Abstract
Objective
To determine the impacts of the Medicaid expansion on revenues, costs, assets, and liabilities of federally funded community health centers.
Data sources
We combined data from the Uniform Data System, Internal Revenue Service nonprofit tax returns, and county‐level characteristics from the Census Bureau. Our final dataset included 5841 center‐year observations.
Study design
We used difference‐in‐differences model to estimate the fiscal impacts of the Medicaid expansion on community health centers. We employed event study models, state‐specific trend models, and placebo law tests as robustness checks.
Data collection methods
Not applicable.
Principal findings
On the revenue side, we found a $2.08 million relative increase (p = 0.002) in Medicaid revenues, offset by a $0.44 million decrease (p = 0.015) in total grants among community health centers in expansion states compared with centers in non‐expansion states. On the expenditure side, we found a large but not statistically significant $0.98 million relative increase (p = 0.201) in total expenditures among centers in expansion states. Uncompensated care for health centers in expansion states decreased by $1.19 million (p < 0.001) relative to their counterparts in non‐expansion states.
Conclusions
Community health centers in expansion states benefited from the increased, stable revenue stream from Medicaid expansions. While Medicaid revenue increased as a result of the policy, we find no major evidence of substitution away from other revenue lines, with one notable exception (i.e., substitution away from state and local government grants). From a policy perspective, these results are encouraging as the Biden Administration starts to implement the safety‐net enhancements from the American Rescue Plan Act of 2021 and as more non‐expansion states are considering opting into Medicaid expansions. It is anticipated that these added revenue streams will help to sustain health centers in the delivery of health care services to the underserved population.
Keywords: Affordable Care Act, community health centers, Medicaid expansion
What is known on this topic
Medicaid expansion has led to increased utilization of community health centers.
The early studies on the impact of Medicaid expansions on community health centers staffing were inconclusive.
What this study adds
Community health centers in expansion states benefited from the increased, stable revenue stream from Medicaid expansions.
While Medicaid revenue increased as a result of the Medicaid expansion, we find no major evidence of substitution away from other revenue lines, with one exception (decreased grants).
1. INTRODUCTION
Community health centers (CHCs) are “community‐based and patient‐directed” not‐for‐profit organizations that deliver comprehensive primary care to medically underserved areas. CHCs serve primarily uninsured and Medicaid patients. In 2019, 1385 health centers served nearly 30 million patients, of which 48.2% were on Medicaid, and 22.7% were uninsured. 1 CHCs are important safety‐net providers; they are required to provide services to all patients regardless of their ability to pay.
Starting in 2014, selected states expanded their Medicaid eligibility to cover all individuals under 138% of Federal Poverty Line (FPL), as part of the Affordable Care Act (ACA). As of today, 36 states and the District of Columbia expanded income eligibility for Medicaid. 2 Medicaid expansions led to a sharp increase in Medicaid coverage in expansion states. 3
Medicaid expansions were expected to have profound impacts on CHCs because they disproportionally serve uninsured and low‐income populations. Indeed, prior research has found clear evidence of increased utilization and decreased uninsured rates among CHC patients due to the ACA and state‐specific expansions. 4 , 5 , 6 , 7 , 8 The effect of Medicaid expansions on CHCs' finances, however, remains unclear. In this study, we aim to address this gap in knowledge by investigating the impact of Medicaid expansions on a broad range of CHC's financial outcomes with the added contribution of gauging the actual dollar amounts and flows. Additionally, we examine possible substitutions in revenue lines that may have occurred in response to the expansion of Medicaid. For instance, did federal, state, local, or private grants decline concomitantly with the addition of Medicaid funding? Moreover, we investigate whether the services provided by the CHCs have expanded, and whether the financial stability of CHCs has improved as a result of Medicaid expansion.
Considering the fact that CHCs rely heavily on Medicaid revenue, and that many centers tend to operate at or below the breakeven point (CHCs' total margins were 0.8% on average in 2019), it is imperative to understand the impact of Medicaid expansions on the substitution between different sources of CHCs' revenue. In particular, if the Medicaid expansion caused more reliance on revenue sources that are contingent on service volume (e.g., Medicaid reimbursement) rather than those that are not (e.g., grants), this may leave CHCs at greater risk of financial instability when service volume is disrupted due to any unexpected major event. The COVID‐19 pandemic is a case in point. The pandemic has caused substantial disruptions in all sectors of the economy, including health care, whereby reductions in health care utilization led to sharp declines in revenues. Some estimates suggest that CHCs experienced a roughly 30% decline in their revenues during the pandemic due to the reduction in patient visits. 9 Thus, understanding the degree of substitution between revenue sources in the pre‐pandemic period of Medicaid expansions will also shed light on the financial consequences of service delivery disruptions from current and potentially future catastrophic events.
1.1. Conceptual model
1.1.1. Assumptions
To better understand the reallocation of funds and payment sources in response to Medicaid expansion, we rely on related microeconomic literature positing substitution away from various payment sources as Medicaid benefits become more generous. 10 , 11 , 12 Particularly, we rely on Martin and Wildasin's conceptual framework of an autonomous State agency that faces an incentive to shift resources away from primary indigent health care (e.g., Medicaid, uninsured) to other programs, in response to the federal subsidies.
