Abstract
Air pollution, to which children are more susceptible than adults, can promote airway inflammation, potentially exaggerating the effects of respiratory viral infection. This study examined the association between the clinical manifestation of COVID-19 in unvaccinated pediatric patients hospitalized in Poland (n = 766) and levels of particulate matter 2.5 (PM2.5) and benzo(a)pyrene (B(a)P) within a week before hospitalization. Children aged ≤ 12 years exposed to mean and max 24 h B(a)P levels > 1 ng/m3 revealed higher odds of cough, dyspnea, fever, and increased concentrations of inflammatory markers (C-reactive protein, interleukin-6, procalcitonin, white blood cell count). In older patients (13–17 years), elevated mean 24 h B(a)P levels increased odds of dyspnea, fever, and diarrhea, and higher concentrations of C-reactive protein and procalcitonin. Exposure to max 24 h PM2.5 levels > 20 µg/m3 was associated with higher odds of cough, increased concentrations of C-reactive protein (group ≤12 years), and increased procalcitonin concentration (groups ≤12 years and 13–17 years). In both age groups, length of stay was extended in patients exposed to elevated levels of max 24 h PM2.5, mean and max 24 h B(a)P. This study suggests that worse air quality, particularly reflected in increased B(a)P levels, might affect the clinical course of COVID-19 in pediatric patients and adds to the disease burden during a pandemic.
Keywords: Pandemic, Particulate matter, Benzo(a)pyrene, Pediatric, Inflammation, Epidemiology
Graphical Abstract
1. Introduction
The COVID-19 pandemic has posed a tremendous challenge to the healthcare system, overwhelming its different sectors and branches. The hospitalized patients mainly included elderly individuals suffering from obesity and various comorbidities. Although children are susceptible to SARS-CoV-2 infection and contribute to its spread in the population, most pediatric cases are asymptomatic or mild with fever and cough but no hospitalization requirement (Jackson et al., 2022). The risk of severe disease and death in this group is low (Mania et al., 2022, Pokorska-Śpiewak et al., 2021). Despite it, some children and adolescents require hospitalization and may develop pediatric inflammatory multi-system syndrome due to SARS-CoV-2 infection (Ward et al., 2022).
Apart from socioeconomic and ethnicity disparities, comorbidities, such as asthma, diabetes, cardiovascular diseases, neurologic disorders obesity, were identified as the leading risk factor of severe COVID-19 in children. In particular, medically complex individuals are more likely to be hospitalized due to SARS-CoV-2 infection (Graff et al., 2021, Woodruff et al., 2021). At the same time, it is known that air pollutants, such as particulate matter (PM), especially its PM2.5 fraction (with aerodynamic diameter ≤ 2.5 µm), and benzo(a)pyrene, can act as an irritant and promote inflammation in the respiratory tract (Rzymski et al., 2022). Compared to adults, children are at higher risk of the adverse effects of these pollutants due to smaller airway caliber with lower pulmonary capacity but a higher respiratory rate and more susceptible epithelium (Kurt et al., 2016, Babin et al., 2007; I.-J. Wang et al., 2016).
This study aimed to analyze whether air pollution, PM2.5 and B(a)P, is related to the severity of COVID-19 among patients aged < 18 years (n = 766) who required hospitalization in selected Polish medical units over 17 months of the pandemic. Specifically, the relations between increased levels of air pollutants and the manifestation of various COVID-19 symptoms, the concentration of inflammatory markers at admission, oxygen saturation, and length of hospital stay were examined. Both pollutants considered in the present study are particularly concerning in regions such as Central Europe, where the combustion of wood and coal continues to play a role in domestic heating. This results in elevated emissions of PM and PM-bound polycyclic hydrocarbons, especially between late autumn and early spring (Anioł et al., 2021, Nazar and Niedoszytko, 2022). Moreover, contrary to many world regions, the COVID-19 lockdown in Poland was not associated with a temporary decline in PM emissions, while in selected locations, they were even increased (Rogulski and Badyda, 2021).
2. Material and methods
2.1. Patients data
All clinical data of hospitalized patients aged < 18 years were retrieved from the SARSTer database, managed by the Polish Association of Epidemiologists and Infectiologists. A total of 766 records of children, and adolescents, hospitalized with COVID-19 in different healthcare units in Poland between March 2020 and July 2021 (17 months) were collected. All patients were unvaccinated against COVID-19. All of these individuals were diagnosed and treated according to the Polish recommendations for the management of COVID-19 (Flisiak et al., 2020a, Flisiak et al., 2021, Flisiak et al., 2020, Flisiak et al., 2020b, Marczyńska et al., 2020, Okarska-Napierała et al., 2021).
The clinical data collected for this study included:
-
(i)
frequency of early COVID-19 symptoms cough, dyspnea, fatigue, fever, headache, fatigue, anosmia, nausea, diarrhea, and vomiting;
-
(ii)
levels of inflammatory markers at admission: C-reactive protein (CRP), interleukin-6 procalcitonin (PCT), interleukin-6, and white blood cell (WBC) – the following levels were defined as hyperinflammation: CRP > 10 mg/L, IL-6 > 37 pg/mL, PCT > 0.1 ng/mL and WBC > 11 × 103/µL (Yasuhara et al., 2020, Shafiek et al., 2021);
-
(iii)
the parameters of the clinical course of the disease: oxygen saturation (SpO2) at admission, the need for oxygen therapy and mechanical ventilation, length of hospital stay, and outcome (survival or death).
As the immune system undergoes changes in children and adolescents (Bartlett et al., 1998), two age groups were considered: ≤ 12 years and 13–17 years. Moreover, the previous epidemiological studies have shown that individuals aged 13–17 years are far more likely to be infected with SARS-CoV-2 and experience symptomatic infection than ≤ 12 years (Jang et al., 2022, Ryan et al., 2022). Moreover, in the present study, these two age groups had a similar sex distribution and did not differ in frequencies of comorbidities.
The study had a retrospective, non-interventional nature, and according to the Polish law (Dz.U. 2020 poz. 1291) it did not require written consent from patients and bioethical approval. All personal data were protected according to the European Union General Data Protection Regulation.
2.2. Air pollution data
The following air pollution parameters were included in the analysis: PM2.5, and B(a)P. The data was collected from the Polish Chief Inspectorate Of Environmental Protection database, which is legally responsible for the air pollution monitoring in Poland. The mean 24 h and max 24 h levels in the inhabited area during a week preceding the hospitalization were retrieved for each patient. If more than one air quality monitoring station was available in a particular area, the data were collected from all of them and averaged. The period of the week before hospitalization was chosen because it most likely represented a time of transition of SARS-CoV-2 infection from incubation phase to symptomatic one, a time during which the innate immune response constitutes an essential line of the antiviral defense (Rzymski et al., 2022)(Kasuga et al., 2021, Diamond and Kanneganti, 2022). Its disruption can lead to cellular overactivation and hyper-inflammation, subsequently favoring a more severe clinical course of COVID-19 and worsening the prognosis (Peyneau et al., 2022, Galani and Andreakos, 2021, Blot et al., 2020, Janssen et al., 2021). In turn, air pollutants such as PM2.5 and B(a)P have been evidenced to promote inflammation and adversely affect innate immune response (Glencross et al., 2020). As shown in experimental and epidemiological studies, the pro-inflammatory effect may also occur in the respiratory system following the short-term exposure to increased levels of these pollutants (Fan et al., 2021; Y. Li et al., 2021; Coker et al., 2021; Chen et al., 2017).
