Summary
Background
Mandatory vaccination has been mooted to combat falling childhood vaccine uptake rates in England. This study investigated parental preferences for a mandatory vaccination scheme.
Methods
Discrete choice experiment. Six attributes were investigated: vaccine, child age group, incentive, penalty, ability to opt out, and compensation scheme. Mixed effects conditional logit regression models were used to investigate parental preferences and relative importance of attributes.
Findings
Participants were 1,001 parents of children aged 5 years and under in England (53% female; mean age=33·6 years, SD=7·1; 84% white). Parental preferences were mostly based on incentives (30·7% relative importance; 80·9% [95% confidence interval 76·3–85·0%] preference for parent and 74·8% [71·0–78·3%] for child incentive; reference: no incentive) and penalties (25·4% relative importance; 69·5% [65·7–73·1%] preference for schemes where unvaccinated children cannot attend school or day care and 67·6% [63·6–71·4%] for those withholding financial benefits for parents of unvaccinated children; reference: £450 fine). Parents also preferred schemes that: offered a compensation scheme (18·1% relative importance; 66·4% [62·7–69·8%] preference; reference: not offered), mandated vaccination in children aged 2 years (versus 5 years; 11·4% relative importance; 42·6% [39·4–45·9%] preference; reference: 2 years), mandated the 6-in-1 vaccine (10·5% relative importance; 58·2% [54·6–61·7%] preference; reference: MMR), and that offered only medical exemptions (versus medical and religious belief exemptions; 4·0% relative importance; 45·5% [41·1–50·0%] preference; reference: medical exemptions).
Interpretation
These findings can inform policymakers’ decisions about how best to implement a mandatory childhood vaccination scheme in England.
Funding
Data collection was funded by a British Academy/Leverhulme Small Research Grants (SRG1920\101118).
Keywords: Childhood vaccine, Vaccine hesitancy, Financial incentives, Exemptions, Policy
Research in context.
Evidence before this study
Uptake of childhood vaccines in high-income countries has decreased in recent years. Making vaccination mandatory has the potential to increase uptake. There is no standard approach to mandatory vaccination schemes. Research suggests that the cultural context will affect perceived acceptability of vaccine laws. Mandatory vaccination has been mooted in England as a way to increase vaccine uptake. However, there is no recent research investigating parental preferences for how a mandatory vaccine scheme could be implemented.
Added value of this study
We used a discrete choice experiment to investigate English parents’ preferences for a mandatory childhood vaccination scheme. Variables included were parameters that are likely to be considered by policymakers if a mandatory vaccination scheme were to be proposed.
Implications of all the available evidence
Study results indicate that parents prefer mandatory vaccination schemes that offer financial incentives for vaccination. The penalty imposed for missing a vaccine dose, and the inclusion of a compensation scheme for severe adverse effects also influenced preferences. These results can be used to inform policy should a mandatory vaccination scheme be proposed in England.
Alt-text: Unlabelled box
Introduction
The World Health Organization estimates that 4 to 5 million lives are saved by vaccination annually; a further 1.5 million deaths could be avoided if vaccine uptake improves.1 The COVID-19 pandemic has highlighted the importance of vaccination. However, uptake of childhood vaccines is declining in high-income countries.2,3 Where vaccinations are mandatory, recent rates of non-medical exemptions have increased.4 Currently, child vaccination is voluntary in England, but mandating it has been mooted to combat falling vaccine rates.5
There is no standard approach to mandatory vaccination schemes. Approaches vary by which vaccines are mandatory, age groups included, and flexibility of the mandate (e.g. penalties, enforcement, ability to opt out, compensation for serious adverse events). Of the 105 countries that mandated vaccination in December 2018, the most common penalty used was limiting the unvaccinated child's access to schooling or day care.6 A recent review of vaccination laws in Europe found much variation between countries, and that no common “best approach” could be pinpointed.7 Instead, the report found that context in individual countries should be considered when drafting vaccine laws.
In England, there is a lack of research investigating parents’ views on, and preferences for, a mandatory vaccination scheme. This is partly because child vaccination is voluntary. The COVID-19 pandemic has re-ignited the debate around mandatory vaccination, with COVID-19 vaccination being mandated in frontline health and social care workers in England.8 Research into the acceptability of financial incentives and quasi-mandatory childhood vaccination schemes (where parents can opt their child out of vaccination for medical, religious, or philosophical reasons) in England indicates that parents prefer universal, rather than targeted, schemes, and that financial incentives are not considered appropriate motivation for vaccination.9,10 Quantitative research indicates that parents at high risk of incomplete vaccination prefer schemes offering cash incentives to no incentive; there was no preference in parents not at high risk of vaccine refusal.9, 10, 11 However, this study did not investigate parental preferences for other aspects of mandatory vaccination schemes that would need to be considered before implementation, such as the ability to opt out.
The aim of the present study was to assess parental preferences for a mandatory vaccination scheme in parents of children aged five years and under who lived in England. Subgroup analyses assessed variation in preferences in groups identified a-priori as being more likely to refuse child vaccinations and less likely to approve of mandatory vaccination.
Methods
Discrete choice experiments (DCE) allow researchers to investigate participant preferences for a number of pre-selected attributes, each with multiple levels.12 Participants are presented with two different hypothetical scenarios, known as a choice set, which vary in the levels of the attributes, and are asked to indicate their preference (scenario a, scenario b, both the same). Researchers can then identify participant preferences for the levels of each attribute and the relative weight of each attribute in participant preferences. This approach is increasingly used in health policy research.
