sex, and severity of illness (aOR: 0.6, 95% CI: 0.5–0.8, p = .001). Increased age (aOR per 10 years: 1.3, 95% CI: 1.2–1.5, p < .002), greater illness severity (ICU admission aOR: 2.2, 95% CI: 1.7–2.9, p < .001; length of stay aOR: 1.1, 95% CI: 1.1–1.1, p < .001), baseline nonindependence (aOR: 2.2, 95% CI: 1.6–3.0; p < .001), and noncommercial payers (Medicare aOR: 1.9, 95% CI: 1.3–2.6, p < .001; Medicaid aOR: 1.6, 95% CI: 1.1–2.2, p = .01) remained associated with receipt of PT and/or OT.
DISCUSSION
This analysis aimed to test whether referral to and delivery of rehabilitation therapy services differed among racial/ethnic minority patients compared with non‐Hispanic White patients, contributing to poorer outcomes in this population. Furthermore, we explored potential explanations for disparate allocation if present. In a diverse cohort of patients hospitalized for COVID‐19 across a regional healthcare system, referral rates for PT and/or OT were significantly lower among patients who were Hispanic compared with patients who were non‐Hispanic White, after adjustment for available demographic and illness severity variables. Furthermore, in a subanalysis of patients with available billing data for PT and/or OT services received, patients who were Hispanic were also less likely to actually receive these rehabilitation therapy services compared with patients who were non‐Hispanic White.
There are many possible explanations for these disparities observed with both referral rates and receipt of rehabilitation therapy services. Notably, patients who were Hispanic in our cohort were younger and more independent at baseline. Yet, studies of hospitalized COVID patients report longer‐term impairments often with new disabilities despite normal function at baseline. 8 These factors may impact a provider's clinical decision‐making surrounding referral to PT and/or OT as well as rehabilitation therapist's decisions on which patients to evaluate and/or treat at the bedside. Physical therapists and occupational therapists within acute care hospitals are often consulted to assist with discharge planning, especially for patients who may require placement and/or postacute care rehabilitation. 23 , 24 Therefore, acute care rehabilitation therapy practices may not prioritize patients who are physically and functionally able to discharge home, even when these patients exhibit new impairments and/or are at risk for long term functional issues. 24
Translation services may contribute to inequity of rehabilitation therapy delivery, as a potentially modifiable factor. Patients requiring translation services were significantly less likely to receive these referrals compared with English‐speaking patients. Inaccessible or inadequate translation services increase cost, prolong lengths of stay, and increase errors among care teams caring for patients with limited English proficiency. 25 Translation services for patients with COVID‐19 in our hospital occur via video bedside translators. Although access is usually not a barrier, the perceived necessary time needed for translation may be a barrier to initial referral amongst medical providers.
The observed disparities in referral rates and delivery of therapy services may reflect overall differences in access to care for patients of Hispanic identity. Interestingly, we saw temporal variation in referral rates and delivery of services that appeared to correspond with clinical COVID‐19 surges. Insurance coverage in our cohort was a significant predictor of therapy referral and delivery; this association is likely confounded by age and comorbid illness since patients with Medicare represent a commonly identified group who require therapy services due to advanced age and potential frailty. Contrary to these confounding factors, patients who are Hispanic had the lowest proportion of Medicare beneficiaries and the highest proportion of Medicaid and other/unknown beneficiaries, suggesting that this group is likely underinsured. In this situation, providers may not place a referral for rehabilitation therapy for patients with Medicaid or unknown insurance status, assuming there is a potential for increased out‐of‐pocket costs. Overall, we found that Medicaid and unknown insurance were associated with greater odds of rehabilitation referral. Indeed, providing in‐hospital rehabilitation services to underinsured or uninsured individuals may be important to prioritize because it may not be financially feasible for these individuals to receive home‐ nor outpatient‐based rehabilitation services following hospital discharge; this lack of access to rehabilitation services across the care continuum increases the risk of perpetuating posthospital impairments contributing to long‐term morbidity.