The following air quality limits were considered in this study: mean 24 h and max 24 h PM2.5 > 20 µg/m3, and mean 24 h and max 24 h B(a)P > 1.0 ng/m3 (Directive 2004/107/EC,, Directive 2008/50/EC,)
2.3. Statistical analysis
The data was analyzed with Statistica v. 13.1 (StatSoft, USA) separately for patients aged ≤ 12 and 13–17 years. For continuous variables, differences were tested with a Student's t-test. To evaluate associations between exceedance of air pollution limits and symptomatology, biochemical parameters, and clinical course, the classical odds ratios (ORs) with a 95% confidence interval (CI) were calculated according to the formulas given by Bland and Altman using MedCalc (MedCalc, Ostend, Belgium). A p-value < 0.05 was considered statistically significant.
3. Results
3.1. Group characteristics
The studied group constituted 766 pediatric patients aged 0–17 years hospitalized between March 2020 and July 2021 due to COVID-19. None of the individuals was vaccinated. Their demographic characteristics and general clinical data are presented in Table 1. The number of patients requiring oxygen therapy or mechanical ventilation was very low, similar to fatal cases.
Table 1.
Demographic and basic clinical characteristics of the studied group of pediatric patients (n = 766).
|
Age (years), mean±SD ≤ 12 years, n (%) 13–17 years, n (%) |
7.5 ± 5.9 557 (72.7) 209 (27.3) |
| Male / female, n (%) | 406 (53) / 360 (47) |
| Comorbidities, n (%) Asthmatic children, n (%) |
158 (20.6) 10 (1.3) |
| Exposed to air pollution exceeding the limits mean 24 h PM2.5 > 20 µg/m3, n (%) max 24 h PM2.5 > 20 µg/m3, n (%) mean 24 h B(a)P > 1 ng/m3, n (%) max 24 h B(a)P > 1 ng/m3, n (%) |
43 (5.6) 205 (26.8) 292 (38.1) 377 (49.2) |
| Hospital stay (days), mean±SD | 4.4 ± 5.8 |
| Requiring oxygen therapy, n (%) | 9 (1.2) |
| Requiring mechanical ventilation, n (%) | 2 (0.3) |
| Fatal cases, n (%) | 1 (0.1) |
3.2. Air pollution and early symptoms of COVID-19
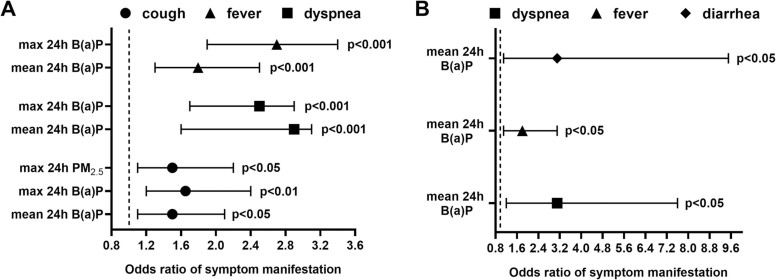
Association between exposure to air pollution above quality limits and the presence of selected early symptoms of COVID-19 were observed ( Fig. 1). The odds of cough, fever, and dyspnea were higher in children aged ≤ 12 years exposed to high mean and max levels of 24 h B(a)P. Odds of cough were also increased in this group when exposed to elevated max 24 h PM2.5 levels (Fig. 1A). Exposure to max 24 h B(a)P level exceeding the limit increased odds of fever, dyspnea, and diarrhea in patients aged 13–17 years (Fig. 1B). Exceedances of air pollution parameters did not alter the odds of other symptoms considered in the study.
Fig. 1.
The odds ratio (95% confidence interval) of early COVID-19 symptoms manifestation in relation to the exposure of pediatric patients aged < 12 years (A) and 13–17 years (B) to air pollution parameters exceeding limits during a week before hospitalization.
3.3. Air pollution and inflammatory markers at admission
The levels of inflammatory markers in the studied groups are summarized in Table 2. In the group aged ≤ 12 and 13–17 years, significantly elevated IL-6 concentrations were noted in individuals exposed to max 24 h PM2.5 (by 3.8-fold and 8.6-fold, respectively), mean 24 h B(a)P (by 5.7-fold and 8.8-fold, respectively) and max 24 h B(a)P (by 5.4-fold and 4.9-fold, respectively) at levels exceeding the limits exhibited significantly elevated IL-6 concentrations at admission. PCT concentrations were increased only in children aged ≤ 12 years exposed to high levels of mean 24 h B(a)P (by 2.0-fold) and max 24 h B(a)P (by 4.0-fold). CRP and WBC concentrations were significantly elevated in children aged ≤ 12 years exposed to increased levels of mean 24 h B(a)P (by 1.8-fold and 1.1-fold, respectively) and max 24 h B(a)P (by 2.0-fold and 1.1-fold, respectively). In addition, both parameters were higher in individuals aged 13–17 exposed to mean 24 h B(a)P exceeding the limit (by 2.0-fold and 1.1-fold, respectively).
Table 2.
The inflammatory markers (mean±SD) in patients aged < 18 years (n = 766) exposed to air pollutants exceeding/not exceeding the limits during a week before hospitalization.