While their approach is highly stylized, we can draw useful insights from a simple adaptation of their model. Accordingly, we initially posit a state agency utility function, in which the state values two types of services, health care to the poor (indicated by h; either through Medicaid or grants to health care providers to cover uninsured) versus services in other programs (indicated by o). The agency also faces a budget constraint, where it attempts to match its tax receipts with direct spending on the health care to the poor (state contribution in direct patient care in Medicaid and grants to health care providers) and other constituent programs. Using fundamental economics, from the agency's perspective, the optimal allocation occurs when
U h is the marginal utility from providing health care services to the poor, P h is the costliness of those services borne by the state (price); U o and P o are the corresponding values for other programs. States will allocate resources away from health care to the poor and toward other programs if the relative value of health care to the poor is less than the relative value of other programs (U h /P h < U o /P o ).
1.1.2. Expected effect of the federal subsidy
With enhanced Medicaid, the federal government subsidizes a larger proportion of Medicaid costs, leaving the state to cover less of the cost, effectively lowering P h and the costliness of providing health care to the poor relative to other programs. This gives rise to the substitution effect by allocating resources from other state programs to health care for the poor. Concomitantly, the decrease in P h increases the purchasing power of the state to cover expenditures in both services (income effect). These two effects operate in opposite directions, and which effect is dominant is the matter of empirical question. If the substitution effect is dominant, state will allocate resources from o to h. On the contrary, if the income effect is dominant, the state will allocate resources from h to o. In this case, state has the option to reduce the generosity of the Medicaid program or to reallocate resources from grants to health care providers to other programs. However, states have less incentive to reduce the generosity of the Medicaid given that they share program costs with the federal government, thus a $1 reduction in Medicaid expenditures has less than a $1 impact on the state's budget constraint. Additional details on theoretical model are presented in the Supporting information.
1.1.3. Substitutions within direct patient care programs
Medicaid expansions may have reduced the number of uninsured patients seeking care from CHCs. We would expect Medicaid expansion to increase the stream of revenues from Medicaid yet decrease out‐of‐pocket payments by self‐pay patients. Because Medicaid payments exceed self‐pay enumeration and help cover previously uncompensated care, we expect patient revenue to increase overall in CHCs in expansion states relative to non‐expansion states. The overall effect of Medicaid expansion on total revenue (sum of patient revenue and grants) is unknown since the magnitude of the effect of Medicaid expansion on grants is ambiguous. Moreover, by reducing uncompensated care, we would expect Medicaid expansion to improve financial stability of CHCs.
2. STUDY DATA AND METHODS
2.1. Data
The primary database we used is Uniform Data System (UDS) for the period of 2010–2018. UDS data are maintained by the Bureau of Primary Health Care (BPHC) of the Health Resources and Services Administration. Grantee Health Centers of Section 330 under the Public Health Service Act are required to report health center level information including staffing levels, patient demographic and utilization, selected diagnostic categories visits, and other information annually.
The other important data source was the IRS Form 990 that provides information on capital stock and expenditure of nonprofit CHCs. The electronically filed 990 Forms are publicly available from IRS, hosted by Amazon Web Services. Paper filed 990 Forms are publicly available from ProPublica Nonprofit Explorer. We used address, zip code, city name, and organization name to match the 990 forms with the UDS data. The accounting year for CHCs might differ from the calendar year. In these cases, we combined the weighted average of outcome variables based on the number of calendar year days that overlap with each tax return. IRS 990 Forms are due roughly 6 months after the closing of an organization's fiscal year with a potential extension of another 6 months. Thus, we found very few organizations with complete data from IRS Form 990 for 2018 since many tax returns covering 2018 calendar year (which involves accounting years 2017, 2018, and 2019) were not submitted until 2020. Because of the aforementioned limitation in tax return data, we only used data from 2010 to 2017 for the analysis involving form IRS 990.
We engaged in extensive data cleaning to match outcomes reported in fiscal years as closely as possible to calendar years, address CHCs merger and acquisitions, and address outlier (likely incorrect) values; see Supporting information for more detail.
In the analysis, we also included CHC‐level time‐varying covariates from UDS and county‐level covariates from Census Bureau, Economic Research Service, and Kaiser Family Foundation; see Supporting information for more detail. The complete list of covariates and the sources is presented in Appendix Table A1, in Supporting information.
2.2. Inclusion and exclusion criteria of states and sample selection
We followed Simon et al. 13 to categorize expansion states into “full expansion,” “substantial expansion,” and “mild expansion” states based on past expansion provisions and marginal increases in Medicaid enrolled populations. In our primary analysis, we used full‐expansion and non‐expansion states, and excluded substantial and mild expansion states that partially expanded Medicaid to childless adult before 2014. For sensitivity analysis, we included substantial and mild expansion states in our sample (see Table 1 and Appendix Table A2 in Supporting information). 14 Additionally, we excluded all health centers outside of 50 US states and DC. We also dropped CHCs that never received community health center grants from BPHC as well as those that do not file IRS 990 Forms (CHCs operated by a state university health system, an Indian tribal organization, or a government entity). We then constructed a balanced sample by excluding centers closed or opened during the study period. The final sample includes 5841 observations from 649 CHCs. The CONSORT flowchart of inclusion and exclusion criteria is presented in Appendix Figure A1, in Supporting information.