Measures
Discrete choice experiment
Attribute selection
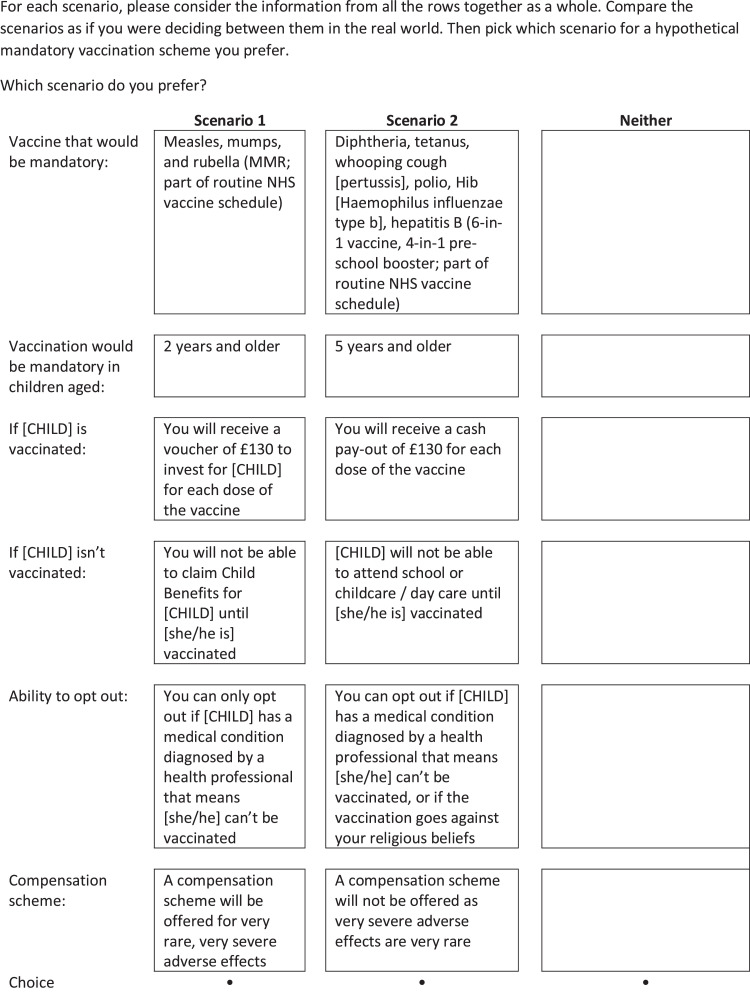
Attributes for investigation were based on a recent systematic review conducted by our team,13 and on those which are likely to be considered by policymakers if a mandatory vaccination scheme were to be proposed (see supplementary materials 1 for detailed rationale). For this study, we selected six attributes, four with two levels (vaccine [6-in-1, measles, mumps, and rubella (MMR)], child age group [2 years and older, 5 years and older], ability to opt out [medical exemptions only, medical and religious belief exemptions], availability of a compensation scheme [offered, not offered]) and two attributes with three levels (incentive [no incentive, £130 cash pay-out for parent per vaccine dose, £130 voucher for child per vaccine dose], penalty [£450 fine for each dose of the vaccine missed, child unable to attend school or childcare if unvaccinated, parent not able to claim Child Benefits1 if child not vaccinated]; Table 1).
Table 1.
Attributes and levels included in the discrete choice experiment.
| Attribute | Level 1 | Level 2 | Level 3 |
|---|---|---|---|
| Vaccine that would be mandatory: | Measles, mumps, and rubella (MMR; part of routine NHS vaccine schedule) | Diphtheria, tetanus, whooping cough [pertussis], polio, Hib [Haemophilus influenzae type b], hepatitis B (6-in-1 vaccine, 4-in-1 pre-school booster; part of routine NHS vaccine schedule) | - |
| Vaccination would be mandatory in children aged: | 2 years and older | 5 years and older | - |
| If [CHILD] is vaccinated: | You will receive a voucher of £130 to invest for [CHILD] for each dose of the vaccine | You will receive a cash pay-out of £130 for each dose of the vaccine | Neither you nor [CHILD] will receive a monetary pay-out for each dose of the vaccine |
| If [CHILD] is not vaccinated: | You will not be able to claim Child Benefits for [CHILD] until she/he is vaccinated | [CHILD] will not be able to attend school or childcare / day care until she/he is vaccinated | You will be fined £450 for each dose of the vaccine missed |
| Ability to opt out: | You can only opt out if [CHILD] has a medical condition diagnosed by a health professional that means she/he cannot be vaccinated | You can opt out if [CHILD] has a medical condition diagnosed by a health professional that means she/he cannot be vaccinated, or if the vaccination goes against your religious beliefs | - |
| Compensation scheme: | A compensation scheme will be offered for very rare, very severe adverse effects | A compensation scheme will not be offered as very severe adverse effects are very rare | - |
Experimental design
For this study, a full factorial design would require participants to rate every scenario (32 × 24 = 144); this was not practical. We used a fractional factorial design with each participant rating sixteen choice sets. The sample was split, with half receiving group set A and half receiving group set B. Thus, we used 32 choice sets (total of 64 scenarios). The design was optimised using a modified Fedorov algorithm (D-optimisation) to determine the 64 most optimal allocations, and 32 most optimal comparisons from the complete factorial design.14,15 Within each group set, choice sets were randomly presented to avoid order effects.
For each choice set, participants were asked which of the scenarios for a hypothetical mandatory vaccination scheme they preferred (scenario 1 or 2). Participants could also indicate that they did not prefer either scenario by choosing a third opt-out option (“neither”). Where participants selected that they did not prefer either scenario, they were subsequently asked to indicate which scenario was most preferable (“the least bad”). This is common practice in DCEs.9, 10, 11 Figure 1 shows an example choice set.
Figure 1.
Example choice set.
Internal validity was measured using a repeated question to check the stability of responses.16 We randomly selected a choice set from group set A and group set B, which was presented to participants at the end of the group set. The choice set was inverted (scenario 1 became scenario 2, and vice versa). Thus, participants rated a total of seventeen choice sets. Results from the internal validity choice set were not included in DCE analyses.
Final survey materials are presented in the supplementary materials 2.
Psychological factors
Participants were asked to what extent they agreed with a series of eleven statements on an eleven-point Likert scale (“strongly disagree (0)” to “strongly agree (10)”). Statements measured theoretically driven constructs associated with uptake of vaccines, guided by the Protection Motivation Theory17 and the validated Vaccination Attitudes Examination (VAX) scale,18 including perceived susceptibility and severity of vaccine preventable illnesses, perceived effectiveness and safety of child vaccines, approval of mandatory vaccination in general, thinking that vaccination campaigns are about making money for the manufacturers, preference for natural immunity and herd immunity. Statements were adapted from existing literature.10,18,19
Socio-demographic characteristics
We asked participants for their age, sex, ethnicity, highest educational qualification, employment status, total household income, marital status, how many children they were the parent or legal guardian of, and whether they had a chronic illness.
For the questionnaire, we asked participants to think about one of their children who was aged 5 years or younger (index child). We collected data about this child's age (in years), sex, and whether they had a chronic illness.
Participants provided their full postcode, from which region and index of multiple deprivation (2019) were derived.