| Parameter | Age group |
mean 24 h PM2.5 |
max 24 h PM2.5 |
mean 24 h B (a)P |
max 24 h B (a)P |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ≤ 20 µg/m3 | > 20 µg/m3 | p | ≤ 20 µg/m3 | > 20 µg/m3 | p/t | ≤ 1 ng/m3 | > 1 ng/m3 | p | ≤ 1 ng/m3 | > 1 ng/m3 | p | ||
| CRP [mg/L] | ≤ 12 | 13.3 ± 29.6 |
10.6 ± 16.7 |
ns | 12.5 ± 27.2 |
14.5 ± 32.7 |
ns | 9.6 ± 20.5 |
17.6 ± 36.6 |
* * | 8.6 ± 19.1 |
17.1 ± 34.9 |
* * |
| 13–17 | 10.0 ± 19.4 |
12.3 ± 21.0 |
ns | 9.1 ± 16.9 |
13.0 ± 25.1 |
ns | 7.7 ± 14.6 |
15.3 ± 26.4 |
* | 8.7 ± 15.7 |
12.0 ± 23.5 |
ns | |
|
IL-6 [pg/mL) |
≤ 12 | 8.7 ± 23.3 |
23.7 ± 18.4 |
ns | 7.5 ± 20.2 |
28.7 ± 47.8 |
* * | 4.5 ± 9.3 |
25.9 ± 44.7 |
* ** | 4.5 ± 9.4 |
24.2 ± 43.3 |
* ** |
| 13–17 | 5.9 ± 18.4 |
15.2 ± 12.0 |
ns | 3.5 ± 10.1 |
30.1 ± 45.9 |
* ** | 3.7 ± 10.1 |
32.6 ± 49.8 |
* ** | 3.5 ± 10.7 |
17.2 ± 35.5 |
* | |
|
PCT [ng/mL] |
≤ 12 | 0.3 ± 0.9 |
0.2 ± 0.3 |
ns | 0.2 ± 0.9 |
0.4 ± 1.1 |
ns | 0.2 ± 0.5 |
0.4 ± 1.3 |
* | 0.1 ± 0.5 |
0.4 ± 1.3 |
* * |
| 13–17 | 0.2 ± 0.7 |
0.3 ± 0.5 |
ns | 0.1 ± 0.7 |
0.3 ± 0.7 |
ns | 0.1 ± 0.8 |
0.3 ± 0.6 |
ns | 0.2 ± 0.8 |
0.2 ± 0.5 |
ns | |
|
WBC [× 103/µL] |
≤ 12 | 8.5 ± 4.4 |
9.2 ± 3.0 |
ns | 8.5 ± 4.5 |
8.8 ± 3.8 |
ns | 8.1 ± 3.9 |
9.1 ± 4.8 |
* | 7.9 ± 3.5 |
9.0 ± 4.9 |
* * |
| 13–17 | 6.3 ± 3.1 |
6.5 ± 3.0 |
ns | 6.1 ± 3.0 |
7.0 ± 3.2 |
ns | 6.0 ± 3.0 |
7.2 ± 3.2 |
* | 6.1 ± 3.1 |
6.8 ± 3.1 |
ns | |
ns – not significant; * - p < 0.05; * * - p < 0.01; * ** - p < 0.001
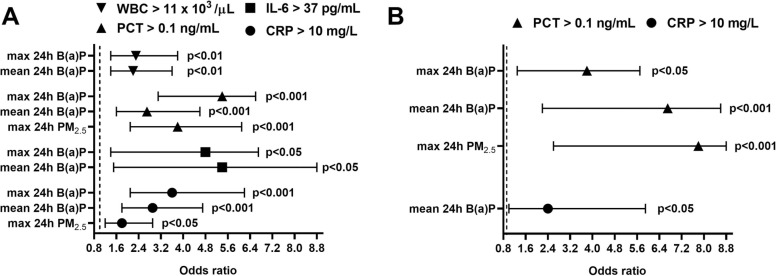
As further demonstrated, patients aged ≤ 12 years exposed to max 24 h PM2.5 levels exceeding the quality limit revealed increased odds of CRP > 10 mg/L and PCT > 0.1 ng/mL at admission. In turn, exposure to elevated mean and max B(a)P concentrations increased odds for CRP > 10 mg/L, IL-6 > 37 pg/mL, PCT > 0.1 ng/mL and WBC > 11 × 103/µL.( Fig. 2A). In case of patients aged 13–17 years, exceedances of max 24 PM2.5, mean and max B(a)P levels were associated with higher odds of PCT > 0.1 ng/mL. Increased odds of CRP > 10 mg/L were also found for patients exposed to max 24 h level above the quality limit (Fig. 2B).
Fig. 2.
The odds ratio (95% confidence interval) of significantly increased inflammatory markers at admission in pediatric patients aged ≤ 12 years (A) and 13–17 years (B) in relation to the exposure to air pollution parameters exceeding limits during a week before hospitalization.
3.4. Air pollution and the clinical course of COVID-19
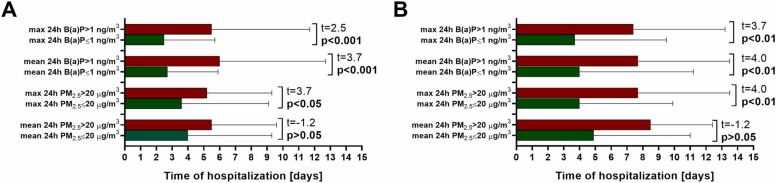
Odds for SpO2 < 95% at admission were increased only in patients aged ≤ 12 years exposed to elevated mean 24 h B(a)P level (OR: 3.2, 95% CI: 1.2–10.6, p < 0.05). Children aged ≤ 12 years exposed to max 24 h PM2.5, mean 24 h B(a)P and max 24 h B(aP) levels exceeding the limits required an extended hospital stay, on average by 40.5%, 118.5% and 120.0%, respectively ( Fig. 3A). Similarly, in patients aged 13–17 years, the length of hospital stay was longer by 92.5%, 92.5% and 100.0%, respectively (Fig. 3B). Association between air pollution and death or the need for oxygen therapy and mechanical ventilation was not evaluated due to a low number of pediatric patients with these outcomes (Table 1).
Fig. 3.
The length of hospital stay (mean ± SD) in patients aged ≤ 12 (n = 557) (A) and 13–17 years (n = 209) (B) exposed to air pollutants exceeding/not exceeding the limits during a week before hospitalization. The red bar – pollution level exceeding the quality limit; the green bar – pollution level within the quality limit.
4. Discussion
This study demonstrates the direct links between outdoor air pollution and clinical manifestation of COVID-19 in pediatric patients, indicating that exposure to pollutants such as PM2.5 and B(a)P can increase the odds of selected symptoms manifestation, increased inflammatory response, and extended hospital stay. Although the links between the severity of COVID-19 and air pollution have already been explored, contrary to our study, previous research focused on adult or general populations, not specifically on pediatric groups (Rzymski et al., 2022; Martinez-Boubeta and Simeonidis, 2022, Bowe et al., 2021, Kogevinas et al., 2021).
The present study's findings add to a general understanding of the adverse health effects of air pollution. They are particularly relevant for regions with deteriorated air quality, such as Poland, where air pollution in almost all areas exceeds air standards due to extensive coal-burning (European Environment Agency, 2021). Notably, increased airborne levels of PM2.5 and B(a)P in the temperate zone overlap with the seasonal increase in SARS-Cov-2 infections (Gavenčiak et al., 2021, Rogula-Kozłowska et al., 2014). The present research highlights that this can increase the overall COVID-19 burden related to pediatric patients.
Instead of using generalized population-based data as in numerous previous analyses of the relationship between air pollution and COVID-19, the levels of PM2.5 and B(a)P before hospitalization were matched for each patient allowing to postulate the existence of a causative relationship between exposure to air pollutants and clinical course of the disease. A week preceding hospitalization represents a period of transition of SARS-CoV-2 infection from incubation phase to symptomatic one. During this time, the antiviral defense in unvaccinated individuals is solely based on the innate immune response. It includes a repertoire of cells, i.e., macrophages, natural killer cells, monocytes, neutrophils, and dendritic cells, recognizing pathogen-associated molecular patterns and inducing inflammatory signaling (Kasuga et al., 2021, Diamond and Kanneganti, 2022). Children have been shown to display higher basal expression of the relevant pattern-recognition receptor pathways in respiratory epithelial cells, dendritic cells, and macrophages, ultimately resulting in a more robust innate antiviral response to SARS-CoV-2 infection compared to adult subjects (Loske et al., 2021). As postulated, this is, at least partially, responsible for the higher rate of asymptomatic and mild cases of COVID-19, faster recovery, and lower incidence of long-term consequences of disease in children (Ding et al., 2020, Falahi et al., 2021, Molteni et al., 2021). Significantly in this context, PM2.5 and B(a)P are well documented to affect innate immune responses adversely and trigger hyper-inflammation in the respiratory tract, effectively jeopardizing its function (Xing et al., 2016, Lewis et al., 2005).