TABLE 1.
Medicaid expansion states (2010–2018)
| State | Treatment/control/exclusion status | Expansion type |
|---|---|---|
| Alabama | C [.] | None |
| Alaska | T [2016] | Full |
| Arizona | T [2014] | Full |
| Arkansas | T [2014] | Full |
| California | Excluded (early expansion) | Substantial |
| Colorado | T [2014] | Full |
| Connecticut | Excluded (early expansion) | Substantial |
| Delaware | Excluded (early expansion) | Mild |
| District of Columbia | Excluded (early expansion) | Mild |
| Florida | C [.] | None |
| Georgia | C [.] (will expand in 2021) | Substantial |
| Hawaii | Excluded (early expansion) | Substantial |
| Idaho | C [.] (expanded in 2020) | Full |
| Illinois | T [2014] | Full |
| Indiana | T [2015] | Full |
| Iowa | T [2014] | Full |
| Kansas | C [.] | None |
| Kentucky | T [2014] | Full |
| Louisiana | T [2017] | Full |
| Maine | C [.] (expanded in 2019) | Full |
| Maryland | T [2014] | Full |
| Massachusetts | Excluded (early expansion) | Mild |
| Michigan | T [2014] | Full |
| Minnesota | Excluded (early expansion) | Substantial |
| Mississippi | C [.] | None |
| Missouri | C [.] (will expand in 2021) | Full |
| Montana | T [2016] | Full |
| Nebraska | C [.] (expanded in 2020) | Full |
| Nevada | T [2014] | Full |
| New Hampshire | T [2015] | Full |
| New Jersey | T [2014] | Full |
| New Mexico | T [2014] | Full |
| New York | Excluded (early expansion) | Mild |
| North Carolina | C [.] | None |
| North Dakota | T [2014] | Full |
| Ohio | T [2014] | Full |
| Oklahoma | C [.] (will expand in 2021) | Full |
| Oregon | T [2014] | Full |
| Pennsylvania | T [2015] | Full |
| Rhode Island | T [2014] | Full |
| South Carolina | C [.] | None |
| South Dakota | C [.] | None |
| Tennessee | C [.] | None |
| Texas | C [.] | None |
| Utah | C [.] (expanded in 2020) | Full |
| Vermont | Excluded (early expansion) | Mild |
| Virginia | C [.] (expanded in 2019) | Full |
| Washington | T [2014] | Full |
| West Virginia | T [2014] | Full |
| Wisconsin | Excluded (early expansion) | Substantial |
| Wyoming | C [.] | None |
Note: Medicaid expansion status through year‐end 2018. See Appendix Table A2 in Supporting information for additional details and sources. In the “inclusion/exclusion column,” C = control (non‐expansion), T = treatment (full expansion); other states are excluded.
2.3. Variables
2.3.1. Dependent variables
We study five broad range of outcomes: (i) CHCs' revenue including total revenue from all sources (patient revenue and grants), total patient revenue, Medicaid revenue, Medicare revenue, private revenue, other public revenue (mostly from state‐funded public insurance program), and self‐pay revenue; (ii) uncompensated care loss defined as sum of bad debt and sliding discount for self‐pay patients; (iii) grants including total grants, federal grants (BPHC grants and other federal grants), state and local government grants, and private grants; (iv) expenditures including total expenditures and by type of services (medical, dental health, mental health, and substance abuse treatments), overhead costs, and capital expenditures; and (v) assets and liabilities including cash reserves, capital stock, and total liabilities (as these measures are frequently used to assess the financial stability of a nonprofit organization). 15
2.3.2. Primary independent variables
The primary independent variable of interest is Medicaid expansion, a dummy variable set to 1 for expansion states in post‐expansion years and 0 otherwise. Medicaid expansion dummy variable takes the value of 1 if a state had implemented Medicaid expansion in the first half of the year or earlier and 0 otherwise. If a state implemented Medicaid expansion in the second half of a year, we treated that state as a non‐expansion state in that year, and as an expansion state in the subsequent years. Non‐expansion states were defined as states that had not implemented Medicaid expansion by July 2018. The list of other covariates is presented Appendix Table A1 in Supporting information.
2.4. Statistical analysis
We analyzed the overall change in outcome variables using difference‐in‐differences (DID) approach. We estimate:
| (1) |
where i indexes CHCs, c indexes county, s indexes states, and t indexes year. represents the expansion status of states in year t ( is the coefficient of interest). and are CHC‐specific and county‐level time‐varying variables. 16 is year fixed effect, is CHC fixed effect, and is the error term. All the outcomes are measured in million dollars. We cluster standard errors at the state level.
