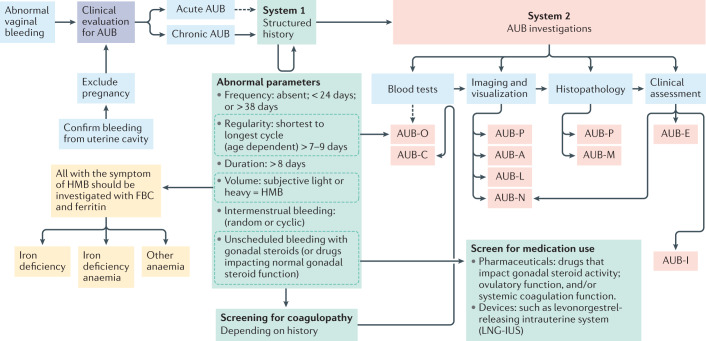
Fig. 5. Diagnostic pathway for abnormal uterine bleeding, and iron deficiency and/or iron deficiency anaemia.
On presentation with abnormal vaginal bleeding, the patient requires an initial assessment for pregnancy and to determine that the bleeding is coming from within the uterus, to confirm abnormal uterine bleeding (AUB). Such bleeding might either be acute or chronic (or acute on chronic). The time frame in which acute AUB is investigated varies, as the initial clinical priority is to stem the acute haemorrhage. In those with chronic AUB, it is necessary to perform a thorough assessment to determine the cause or causes in order to direct management. These include understanding the precise AUB symptoms using the International Federation of Gynecology and Obstetrics (FIGO) AUB System 1 (green boxes)2 prior to undertaking the appropriate investigations to identify the cause or causes of AUB using FIGO AUB System 2 classification (red boxes)2. Imaging and visualization can occur with one or a combination of transvaginal ultrasonography, sonohysterography, MRI and hysteroscopy. Of note, blood tests for AUB-C would follow a positive screen for coagulopathy. AUB-O is primarily diagnosed on the basis of the structured history and blood tests are generally not necessary, but measurement of serum levels of progesterone might be useful in selected instances. AUB-E is a primary disorder of endometrial haemostasis. The clinician makes this diagnosis if there is no other explanation found on the clinical assessment including history, physical examination, appropriate blood tests and uterine imaging. HMB, heavy menstrual bleeding; FBC, full blood count.