Furthermore, some studies demonstrated that children's nasal epithelium and bronchial tissue reveal significantly lower expression of receptor angiotensin-converting enzyme 2 (ACE2), acting as a cellular receptor for SARS-CoV-2, and lower expression of TMPRSS2, which along with furin is essential for its proteolytic activation (Bunyavanich et al., 2020, Saheb Sharif-Askari et al., 2020). In turn, exposures to PM2.5 and B(a)P have been shown to up-regulate ACE2 and TMPRSS2 (Borro et al., 2020; H.-H. Li et al., 2021; G. Wang et al., 2021). Therefore, exposure to elevated levels of air pollutants overlapping the SARS-CoV-2 infection can aggravate the clinical severity of COVID-19 in children. This may also explain the previously observed increase in the number of children with symptomatic SARS-CoV-2 infections and pediatric patients requiring hospitalization due to COVID-19 during the second pandemic wave (September-December 2020) when compared to the first wave (March-August 2020) (Pokorska-Śpiewak et al., 2021).
Although air pollution affected symptomatology, inflammatory markers, and length of hospitalization in both age groups of pediatric patients considered in the study, broader effects were observed for children ≤ 12 years. This can be to several interlinked factors characterizing this group compared to older children, such as increased minute ventilation, immature immune response, dynamically developing respiratory system, and tendency to spend more time outdoors, ultimately resulting in greater exposure and its health consequences (Buka et al., 2006, Dixon, 2002, Gilliland et al., 1999, Pinkerton and Joad, 2000). In addition, during the pandemic lockdowns and periods of remote learning, children may be increasingly exposed to household air pollution. During periods of high outdoor concentrations, air pollutants can infiltrate indoors and be trapped to varying degrees depending on buildings' topography, configuration, and ventilation (Nandasena, Wickremasinghe, and Sathiakumar, 2013).
Importantly, the present study shows that children's exposure to elevated levels of B(a)P may have more profound effects on the COVID-19 clinical course than in the case of PM2.5. However, the majority of previous research on air pollution and COVID-19 and other respiratory diseases focuses not on polycyclic aromatic hydrocarbons such as B(a)P, but on particulates, ozone, sulfur dioxide, and nitrous oxides infections (Rodrigues et al., 2019, Wrotek et al., 2021, Nenna et al., 2017, Mele et al., 2021, Mendy et al., 2021, Veronesi et al., 2022). Among multifaceted harmful effects of B(a)P on human health, including promotion of cancerogenesis, its short-term exposure was shown to induce airway epithelial injury and enhance the release of epithelial-derived pro-inflammatory cytokines, such as thymic stromal lymphopoietin (a distant paralog of IL-7) and IL-33 (Fan et al., 2021). In turn, increased IL-33 was linked to more severe COVID-19 as it facilitates inflammation in the respiratory tract by inducing the release of innate pro-inflammatory cytokines, i.e., IL-1β, IL-6, TNF-α, IL-12, and IL-23 (Markovic et al., 2021). Moreover, thymic stromal lymphopoietin, which, along with its receptor, mediates the release of pro-inflammatory cytokines (including IL-6_ and chemokines, ultimately contributing to airway inflammation, has also been shown to correlate with more severe COVID-19 (Caterino et al., 2021, Shan et al., 2010)). Notably, in the present study, pediatric patients (particularly ≤12 years) exposed to elevated levels of B(a)P before hospitalization exhibited higher concentrations of different inflammatory markers at admission, including IL-6. All in all, further studies on air pollution and the severity of COVID-19 and other respiratory diseases in pediatric and adult patients should include B(a)P as a separate risk factor.
Although the present findings provide important data for public health policy, study limitations must be stressed. The research was focused on two major air pollutants, PM2.5 and B(a)P, in regions such as Poland, where coal and wood combustion plays a significant role in domestic heating (Anioł et al., 2021, Nazar and Niedoszytko, 2022). However, studies show that other air pollutants, i.e., nitrogen oxides and ozone, may also affect the COVID-19 severity and mortality (Mele et al., 2021, Khorsandi et al., 2021, Achebak et al., 2021). One should also note that the present investigation did not include the potential differences in socioeconomic factors, health behaviors (e.g., physical activity) and presence of comorbidities (e.g., chronic lung disease, diabetes, heart disease, immune deficiencies, seizure disorders, obesity,) that may affect the susceptibility of children to COVID-19 (Choi et al., 2022, Størdal et al., 2022). Moreover, the patient data were collected over 17 months, during which various SARS-CoV-2 variants emerged and dominated (Hryhorowicz et al., 2021, Jabłońska et al., 2021). The shifts in viral variants were not included in the study because the efficient nationwide genomic surveillance was not available in Poland, while the number of SARS-CoV-2 sequences deposited by Polish institutions in the GISAID database was very low (Furuse, 2021). However, one should note that the epidemiological study conducted in Poland during the same period did not show significant increases in the admission of individuals < 18 that would otherwise indicate changes in virus pathogenicity (Flisiak, Rzymski et al., 2021). Similarly, a study comparing the illness profile in children infected with B.1.1.7 (alpha) variant, dominant at the beginning of 2021, and B.1.617.2 (delta) variant, predominantly circulating since May 2021, did not show any relevant differences in symptoms prevalence, disease duration, and burden (Molteni, Sudre, Canas, Bhopal, Hughes, Chen et al., 2021). Children diagnosed with COVID-19 caused by delta variant did not show significant differences in inflammatory markers when compared to those infected from February to March 2020 (Sheng, Shao, and Wang, 2021). Therefore, the SARS-CoV-2 evolution appears insufficient in explaining the differences in the clinical parameters found in the present study between children exposed to and not exposed to air pollutants exceeding quality standards. One should also note that the clinical course of COVID-19 can be, to some extent, influenced by meteorological factors such as temperature and humidity (Bochenek et al., 2022), which were not included in the present study. Moreover, the data on the daily duration of outdoor activity and indoor pollution levels, which may affect the exposure to B(a)P and PM2.5 (Christian et al., 2022; Rivas et al., 2014), were not available for the studied group. Last but not least, the pediatric group in this study was constituted only of unvaccinated individuals. Whether COVID-19 vaccination may suppress the effect of air pollution on the inflammation levels during SARS-CoV-2 infection and the clinical severity of the disease require further investigations.
5. Conclusion
The results of this study suggests that exposure to air pollutants, particularly B(a)P, at a time of SARS-CoV-2 infection might affect the clinical manifestation of COVID-19 in pediatric patients, with a more significant broad effect seen in those aged ≤ 12 years. Overall, the findings call for more epidemiological studies on the effect of B(a)P on the severity of COVID-19 and other respiratory diseases and highlight that successful mitigation of the COVID-19 burden should also include measures to decrease the exposure to air pollution.
Funding
This research was supported by the Medical Research Agency in Poland, grant number 2020/ABM/COVID19/PTEILCHZ, the Polish Association of Epidemiologists and Infectiologists, and the Department of Environmental Medicine (Poznan University of Medical Sciences, Poland).