The DID approach assumes that the outcomes in treated and control states would have evolved in parallel in the absence of treatment. This assumption is not directly testable, but it is more plausible to hold if the trends appear to be parallel during the pretreatment period. We used the event study (i.e., leads‐and‐lags) to investigate the plausibility of parallel trends, as well as the dynamics of post‐treatment effects. We estimate:
Here, k indexes “event time” relative to the ACA Medicaid expansion year. = 0 for control states for all t and k. For treatment states, = 1 for the kth year relative to the expansion year, 0 otherwise. For example, takes the value of 1 4 years before the expansion, 0 otherwise; = 1 2 years after expansion, 0 otherwise. Therefore, α 0 provides the estimated effect at the year when Medicaid is expanded. α 1 provides the effect of reform 1 year after the expansion, and α −1 is the estimated effect 1 year before the expansion. Since the IRS tax return data were available through 2017 for most CHCs, we include four leads and four lags for outcomes from UDS and four leads and three lags for outcomes from IRS tax return data. We adjust the coefficients by subtracting α −3 from each, so that the reported α −3 ≡ 0. The wax and wane of lag terms () could be viewed as the change of policy impact over time.
3. RESULTS
Table 2 presents the descriptive statistics separately for CHCs in expansion states and non‐expansion states in the pre‐expansion years (2010–2013). CHCs in expansion states had higher revenues, driven primarily by higher Medicaid revenues. Federal grants were very similar in expansion and non‐expansion states. On the other hand, CHCs in expansion states received higher state and local government grants before the implementation of Medicaid expansion, but the difference falls short of statistical significance at the conventional level. CHCs in expansion states also experienced higher costs, driven primarily by higher medical costs and overhead costs.
TABLE 2.
Summary statistics (averages for years 2010–2013)
| Non‐expansion states | Expansion states | Difference | ||||
|---|---|---|---|---|---|---|
| Variablea | Mean | SD | Mean | SD | Estimate | p‐Value |
| Revenues | ||||||
| Total revenues | 10.114 | [10.053] | 12.813 | [14.401] | −2.699 | (0.000) |
| Total patient revenues | 5.756 | [6.490] | 8.320 | [10.989] | −2.564 | (0.000) |
| Medicaid | 3.039 | [4.191] | 5.231 | [7.978] | −2.192 | (0.000) |
| Self‐pay | 0.982 | [1.039] | 0.894 | [1.050] | 0.088 | (0.028) |
| Medicare | 0.781 | [1.289] | 0.807 | [1.067] | −0.025 | (0.575) |
| Other public | 0.162 | [0.517] | 0.145 | [0.507] | 0.017 | (0.391) |
| Private | 0.791 | [1.222] | 1.242 | [2.170] | −0.451 | (0.000) |
| Grants | ||||||
| Total grants | 4.358 | [4.655] | 4.493 | [4.454] | −0.135 | (0.440) |
| BPHC grants | 2.472 | [2.032] | 2.396 | [2.226] | 0.075 | (0.361) |
| Other federal grants | 0.595 | [1.023] | 0.691 | [1.216] | −0.096 | (0.028) |
| State and local government grants | 0.890 | [2.891] | 1.028 | [1.714] | −0.137 | (0.123) |
| Private grants | 0.401 | [0.941] | 0.378 | [0.722] | 0.023 | (0.476) |
| Uncompensated care loss | 3.023 | [3.849] | 2.419 | [3.068] | 0.605 | (0.000) |
| Expenditures | ||||||
| Total costs | 9.991 | [9.996] | 12.685 | [14.311] | −2.694 | (0.000) |
| Medical services | 4.183 | [4.016] | 5.248 | [6.165] | −1.064 | (0.000) |
| Dental health services | 0.824 | [1.083] | 1.095 | [1.445] | −0.271 | (0.000) |
| Mental health services | 0.356 | [1.428] | 0.341 | [0.843] | 0.015 | (0.733) |
| SUD Tx services | 0.025 | [0.128] | 0.033 | [0.177] | −0.007 | (0.216) |
| Overhead expenditures | 3.310 | [3.404] | 4.299 | [5.024] | −0.989 | (0.000) |
| Capital expenditures | 0.720 | [0.843] | 1.416 | [9.703] | −0.696 | (0.013) |
| Assets and liabilities | ||||||
| Total assets | 6.147 | [6.703] | 11.646 | [64.399] | −5.499 | (0.003) |
| Cash reserves | 1.602 | [2.492] | 2.263 | [4.023] | −0.662 | (0.000) |
| Capital stock | 7.059 | [7.238] | 16.229 | [134.761] | −9.170 | (0.018) |
| Total liabilities | 2.741 | [3.739] | 7.267 | [63.085] | −4.527 | (0.013) |
Note: Table presents mean of annual outcome variables (in millions) in 23 full‐expansion states and 18 non‐expansion states for 2010–2013, including two‐sample p value for differences in means.
Bold values are indicates p < 0.05.
3.1. Revenues and uncompensated care
Panel A of Table 3 presents the covariate‐adjusted DID estimates on revenue outcomes and uncompensated care. The DID analysis shows that CHCs in expansion states experienced a $1.28 million relative increase (p = 0.12) in total revenues compared with their counterparts in non‐expansion states, or a 9.9% increase relative to pre‐expansion mean in expansion states. This was due to a relative $1.72 million increase (21% increase, p = 0.02) in patient revenue and a relative decline of $0.44 million (9.8% decline, p = 0.02) in total grant revenue (see next section). The relative increase in total patient‐related revenues was driven by an increase in Medicaid revenue ($2.08 million or 40% increase, p = 0.002), offset by a decline in self‐pay revenue ($0.19 million or 21% decline, p < 0.001) and in other public insurance revenue ($0.08 million or 50% decline, p = 0.06). Uncompensated care declined by a relative 1.19 million (49% decrease, p < 0.001). There was no statistically significant change in Medicare revenue that we treat as a placebo outcome that should not be affected by Medicaid expansion.
