Fig. 4 |. Platelet and endothelial interactions.
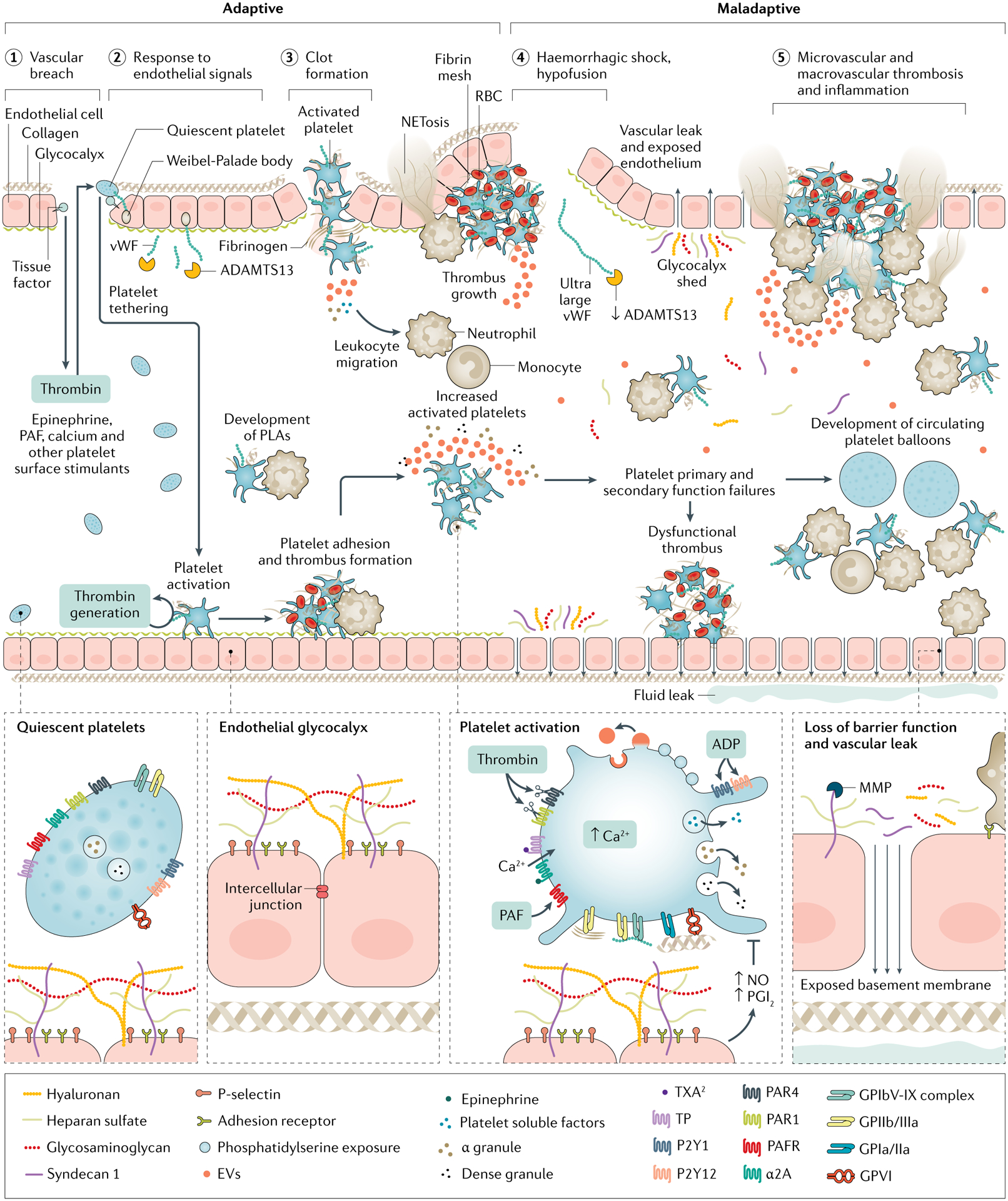
Projecting beyond the cell membrane of healthy endothelial cells is a glycocalyx of polysaccharides linked to membrane and trans-membrane proteoglycans, which is fortified with soluble glycoproteins that coordinate coagulation and immune functions. The glycocalyx provides cytoprotection, membrane integrity and anti-apoptotic antithrombotic signalling. Clot formation relies on platelet plug construction (primary haemostasis), which begins with platelet tethering and adhesion to exposed extravascular matrices including tissue factor and collagen via von-Willebrand factor (vWF). Extravascular adhesion and thrombin stimulation activate platelets, resulting in procoagulant calcium mobilization, structural changes, soluble factor degranulation, phosphatidylserine exposure and glycoprotein (GP) IIb/IIIa receptor conformational change to accept fibrin binding. Additionally, platelets control local fibrinolysis via degranulation of soluble factors from alpha granules including plasminogen activator inhibitor-1 (PAI-1) and α2 antiplasmin to maintain prothrombotic, antifibrinolytic clot architecture. Secondarily, activated platelets recruit leukocytes to local environments. Further, via reciprocal release of trophogens, platelets promote endothelial stability and angiogenesis in return for endothelial control of platelet-dependent haemostasis and release of cytokines that signal megakaryopoiesis. However, in trauma-induced coagulopathy, platelet activation pathways are maladaptive, that is, they result in primary and secondary platelet function failures. This is characterized by altered and shed glycoprotein VI and Ibα, impaired extracellular and intracellular calcium, circulating soluble platelet inhibitors, altered granule content and loss of endothelial protection and trophogenesis. Further, a procoagulant and pro-inflammatory milieu is promoted by circulating platelet–leukocyte aggregates (PLAs) and platelet ballooning, sustained exocytosis and impaired clearance of vWF by ADAMTS13 (a disintegrin and metalloproteinase with thrombospondin motifs 13), and metalloproteinase (MMP) cleavage of the protective ectodomains of glycocalyx components exposing neutrophil adhesion receptors for neutrophil binding and release of chemoattractant molecules and cytokines. In this setting, the endothelium becomes denuded and leaky. These trauma-induced coagulopathy (TIC)-associated procoagulant and pro-inflammatory platelet and endothelial biologies are associated with micro-thrombosis and macro-thrombosis. EV, extravcellular vesicle; PAF, platelet activating factor; PAR, protease-activating receptor, PGI2, prostaglandin I2; RBC, red blood cell; TP, TXA2/PG endoperoxidases; TXA, tranexamic acid; TXA2, thromboxane A2.