CRediT authorship contribution statement
Piotr Rzymski, Barbara Poniedziałek, Robert Flisiak: Conceptualization. Piotr Rzymski, Barbara Poniedziałek, Robert Flisiak: Data curation. Piotr Rzymski, Barbara Poniedziałek, Joanna R Rosińska: Formal analysis. Barbara Poniedziałek, Robert Flisiak: Funding acquisition. Piotr Rzymski, Barbara Poniedziałek, Joanna Rosińska, Przemysław Ciechanowski, Michał Peregrym, Maria Pokorska-Śpiewak, Ewa Talarek, Izabela Zaleska, Paulina Frańczak-Chmura, Małgorzata Pilarczyk, Magdalena Figlerowicz, Izabela Kucharek, Robert Flisiak: Investigation. Piotr Rzymski, Barbara Poniedziałek, Robert Flisiak: Methodology. Robert Flisiak: Project administration. Barbara Poniedziałek, Robert Flisiak: Resources. Piotr Rzymski, Robert Flisiak: Supervision. Piotr Rzymski: Roles/Writing – original draft.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- Achebak, Hicham, Hervé Petetin, Marcos Quijal-Zamorano, Dene Bowdalo, Carlos Pérez García-Pando, and Joan Ballester, 2021, Trade-Offs between Short-Term Mortality Attributable to NO2 and O3 Changes during the COVID-19 Lockdown across Major Spanish Cities. Environmental Pollution (Barking, Essex: 1987) 286 (117220): 117220. [DOI] [PMC free article] [PubMed]
- Anioł Ewa, Suder Jacek, Bihałowicz Jan Stefan, Majewski Grzegorz. The quality of air in polish health resorts with an emphasis on health on the effects of benzo(a)pyrene in 2015–2019. Climate. 2021;9(5):74. [Google Scholar]
- Babin Steven M., Howard S., Burkom, Holtry Rekha S., Tabernero Nathaniel R., Stokes Lynette D., Davies-Cole John O., DeHaan Kerda, Lee Deitra H. Pediatric patient asthma-related emergency department visits and admissions in Washington, DC, from 2001-2004, and associations with air quality, socio-economic status and age group. Environ. Health.: A Glob. Access Sci. Source. 2007;6(1):9. doi: 10.1186/1476-069X-6-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartlett J.A., Schleifer S.J., Demetrikopoulos M.K., Delaney B.R., Shiflett S.C., Keller S.E. Immune function in healthy adolescents. Clin. Diagn. Lab. Immunol. 1998;5(1):105–113. doi: 10.1128/cdli.5.1.105-113.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blot Mathieu, Bour Jean-Baptiste, Quenot Jean Pierre, Bourredjem Abderrahmane, Nguyen Maxime, Guy Julien, Monier Serge, et al. The Dysregulated Innate Immune Response in Severe COVID-19 Pneumonia That Could Drive Poorer Outcome. J. Transl. Med. 2020;18(1):457. doi: 10.1186/s12967-020-02646-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bochenek Bogdan, Jankowski Mateusz, Gruszczynska Marta, Jaczewski Adam, Ziemianski Michal, Pyrc Robert, Wyszogrodzki Andrzej, et al. Weather as a Potential Cause of Regional Differences in the Dynamics of COVID-19 Transmission in Poland: Implications for Epidemic Forecasting. Pol. Arch. Intern. Med. 2022;132(1) doi: 10.20452/pamw.16110. [DOI] [PubMed] [Google Scholar]
- Borro Marina, Girolamo Paolo Di, Gentile Giovanna, Luca Ottavia De, Preissner Robert, Marcolongo Adriano, Ferracuti Stefano, Simmaco Maurizio. Evidence-Based Considerations Exploring Relations between SARS-CoV-2 Pandemic and Air Pollution: Involvement of PM2.5-Mediated up-Regulation of the Viral Receptor ACE-2. Int. J. Environ. Res. Public Health. 2020;17(15):5573. doi: 10.3390/ijerph17155573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowe Benjamin, Xie Yan, Gibson Andrew K., Cai Miao, van Donkelaar Aaron, Martin Randall V., Burnett Richard, Al-Aly Ziyad. Ambient fine particulate matter air pollution and the risk of hospitalization among COVID-19 positive individuals: cohort study. Environ. Int. 2021;154(106564) doi: 10.1016/j.envint.2021.106564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buka Irena, Koranteng Samuel, Osornio-Vargas Alvaro R. The effects of air pollution on the health of children. Paediatr. Child Health. 2006;11(8):513–516. [PMC free article] [PubMed] [Google Scholar]
- Bunyavanich Supinda, Do Anh, Vicencio Alfin. Nasal gene expression of angiotensin-converting enzyme 2 in children and adults. JAMA: J. Am. Med. Assoc. 2020;323(23):2427–2429. doi: 10.1001/jama.2020.8707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caterino Marianna, Gelzo Monica, Sol Stefano, Fedele Roberta, Annunziata Anna, Calabrese Cecilia, Fiorentino Giuseppe, et al. Dysregulation of lipid metabolism and pathological inflammation in patients with COVID-19. Sci. Rep. 2021;11(1):2941. doi: 10.1038/s41598-021-82426-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Renjie, Yin Peng, Meng Xia, Liu Cong, Wang Lijun, Xu Xiaohui, Ross Jennifer A., et al. Fine Particulate Air Pollution and Daily Mortality. A Nationwide Analysis in 272 Chinese Cities. Am. J. Respir. Crit. Care Med. 2017;196(1):73–81. doi: 10.1164/rccm.201609-1862OC. [DOI] [PubMed] [Google Scholar]
- Choi Jae Hong, Choi Soo-Han, Yun Ki. Wook. Risk Factors for Severe COVID-19 in Children: A Systematic Review and Meta-Analysis. J. Korean Med. Sci. 2022;37(5) doi: 10.3346/jkms.2022.37.e35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coker Eric S., Martin James, Bradley Lauren D., Sem Karen, Clarke Kayan, Sabo-Attwood Tara. A time series analysis of the ecologic relationship between acute and intermediate PM2.5 exposure duration on neonatal intensive care unit admissions in Florida. Environ. Res. 2021;196(110374) doi: 10.1016/j.envres.2020.110374. [DOI] [PubMed] [Google Scholar]
- Diamond Michael S., Kanneganti Thirumala-Devi. Innate immunity: the first line of defense against SARS-CoV-2. Nat. Immunol. 2022;23(2):165–176. doi: 10.1038/s41590-021-01091-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ding Yudan, Yan Haohao, Guo Wenbin. Clinical characteristics of children with COVID-19: a meta-analysis. Front. Pediatr. 2020;8(July):431. doi: 10.3389/fped.2020.00431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Directive 2004/107/EC n.d. Accessed February 7, 2022. https://eur-lex.europa.eu/legal-content/EN/TXT/?uri=CELEX:02004L0107–20150918.
- Directive 2008/50/EC. n.d. Accessed February 7, 2022. https://eur-lex.europa.eu/legal-content/EN/TXT/?uri=CELEX:02008L0050–20150918.
- Dixon Jane K. Kids need clean air: air pollution and children’s health. Fam. Community Health. 2002;24(4):9–26. doi: 10.1097/00003727-200201000-00004. [DOI] [PubMed] [Google Scholar]
- European Environment Agency, 2021, Air Quality in Europe 2021. November 26, 2021. https://www.eea.europa.eu/publications/air-quality-in-europe-2021.