Importantly, implicit bias may influence both the referral for PT/OT services and the delivery of therapy services. Disparities in care continue to exist, and those with limited financial resources and those of racial minorities or Hispanic ethnicity appear to be most impacted. Recent studies have demonstrated lower specialist referrals among Black compared with white patients. 26 , 27 Little is known about implicit biases present in receipt of inpatient PT and OT services; however, Hispanic older adults are significantly less likely to be referred for home health services compared with non‐Hispanic White patients, a finding driven primarily by insurance coverage. 28 Furthermore, in a separate study, both Hispanic and Black patients were significantly less likely than non‐Hispanic White patients to receive intensive rehabilitation following traumatic brain injury, and this difference persisted in the Medicare population, indicating that factors other than insurance coverage contributed to this observed disparity. 29 Identifying factors related to and working to overcome implicit bias is imperative in providing equitable care for all.
Patients hospitalized for COVID‐19, especially those requiring critical care, are likely to experience significant in‐hospital morbidity and are at high risk for posthospital functional impairment. 6 , 7 There is a significant need to equitably identify all individuals who demonstrate the need for rehabilitation services during their hospital stay to ensure their needs are met both during and after hospitalization. Additionally, after identification, it is vital to ensure appropriate and equitable allocation of rehabilitation services. The present analysis identified that Hispanic males had significantly lower odds of both receiving a referral for PT/OT and bedside rehabilitation services. The limitations of a retrospective data set analysis, however, restrict our ability to identify why this inequity occurred, especially when one considers the inherent multilevel complexity of a healthcare system during a pandemic. Emerging literature surrounding processes for the identification of patients who may benefit from rehabilitation services during hospitalization suggest that healthcare systems that integrate the multidisciplinary measurement of physical function and mobility appear to result in more appropriate therapy referrals and visits for patients with more severe impairments. 30 , 31 It is unknown if the use of standardized screening procedures and objective measures of physical function would help address systemic health disparities such as those identified in the present analysis.
There are several important limitations to our current study. Retrospective, administrative clinical data limit our ability to fully explain disparities observed in the data, especially given the presence of missing data and unknown reliability and validity of some of the documentation constructs. Data pertaining to reasons for lack of both referral and delivery of PT/OT services were not available in the data set; for example, it is possible that some patients declined services due to ongoing symptoms or lack of desire for therapy. Additionally, we are unable to obtain information about provider practices regarding placement of referrals for rehabilitation therapy nor about PT/OT practices regarding service delivery; as a result, there are likely multilevel factors affecting these care decisions that are not accounted for within our current analysis. Similarly, it is recognized that mobility culture within individual hospitals can vary significantly. We attempted to control for this by including hospital region as a mixed effect in our model, but were not able to adjust by individual hospital due to data‐sharing limitations and small numbers of included individuals. We were also limited in incorporating only sociodemographic information available in the EHR. Many social determinants of health such as proximity to care, health literacy, annual income, and access to culturally appropriate care are not standard constructs included in the EHR. Likewise, hospital‐level factors may alter the placement of referrals and delivery of rehabilitation services, including hospital culture, staffing, standards of care, and provider experience; however, these factors are not available within our current data set. Future studies should aim to better understand social determinants of health as they relate to therapy resource allocation within and after acute care hospitalization. Finally, while we adjusted for the markers of illness severity available within the data set, there is likely residual confounding by illness severity that explains some of the variances in referral rates and delivery.
CONCLUSIONS
In a diverse cohort of patients hospitalized for COVID‐19 across a regional healthcare system, referral rates, and delivery of PT and/or OT services was significantly reduced for Hispanic patients compared with non‐Hispanic White patients after adjusting for potential confounding. We identified the use of interpreter service and insurance payer mix as potentially modifiable factors associated with these disparities. Future studies should determine the risk of poor long‐term outcomes amongst this population to better inform inpatient staffing models and to better target acute services to groups with a high likelihood of improved functional recovery and explore methods for ensuring equitable allocation of rehabilitative resources in hospitalized patients.
CONFLICT OF INTEREST
The authors declare that there are no conflicts of interest.
Supporting information
Supporting information.