TABLE 3.
Difference‐in‐differences estimates of Medicaid expansion on financial outcomes
| Panel A—Revenues and uncompensated care loss | |||||||
|---|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (7) | (8) | (9) |
| Total | Total patient | Medicaid | Self‐pay | Medicare | Other public | Private | Uncompensated care loss |
| [12.81] | [8.32] | [5.23] | [0.89] | [0.81] | [0.16] | [1.24] | [2.42] |
| 1.28 | 1.72** | 2.08*** | −0.19*** | 0.07 | −0.08* | −0.16 | −1.19*** |
| (0.81) | (0.74) | (0.62) | (0.05) | (0.09) | (0.04) | (0.13) | (0.16) |
| Panel B—Grants awarded | ||||
|---|---|---|---|---|
| Total grants | BPHC grants | Other federal grants | State and local government grants | Private grants |
| [4.49] | [2.40] | [0.69] | [1.03] | [0.72] |
| −0.44** | −0.05 | −0.06 | −0.21*** | −0.11 |
| (0.17) | (0.10) | (0.05) | (0.08) | (0.11) |
| Panel C—Expenditures | ||||||
|---|---|---|---|---|---|---|
| Total | Medical | Dental health | Mental health | Substance use disorder | Overhead | Capital |
| [12.68] | [5.25] | [1.10] | [0.34] | [0.03] | [4.30] | [1.42] |
| 0.98 | 0.26 | 0.11 | 0.09 | 0.01 | 0.34 | 0.07 |
| (0.75) | (0.25) | (0.13) | (0.06) | (0.01) | (0.23) | (0.05) |
| Panel D—Assets and liabilities | |||
|---|---|---|---|
| Total assets | Cash | Capital stock | Total liabilities |
| [6.15] | [1.6] | [7.06] | [2.74] |
| 0.76 | 0.40 | 0.90 | 0.43 |
| (0.56) | (0.24) | (0.62) | (0.37) |
Note: Difference‐in‐difference estimates of Medicaid expansion on financial outcomes of CHCs in full‐expansion states versus non‐expansion states. All the outcomes are in millions. Regressions include CHC and year fixed effects and time‐varying CHC and county‐level characteristics. Coefficients on other covariates are suppressed. Numbers in brackets are means of the dependent variables during 2010–2013 in expansion states. Standard errors are shown in parentheses and clustered at the state level. *, **, *** indicate statistical significance at 10%, 5%, and 1% level.
3.2. Grants awarded
Panel B of Table 3 presents covariate‐adjusted DID estimates for all of the grant funding CHCs receive. We found a statistically significant decline of $0.44 million (p = 0.02) for CHCs in expansion states relative to those in non‐expansion states. The effect of Medicaid expansion on individual categories of grants was less precisely estimated. Medicaid expansion did not have a statistically significant effect on BPHC grant, other federal grants, and private grants. However, point estimates were all negative. On the other hand, there was a statistically significant decline in state and local government grants ($0.21 million or 20% decline, p = 0.008).
3.3. Expenditures
Panel C of Table 3 presents covariate‐adjusted DID estimates on expenditure outcomes. CHCs in expansion states experienced a $0.98 million (8% increase, p = 0.20) relative increase in total expenditures after Medicaid expansion, compared with CHCs in non‐expansion states. Medicaid expansions did not have a statistically significant effect on distinct categories of expenditures, including medical, dental health, mental health, substance use disorder treatment, overhead expenditures, and capital expenditures.
3.4. Assets and liabilities
Panel D of Table 3 presents the simple DID estimates and covariate‐adjusted DID estimates on assets and liabilities. Adjusting for covariates, the increase in total assets was not statistically significant ($0.76 million or 12% increase, p = 0.184). However, CHCs in expansion states experienced a $0.90 million (12% increase, p = 0.157) relative increase in capital stock, and a $0.43 million (16% increase, p = 0.109) relative increase in cash reserve after Medicaid expansion. The effects of Medicaid expansions on total liability were not statistically significant.
3.5. Event study models
Figure 1 presents results from event study models for selected financial outcomes. The leads and lags for the remaining outcomes are reported in Appendix Figure C1 in Supporting information. The black dots in the graphs represent the point estimates of event study models, and the orange bars represent the 95% confidence interval around the point estimates. Period 0 in the graphs represents the expansion year in event time.
FIGURE 1.