Pilot testing
We piloted the survey, including the DCE, with five parents of children aged 5 years or younger (three female, two male) for understanding of materials. Pilot participants were asked to give their interpretation of, and answer, each question. In doing so, we were able to identify problems with phrasing and presentation of items. Comments from pilot participants resulted in framing the DCE with reference to a named index child, changes in wording to the study materials and changes in the layout of the DCE.
Data collection
Design
Data were collected using an online cross-sectional survey (conducted 20 May to 7 June 2021) conducted by Panelbase, a Market Research Society Company Partner.
Participants
Participants were recruited from two specialist research panel providers (people who have opted in to take part in online surveys; Panelbase and Lucid). Those aged 18 years or older, living in England, with a child aged 5 years or younger were eligible. Recruitment used non-probability sampling, an approach common in standard opinion polling methods. Quota sampling was based on sex (50% female), ethnicity (86% white) and Government Office Region (nationally representative) using targets from the Office for National Statistics,20 to ensure the sample was broadly representative of the English general population.
Power
A full sample size calculation would require estimates of the true values of the parameters, which are not known before beginning the research. Estimates indicate that a reliable model can be achieved with a minimum of twenty participants per choice set.21 Given 32 choice sets, we aimed to recruit 1000 participants (32 × 30 = 960), to give us adequate power for model convergence in the main analysis.
Ethics
Ethical approval for this study was granted by King's College London Psychiatry, Nursing, and Midwifery Research Ethics subcommittee (reference number LRS-20/21-21880).
Data analysis
Socio-demographic characteristics of participants, parent vaccine sentiment and approval of mandatory vaccination were analysed by index child vaccination status (not, partially or fully vaccinated).
To check D-efficient design properties of the DCE, sample attribute level balance summary statistics were calculated, orthogonality of the design was assessed by inspection of the correlation matrix, and choice sets were observed visually to inspect the overlap.
DCE analysis (mixed-effect logit regression)
Mixed effects conditional logit regression models were run to investigate parental preferences for each level of individual attributes, fitting the attributes as random effects, with 500 Halton draws.12,22 We calculated conditional preference for levels within the attributes and comparisons of relative importance of attributes, log likelihood, likelihood ratio test and the Akaike information criterion (AIC) for goodness of fit of the model. These analyses were run in Stata version 16.23
We conducted a sensitivity analysis, excluding all participants who did not answer the internal validity question consistently.
Subgroup analyses
We identified groups in whom uptake of child vaccination and approval of mandatory vaccination were lower based on parent socio-demographic characteristics. Groups and cut-offs were identified a-priori based on the literature (lower parental education [other or no qualifications, vs degree or higher], lower total household income [up to £29,999, vs £30,000 or higher], greater number of children [one, vs two, three or more; proxy for household size], not identifying as white ethnicity [white, vs other], living in London [London, vs the North (North East, North West, Yorkshire and the Humber), the Midlands (East Midlands, West Midlands, East of England), the South (South East, South West)], not being partnered [not partnered, vs partnered], younger parent age [under 30 years, vs 30 years and over]).3,9,13,24, 25, 26, 27, 28 We also grouped parents by index of multiple deprivation using a three-way split (lowest [living in most deprived deciles, 1 to 3], vs middle [living in deciles, 4 to 7], highest [living in least deprived deciles, 8 to 10].
We used dimension reduction techniques to aid feature identification for psychological factors. We conducted an exploratory factor analysis, using direct oblimin rotation as items may have been correlated. All psychological factor items were included in the factor analyses. Two components explained 62% of the variance, with the addition of a third explaining only 6% more. As the third component had an Eigenvalue of substantially less than one (0·7), we interpreted there to be two main components emerging from principal component analyses. We created a single variable (“approval of child vaccination”) by summing scores for six variables that loaded strongly onto the first component (resulting variable range 0–60), with higher scores reflecting more positive vaccination beliefs. We hypothesised that people with more positive vaccine sentiments would be more likely to vaccinate their child and to approve of mandatory vaccination schemes. To group participants a-priori, we used a tertile split (approval of child vaccination: lowest [scores 0 to 42], vs middle [scores 43 to 52], highest [scores 53 to 60]). SPSS version 26 was used for these analyses.29
DCE analyses were repeated within each subgroup.
Results
Participants
1056 participants completed the survey, but 55 were excluded for quality assurance purposes (e.g. completing the survey too quickly, or giving the same answer to several consecutive questions). Therefore, the final sample was 1001. Participants were broadly representative of the English population (53% female, 84% white ethnicity) and ranged in age between 18 and 65 years (mean=33·6 years, SD=7·1). Participant characteristics differed by child vaccination status, with female, older, white, and partnered parents being more likely to report that their child was fully vaccinated (Table 2). People who lived in London were less likely to have a fully vaccinated child, as were those whose child had a chronic illness.
Table 2.
Participant characteristics, by index child vaccination status.