ACKNOWLEDGMENTS
The current project is supported by NIH/NIA R01 AG 054366‐05S1 (to Kristine M. Erlandson and Jennifer Stevens‐Lapsley, MPI). Dr. Jolley is supported by NIH/NIAAA K23 AA 026315‐05. Dr. Capin is supported by NIH/NIA F32‐AG066274, Advanced Geriatrics Fellowship from the United States (US) Department of Veterans Affairs Geriatric Research Education and Clinical Center, and Academy of Orthopedic Physical Therapy Career Development Award. Ms. Heery is supported by NIH/NCATS Colorado CTSA Grant Number TL1 TR002533. This project is supported by Health Data Compass Data Warehouse (healthdatacompass.org). REDCap Database is supported by NIH/NCATS Colorado CTSA Grant Number UL1 TR002535. Rapid Response Data for Discoveries (R2D2) is funded by the Gordon and Betty Moore Foundation https://covid19questions.org/. The contents are the authors' sole responsibility and do not necessarily represent official NIH views.
Jolley S, Nordon‐Craft A, Wilson MP, et al. Disparities in the allocation of inpatient physical and occupational therapy services for patients with COVID‐19. J Hosp Med. 2022;17:88‐95. 10.1002/jhm.12785
REFERENCES
- 1. Gill TM, Allore HG, Holford TR, Guo Z. Hospitalization, restricted activity, and the development of disability among older persons. JAMA. 2004;292(17):2115‐2124. [DOI] [PubMed] [Google Scholar]
- 2. Kortebein P. Rehabilitation for hospital‐associated deconditioning. Am J Phys Med Rehabil. 2009;88(1):66‐77. [DOI] [PubMed] [Google Scholar]
- 3. Herridge MS, Cheung AM, Tansey CM, et al. One‐year outcomes in survivors of the acute respiratory distress syndrome. N Engl J Med. 2003;348(8):683‐693. [DOI] [PubMed] [Google Scholar]
- 4. Herridge MS, Tansey CM, Matte A, et al. Functional disability 5 years after acute respiratory distress syndrome. N Engl J Med. 2011;364(14):1293‐1304. [DOI] [PubMed] [Google Scholar]
- 5. Ferrante LE, Pisani MA, Murphy TE, Gahbauer EA, Leo‐Summers LS, Gill TM. Functional trajectories among older persons before and after critical illness. JAMA Intern Med. 2015;175(4):523‐529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Leite VF, Rampim DB, Jorge VC, et al. Persistent symptoms and disability after COVID‐19 hospitalization: data from a comprehensive telerehabilitation program. Arch Phys Med Rehabil. 2021;102:1308‐1316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Paneroni M, Vogiatzis I, Bertacchini L, Simonelli C, Vitacca M. Predictors of low physical function in patients with COVID‐19 with acute respiratory failure admitted to a subacute unit. Arch Phys Med Rehabil. 2021;102(6):1228‐1231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Iwashyna TJ, Kamphuis LA, Gundel SJ, et al. Continuing cardiopulmonary symptoms, disability, and financial toxicity one month after hospitalization for 3rd wave COVID‐19: early results from a U.S. Nationwide Cohort. J Hosp Med. 2021;16:531‐537. [DOI] [PubMed] [Google Scholar]
- 9. Simpson R, Robinson L. Rehabilitation after critical illness in people with COVID‐19 infection. Am J Phys Med Rehabil. 2020;99(6):470‐474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Olezene CS, Hansen E, Steere HK, et al. Functional outcomes in the inpatient rehabilitation setting following severe COVID‐19 infection. PLoS ONE. 2021;16(3):e0248824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Zampogna E, Paneroni M, Belli S, et al. Pulmonary rehabilitation in patients recovering from COVID‐19. Respiration. 2021;100(5):416‐422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Schweickert WD, Pohlman MC, Pohlman AS, et al. Early physical and occupational therapy in mechanically ventilated, critically ill patients: a Randomised Controlled Trial. Lancet. 2009;373(9678):1874‐1882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Morris PE, Berry MJ, Files DC, et al. Standardized rehabilitation and hospital length of stay among patients with acute respiratory failure: a Randomized Clinical Trial. JAMA. 2016;315(24):2694‐2702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Eggmann S, Kindler A, Perren A, et al. Early physical therapist interventions for patients with COVID‐19 in the acute care hospital: a case report series. Phys Ther. 2021;101(1):1574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Johnson JK, Lapin B, Green K, Stilphen M. Frequency of physical therapist intervention is associated with mobility status and disposition at hospital discharge for patients with COVID‐19. Phys Ther. 2021;101(1):1708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Piquet V, Luczak C, Seiler F, et al. Do patients with COVID‐19 benefit from rehabilitation? Functional outcomes of the first 100 patients in a COVID‐19 rehabilitation unit. Arch Phys Med Rehabil. 