Figure 3. Potential influence of the gut microbiota and their associated SCFAs on osseointegration.
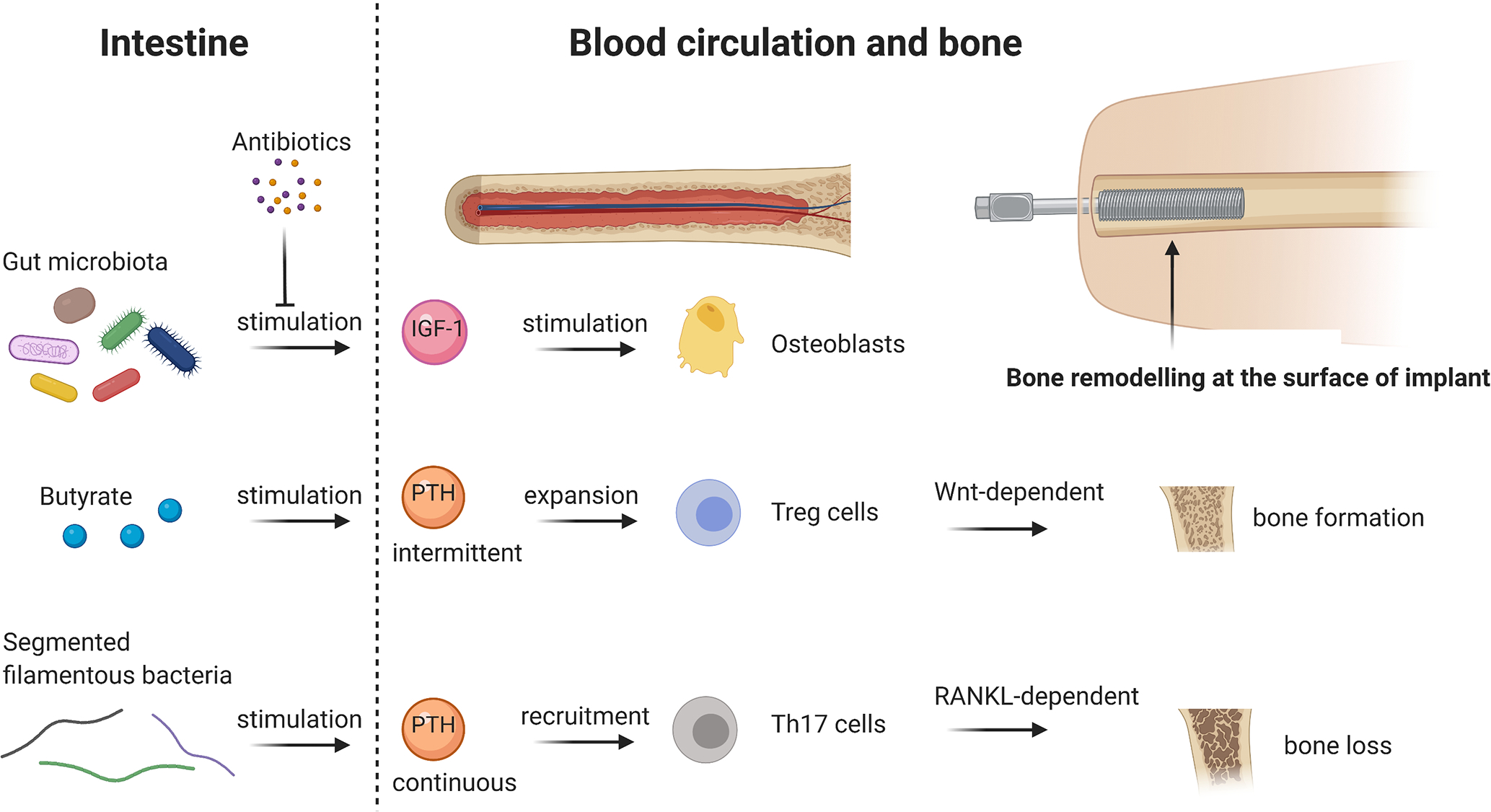
The presence of the gut microbiota increases IGF-1 hormone levels in serum, which further stimulate osteoblasts and bone formation, respectively. In contrast, eradication of the gut microbiota by antibiotics decreases IGF-1 in serum and therefore inhibits bone formation. SCFAs, namely butyrate, stimulate intermittent, physiological PTH release, which expands Treg cells in the bone marrow and further enhances bone formation in a Wnt-dependent way. However, the presence of segmented filamentous bacteria stimulates continuous PTH release, as it is the case in hyperthyroidism. This leads to Th17 recruitment in the bone marrow and causes RANKL-dependant bone loss. Bone remodelling, in particular bone formation, at the surface of an implant is crucial for proper osseointegration and the gut microbiota could be a potent regulator in this process. Abbreviations: IGF-1 = Insulin-like growth factor 1, PTH = Parathyroid hormone, Wnt = wingless-related integration site, RANKL = receptor activator of NF-κB ligand. Figure created with BioRender.com.