| Socio-demographic characteristics | Level | Not vaccinated, n = 39 | Partially vaccinated, n = 145 | Fully vaccinated, n = 817 | p-value | |
|---|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | ||||
| Parent | Sex | Male | 28 (6·0) | 80 (17·1) | 360 (76·9) | 0·002 |
| Female | 10 (1·9) | 64 (12·1) | 456 (86·0) | |||
| Other | 1 (100·0) | 0 (0·0) | 0 (0·0) | |||
| Prefer not to say | 0 (0·0) | 1 (50·0) | 1 (50·0) | |||
| Age (years) | M, SD |
M = 31·7, SD=6·7 |
M = 31·6, SD=7·6 |
M = 34·0, SD=6·9 |
<0·001 | |
| Ethnicity | White British | 32 (4·2) | 96 (12·6) | 635 (83·2) | 0·02 | |
| White other | 1 (1·3) | 12 (15·8) | 63 (82·9) | |||
| Black and minoritised ethnic | 5 (3·3) | 33 (21·9) | 113 (74·8) | |||
| Prefer not to say | 1 (9·1) | 4 (36·4) | 6 (54·5) | |||
| Chronic illness | Not present | 24 (3·9) | 80 (12·9) | 515 (83·2) | 0·002 | |
| Present | 13 (3·7) | 52 (14·7) | 288 (81·6) | |||
| Do not know | 0 (0·0) | 6 (54·5) | 5 (45·5) | |||
| Prefer not to say | 2 (11·1) | 7 (38·9) | 9 (50·0) | |||
| Highest qualification | Degree equivalent or higher | 14 (3·2) | 56 (12·7) | 372 (84·2) | 0·09 | |
| Other or no qualifications | 24 (4·3) | 87 (15·7) | 442 (79·9) | |||
| Prefer not to say | 1 (16·7) | 2 (33·3) | 3 (50·0) | |||
| Employment status | Full-time | 26 (4) | 96 (14·7) | 530 (81·3) | 0·10 | |
| Part-time | 6 (3·8) | 24 (15·1) | 129 (81·1) | |||
| Not working/other | 6 (3·2) | 23 (12·4) | 157 (84·4) | |||
| Prefer not to say | 1 (25·0) | 2 (50·0) | 1 (25·0) | |||
| Total household income | Under £10,000 | 4 (9·8) | 6 (14·6) | 31 (75·6) | 0·09 | |
| £10,000–£19,999 | 6 (4·4) | 24 (17·8) | 105 (77·8) | |||
| £20,000–£29,999 | 10 (5·7) | 32 (18·2) | 134 (76·1) | |||
| £30,000–£39,999 | 3 (1·8) | 28 (16·7) | 137 (81·5) | |||
| £40,000–£49,999 | 6 (3·9) | 19 (12·3) | 130 (83·9) | |||
| £50,000–£74,999 | 4 (2·0) | 18 (9·1) | 175 (88·8) | |||
| £75,000 or over | 3 (3·1) | 15 (15·3) | 80 (81·6) | |||
| Do not know | 0 (0·0) | 1 (25·0) | 3 (75·0) | |||
| Prefer not to say | 3 (11·1) | 2 (7·4) | 22 (81·5) | |||
| Region | East Midlands | 3 (2·9) | 14 (13·5) | 87 (83·7) | 0·001 | |
| East of England | 5 (5·7) | 13 (14·9) | 69 (79·3) | |||
| London | 16 (8·7) | 41 (22·4) | 126 (68·9) | |||
| North East | 0 (0·0) | 6 (11·8) | 45 (88·2) | |||
| North West | 4 (3·3) | 14 (11·5) | 104 (85·2) | |||
| South East | 2 (1·4) | 14 (9·6) | 130 (89·0) | |||
| South West | 4 (5·1) | 8 (10·3) | 66 (84·6) | |||
| West Midlands | 3 (2·6) | 13 (11·4) | 98 (86·0) | |||
| Yorkshire and the Humber | 2 (1·7) | 22 (19·0) | 92 (79·3) | |||
| Partnership status | Single / separated / divorced / widowed | 8 (4·7) | 37 (21·9) | 124 (73·4) | 0·003 | |
| Married / partnered | 30 (3·6) | 108 (13) | 692 (83·4) | |||
| Prefer not to say | 1 (50·0) | 0 (0·0) | 1 (50·0) | |||
| Number of children aged 17 years or younger | One | 16 (4·4) | 58 (15·9) | 291 (79·7) | 0·37 | |
| Two | 13 (3·3) | 58 (14·8) | 320 (81·8) | |||
| Three | 7 (4·9) | 12 (8·3) | 125 (86·8) | |||
| Four or more | 3 (3·0) | 17 (16·8) | 81 (80·2) | |||
| Positive vaccine sentiment | M, SD |
M = 30·4, SD=15·1 |
M = 36·2, SD=12·2 |
M = 48·2, SD=9·8 |
<0·001 | |
| I approve of mandatory vaccination | Strongly disagree (0) to Strongly agree (10) |
M = 4·4, SD=3·3 |
M = 5·4, SD=3·2 |
M = 7·7, SD=2·6 |
<0·001 | |
| Index child | Sex | Male | 20 (3·8) | 80 (15·1) | 429 (81·1) | 0·52 |
| Female | 19 (4·0) | 64 (13·6) | 387 (82·3) | |||
| Prefer not to say | 0 (0·0) | 1 (50·0) | 1 (50·0) | |||
| Age (years) | Mean, SD |
M = 2·5, SD=1·6 |
M = 3·0, S D=1·5 |
M = 3·0, SD=1·5 |
0·12 | |
| Chronic illness | Not present | 31 (3·6) | 112 (13·0) | 717 (83·4) | <0·001 | |
| Present | 4 (3·4) | 26 (21·8) | 89 (74·8) | |||
| Do not know | 1 (10·0) | 6 (60·0) | 3 (30·0) | |||
| Prefer not to say | 3 (25·0) | 1 (8·3) | 8 (66·7) |
Parents with fully vaccinated children were likely to hold more positive vaccine sentiments and approve of mandatory vaccination (Table 2).
Discrete choice experiment
The attributes that most influenced participants’ preferences were incentives and penalties included in mandatory vaccination schemes, followed by the availability of a compensation scheme (Table 3). Participants had a strong preference for mandatory vaccination schemes that offered a financial incentive to themselves or their child for each vaccine dose, compared to not receiving an incentive. When using incentivisation to the child as the reference category, participants slightly preferred a cash incentive for themselves, compared to an incentive to their child. Compared to receiving a £450 fine for each dose of the vaccine missed, parents preferred schemes that did not allow unvaccinated children to attend school or day care and those that withheld financial benefits for parents of unvaccinated children. When denying unvaccinated children schooling or childcare was denoted as the reference category, there was no significant preference for schemes that withheld benefits for parents of unvaccinated children. Participants preferred schemes that: offered a compensation scheme, versus not offering one; mandated the 6-in-1, rather than MMR vaccine; mandated vaccination in children aged 2 years and older, compared to 5 years and older; and had a slight preference for schemes with medical exemptions only, rather than those with medical and religious exemptions.
Table 3.