2021;102(6):1067‐1074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Prvu Bettger J, Thoumi A, Marquevich V, et al. COVID‐19: maintaining essential rehabilitation services across the care continuum. BMJ Glob Health. 2020;5(5):e002670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. COVID‐19 racial and ethnic health disparities: disparities in COVID‐19‐associated hospitalizations. Centers for Disease Control and Prevention. Health Equity‐Promoting Fair Access to Health Website. National Center for Immunization and Respiratory Diseases (NCIRD) DoVD. May 17, 2021. Accessed May 27, 2021. https://www.cdc.gov/coronavirus/2019-ncov/community/health-equity/racial-ethnic-disparities/disparities-hospitalization.html
- 19. McWilliams D, Weblin J, Hodson J, Veenith T, Whitehouse T, Snelson C. Rehabilitation Levels in patients with COVID‐19 admitted to intensive care requiring invasive ventilation. An observational study. Ann Am Thorac Soc. 2021;18(1):122‐129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Joseph NP, Reid NJ, Som A, et al. Racial and ethnic disparities in disease severity on admission chest radiographs among patients admitted with confirmed coronavirus disease 2019: a Retrospective Cohort Study. Radiology. 2020;297(3):E303‐E312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Landon BE, Onnela J‐P, Meneades L, O'Malley AJ, Keating NL. Assessment of racial disparities in primary care physician specialty referrals. JAMA Network Open. 2021;4(1):e2029238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kim J. Privacy‐protecting, reliable response data discovery using COVID‐19 patient observations. J Am Med Inform Assoc. 2021;28(8):1765‐1776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Falvey JR, Burke RE, Ridgeway KJ, Malone DJ, Forster JE, Stevens‐Lapsley JE. Involvement of acute care physical therapists in care transitions for older adults following acute hospitalization: a cross‐sectional national survey. J Geriatr Phys Ther. 2019;42(3):E73‐E80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Jette DU, Brown R, Collette N, Friant W, Graves L. Physical therapists' management of patients in the acute care setting: an observational study. Phys Ther. 2009;89(11):1158‐1181. [DOI] [PubMed] [Google Scholar]
- 25. Al Shamsi H, Almutairi AG, Al Mashrafi S, Al, Kalbani T. Implications of language barriers for healthcare: a systematic review. Oman Med J. 2020;35(2):e122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Miller T, Carter SV, Smith BA. Disparities in acute decompensated heart failure. Curr Opin Cardiol. 2021;36(3):335‐339. [DOI] [PubMed] [Google Scholar]
- 27. Al Shamsi H, Almutairi AG, Al Mashrafi S, Al Kalbani T. Geographic variation and disparities in total joint replacement use for medicare beneficiaries: 2009 to 2017. J Bone Joint Surg Am. 2020;102(24):2120‐2128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Miller T, Carter SV, Smith BA. Differences in transitional care provided to Mexican American and non‐Hispanic White older adults. J Transcult Nurs. 2017;28(2):159‐167. [DOI] [PubMed] [Google Scholar]
- 29. Meagher AD, Beadles CA, Doorey J, Charles AG. Racial and ethnic disparities in discharge to rehabilitation following traumatic brain injury. J Neurosurg. 2015;122(3):595‐601. [DOI] [PubMed] [Google Scholar]
- 30. Crist JD, Koerner KM, Hepworth JT, et al. Using systematic functional measurements in the acute hospital setting to combat the immobility harm. Arch Phys Med Rehabil. 2020;28:159‐167. [DOI] [PubMed] [Google Scholar]
- 31. Meagher AD, Beadles CA, Doorey J, Charles AG. Choosing Wisely Together: physical and occupational therapy consultation for acute neurology inpatients. Neurohospitalist. 2018;8(2):53‐59. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting information.