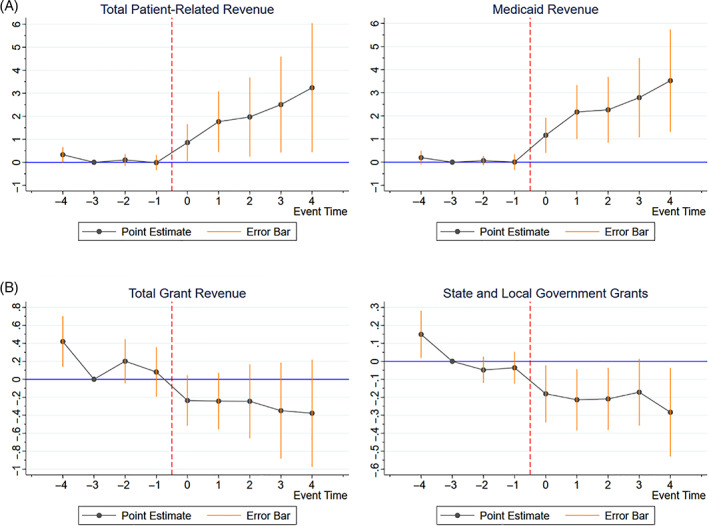
Event studies (leads‐and‐lags models) of the financial impacts of Medicaid expansions on community health centers. (A) Patient‐related revenues. (B) Grants awarded. Event study of the impacts of Medicaid expansions on community health centers' finances in full‐expansion states versus non‐expansion states. Sample, covariates, and fixed effects are similar to our DID model. Error bars represent a 95% confidence interval around the point estimates. Standard errors are clustered at the state level [Color figure can be viewed at wileyonlinelibrary.com]
All revenue categories except revenue from other public insurance sources display flat pretreatment trends, confirming that the findings from the simple DID model are plausibly causal. The minor exception of a decline in other public insurance revenues (mostly from state‐funded public insurance program) post‐treatment appears to be a continuation of pretreatment trends. Uncompensated care losses were declining prior to the expansion, but there is clear evidence of change in trend after expansion (Figure 1A; Appendix Figure C1, Panels A and B in Supporting information).
The pretreatment trends for grant revenue were reasonably flat and declined after Medicaid expansion. There is no evidence of change in BPHC grant and other federal grants. There is clear evidence of decline in state and local government grants and private grants after the Medicaid expansion. However, the event‐year‐specific coefficients were not individually significant for private grants (Figure 1B; Appendix Figure C1, Panel C in Supporting information).
There is clear evidence of post‐expansion increases in expenditures. Although the event‐year‐specific coefficients are not statistically significant for most expenditure categories, there is clear evidence of change in trend after Medicaid expansion, and the post‐expansion coefficients are jointly significant. Pretreatment trends were reasonably flat for all the outcomes except substance use expenditures. Substance use expenditure increased in expansion states relative to non‐expansion states before the expansions and continued to rise thereafter (Appendix Figure C1, Panel D in Supporting information).
Most categories in assets and liabilities exhibited differential pretreatment trends. There is one notable exception, cash reserves in CHCs in expansion states increased relative to their counterparts in non‐expansion states, with reasonably parallel pretreatment trends (Appendix Figure C1, Panel E in Supporting information). Additionally, our state‐by‐state analysis confirms that our results were not driven by select group of states (Appendix Figure C2 in Supporting information).
3.6. Robustness check
3.6.1. Alternative specifications and samples
We conducted the following robustness checks to ensure that our findings were not explained by the choice of identification strategy or sample: (i) inclusion of linear state‐specific time trends in our specification; (ii) inclusion into the treatment group states with “substantial” and “mild” expansions; (iii) use of log‐transformed outcomes as dependent variables; (iv) and inclusion of centers that either opened or closed between 2010 and 2018.
Inclusion of state‐specific time trends resulted in smaller coefficients for most outcome, but the coefficients remained mostly consistent with our findings from the main specification in terms of the effect sign and statistical significance. There were some notable differences: The decline in state and local government grants was no longer statistically significant after the inclusion of state‐specific trends, and the coefficient on the effect of Medicaid expansion on capital stock changed sign. Adding “substantial” and “mild” expansion states to the treatment group resulted in larger coefficients for most outcomes. However, these results should be interpreted with caution since leads‐and‐lags graphs of these robustness checks (available upon request) exhibited evidence of nonparallel pretreatment trends for most outcomes. These states expanded Medicaid at lower eligibility threshold before 2014, which can cause a change in outcomes relative to non‐expansion states. These states experienced another major expansion when ACA Medicaid expansion went into effect. Thus, it is difficult to discern the effect of these early expansions from the ACA Medicaid expansion. The results from log‐transformed outcomes were in general agreement with our main findings. Given that linear models yield more directly interpretable results in terms of the revenue flows of interest, we opted to focus on the non‐transformed outcomes in our main specification. The results from the unbalanced panel were very similar to the results from the main specification. Detailed results of robustness checks are given in Appendix Tables B1 to B4, in Supporting information.
3.7. Inference
By clustering standard error at the state level, the inference relies on the assumption that the error terms are correlated within each state. Clustering standard errors also requires a large enough number of clusters to prevent downward bias in estimating standard errors. We assess the risk of bias in standard errors in our main specification by implementing a randomized inference test based on placebo laws. 17 , 18 Here, we first randomly select a set of pseudo treatment observations and then re‐estimate the DID model using the pseudo sample. We repeat these steps 1000 times. We finally compare the observed estimates from the main specification against the distribution of DID estimates from the placebo. We expect the distribution of these pseudo treatments to be normally distributed, centered around zero. We further expect the estimated coefficients from the main specification to lie on the tail of the distribution of placebo estimates.