Percentage of participants who have a positive preference for a mandatory vaccine scheme attribute.
| Attribute | Level | Preference mean difference (standard error) | % who prefer this level (95% CI) | p-level | Relative importance |
|---|---|---|---|---|---|
| Vaccine | MMR | Reference | 10·5% | ||
| 6-in-1 | 0·13 (0·03) | 58·2 (54·6 to 61·7) | <0·001 | ||
| Child age group | 2 years and older | Reference | 11·4% | ||
| 5 years and older | -0·14 (0·03) | 42·6 (39·4 to 45·9) | <0·001 | ||
| Incentive | No incentive | Reference | 30·7% | ||
| Incentive for child (£130 voucher) | 0·32 (0·03) | 74·8 (71·0 to 78·3) | <0·001 | ||
| Incentive for parent (£130 cash pay-out) | 0·39 (0·03) | 80·9 (76·3 to 85·0) | <0·001 | ||
| Incentive for child (£130 voucher) Incentive for parent (£130 cash pay-out) |
0·06 (0·03) | Reference 56·3 (50·0 to 62·4) |
0·05 | ||
| Penalty | £450 fine | Reference | 25·4% | ||
| Parent not able to claim Child Benefits for child until they are vaccinated | 0·29 (0·03) | 67·6 (63·6 to 71·4) | <0·001 | ||
| Child not able to attend school or childcare / day care until they are vaccinated | 0·32 (0·03) | 69·5 (65·7 to 73·1) | <0·001 | ||
| Child not able to attend school / day care until they are vaccinated Parent not able to claim Child Benefits for child until they are vaccinated |
-0·04 (0·03) | Reference 47·5 (42·8 to 52·2) |
0·30 | ||
| Ability to opt out | Medical exemption | Reference | 4·0% | ||
| Medical and religious belief exemption | -0·05 (0·03) | 45·5 (41·1 to 50·0) | 0·05 | ||
| Compensation scheme | Not offered | Reference | 18·1% | ||
| Offered | 0·23 (0·03) | 66·4 (62·7 to 69·8) | <0·001 | ||
Model fit summary statistics. Log likelihood = -10,313·87, Likelihood Ratio Test = 1,030·58, p < 0·0001, Akaike's Information Criterion = 20,661·73.
In group set A, internal validity was 63% (n = 298/473), whereas in group set B, internal validity was 67% (n = 355/528). Results of the sensitivity analysis, excluding all participants who did not answer the internal validity question consistently, found the same patterns as full group analyses (supplementary materials 3).
Subgroup analyses
Subgroup analyses followed the same pattern as in the whole sample. Major differences in subgroups are described narratively; all results are reported in the supplementary materials 4.
Socio-demographic characteristics
Participants from black and minoritized ethnic groups showed different patterns of preferences to white participants, placing more importance on the ability to opt out of a mandatory vaccination scheme (Black and minoritized ethnic group relative importance=11·1%, preference for schemes allowing medical exemptions only [27·6% (95% CI 13·7% to 46·1%) preference for schemes allowing medical and religious belief exemptions]; white group relative importance=3·0%, no preference for ability to opt out [46·7% (95% CI 42·0% to 51·4%) preference for schemes allowing medical and religious belief exemptions] and that offered a compensation scheme (Black and minoritized ethnic group relative importance=22·9%, white group relative importance=17·3%). Less emphasis was placed on which vaccine (Black and minoritized ethnic group relative importance=1·8%, no preference for vaccine [48·4% (95% CI 38·3% to 58·5%) preference for 6-in-1 vaccine]; white group relative importance=13·6%, 60·8% [95% CI 56·8% to 64·7%] preference for 6-in-1 vaccine) and age group the vaccine would be made mandatory (Black and minoritized ethnic group relative importance=5·7%, no age preference [45·7% (95% CI 36·9% to 54·8%) preference for children aged 5 years and older]; white group relative importance=11·3%, prefer schemes for children aged 2 years and older [42·7% (95% CI 39·2% to 46·2%) preference for children aged 5 years and older]).
There were some regional differences in preferences for mandatory vaccination schemes. Participants living in the South placed less emphasis on incentives (South relative importance=21·2%, other regions relative importance =26·2% to 34·3%) and penalties (South relative importance=17·2%, other regions relative importance =26·4% to 30·5%) of vaccination schemes. People living in the South and London placed more importance on the ability to opt out (South relative importance=13·4%, preference for schemes allowing only medical exemptions [38·0% (95% CI 31·1% to 45·2%) preference for schemes allowing medical and religious belief exemptions]; London relative importance=12·1%, preference for schemes allowing only medical exemptions [36·6% (95% CI 25·7% to 48·7%) preference for schemes allowing medical and religious belief exemptions]; North relative importance=4·6%, no preference for ability to opt out [60·6% (95% CI 48·6% to 71·7%) preference for schemes allowing medical and religious belief exemptions]; Midlands relative importance=0·7%, no preference for ability to opt out [49·2% (95% CI 40·6% to 57·9%) preference for schemes allowing medical and religious belief exemptions]).
Participants who reported not having a partner placed more emphasis on the ability to opt out of a mandatory vaccination scheme (participants who were not partnered relative importance=10·9%, partnered participants relative importance=6·9%). Participants who were not partnered preferred schemes that offered medical and religious belief exemptions (69·1% [95% CI 53·9% to 81·5%] preference for schemes allowing medical and religious belief exemptions), while partnered participants preferred schemes allowing only medical exemptions (42·3% [95% CI 37·7% to 47·0%] preference for schemes allowing medical and religious belief exemptions).
Participants with three or more children placed a much stronger emphasis on incentives for vaccination (participants with three or more children relative importance=39·1%, participants with two children or fewer relative importance=26·7% to 29·2%), and less emphasis on the age group in which vaccine would be mandated (participants with three or more children relative importance=1·6%, no age preference [48·8% (95% CI 41·5% to 56·1%) preference for children aged 5 years and older]; participants with two children relative importance=13·5%, preference for children aged 2 years and younger [40·7% (95% CI 35·6% to 45·9%) preference for children aged 5 years and older]; participants with one child relative importance=12·5%, preference for children aged 2 years and younger [42·6% (95% CI 37·5% to 47·9%) preference for children aged 5 years and older]). Parents aged under 30 did not show a preference for schemes that would not allow them to claim benefits for their child if not vaccinated (parents aged under 30 years, 57·9% [95% CI 47·0% to 68·2%] preference for schemes not allowing parents to claim benefits for their child if not vaccinated; parents aged 30 years or over, 70·3% [95% CI 65·9% to 74·3%] preference for schemes not allowing parents to claim benefits for their child if not vaccinated.
Psychological factors
Dimension reduction techniques indicated that psychological factors could be grouped into two distinct groups, with the first component being the most influential (supplementary materials 5). The first component reflected generally positive vaccine sentiments (“approval of child vaccines”; child vaccines are effective and safe, approval of mandatory vaccination), while the second reflected generally negative vaccine sentiments (“disapproval of child vaccines”; child vaccines cause side effects, not liking child vaccines generally, preferring natural immunity, and thinking that child vaccination campaigns are financially motivated). Factor loadings of individual items onto components are reported in supplementary materials 5.