- Falahi S., Abdoli A., Kenarkoohi A. Claims and Reasons about Mild COVID-19 in Children. N. Microbes N. Infect. 2021;41(100864) doi: 10.1016/j.nmni.2021.100864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fan Lieyang, Li Wei, Ma Jixuan, Cheng Man, Xie Li, Ye Zi, Xie Yujia, et al. Benzo(a)pyrene induces airway epithelial injury through wnt5a-mediated non-canonical Wnt-YAP/TAZ signaling. Sci. Total Environ. 2021;815(151965) doi: 10.1016/j.scitotenv.2021.151965. [DOI] [PubMed] [Google Scholar]
- Flisiak Robert, Horban Andrzej, Jaroszewicz Jerzy, Kozielewicz Dorota, Mastalerz-Migas Agnieszka, Owczuk Radosław, Parczewski Mi.łosz, et al. Management of SARS-CoV-2 Infection: Recommendations of the Polish Association of Epidemiologists and Infectiologists as of April 26, 2021. Pol. Arch. Intern. Med. 2021;131(5):487–496. doi: 10.20452/pamw.15979. [DOI] [PubMed] [Google Scholar]
- Flisiak Robert, Horban Andrzej, Jaroszewicz Jerzy, Kozielewicz Dorota, Pawłowska Ma.łgorzata, Parczewski Mi.łosz, Piekarska Anna, Simon Krzysztof, Tomasiewicz Krzysztof, Zarębska-Michaluk Dorota. “Management of SARS-CoV-2 Infection: Recommendations of the Polish Association of Epidemiologists and Infectiologists as of March 31, 2020. Pol. Arch. Intern. Med. 2020;130(4):352–357. doi: 10.20452/pamw.15270. [DOI] [PubMed] [Google Scholar]
- Flisiak Robert, Horban Andrzej, Jaroszewicz Jerzy, Kozielewicz Dorota, Pawłowska Ma.łgorzata, Parczewski Mi.łosz, Piekarska Anna, Simon Krzysztof, Tomasiewicz Krzysztof, Zarębska-Michaluk Dorota. Management of SARS-CoV-2 Infection: Recommendations of the Polish Association of Epidemiologists and Infectiologists. Annex No. 1 as of June 8, 2020. Pol. Arch. Intern. Med. 2020;130(6):557–558. doi: 10.20452/pamw.15424. [DOI] [PubMed] [Google Scholar]
- Flisiak Robert, Parczewski Mi.łosz, Horban Andrzej, Jaroszewicz Jerzy, Kozielewicz Dorota, Pawłowska Ma.łgorzata, Piekarska Anna, Simon Krzysztof, Tomasiewicz Krzysztof, Zarębska-Michaluk Dorota. Management of SARS-CoV-2 Infection: Recommendations of the Polish Association of Epidemiologists and Infectiologists. Annex No. 2 as of October 13, 2020. Pol. Arch. Intern. Med. 2020;130(10):915–918. doi: 10.20452/pamw.15658. [DOI] [PubMed] [Google Scholar]
- Flisiak Robert, Rzymski Piotr, Zarębska-Michaluk Dorota, Rogalska Magdalena, Rorat Marta, Czupryna Piotr, Lorenc Beata, et al. Demographic and Clinical Overview of Hospitalized COVID-19 Patients during the First 17 Months of the Pandemic in Poland. J. Clin. Med. 2021;11(1):117. doi: 10.3390/jcm11010117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furuse Yuki. Genomic sequencing effort for SARS-CoV-2 by country during the pandemic. Int. J. Infect. Dis.: IJID: Off. Publ. Int. Soc. Infect. Dis. 2021;103(February):305–307. doi: 10.1016/j.ijid.2020.12.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galani Ioanna-Evdokia, Andreakos Evangelos. Impaired innate antiviral defenses in COVID-19: causes, consequences and therapeutic opportunities. Semin. Immunol. 2021;55(101522) doi: 10.1016/j.smim.2021.101522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gavenčiak Tomáš., Monrad Joshua Teperowski, Leech Gavin, Sharma Mrinank, Mindermann S.ören, Brauner Jan Markus, Bhatt Samir, Kulveit Jan. Seasonal variation in SARS-CoV-2 transmission in temperate climates. BioRxiv. medRxiv. 2021 doi: 10.1101/2021.06.10.21258647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilliland F.D., McConnell R., Peters J., Gong H., Jr. A theoretical basis for investigating ambient air pollution and children’s respiratory health. Environ. Health Perspect. 1999;107(Suppl 3):403–407. doi: 10.1289/ehp.99107s3403. (June) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glencross, Drew A., Tzer-ren Ho, Nuria Camiña, Catherine M. Hawrylowicz, And Paul E. Pfeffer, 2020, Air Pollution and Its Effects on the Immune System. Free Radical Biology & Medicine 151 (May): 56–68. [DOI] [PubMed]
- Graff Kelly, Smith Christiana, Silveira Lori, Jung Sarah, Curran-Hays Shane, Jarjour Jane, Carpenter Lauren, et al. Risk factors for severe COVID-19 in children. Pediatr. Infect. Dis. J. 2021;40(4):e137–e145. doi: 10.1097/INF.0000000000003043. [DOI] [PubMed] [Google Scholar]
- Hryhorowicz Szymon, Ustaszewski Adam, Kaczmarek-Ryś Marta, Lis Emilia, Witt Michał., Pławski Andrzej, Ziętkiewicz Ewa. European context of the diversity and phylogenetic position of SARS-CoV-2 sequences from polish COVID-19 patients. J. Appl. Genet. 2021;62(2):327–337. doi: 10.1007/s13353-020-00603-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jabłońska Katarzyna, Aballéa Samuel, Auquier Pascal, Toumi Mondher. On the Association between SARS-COV-2 Variants and COVID-19 Mortality during the Second Wave of the Pandemic in Europe. J. Mark. Access Health Policy. 2021;9(1) doi: 10.1080/20016689.2021.2002008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson William M., Price Jerri C., Eisler Lisa, Sun Lena S., Lee Jennifer J. COVID-19 in pediatric patients: a systematic review. J. Neurosurg. Anesthesiol. 2022;34(1):141–147. doi: 10.1097/ANA.0000000000000803. [DOI] [PubMed] [Google Scholar]
- Jang Jinhwa, Hwang Myung-Jae, Kim Yoo-Yeon, Park Shin Young, Yoo Myeongsu, Kim Seong-Sun, Lee Sangwon, Kwon Donghyok. Epidemiological Characteristics and Transmission Patterns of COVID-19 Cases among Children and Adolescents Aged 0-18 Years in South Korea. Risk Manag. Healthc. Policy. 2022;15(February):219–227. doi: 10.2147/RMHP.S338121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janssen Nico A.F., Grondman Inge, de Nooijer Aline H., Boahen Collins K., Koeken Valerie A.C.M., Matzaraki Vasiliki, Kumar Vinod, et al. Dysregulated innate and adaptive immune responses discriminate disease severity in COVID-19. J. Infect. Dis. 2021;223(8):1322–1333. doi: 10.1093/infdis/jiab065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kasuga Yusuke, Zhu Baohui, Jang Kyoung-Jin, Yoo Ji-Seung. Innate immune sensing of coronavirus and viral evasion strategies. Exp. Mol. Med. 2021;53(5):723–736. doi: 10.1038/s12276-021-00602-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khorsandi Babak, Farzad Kiarash, Tahriri Hannaneh, Maknoon Reza. Association between short-term exposure to air pollution and COVID-19 hospital admission/mortality during warm seasons. Environ. Monit. Assess. 