This test relies on the assumption that the policy variable is independent of potential outcomes conditional on covariates and fixed effects included in the model (which is the basis of our DID identification strategy) and does not impose any assumption about clustering and serial correlation. However, as Wing and Marie 17 pointed out, the true process of adopting Medicaid expansion is unknown to researchers. Thus, we tested three different permutation strategies: (i) permuting state‐year that randomizes states as well as expansion years; (ii) permuting expansion year that holds the expansion states similar to those in our main specification and randomizes expansion year; and (iii) permuting expansion states that keep the expansion years similar to those in our main specification and randomizes the expansion states. The placebo law generally confirms that clustered standard errors are unlikely to overstate estimator precisions, and in some cases, indicates clustered standard errors might be overly conservative. See Appendix Figure C3 in Supporting information and related discussion therein.
4. DISCUSSION
This study evaluated the impact of Medicaid expansions on a sample of CHCs during the 2010–2018 period, focusing on five aspects of CHC finances: revenues, uncompensated care cost, grants, expenditures, and assets and liabilities. Five general findings are particularly notable. First, as expected, Medicaid expansions resulted in a greater increase in Medicaid revenues at centers located in expansion states relative to those in non‐expansion states. Second, the relative increase in Medicaid revenue outweighs declines in other sources of revenue and grants, resulting in an overall increase in CHCs' revenue. Third, the increase in Medicaid revenues was countered by relatively moderate declines in state and local government grants. On average, centers in expansion states experienced a relative increase of $2.08 (40%) million in Medicaid revenues, compared with a statistically significant decline of $0.21 million in state and local government grant funding.
Fourth, the relative increase in revenues for CHCs in expansion states is accompanied by a relative increase in expenditures. Indicating that the additional resources available to the CHCs have been translated into additional services to the community. Fifth, notwithstanding the national urgency of the opioid addiction epidemic, there was only a very limited and not statistically significant increase in substance abuse treatment expenditures in expansion states relative to non‐expansion states during our sample period, even though other studies have suggested that access to and utilization of substance use treatments had increased in expansion states relative to non‐expansion states. 19 , 20
Our analysis is restricted to private, nonprofit CHCs and does not include CHCs operated by local government or tribal organizations. Thus, our results cannot be generalized to all CHCs. Moreover, the UDS data only provide information at the grantee level, and we are unable to conduct analysis at separate CHC sites level.
These findings have several policy implications. First, while CHCs in expansion states seized the opportunity to gain more revenue, cut on their uncompensated care losses, and provide more services to the community, they were juggling two main sources of funding to keep their operation afloat: patient revenues, particularly from Medicaid, and grants, federal grants more specifically. As uninsured patients gained Medicaid coverage in Medicaid expansion states, CHCs had less of a need for grants to defray the cost of providing care to uninsured patients, thereby creating incentives for governmental agencies to shift away grants from CHCs, causing CHCs to rely more heavily on patient revenue. While this shift did not impact the flow of federal grants, it led to a significant reduction in state and local government grants in expansion states. Patient revenue requires maintaining patient volume. If a decline in patient revenue occurs for some reason, such as a loss of patient volume due to the COVID‐19 pandemic, CHCs in expansion states would then quickly face a deepening dilemma between meeting the community needs and their ability to maintain their operations, particularly when the loss in patient revenue is not replenished by grants.
This research raises related questions regarding the potential impact of the COVID‐19 epidemic on the financial stability of CHCs. On the one hand, the pandemic is known to have caused disruptions in health care utilization across the board, potentially leading to losses. While demand for primary care services appears to be recovering presently, the full extent of the effect of pandemic on the utilization patterns is not yet known. On the other hand, financial assistance offered to CHCs in conjunction with the pandemic (e.g., in the CARES Act of 2020 and in the American Rescue Plan Act of 2021) may have provided a basis for future sustainability. Future research may focus on the differential effects of COVID in expansion and non‐expansion states.
Overall, CHCs in expansion states benefited from the increased, stable revenue stream from Medicaid expansions. From a policy perspective, these results are encouraging as the Biden Administration starts to implement the safety‐net enhancements from the American Rescue Plan Act of 2021 and as more non‐expansion states may be considering opting into Medicaid expansions. It is anticipated these added revenue streams will help to sustain health centers in the delivery of health care services to the underserved population.
CONFLICT OF INTEREST
None of the authors has any affiliation or financial involvement that conflicts with the material presented in this report.
Supporting information
Appendix S1. Supporting information.
ACKNOWLEDGMENTS
This project was funded under grant number 1R01HS026816‐01 from the Agency for Healthcare Research and Quality (AHRQ), U.S. Department of Health and Human Services (HHS). The authors are solely responsible for this document's contents, findings, and conclusions, which do not necessarily represent the views of AHRQ. Readers should not interpret any statement in this report as an official position of AHRQ or of HHS.