Preferences for a mandatory vaccination scheme varied by vaccine sentiment. Those with the most positive vaccine sentiments placed less emphasis on penalties (participants with the least positive vaccine sentiments relative importance=28·7%; participants scoring in the middle range for positive vaccine sentiments relative importance=30·0%; participants with the most positive vaccine sentiments relative importance=21·1%) of the schemes, and more emphasis on the vaccine to be made mandatory (participants with the least positive vaccine sentiments relative importance=7·6%, no vaccine preference [57·0% (95% CI 49·6% to 64·1%) preference for 6-in-1 vaccine]; participants scoring in the middle range for positive vaccine sentiments relative importance=4·2%, no vaccine preference [54·3% (95% CI 47·4% to 61·0%) preference for 6-in-1 vaccine]; participants with the most positive vaccine sentiments relative importance=15·0%, 63·4% [95% CI 57·9% to 68·7%] preference for 6-in-1 vaccine) and the age group in which vaccines should be made mandatory, with participants with the least positive vaccine sentiments showing a preference for mandatory vaccination schemes that mandated vaccination in older children (participants with the least positive vaccine sentiments relative importance=9·3%, 56·2% [95% CI 50·2% to 62·0%] preference for children aged 5 years and older; participants scoring in the middle range for positive vaccine sentiments relative importance=15·8%, preference for children aged 2 years and older [37·4% (95% CI 32·0% to 43·2%) preference for children aged 5 years and older]; participants with the most positive vaccine sentiments relative importance=17·0%, preference for children aged 2 years and older [36·3% (95% CI 31·3% to 41·5%) preference for children aged 5 years and older]). Participants with the least positive vaccine sentiments showed a preference for mandatory vaccination schemes that allowed medical and religious belief exemptions (participants with the least positive vaccine sentiments, 60·2% [95% CI 51·2% to 68·6%] preference for schemes allowing medical and religious belief exemptions; participants scoring in the middle range for positive vaccine sentiments, preference for schemes allowing medical exemptions only [39·9% (95% CI 31·9% to 48·3%) preference for schemes allowing medical and religious belief exemptions]; participants with the most positive vaccine sentiments, preference for schemes allowing medical exemptions only [38·4% (95% CI 32·2% to 45·0%) preference for schemes allowing medical and religious belief exemptions]).
Discussion
We investigated English parents’ preferences for a mandatory childhood vaccination scheme. The attributes that most strongly influenced parental preferences were financial incentives for vaccination, the penalty imposed for missing a vaccine dose, and the inclusion of a compensation scheme for severe adverse effects. Our results contrast with systematic review findings that parents dislike mandatory vaccination schemes that offer financial incentives.13 This difference is likely due to selective sampling used in qualitative studies that were synthesised in the systematic review, with studies included selectively recruiting parents who had refused all vaccines for their child and who were home schooling their child in countries where school vaccine mandates were in operation. Social desirability bias may also have affected results in qualitative interview or focus group studies more so than in our anonymised survey. A previous DCE in English parents found a preference for financial incentives only in parents “at high risk” of vaccine refusal (those living in more deprivation, who had a child with a chronic illness, single parents, were aged less than 20 years, or had three or more children).10,11 However, this study included fewer parents in each subgroup and so had less power to detect smaller effects.
We found that parents preferred schemes that denied access to schooling and childcare, or that stopped parents of unvaccinated children receiving tax benefits, compared to receiving a fine for each vaccine dose missed. Systematic review findings indicate that parents felt peace of mind in schemes that restricted mixing of unvaccinated children at school or day care.13 Should a mandatory vaccination scheme be proposed, this may be the preferential option. However, caution should be taken as parents who strongly oppose vaccination may seek alternative ways to school their child such as home-schooling.30 Further research is needed to quantify the percentage of parents who may seek alternative schooling for their children if a mandatory vaccine scheme restricting access to schooling or childcare for unvaccinated children were to be implemented. Studies should investigate whether there is a disproportionate effect on children from disadvantaged groups, or those of parents who are vaccine hesitant. Care should also be taken to avoid penalizing the child for their parents’ vaccination decision.13
Implementing a mandatory vaccination scheme is unlikely to affect vaccination decisions in parents of children who vaccinate their child voluntarily. Instead, their aim is to increase uptake in those who refuse vaccines for their children. We investigated parental preferences in subgroups that were less likely to vaccinate their child and have less positive attitudes towards mandatory vaccination. There were few meaningful differences between subgroup and whole sample analyses. However, parents with the least positive vaccine beliefs using our composite measure displayed significant differences in their preferences, preferring schemes that allowed medical and religious belief exemptions (versus medical exemptions only) and that mandated vaccination in older (versus younger) children. Previous research indicates that mandating vaccination has the potential to increase vaccine refusal in children of vaccine hesitant parents,31 and entrench negative vaccine beliefs.30 While some vaccine hesitant parents may choose to vaccinate their child, it is possible that implementing a mandatory vaccination scheme that does not align with one's preferences may lead to more negative vaccine beliefs and refusal in others. Steps should be taken to quantify this before deciding to implement a mandatory vaccination scheme, and the decision to implement such a mandatory vaccine scheme should be taken with caution.