2021;193(7):426. doi: 10.1007/s10661-021-09210-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kogevinas Manolis, Castaño-Vinyals Gemma, Karachaliou Marianna, Espinosa Ana, Cid Rafael de, Garcia-Aymerich Judith, Carreras Anna, et al. Ambient Air Pollution in Relation to SARS-CoV-2 Infection, Antibody Response, and COVID-19 Disease: A Cohort Study in Catalonia, Spain (COVICAT Study).”. Environ. Health Perspect. 2021;129(11) doi: 10.1289/EHP9726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurt Ozlem Kar, Zhang Jingjing, Pinkerton Kent E. Pulmonary health effects of air pollution. Curr. Opin. Pulm. Med. 2016;22(2):138–143. doi: 10.1097/MCP.0000000000000248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis Toby C., Robins Thomas G., Timothy Dvonch J., Keeler Gerald J., Yip Fuyuen Y., Mentz Graciela B., Lin Xihong, et al. Air pollution–associated changes in lung function among asthmatic children in detroit. Environ. Health Perspect. 2005;113(8):1068–1075. doi: 10.1289/ehp.7533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Hsin-Hsien, Liu Chen-Chi, Hsu Tien-Wei, Lin Jiun-Han, Hsu Jyuan-Wei, Li Anna Fen-Yau, Yeh Yi-Chen, Hung Shih-Chieh, Hsu Han-Shui. Upregulation of ACE2 and TMPRSS2 by Particulate Matter and Idiopathic Pulmonary Fibrosis: A Potential Role in Severe COVID-19. Part. Fibre Toxicol. 2021;18(1):11. doi: 10.1186/s12989-021-00404-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Yang, Batibawa Josevata Werelagi, Du Zhou, Liang Shuang, Duan Junchao, Sun Zhiwei. Acute exposure to PM2.5 triggers lung inflammatory response and apoptosis in rat. Ecotoxicol. Environ. Saf. 2021;222(112526) doi: 10.1016/j.ecoenv.2021.112526. [DOI] [PubMed] [Google Scholar]
- Loske J., Röhmel J., Lukassen S., Stricker S., Magalhães V.G., Liebig J., Chua R.L., et al. Pre-activated antiviral innate immunity in the upper airways controls early SARS-CoV-2 infection in children. Nat. Biotechnol. 2021:1–6. doi: 10.1038/s41587-021-01037-9. (August) [DOI] [PubMed] [Google Scholar]
- Mania Anna, Pokorska-Śpiewak Maria, Figlerowicz Magdalena, Pawłowska Ma.łgorzata, Mazur-Melewska Katarzyna, Faltin Kamil, Talarek Ewa, et al. Pneumonia, gastrointestinal symptoms, comorbidities, and coinfections as factors related to a lengthier hospital stay in children with COVID-19-analysis of a paediatric part of polish register SARSTer. Infect. Dis. (Lond., Engl. ) 2022;54(3):196–204. doi: 10.1080/23744235.2021.1995628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marczyńska Magdalena, Pokorska-Śpiewak Maria, Talarek Ewa, Figlerowicz Magdalena, Kalicki Bolesław, Kuchar Ernest, Majda-Stanisławska Ewa, et al. Management of a child with Covid-19. Recommendations for pediatricians and family medicine physicians in primary healthcare and hospital settings. Przegląd Pedia. 2020;49(4):1–7. [Google Scholar]
- Markovic, Sekulic Sofija, Jovanovic Marina, Gajovic Nevena, Jurisevic Milena, Arsenijevic Nebojsa, Jovanovic Marina, Jovanovic Milan, et al. IL 33 Correlates with COVID-19 Severity, Radiographic and Clinical Finding. Front. Med. 2021;8(November) doi: 10.3389/fmed.2021.749569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez-Boubeta C., Simeonidis K. Airborne Magnetic Nanoparticles May Contribute to COVID-19 Outbreak: Relationships in Greece and Iran. Environ. Res. 204 (Pt B) 2022 doi: 10.1016/j.envres.2021.112054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mele Marco, Magazzino Cosimo, Schneider Nicolas, Strezov Vladimir. NO2 levels as a contributing factor to COVID-19 deaths: the first empirical estimate of threshold values. Environ. Res. 2021;194(110663) doi: 10.1016/j.envres.2020.110663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mendy Angelico, Wu Xiao, Keller Jason L., Fassler Cecily S., Apewokin Senu, Mersha Tesfaye B., Xie Changchun, Pinney Susan M. Air Pollution and the Pandemic: Long-Term PM2.5 Exposure and Disease Severity in COVID-19 Patients. Respirol. (Carlton, Vic. ) 2021;26(12):1181–1187. doi: 10.1111/resp.14140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molteni Erika, Sudre Carole H., Canas Liane S., Bhopal Sunil S., Hughes Robert C., Antonelli Michela, Murray Benjamin, et al. Vol. 5. 2021. Illness duration and symptom profile in symptomatic UK School-Aged Children Tested for SARS-CoV-2; pp. 708–718. (The Lancet. Child & Adolescent Health). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molteni Erika, Sudre Carole H., Canas Liane S., Bhopal Sunil S., Hughes Robert C., Chen Liyuan, Deng Jie, et al. Illness Characteristics of COVID-19 in Children Infected with the SARS-CoV-2 Delta Variant. BioRxiv. 2021 doi: 10.1101/2021.10.06.21264467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nandasena Sumal, Wickremasinghe Ananda Rajitha, Sathiakumar Nalini. Indoor air pollution and respiratory health of children in the developing world. World J. Clin. Pediatr. 2013;2(2):6–15. doi: 10.5409/wjcp.v2.i2.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nazar Wojciech, Niedoszytko Marek. Air Pollution in Poland: A 2022 Narrative Review with Focus on Respiratory Diseases. Int. J. Environ. Res. Public Health. 2022;19(2):895. doi: 10.3390/ijerph19020895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nenna Raffaella, Evangelisti Melania, Frassanito Antonella, Scagnolari Carolina, Pierangeli Alessandra, Antonelli Guido, Nicolai Ambra, et al. Respiratory Syncytial Virus Bronchiolitis, Weather Conditions and Air Pollution in an Italian Urban Area: An Observational Study. Environ. Res. 2017;158(October):188–193. doi: 10.1016/j.envres.2017.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okarska-Napierała Magdalena, Ludwikowska Kamila, Jackowska Teresa, Książyk Janusz, Buda Piotr, Mazur Artur, Szenborn Leszek, Werner Bo.żena, Wysocki Jacek, Kuchar Ernest. Approach to a Child with Pediatric Inflammatory Multisystem Syndrome with Covid-19. Recommendations by the Polish Pediatric Society Expert Group. Update February 2021. Przegląd Ped. 2021;50(2):1–11. [Google Scholar]
