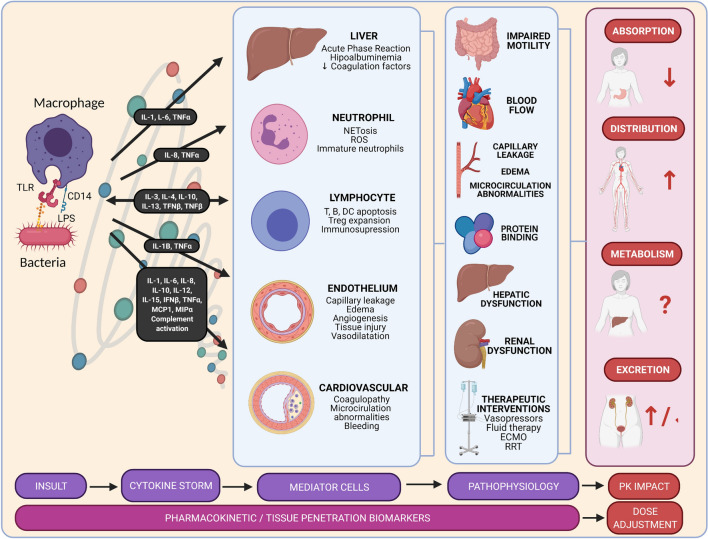
Fig. 2.
Sepsis pathophysiology and its implications in pharmacokinetics. Sepsis occurs when there is a dysregulated immune response. During infections, pathogen-associated molecular patterns, such as LPS or peptidoglycan, bind to pattern-recognizing receptors, such as TLRs, potentiated by the CD14 receptors. As a result, the immune system might respond with an exaggerated, uncontrolled, and massive release of proinflammatory cytokines. This cytokine storm results in the continuous activation and expansion of immune cells, lymphocytes, and macrophages from the circulation to the infection, with destructive effects on human tissue. Consequently, endothelial cell interactions destabilize vascular barrier damages and there is multiorgan failure. The overwhelming systemic response causes an increase in cardiac output, fluid extravasation, a decrease in protein binding, and hepatic and renal dysfunction. Together with the aggressive therapeutic interventions in the critically ill, these pathophysiological changes might lead to variability in pharmacokinetics (absorption, distribution, metabolism, and excretion). DC dendritic cell, ECMO extracorporeal membrane oxygenation, IFN interferon, IL interleukin, LPS lipopolysaccharide, MCP monocyte chemoattractant protein, MIP macrophage inflammatory protein, PK pharmacokinetics, ROS reactive oxygen species, RRT renal replacement therapy, TLR toll-like receptor, TNF tumor necrosis factor, Treg T-regulatory cells