Parent-reported child vaccine uptake in this study broadly followed patterns seen in other literature and official national statistics, with lower uptake of vaccines in children of younger parents, single parents, parents of Black and minoritized ethnic groups, and parents living in London.3,24,26 Men reported lower uptake of vaccination in their children; we are unsure why this may be. Children with a chronic illness were also less likely to be vaccinated. This may be due to contraindications for vaccination, however true contraindications in children are rare. Parents with less positive vaccine sentiments also reported lower child vaccine uptake. Parents may not vaccinate their child due to lack of access to vaccination or not wanting to vaccinate.32 While mandating vaccination may affect parents’ willingness to vaccinate their child, they are unlikely to address access problems. If the decision to implement a mandatory vaccination scheme is made, care should be taken to ensure that it does not disproportionately affect disadvantaged groups.6
Strengths of this study include the use of a large sample of parents, whose socio-demographic characteristics (sex, ethnicity, region) were broadly reflective of the general English population. As quota sampling uses targets based on socio-demographic characteristics and prevents people from completing the survey if targets have already been fulfilled, response rate is not an accurate measurement of response bias. Limitations include that power to detect differences in subgroup analyses was lower than in whole-sample analyses. We are unsure whether the beliefs and attitudes of those who sign up to take part in online research are representative of the beliefs and attitudes of the general population. However associations within the data should remain valid.33 To minimise biasing of the sample towards those interested in vaccination, participants did not know the topic of the survey when choosing to take part. Internal validity for the sample was 63% (group A) to 67% (group B). This is likely because scenarios were complex. Previous research suggests that excluding participants who do not answer consistently may remove valid preferences from the data and reduce the power of the experiment.34 We conducted a sensitivity analysis, re-running DCE analyses excluding those who answered the internal validity question inconsistently; there were no differences in results. We presented participants with sixteen choice sets as part of the DCE, under the maximum recommended, to reduce the influence of research fatigue.12 We investigated parental preferences for scenarios in which there were no incentives for not vaccinating one's child, but there was no “no penalty” option. This was because we hypothesised that where there was the choice to receive or not receive a penalty for not vaccinating one's child, the preference would be not to receive a penalty. Therefore, we chose to investigate parental preferences for different types of penalties. We could have chosen different age groups for the vaccine to be mandated in, for example selecting children aged 18 months and 3 years 10 months (to allow 6 months from the recommended dates for child vaccination35), rather than aligning age groups with NHS uptake figures. As child age group had a relatively small influence on parental preferences (11·4% relative importance), we do not expect that using slightly different age groups would have a meaningful effect on the overall pattern of results. Scenarios were designed to convey that children would need to be fully immunised with the selected vaccine as appropriate for the ages selected. However, we did not specify the number of doses that a child would need to be up to date with the MMR or 6-in-1 vaccine at different ages (MMR, age 2 years: 1 dose, age 5 years: 2 doses. 6-in-1, age 2 years: 3 doses, age 5 years: 3 doses). It may have been appropriate to include other illnesses in our definition of child chronic illness (e.g. cerebral palsy) and removed others (e.g. high blood pressure), due to their prevalence in childhood. Due to the COVID-19 pandemic and additional burden that public health officials and policy makers were under, we were unable to conduct qualitative interviews to inform our DCE materials. Respondent preferences may not reflect acceptability for a mandatory vaccination scheme; further research is needed to investigate this. Results may not be generalisable to other countries or vaccines.
While mandatory vaccination schemes have been implemented in several countries, the cultural context is likely to determine their sucess.7 Results of this study should be used to inform policymakers’ decisions about how best to implement a mandatory vaccination scheme in England in the eventuality that one is proposed. Results suggest that direct financial rewards were key drivers to English parents’ preferences for a mandatory vaccination scheme, followed by the indirect financial security of having a compensation scheme in place for complications stemming from the vaccine. However, preferences differed by vaccine sentiment.
Author contributions
LS and BC conceptualised, acquired funding for the study, curated and validated data, contributed to the study methodology, and drafted the original version of the manuscript. LS is the guarantor of these findings.
Source of funding
Data collection was funded by a British Academy/Leverhulme Small Research Grants awarded to LS and BC (SRG1920\101118). The funding source had no role in analysis, decision to publish, or preparation of the manuscript. This paper represents independent research part funded by the National Institute for Health Research (NIHR) Biomedical Research Centre at South London and Maudsley NHS Foundation Trust and King's College London. The views expressed are those of the authors and not necessarily those of the NIHR or the Department of Health and Social Care.
Data sharing
Anonymised data, and an accompanying data dictionary will be made available to others after publication, beginning 3 months and ending 5 years following article publication. Researchers who provide a statistical analysis plan addressing a methodological robust legitimate research question will be able to request the data to achieve the aims in the approved proposal. Proposals should be directed to louise.e.smith@kcl.ac.uk to gain access. Data requestors will need to sign a data access agreement.
Declaration of interests
LS is a participant of the UK's Scientific Pandemic Insights Group on Behaviours (SPI-B), a subgroup of the Scientific Advisory Group for Emergencies.
Acknowledgments
The authors would like to thank Professor G James Rubin for his help with the study.
Footnotes
In England, parents can receive a Child Benefit allowance for children under 16 years old (https://www.gov.uk/child-benefit).
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.lanepe.2022.100359.
Appendix. Supplementary materials
References
- 1.World Health Organization. Immunization. 2019. https://www.who.int/news-room/facts-in-pictures/detail/immunization. Accessed 6 October 2021.
- 2.The Lancet Child & Adolescent Health Vaccine hesitancy: a generation at risk. Lancet Child Adolesc Health. 2019;3(5):281. doi: 10.1016/S2352-4642(19)30092-6. [DOI] [PubMed] [Google Scholar]
- 3.Screening and Immunisations Team, COVER Team. Childhood vaccination coverage statistics; England, 2019-20, 2020. https://digital.nhs.uk/data-and-information/publications/statistical/nhs-immunisation-statistics/england—2019-20. Accessed 6 October 2021.
- 4.Olive J.K., Hotez P.J., Damania A., Nolan M.S. The state of the antivaccine movement in the United States: a focused examination of nonmedical exemptions in states and counties. PLoS Med. 2018;15(6) doi: 10.1371/journal.pmed.1002578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vaughan A. Should the UK make childhood vaccinations mandatory? 4 November 2019. https://www.newscientist.com/article/2218087-should-the-uk-make-childhood-vaccinations-mandatory/. Accessed 6 October 2021.
- 6.Gravagna K., Becker A., Valeris-Chacin R., et al. Global assessment of national mandatory vaccination policies and consequences of non-compliance. Vaccine. 2020;38(49):7865–7873. doi: 10.1016/j.vaccine.2020.09.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vaccine Institute S. Legislative landscape review: legislative approaches to immunization across the European region, 2018. https://www.sabin.org/sites/sabin.org/files/legislative_approaches_to_immunization_europe_sabin.pdf. Accessed 6 October 2021.
- 8.Department of Health and Social Care, NHS England, Javid S. Government to introduce COVID-19 vaccination as a condition of deployment for all frontline health and social care workers. 2021. https://www.gov.uk/government/news/government-to-introduce-covid-19-vaccination-as-a-condition-of-deployment-for-all-frontline-health-and-social-care-workers. Accessed 20 November 2021.