- Peyneau Marine, Granger Vanessa, Wicky Paul-Henri, Khelifi-Touhami Dounia, Timsit Jean-François, Lescure François-Xavier, Yazdanpanah Yazdan, et al. Innate Immune Deficiencies Are Associated with Severity and Poor Prognosis in Patients with COVID-19. Sci. Rep. 2022;12(1):638. doi: 10.1038/s41598-021-04705-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinkerton K.E., Joad J.P. The mammalian respiratory system and critical windows of exposure for children’s health. Environ. Health Perspect. 2000;108(Suppl 3):457–462. doi: 10.1289/ehp.00108s3457. (June) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pokorska-Śpiewak Maria, Talarek Ewa, Mania Anna, Pawłowska Ma.łgorzata, Popielska Jolanta, Zawadka Konrad, Figlerowicz Magdalena, et al. Clinical and Epidemiological Characteristics of 1283 Pediatric Patients with Coronavirus Disease 2019 during the First and Second Waves of the Pandemic-Results of the Pediatric Part of a Multicenter Polish Register SARSTer. J. Clin. Med. 2021;10(21):5098. doi: 10.3390/jcm10215098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodrigues Ana Filipa, Santos Ana Mafalda, Ferreira Ana Maria, Marino Roberta, Barreira Maria Esmeralda, Cabeda José Manuel. Year-long rhinovirus infection is influenced by atmospheric conditions, outdoor air virus presence, and immune system-related genetic polymorphisms. Food Environ. Virol. 2019;11(4):340–349. doi: 10.1007/s12560-019-09397-x. [DOI] [PubMed] [Google Scholar]
- Rogula-Kozłowska Wioletta, Klejnowski Krzysztof, Rogula-Kopiec Patrycja, Ośródka Leszek, Krajny Ewa, Błaszczak Barbara, Mathews Barbara. Spatial and Seasonal Variability of the Mass Concentration and Chemical Composition of PM2.5 in Poland. Air Qual., Atmosphere, Health. 2014;7(1):41–58. doi: 10.1007/s11869-013-0222-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogulski Mariusz, Badyda Artur. Air Pollution Observations in Selected Locations in Poland during the Lockdown Related to COVID-19. Atmosphere. 2021;12(7):806. [Google Scholar]
- Ryan Kathleen, Snow Kathryn, Danchin Margie, Mulholland Kim, Goldfeld Sharon, Russell Fiona. “SARS-CoV-2 infections and public health responses in schools and early childhood education and care centres in Victoria, Australia: an observational study. Lancet Reg. Health West. Pac. 2022;19(100369) doi: 10.1016/j.lanwpc.2021.100369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rzymski Piotr, Poniedziałek Barbara, Rosińska Joanna, Rogalska Magdalena, Zarębska-Michalik Dorota, Rorat Marta, Moniuszko-Malinowska Anna, Lorenc Beata, Kozielewicz Dorota, Piekarska Anna, Sikorska Katarzyna, Dworzańska Anna, Bolewska Beata, Angielski Grzegorz, Kowalska Justyna, Podlasin Regina, Oczko-Grzesik Barbara, Mazur Włodzimierz, Szymczak Aleksandra, Flisiak Robert. The association of airborne particulate matter and benzo[a]pyrene with the clinical course of COVID-19 in patients hospitalized in Poland. Environmental Pollution. 2022 doi: 10.1016/j.envpol.2022.119469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saheb Sharif-Askari Narjes, Sharif-Askari Fatemeh Saheb, Alabed Mashael, Temsah Mohamed-Hani, Heialy Saba Al, Hamid Qutayba, Halwani Rabih. Airways Expression of SARS-CoV-2 Receptor, ACE2, and TMPRSS2 Is Lower in Children than Adults and Increases with Smoking and COPD. Mol. Ther. Methods Clin. Dev. 2020;18(September):1–6. doi: 10.1016/j.omtm.2020.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shafiek Hala K., Abd El Lateef Hanan M., Boraey Naglaa F., Nashat Mohamed, Abd-Elrehim Ghada A.B., Abouzeid Heba, Hafez Sahbaa F.M., et al. Cytokine Profile in Egyptian Children and Adolescents with COVID-19 Pneumonia: A Multicenter Study. Pediatr. Pulmonol. 2021;56(12):3924–3933. doi: 10.1002/ppul.25679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shan Lianyu, Redhu Naresh Singh, Saleh Ali, Halayko Andrew J., Chakir Jamila, Gounni Abdelilah S. Thymic Stromal Lymphopoietin Receptor-Mediated IL-6 and CC/CXC Chemokines Expression in Human Airway Smooth Muscle Cells: Role of MAPKs (ERK1/2, P38, and JNK) and STAT3 Pathways. J. Immunol. 2010;184(12):7134–7143. doi: 10.4049/jimmunol.0902515. [DOI] [PubMed] [Google Scholar]
- Sheng Jun-Feng, Shao Lan, Wang Yu-Lin. Clinical Features of Children with Coronavirus Disease 2019 caused by delta variant infection. Zhongguo Dang Dai Er Ke Za Zhi [Chin. J. Contemp. Pediatr. ] 2021;23(12):1267–1270. doi: 10.7499/j.issn.1008-8830.2110043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Størdal Ketil, Ruiz Paz Lopez-Doriga, Greve-Isdahl Margrethe, Surén P.ål, Knudsen Per Kristian, Gulseth Hanne L.øvdal, Tapia German. Risk Factors for SARS-CoV-2 Infection and Hospitalisation in Children and Adolescents in Norway: A Nationwide Population-Based Study. BMJ Open. 2022;12(3) doi: 10.1136/bmjopen-2021-056549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veronesi Giovanni, Matteis Sara De, Calori Giuseppe, Pepe Nicola, Ferrario Marco M. Long-Term Exposure to Air Pollution and COVID-19 Incidence: A Prospective Study of Residents in the City of Varese, Northern Italy. Occup. Environ. Med. 2022;79(3) doi: 10.1136/oemed-2021-107833. oemed-2021-107833. [DOI] [PubMed] [Google Scholar]
- Wang Guizhen, Zhao Qun, Zhang Hui, Liang Fan, Zhang Chen, Wang Jun, Chen Zhenyin, et al. Degradation of SARS-CoV-2 Receptor ACE2 by the E3 Ubiquitin Ligase Skp2 in Lung Epithelial Cells. Front. Med. 2021;15(2):252–263. doi: 10.1007/s11684-021-0837-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang I.-Jen, Tung Tao-Hsin, Tang Chin-Sheng, Zhao Zi-Hao. Allergens, air pollutants, and childhood allergic diseases. Int. J. Hyg. Environ. Health. 2016;219(1):66–71. doi: 10.1016/j.ijheh.2015.09.001. [DOI] [PubMed] [Google Scholar]
- Ward Joseph L., Harwood Rachel, Smith Clare, Kenny Simon, Clark Matthew, Davis Peter J., Draper Elizabeth S., et al. Risk Factors for PICU Admission and Death among Children and Young People Hospitalized with COVID-19 and PIMS-TS in England during the First Pandemic Year. Nat. Med. 2022;28(1):193–200. doi: 10.1038/s41591-021-01627-9. [DOI] [PubMed] [Google Scholar]
- Woodruff Rebecca C., Campbell Angela P., Taylor Christopher A., Chai Shua J., Kawasaki Breanna, Meek James, Anderson Evan J., et al. Risk Factors for Severe COVID-19 in Children. Pediatr., Dec. 2021 doi: 10.1542/peds.2021-053418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wrotek August, Badyda Artur, Czechowski Piotr O., Owczarek Tomasz, Dąbrowiecki Piotr, Jackowska Teresa. Air Pollutants’ Concentrations Are Associated with Increased Number of RSV Hospitalizations in Polish Children. J. Clin. Med. 2021;10(15):3224. doi: 10.3390/jcm10153224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xing Yu-Fei, Xu Yue-Hua, Shi Min-Hua, Lian Yi-Xin. The impact of PM2.5 on the human respiratory system. J. Thorac. Dis. 2016;8(1):E69–E74. doi: 10.3978/j.issn.2072-1439.2016.01.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yasuhara Jun, Kuno Toshiki, Takagi Hisato, Sumitomo Naokata. Clinical characteristics of COVID-19 in children: a systematic review. Pediatr. Pulmonol. 2020;55(10):2565–2575. doi: 10.1002/ppul.24991. [DOI] [PubMed] [Google Scholar]