Luo Q, Moghtaderi A, Markus A, Dor A. Financial impacts of the Medicaid expansion on community health centers. Health Serv Res. 2022;57(3):634-643. doi: 10.1111/1475-6773.13897
Funding information Agency for Healthcare Research and Quality (AHRQ), U.S. Department of Health and Human Services (HHS), Grant/Award Number: 1R01HS026816‐01
REFERENCES
- 1. Health Resources and Services Administration (HRSA) . National Health Center Data (2019 UDS). 2020. Accessed December 15, 2020. https://data.hrsa.gov/tools/data-reporting/program-data/national
- 2. Kaiser Family Foundation . Status of state action on the Medicaid expansion decision. 2021. Accessed March 15, 2021. https://www.kff.org/health-reform/state-indicator/state-activity-around-expanding-medicaid-under-the-affordable-care-act
- 3. Decker SL, Lipton BJ, Sommers BD. Medicaid expansion coverage effects grew in 2015 with continued improvements in coverage quality. Health Aff. 2017;36(5):819‐825. doi: 10.1377/10.1377/hlthaff.2016.1462 [DOI] [PubMed] [Google Scholar]
- 4. DeVoe JE, Marino M, Gold R, et al. Community health center use after Oregon's randomized Medicaid experiment. Ann Fam Med. 2015;13(4):312‐320. doi: 10.1370/10.1370/afm.1812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hatch B, Bailey SR, Cowburn S, Marino M, Angier H, DeVoe JE. Community health center utilization following the 2008 medicaid expansion in Oregon: implications for the affordable care act. Am J Public Health. 2016;106(4):645‐650. doi: 10.2105/10.2105/AJPH.2016.303060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Angier H, Hoopes M, Gold R, et al. An early look at rates of uninsured safety net clinic visits after the affordable care act. Ann Fam Med. 2015;13(1):10‐16. doi: 10.1370/10.1370/afm.1741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Cole MB, Galarraga O, Wilson IB, Wright B, Trivedi AN. At federally funded health centers, Medicaid expansion was associated with improved quality of care. Health Aff. 2017;36(1):40‐48. doi: 10.1377/10.1377/hlthaff.2016.0804 [DOI] [PubMed] [Google Scholar]
- 8. Han X, Luo Q, Ku L. Medicaid expansion and grant funding increases helped improve community health center capacity. Health Aff. 2017;36(1):49‐56. doi: 10.1377/10.1377/hlthaff.2016.0929 [DOI] [PubMed] [Google Scholar]
- 9. Corallo B, Tolbert J. Impact of coronavirus on community health centers. Kaiser Family Foundation. 2020. Accessed December 15, 2020. https://www.kff.org/coronavirus-covid-19/issue-brief/impact-of-coronavirus-on-community-health-centers/
- 10. Cutler DM, Gruber J. Does public insurance crowd out private insurance? Q J Econ. 1996;111(2):391‐430. [PubMed] [Google Scholar]
- 11. Marton J, Wildasin DE. State government cash and in‐kind benefits: intergovernmental fiscal transfers and cross‐program substitution. J Urban Econ. 2007;61(1):1‐20. doi: 10.1016/10.1016/j.jue.2006.04.006 [DOI] [Google Scholar]
- 12. Craig SG, Howard LL. Is Medicaid crowding out other state government expenditure? Internal financing and cross‐program substitution. Reg Sci Urban Econ. 2014;49:164‐178. doi: 10.1016/10.1016/j.regsciurbeco.2014.09.003 [DOI] [Google Scholar]
- 13. Simon K, Soni A, Cawley J. The impact of health insurance on preventive care and health behaviors: evidence from the first two years of the ACA Medicaid expansions. J Policy Anal Manage. 2017;36(2):390‐417. doi: 10.1002/10.1002/pam.21972 [DOI] [PubMed] [Google Scholar]
- 14. Moghtaderi A, Pines J, Zocchi M, Black B. The effect of affordable care act Medicaid expansion on hospital revenue. Health Econ. 2020;29(12):1682‐1704. doi: 10.1002/10.1002/hec.4157 [DOI] [PubMed] [Google Scholar]
- 15. Boris ET, Steuerle CE, Sonnevi G. Scope and dimensions of the nonprofit sector. In: Powell WW, Steinberg R, eds. The Nonprofit Sector: A Research Handbook. 2nd ed. Yale University Press; 2006:66‐88. [Google Scholar]
- 16. Luo Q, Dor A, Pittman P. Optimal staffing in community health centers to improve quality of care. Health Serv Res. 2021;56(1):112‐122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Wing C, Marier A. Effects of occupational regulations on the cost of dental services: evidence from dental insurance claims. J Health Econ. 2014;34(1):131‐143. doi: 10.1016/10.1016/j.jhealeco.2013.12.001 [DOI] [PubMed] [Google Scholar]
- 18. Bunnenberg S, Meyer S. Trusting difference‐in‐differences estimates more: an approximate permutation test. SSRN. 2016. doi: 10.2139/10.2139/ssrn.2805116 [DOI]
- 19. Wen H, Hockenberry JM, Borders TF, Druss BG. Impact of Medicaid expansion on Medicaid‐covered utilization of buprenorphine for opioid use disorder treatment. Med Care. 2017;55(4):336‐341. [DOI] [PubMed] [Google Scholar]
- 20. Maclean JC, Saloner B. The effect of public insurance expansions on substance use disorder treatment: evidence from the affordable care act. J Policy Anal Manage. 2019;38(2):366‐393. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. Supporting information.