- 9.Adams J., Bateman B., Becker F., et al. Effectiveness and acceptability of parental financial incentives and quasi-mandatory schemes for increasing uptake of vaccinations in preschool children: systematic review, qualitative study and discrete choice experiment. Health Technol Assess. 2015;19(94):1–176. doi: 10.3310/hta19940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Adams J., McNaughton R.J., Wigham S., Flynn D., Ternent L., Shucksmith J. Acceptability of parental financial incentives and quasi-mandatory interventions for preschool vaccinations: triangulation of findings from three linked studies. PLoS One. 2016;11(6) doi: 10.1371/journal.pone.0156843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Flynn D., Ternent L., Becker F., Oluboyede Y., Adams J. Parental preferences for the organization of preschool vaccination programs including financial incentives: a discrete choice experiment. MDM Policy Pract. 2017;2(1) doi: 10.1177/2381468317708319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mangham L.J., Hanson K., McPake B. How to do (or not to do) ... Designing a discrete choice experiment for application in a low-income country. Health Policy Plan. 2009;24(2):151–158. doi: 10.1093/heapol/czn047. [DOI] [PubMed] [Google Scholar]
- 13.Smith L.E., Hodson A., Rubin G.J. Parental attitudes towards mandatory vaccination; a systematic review. Vaccine. 2021;39(30):4046–4053. doi: 10.1016/j.vaccine.2021.06.018. [DOI] [PubMed] [Google Scholar]
- 14.Cook R.D., Nachtsheim C.J. A comparison of algorithms for constructing exact D-optimal designs. Technometrics. 1980;22(3):315–324. [Google Scholar]
- 15.Carlsson F., Martinsson P. Design techniques for stated preference methods in health economics. Health Econ. 2003;12(4):281–294. doi: 10.1002/hec.729. [DOI] [PubMed] [Google Scholar]
- 16.Johnson F.R., Yang J.C., Reed S.D. The internal validity of discrete choice experiment data: a testing tool for quantitative assessments. Value Health. 2019;22(2):157–160. doi: 10.1016/j.jval.2018.07.876. [DOI] [PubMed] [Google Scholar]
- 17.Rogers RW, Prentice-Dunn S. Protection motivation theory. 1997.
- 18.Martin L.R., Petrie K.J. Understanding the dimensions of anti-vaccination attitudes: the vaccination attitudes examination (VAX) scale. Ann Behav Med. 2017;51(5):625–660. doi: 10.1007/s12160-017-9888-y. [DOI] [PubMed] [Google Scholar]
- 19.Smith L.E., Webster R.K., Weinman J., Amlôt R., Yiend J., Rubin G.J. Psychological factors associated with uptake of the childhood influenza vaccine and perception of post-vaccination side-effects: a cross-sectional survey in England. Vaccine. 2017;35(15):1936–1945. doi: 10.1016/j.vaccine.2017.02.031. [DOI] [PubMed] [Google Scholar]
- 20.Office for National Statistics. Population estimates for the UK, England and Wales, Scotland and Northern Ireland: mid-2018. 2019. https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/bulletins/annualmidyearpopulationestimates/mid2018. Accessed 3 March 2020.
- 21.Lancsar E., Louviere J. Conducting discrete choice experiments to inform healthcare decision making: a user's guide. Pharmacoeconomics. 2008;26(8):661–677. doi: 10.2165/00019053-200826080-00004. [DOI] [PubMed] [Google Scholar]
- 22.Hole A.R. Fitting mixed logit models by using maximum simulated likelihood. Stata J. 2007;7(3):388–401. [Google Scholar]
- 23.StataCorp. Stata statistical software: release 16. College Station, TX: StataCorp LLC; 2019.
- 24.Falagas M.E., Zarkadoulia E. Factors associated with suboptimal compliance to vaccinations in children in developed countries: a systematic review. Curr Med Res Opin. 2008;24(6):1719–1741. doi: 10.1185/03007990802085692. [DOI] [PubMed] [Google Scholar]
- 25.Forshaw J., Gerver S.M., Gill M., Cooper E., Manikam L., Ward H. The global effect of maternal education on complete childhood vaccination: a systematic review and meta-analysis. BMC Infect Dis. 2017;17(1):801. doi: 10.1186/s12879-017-2890-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tabacchi G., Costantino C., Napoli G., et al. Determinants of European parents' decision on the vaccination of their children against measles, mumps and rubella: a systematic review and meta-analysis. Hum Vaccines Immunother. 2016;12(7):1909–1923. doi: 10.1080/21645515.2016.1151990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Office for National Statistics. Average household income, UK: financial year 2020. 21 January 2021. https://www.ons.gov.uk/peoplepopulationandcommunity/personalandhouseholdfinances/incomeandwealth/bulletins/householddisposableincomeandinequality/financialyear2020. Accessed 14 April 2021.
- 28.Office for National Statistics. Births by parents’ characteristics. 2019 edition of this dataset ed; 2020. https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/livebirths/datasets/birthsbyparentscharacteristics. Accessed 14 April 2021.
- 29.IBM Corp. IBM SPSS Statistics for Windows, Version 26.0. Armonk, NY: IBM Corp; 2019.
- 30.Omer S.B., Betsch C., Leask J. Mandate vaccination with care. Nature. 2019;571(7766):469–472. doi: 10.1038/d41586-019-02232-0. [DOI] [PubMed] [Google Scholar]
- 31.Armiento R., Hoq M., Kua E., et al. Impact of Australian mandatory 'No Jab, No Pay' and 'No Jab, No Play' immunisation policies on immunisation services, parental attitudes to vaccination and vaccine uptake, in a tertiary paediatric hospital, the Royal Children's Hospital, Melbourne. Vaccine. 2020;38(33):5231–5240. doi: 10.1016/j.vaccine.2020.05.094. [DOI] [PubMed] [Google Scholar]
- 32.Elliman D., Bedford H. Should the UK introduce compulsory vaccination? Lancet N Am Ed. 2013;381(9876):1434–1436. doi: 10.1016/S0140-6736(13)60907-1. [DOI] [PubMed] [Google Scholar]
- 33.Kohler U. Possible uses of nonprobability sampling for the social sciences. Survey Methods: Insights from the Field 2019.
- 34.Lancsar E., Louviere J. Deleting ‘irrational’ responses from discrete choice experiments: a case of investigating or imposing preferences? Health Econ. 2006;15(8):797–811. doi: 10.1002/hec.1104. [DOI] [PubMed] [Google Scholar]
- 35.UK Health Security Agency. Routine childhood immunisations from February 2022. 21 February 2022. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1055502/UKHSA-12155-routine-childhood-immunisation-schedule_Feb2022.pdf. Accessed 22 February 2022.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.